Introduction
Childhood behavioral health problems impact development and health outcomes across the lifespan. For example, chronic child behavior problems, including internalizing and externalizing symptoms, have not only been associated with lower self-esteem, peer relationship problems, and poor academic outcomes in childhood/adolescence, but also poorer physical and psychological health, substance use problems, less schooling (i.e., lower rates of high school completion, college enrollment, and college graduation), and lower earnings in adulthood (Farmer et al., Reference Farmer, Irvin, Motoca, Leung, Hutchins, Brooks and Hall2015; Ghandour et al., Reference Ghandour, Sherman, Vladutiu, Ali, Lynch, Bitsko and Blumberg2019; King et al., Reference King, McDougall, DeWit, Hong, Miller, Offord and LaPorta2005; Owens, Reference Owens2016; Sroufe & Rutter, Reference Sroufe and Rutter1984). Although a robust body of research suggests that various socio-ecological contexts, including families, neighborhoods, and schools influence children’s health and well-being (Aura et al., Reference Aura, Sormunen and Tossavainen2016), the ways in which these contextual factors differentially influence child behavior problems at different stages of development is unknown. That is, limited attention has been paid to the relative importance of family-, school-, and neighborhood-level contexts to children’s behavioral problems in different developmental periods, or the subsequent long-term impacts of those early contexts on child outcomes over time. Addressing this gap is critical to identifying time periods and contexts for optimal intervention to create environments that promote healthy behaviors across different life stages of childhood and adolescence.
Family context and child behavior problems
Key family protective factors, such as positive parent-child relationships, father involvement, lower parenting stress, positive parenting practices, higher parental education level, and higher parental income, are associated with greater behavioral well-being among children (Chen & Li, Reference Chen and Li2009; Erola et al., Reference Erola, Jalonen and Lehti2016; Lee et al., Reference Lee, Wickrama and Simons2013; Yoon et al., Reference Yoon, Kim, Yang, Lee, Latelle, Wang and Schoppe-Sullivan2021). Conversely, family risks and stressors, such as adverse childhood experiences including child maltreatment, parental mental health problems, and parental substance use, have negative impacts on child internalizing and externalizing behaviors (Burke et al., Reference Burke, Hellman, Scott, Weems and Carrion2011; Yoon et al., Reference Yoon, Yoon, Wang, Tebben, Lee and Pei2017). Based on a robust body of research highlighting child maltreatment and maternal behavioral health problems as salient risk factors for child behavior problems (Clarkson Freeman, Reference Clarkson Freeman2014; Hunt et al., Reference Hunt, Slack and Berger2017), we focus on child physical abuse, emotional abuse, maternal depression, and substance use problems as key family-level contextual factors related to child behavioral health. Child maltreatment, including physical and emotional abuse, has been found to be related to children’s internalizing and externalizing behavior problems, such as depression, anxiety, post-traumatic stress symptoms, aggression, adolescent substance use, and other risk-taking behavior (Gilbert et al., Reference Gilbert, Widom, Browne, Fergusson, Webb and Janson2009; Keiley et al., Reference Keiley, Howe, Dodge, Bates and Pettit2001; Lanier et al., Reference Lanier, Maguire-Jack, Lombardi, Frey and Rose2018; Muniz et al., Reference Muniz, Fox, Miley, Delisi, Cigarran and Birnbaum2019; Silva et al., Reference Silva, Graña and González-Cieza2014; Yoon et al., Reference Yoon, Voith and Kobulsky2018). Similarly, numerous studies have found that higher levels of maternal depression and substance use are associated with greater internalizing (e.g., depression) and externalizing (e.g., aggression) problems across childhood and adolescence (Bountress & Chassin, Reference Bountress and Chassin2015; Fanti & Henrich, Reference Fanti and Henrich2010; Goodman et al., Reference Goodman, Rouse, Connell, Broth, Hall and Heyward2011; Hser et al., Reference Hser, Lanza, Li, Kahn, Evans and Schulte2015; O’Connor et al., Reference O’Connor, Langer and Tompson2017).
Neighborhood context and child behavior problems
Children also are influenced by the broader neighborhood outside of their immediate family context. Neighborhood structural factors refer to a collection of demographic characteristics belonging to a neighborhood, such as poverty rate, age and racial breakdown of residents, amount of time residents have lived in the neighborhood, and number of residents who are unemployed. Growing up in highly impoverished areas has critical impacts on children (Aber et al., Reference Aber, Bennett, Conley and Li1997; Chaudry & Wimer, Reference Chaudry and Wimer2016). Specifically, children from neighborhoods with high poverty rates are more likely to have developmental issues, including higher rates of behavioral health problems (Aber et al., Reference Aber, Bennett, Conley and Li1997).
Neighborhoods are also places in which social interactions occur, and these interactions and bonds can impact children’s behavioral health. Collective efficacy refers to the trust and bonds between neighbors (social cohesion) and the willingness of neighbors to intervene on behalf of the collective good (informal social control) (Sampson et al., Reference Sampson, Raudenbush and Earls1997). Xue et al. (Reference Xue, Leventhal, Brooks-Gunn and Earls2005) found that behavioral health problems were more likely among children in neighborhoods with low levels of neighborhood collective efficacy.
School context and child behavior problems
As children enter school, significant portions of their day are spent engaging within their school environments. Thus, their interaction with peers and teachers and their feelings toward their school environment may also influence their health. For example, behavioral health problems are more common among children who experience bullying by their peers (Ttofi et al., Reference Ttofi, Bowes, Farrington and Lösel2014). Bullying relates to negative behavioral health outcomes through multiple pathways, including influence on a child’s self-esteem and social withdrawal, which can lead to internalizing behavior problems (Ttofi et al., Reference Ttofi, Bowes, Farrington and Lösel2014). Bullying may also increase the risk for externalizing behavior problems and risk-taking behaviors, such as aggression, self-harm, self-medication with drugs and alcohol, and, in extreme circumstances, suicidal ideation, or behaviors (Kodish et al., Reference Kodish, Herres, Shearer, Atte, Fein and Diamond2016). On the other hand, the school context can also serve as a protective zone for children, with certain contextual factors that increase positive behavioral health outcomes in children. For example, children experiencing problems in their home environment sometimes report that school is a respite from the violence occurring in other contexts of their life (Haight et al., Reference Haight, Kayama, Kincaid, Evans and Kim2013). Within school, having positive relationships with peers at school, feeling safe, and feeling connected are all associated with lower levels of depression, anxiety, aggression, and substance use (Bond et al., Reference Bond, Butler, Thomas, Carlin, Glover, Bowes and Patton2007).
Developmental differences
The developmental psychopathology perspective posits that the timing of experiences critically influences an individual’s developmental outcomes, and that similar experiences can have different meaning and impact on the individual’s outcomes depending on the developmental timing of such experiences (Rutter & Sroufe, Reference Rutter and Sroufe2000; Sroufe & Rutter, Reference Sroufe and Rutter1984; Toth & Cicchetti, Reference Toth and Cicchetti2013). Thus, developmental psychopathology emphasizes examining people’s experiences and considers evolving contexts across the social ecology, using longitudinal data to fully understand their developmental pathways and outcomes over time. Similarly, the life course perspective suggests that early life experiences and changing environmental contexts shape one’s developmental outcomes (Sroufe & Rutter, Reference Sroufe and Rutter1984). Together, these theories underscore the importance of using a developmental lens and longitudinal study design to understand a child’s developmental pathways and outcomes. Examining the influences of contextual factors (i.e., family-, neighborhood-, school- level factors) using a developmental lens to is vital to elucidating potential intervention points by identifying critical periods in child development when specific contextual factors strongly influence children’s behavioral health.
The present study
Despite increasing attention and emphasis on the multilevel contexts (e.g., family, neighborhood, school) of child behavioral health outcomes, surprisingly little research has examined the relative importance of such contextual factors at different stages of child development. The existing empirical evidence is mixed and inconclusive: some studies suggest a decreasing influence of family and neighborhood factors during adolescence versus early childhood (Jakes & DeBord, Reference Jakes and DeBord2010; Vartanian & Buck, Reference Vartanian and Buck2005), while others suggest increasing impact of neighborhood factors on youth outcomes during adolescence compared to childhood (Wodtke et al., Reference Wodtke, Elwert and Harding2016); others find no clear differences or changes in the magnitude of family, school, and neighborhood influences on child outcomes across different developmental stages (Leventhal, Reference Leventhal2018; Fleming et al., Reference Fleming, Catalano, Haggerty and Abbott2010). Additionally, it is unclear to what extent the effects of early contextual factors persist to influence behavioral health outcomes at subsequent developmental stages throughout childhood. In an effort to fill such gaps, we examined the effects of several contexts –– including family (i.e., child physical abuse, emotional abuse, maternal depression, maternal substance use), neighborhood (i.e., social cohesion, social control, neighborhood poverty), and school (i.e., school connectedness, peer bullying) –– on child behavioral problems across four developmental stages: early childhood (age 3), young school age (age 5), middle childhood (age 9), and adolescence (age 15). The study focused on two research questions: 1) Are family, neighborhood, and school contexts associated with child behavior problems at each developmental stage? 2) To what extent do family, neighborhood, and school contexts have lasting effects on child behavior problems at subsequent developmental stages?
Methods
Study design and participants
Using data from the Fragile Families and Child Wellbeing (FFCW) study, we conducted a secondary data analysis. FFCW is a longitudinal, birth-cohort study from 20 large urban U.S. cities (Reichman et al., Reference Reichman, Teitler, Garfinkel and McLanahan2001), with an original sample that included 4,898 children. Data were collected at the hospital when the focal child was born, beginning in 1998. Additional data were collected when the children reached ages 1, 3, 5, 9, and 15. For the purposes of the current study, we focus on data from child ages 3 through 15. Of the 4,898 children, the final analytic sample included 1120 children who had no missing data on the predictors. The attrition rates were as follows: age 1 to age 3: 21%, age 3 to age 5: 19%, age 5 to age 9: 23%, age 9 to age 15: 23%. Based on the Little’s MCAR test result (χ2 = 1379.51, p < .001), it was determined that data were not missing completely at random (Li, Reference Li2013). When we compared the analytic sample with the full sample, we found that children in the study sample were more likely to be White or Black, but less likely to be Hispanic; more likely to have mothers with college or more education; and having higher levels of neighborhood social control at ages 9 and 15; great physical abuse at age 3; greater emotional abuse at ages 3–15; higher levels of internalizing problems at age 3 and externalizing problems at age 5. No other significant differences were found between the included and excluded samples. We used the full information maximum likelihood (FIML) method to address missing data on the outcome variables (Enders & Bandalos, Reference Enders and Bandalos2001).
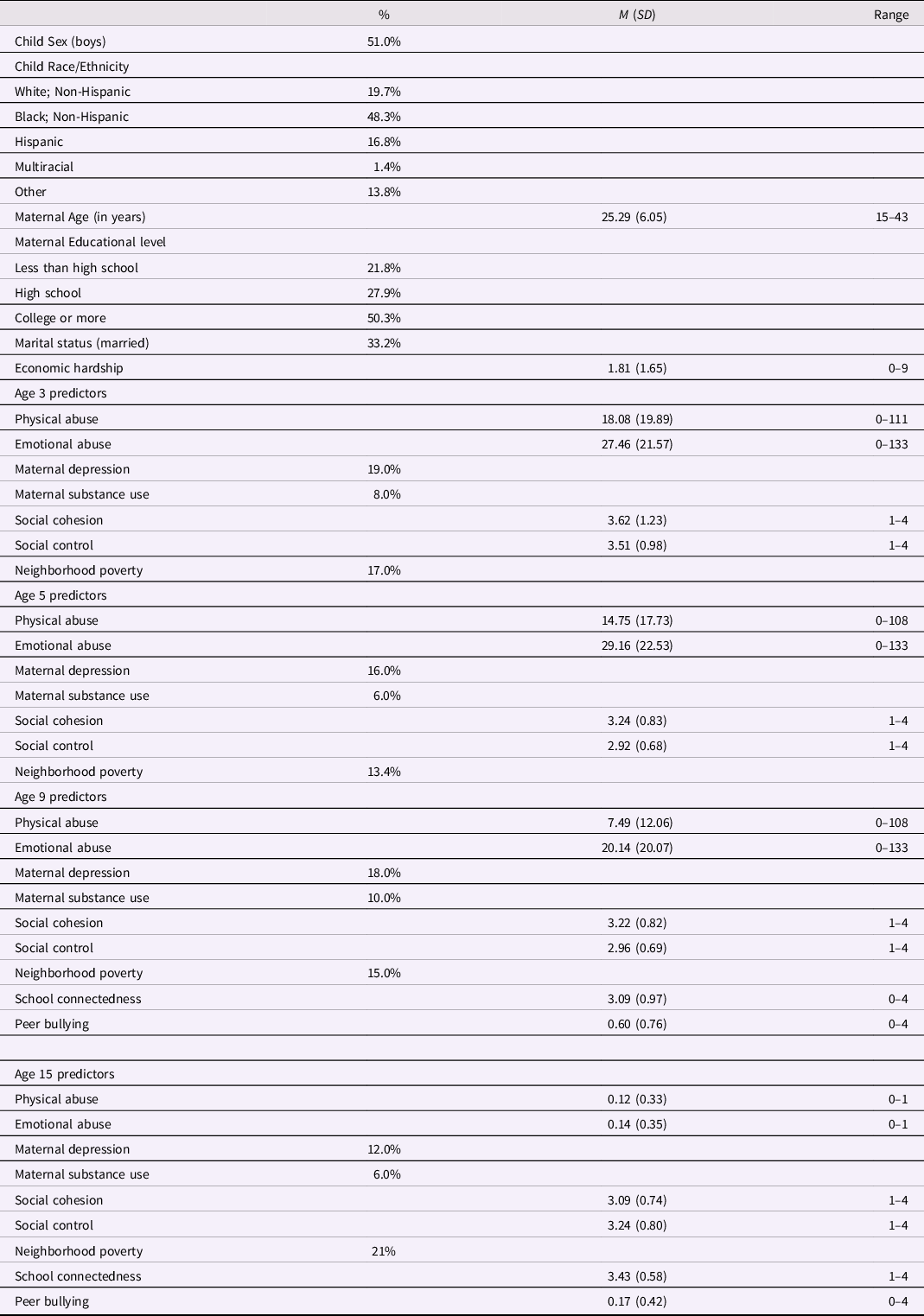
Of the 1,120 children, over half were boys (51.0%). Regarding race/ethnicity, 48.3% were Black/non-Hispanic, 16.8% were Hispanic, 19.7% were White/non-Hispanic, 1.4% were multiracial, and 13.8% were of other races, including American Indian, Asian, and Native Hawaiian/Pacific Islander. The maternal mean age was 25.29 ± 6.05 years (range: 15–43 years). A little over one quarter (27.9%) of the mothers were educated to the high school level, while 50.3% had college or more. Regarding marital status, about 33.2% of the mothers were married. Sample characteristics are presented in Table 1.
Table 1. Sample characteristics and descriptive statistics of key study variables (N = 1120)
Measures
Dependent variables
Child internalizing and externalizing behavior problems were assessed using mother reports on the Child Behavior Checklist (CBCL; Achenbach, Reference Achenbach and Maruish1999) at child ages 3, 5, 9, and 15. The anxious/depressed and withdrawn subscales were combined to proxy internalizing child behavior problems, while the aggressive and destructive subscales were combined to assess externalizing child behavior problems. There were 16 internalizing and 22 externalizing items at age 3 with an inter-item reliability of 0.82 and 0.88, respectively. At child age 5, there were 20 internalizing and 28 externalizing items with an interitem reliability of 0.75 and 0.86, respectively. At child age 9, there were 22 internalizing and 34 externalizing items with an interitem reliability of 0.88 and 0.91, respectively. At age 15, there were 8 internalizing and 20 externalizing items, with an interitem reliability of 0.79 and 0.89, respectively.
Independent variables
Family context. At the family level, we examined parental mental health and substance use issues, as well as two child maltreatment indicators: physical and emotional abuse.
Parental depression was assigned a “1” if the mother met conservative criteria for depression between child ages 1–15, according to the Composite International Diagnostic Interview (Andrews & Peters, Reference Andrews and Peters1998). Parental substance use was assessed with questions relating to maternal alcohol or drug use between child ages 1–15. At child age 1, a mother’s alcohol use was assessed as having five or more drinks in one day at least once in the past month. More data were available at ages 3, 5, 9, and 15. At these ages, maternal problematic alcohol use was assigned a “1” if the mother reported that alcohol use interfered with her ability to work at a job, home, or school at least once in the past year. From child ages 1–15, drug use was assigned a “1” if the mother reported any use of illicit drugs in the past month. Problematic uses of alcohol and illicit drugs were combined into a single dichotomous substance misuse measure.
Items from the Conflict Tactics Scale – Parent Child Version (CTS-PC) (Straus et al., Reference Straus, Hamby, Finkelhor, Moore and Runyan1998) were used to examine physical and emotional child abuse when the focal child was at ages 3–15. The primary caregiver was asked a series of questions about their own behavior as well as the behavior of the other parent, for example “How often in the past year did you slap the child on the hand, arm, or leg?” with frequency response options ranging from “it never happened” to “more than 20 times.” At child ages 3, 5, and 9 there were five physical abuse questions and five emotional abuse questions. In line with recommendations from the scale developer (Straus et al., Reference Straus, Hamby, Finkelhor, Moore and Runyan1998), we assigned the midpoint of the ranges in the following manner: responses of “never” and “not in the past year” were coded as 0; “once” was coded as 1; “twice” was coded as 2; “3-5 times” was coded as 4; “6-10 times” was coded as 8; “11-20 times” was coded as 15; and “20 or more times” was coded as 25. The five questions for each subscale were then added together to create an overall count of the number of times the form of abuse had occurred in the past year. At child age 15, the number of questions was reduced to one physical abuse question and one emotional abuse question, with response options including never, sometimes, and often. We coded never as 0, sometimes as 1, and often as 2.
Neighborhood context. Social cohesion is a component of collective efficacy (Sampson et al., Reference Sampson, Raudenbush and Earls1997) and is intended to measure the relationships between residents of a neighborhood. FFCW included four of the original five items across ages 3, 5, 9, and 15. One item, “People in this neighborhood can be trusted,” was used at age 3, but not in later waves. For consistency, we included only the four items that are consistent across waves. The questions were measured on a Likert scale with the following response options: “strongly agree,” “somewhat agree,” “neither agree nor disagree,” “somewhat disagree,” and “strongly disagree.” The mean was taken for the entire scale at each timepoint, and Cronbach’s alpha for the scale ranged from 0.76 to 0.81, indicating a high degree of interitem reliability.
The second component of collective efficacy is informal social control (Sampson et al., Reference Sampson, Raudenbush and Earls1997). Informal social control is a measure of a resident’s belief that their neighbors would intervene on behalf of the collective good. An example item from this scale is “How likely would your neighbors be to intervene if children were spray painting graffiti on a local building?” At child ages 3, 5, 9, and 15, five items were included with the following response options: “very likely,” “somewhat likely,” “neither likely nor unlikely,” “somewhat unlikely,” and “very unlikely.” The mean was taken for the entire scale at each timepoint, and the Cronbach’s alpha for the scale ranged from 0.81 to 0.88, indicating a high degree of interitem reliability.
Neighborhood poverty rate was measured continuously at the census tract level. The measure indicates the percentage of the census tract that had incomes below the federal poverty level at each of the four waves.
School context. The Child Development Supplement III from the Panel Study of Income Dynamics (The Institute for Social Research, 2012) was used to examine school connectedness when children were ages 9 and 15. This instrument assesses several aspects of connectedness including safety at school, closeness, happiness, and inclusiveness. An example question is “How often did you feel like you were part of your school?” Four questions were asked on a Likert scale, ranging from “Not once in the past month,” to “every day.” The interitem reliability for the scale was 0.70 at age 9 and 0.73 at age 15.
The same supplement was used to assess peer bullying experiences. An example question is “How often have the kids in your school or neighborhood taken things, like your lunch, without asking?” It includes four items assessed on a Likert scale with the following response options: “not once in the past month,” “1–2 times in the past month,” “once a week,” “several times per week,” and “every day.” Cronbach’s alpha for the scale was 0.67 at age 9 and 0.62 at age 15.
Control variables
To isolate the impact of our relationships of interest, we included a variety of control variables that were related to child behavioral problems. These included maternal education and age, child sex and race, and economic hardship. Maternal education was a dichotomous variable indicating whether the mother had a high school degree (or equivalent) or more compared to less than a high school education. Maternal age was included continuously in years. Child sex was included as a dichotomous variable, with a “1” indicating a male child and a “0” indicating a female child. A series of dummy variables were included to indicate whether the child was White, Black, Hispanic, some other race, or multi-racial. In analyses, White was included as the comparison group. Economic hardship was measured as a count of hardships experienced within the past year, e.g., “In the past 12 months, was there anyone in your household who needed to see a doctor or go to the hospital but couldn't go because of the cost?” This measure is a subset of items taken from the Survey of Income and Program Participation (Census Bureau, n.d.).
Data analysis
SPSS v. 27 (IBM Corp, 2020) was used to conduct preliminary analyses prior to our primary analyses to check variable distributions, identify any invalid values or influential outliers, and examine bivariate relationships between key study variables. Then, we performed path analysis with time-varying predictors (i.e., physical abuse, emotional abuse, maternal depression, substance use, neighborhood social control, social cohesion, neighborhood poverty, school connectedness, and peer bullying at ages 3, 5, 9, and 15) and time-invariant control variables (i.e., maternal age, maternal education, economic hardship, child sex, child race/ethnicity). Path analysis is a type of structural equation modeling (SEM), which consists of observed variables only, without latent variables, and is commonly used to examine direct or indirect effects. One advantage of path analysis is that it allows for the simultaneous analysis of a complex model, such as the examination of multiple outcomes in a single model (Jeon, Reference Jeon2015).
Within the path analysis framework, we estimated the concurrent associations between the independent variables and outcome variables at each developmental stage (research question 1) by regressing the outcome variables (i.e., internalizing problems, externalizing problems) on family, neighborhood, and school factors. We estimated the direct effects of the contextual variables on outcomes at each time point to assess the extent to which the contextual factors are concurrently related to children’s behavior problems at each age (i.e., ages 3,5, 9, 15). We also specified lagged paths (e.g., regressing age 5 outcomes on age 3 predictors, regressing age 9 outcomes on age 3 and age 5 predictors, etc.,) in our path model to examine the extent to which contextual factors exert lasting effects on child behavior problems at later developmental stages (research question 2). In doing so, we were able to capture the extent to which early contextual factors had enduring impact on child behavior problems over time. For all path analyses, we estimated auto-regressive paths (i.e., variables at t predict the same variables at t + 1) for each outcome to account for the stability of children’s internalizing and externalizing behavior problems. Several model fit indices were considered to evaluate model fit. Models with the comparative fit index (CFI) >.95, the Tucker-Lewis index (TLI) >.95, root mean square error of approximation (RMSEA) <.06, and the standardized root mean square residual (SRMR) <.05 were considered an acceptable fit (Hu & Bentler, Reference Hu and Bentler1999). We used the full information maximum likelihood (FIML) method to address missing data (Enders & Bandalos, Reference Enders and Bandalos2001). We used Mplus v.8.6. (Muthén & Muthén, Reference Muthén and Muthén2017) to perform path analysis.
Results
Concurrent relationships of contextual factors and child behavior problems
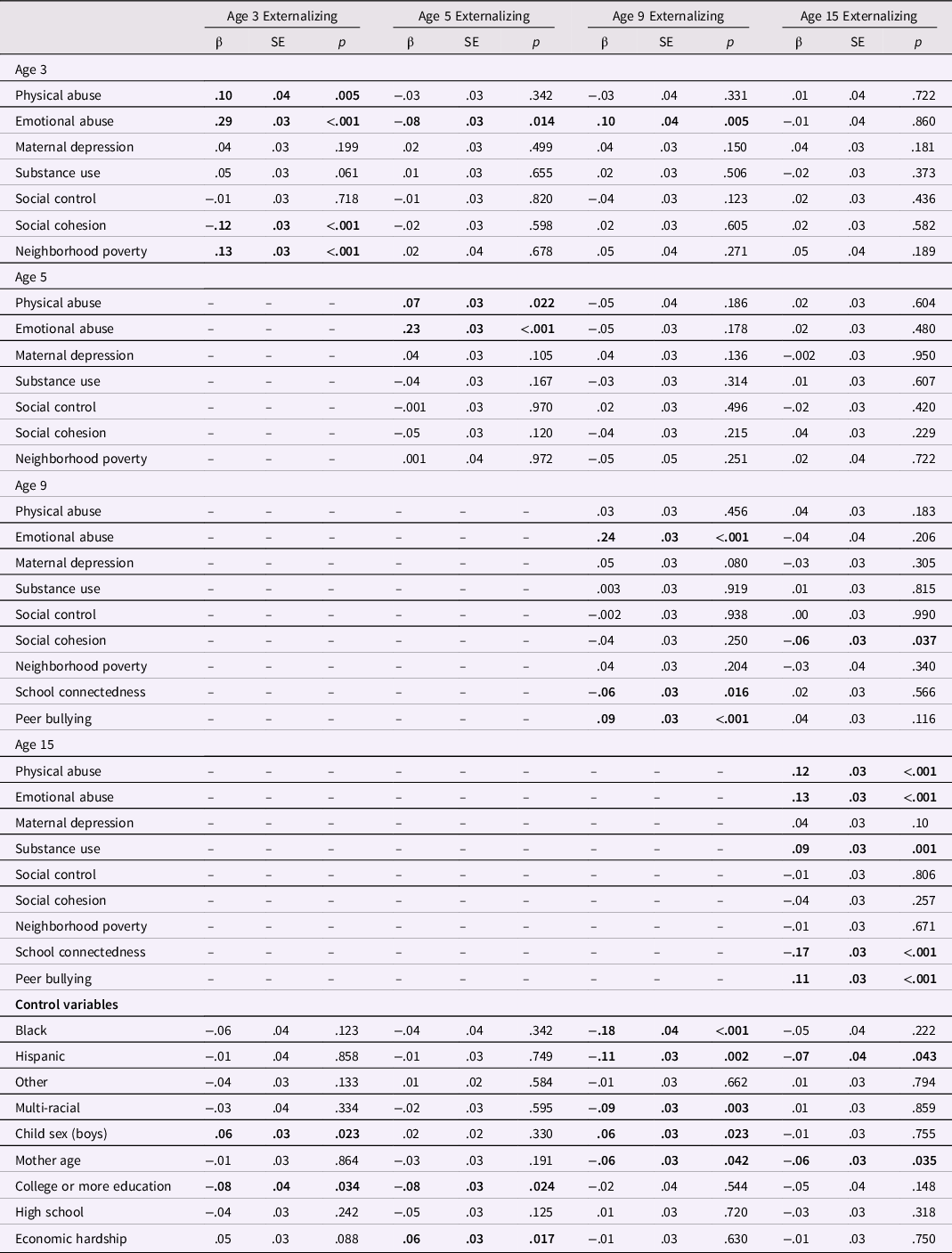
The path model had an acceptable fit to the data: CFI = .97, TLI = .90, RMSEA = .03, 90% CI [.03,.04], SRMR = .03. Tables 2 and 3 present the standardized parameter estimates from the path analysis models, summarizing the results of the concurrent and lagged associations between family, neighborhood, and school contexts and internalizing (Table 2) and externalizing (Table 3) child behavior problems at ages 3, 5, 9, and 15 years. Figure 1 displays the significant concurrent and lagged effects of contextual factors on internalizing and externalizing child behavior problems.
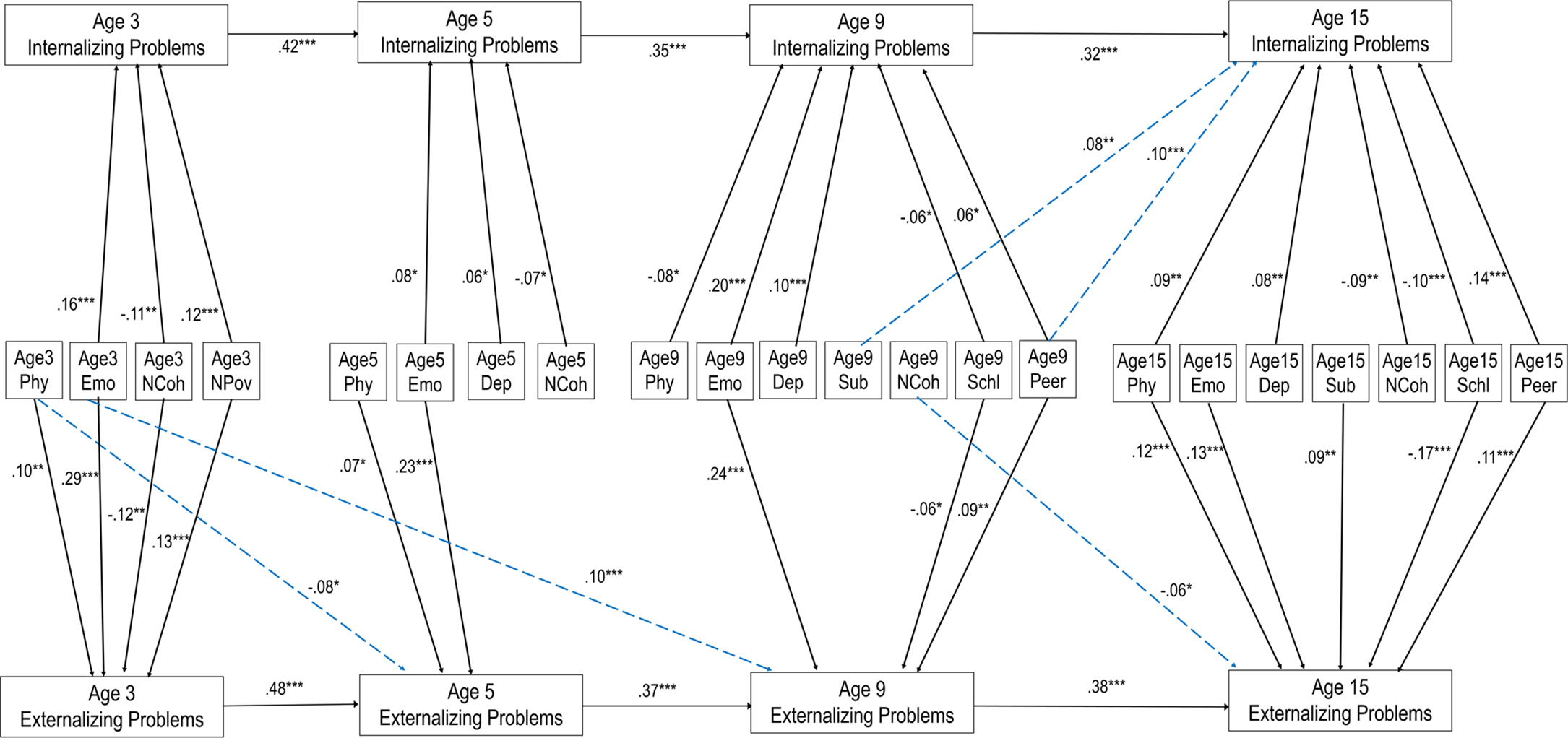
Figure 1. Concurrent and lagged relationships between contextual factors and child internalizing and externalizing behavior problems. Notes. *p < .05, **p < .01, ***p < .001. For clarity, only significant paths are displayed. Standardized parameter estimates are presented. INT = Internalizing behavior problems; EXT = Externalizing behavior problems; Phy=physical abuse; Emo=emotional abuse; Dep=depression; Sub=substance use; NCoh=Neighborhood social cohesion; NPov = Neighborhood Poverty; Schl=school connectedness; Peer=peer bullying.
Table 2. Family, neighborhood, and school contextual predictors of internalizing problems (N = 1120)
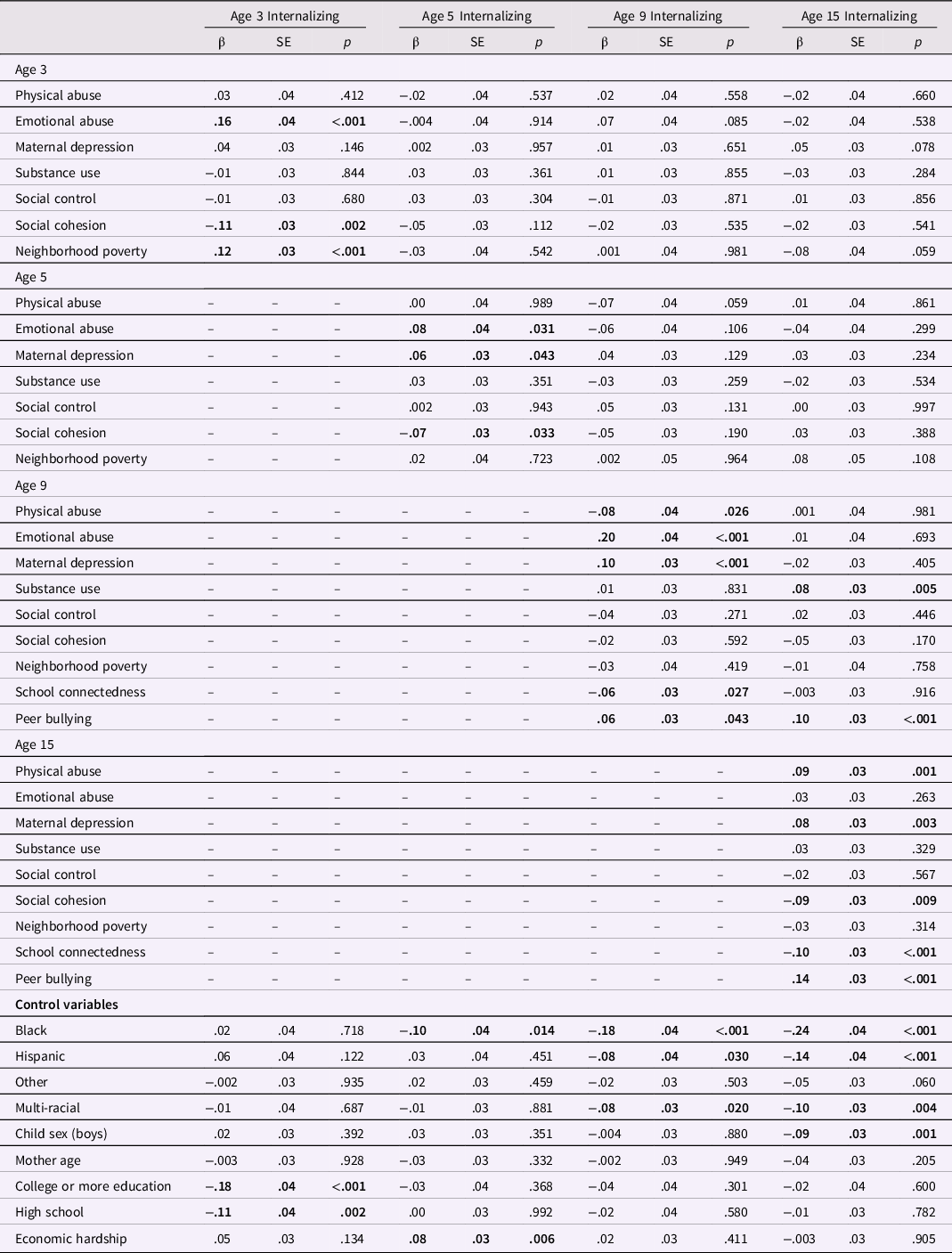
Table 3. Family, neighborhood, and school contextual predictors of externalizing problems (N = 1120)
For internalizing behavior problems (Table 2), at age 3, greater emotional abuse (β =.16, SE = .04, p < .001) and neighborhood poverty (β =.12, SE = .03, p < .001) were related to higher levels of internalizing behavior problems. Conversely, greater social cohesion was associated with lower levels of internalizing (β = −.11, SE = .03, p = .002). At age 5, greater emotional abuse (β = .08, SE = .04, p = .031) and maternal depression (β = .06, SE = .03, p = .043) were associated with higher levels of internalizing behavior problems, while greater social cohesion was associated with lower levels of internalizing behavior problems (β = −.07, SE = .03, p = .033). At age 9, greater emotional abuse (β = .20, SE = .04, p < .001), maternal depression (β =.10, SE = .03, p < .001), and peer bullying (β = .06, SE = .03, p = .043) were associated with higher levels of internalizing behavior problems. Great physical abuse (β = −.08, SE = .04, p = .026) and higher levels of school connectedness (β = −.06, SE = .03, p = .027) were associated with lower levels of internalizing behavior problems. At age 15, greater physical abuse (β = .09, SE = .03, p = .001), maternal depression (β = .08, SE = .03, p = .003), and peer bullying (β =.14, SE = .03, p < .001) were associated with higher levels of internalizing behavior problems. Conversely, higher levels of neighborhood social cohesion (β = −.09, SE = .03, p = .009) and school connectedness (β = −.10, SE = .03, p < .001) were associated with lower levels of internalizing behavior problems.
For externalizing behavior problems (Table 3), at age 3, greater physical abuse (β = .10, SE = .04, p = .005), emotional abuse (β =.29, SE = .03, p < .001), and neighborhood poverty (β = .13, SE = .03, p < .001) were related to higher levels of externalizing behavior problems. Conversely, greater social cohesion was associated with lower levels of externalizing behavior problems (β = −.12, SE = .03, p < .001). At age 5, greater physical abuse (β = .07, SE = .03, p = .022) and emotional abuse (β = .23, SE = .03, p < .001) were associated with higher levels of externalizing behavior problems. At age 9, greater emotional abuse (β = .24, SE = .03, p < .001), and peer bullying (β = .09, SE = .03, p < .001) were associated with higher levels of externalizing behavior problems. Higher levels of school connectedness were associated with lower levels of externalizing behavior problems (β = −.06, SE = .03, p = .016). At age 15, greater physical abuse (β = .12, SE = .03, p < .001), emotional abuse (β = .13, SE = .03, p < .001), maternal substance use (β = .09, SE = .03, p = .001), and peer bullying (β = .11, SE = .03, p < .001) were associated with higher levels of externalizing behavior problems. On the contrary, higher levels of school connectedness predicted lower levels of externalizing behavior problems (β = −.17, SE = .03, p < .001).
Lagged effects of contextual factors on child behavior problems
For internalizing behavior problems, maternal substance use (β = .08, SE = .03, p = .005) and peer bullying (β = .10, SE = .03, p < .001) at age 9 were positively associated with internalizing behavior problems at age 15. For externalizing behavior problems, age 3 physical abuse and emotional abuse predicted externalizing behavior problems at age 5 (β = −.08, SE = .03, p = .014) and age 9 (β = .10, SE = .04, p = .005), respectively. Further, greater social cohesion at age 9 was associated with lower levels of externalizing behavior problems at age 15 (β = −.06, SE = .03, p = .037).
Discussion
This study sought to increase our understanding about the critical contexts that relate to child behavior problems at different developmental stages. By applying a developmental lens, our findings add important new information to the literature on socio-ecological factors associated with child behavioral health outcomes. We found that family-, neighborhood-, and school-level factors all had significant associations with children’s internalizing and externalizing behavior problems. Specifically, child physical abuse, emotional abuse, maternal depression, maternal substance use, social cohesion, neighborhood poverty, school connectedness and peer bullying were significant contextual factors for child behavior problems, but they had differential impact at different developmental periods. Further, several lagged effects were observed, with early abuse experiences (i.e., age 3) and middle childhood contextual factors –– including maternal substance use, neighborhood social cohesion, and peer bullying at age 9 –– having enduring influences on later behavioral outcomes.
At the family level, we examined child physical and emotional abuse, maternal depression, and maternal substance use as a key context for child behavior problems. We found that the family-level risk factors had concurrent associations with higher levels of internalizing and externalizing problems at each time point (ages 3, 5, 9 and 15), though the patterns of significant associations differed by outcomes (i.e., internalizing or externalizing) and age groups. Child emotional abuse was found to be one of the most salient within time predictors of children’s behavioral health outcomes. At each timepoint, child emotional abuse was associated with higher levels of internalizing and externalizing behavior problems, except for age 15 internalizing behavior problems. These findings affirm the past work that indicated child emotional abuse as an influential and pertinent predictor of internalizing (Duprey et al., Reference Duprey, Oshri, Liu, Kogan and Caughy2021) and externalizing (Muniz et al., Reference Muniz, Fox, Miley, Delisi, Cigarran and Birnbaum2019; Silva et al., Reference Silva, Graña and González-Cieza2014) behavior problems. Traditionally, the negative effects of emotional abuse have been less discussed compared to other forms of abuse, such as physical abuse and sexual abuse, yet our findings point to the need for increased awareness of the harmful impact of emotional abuse (Maguire et al., Reference Maguire, Williams, Naughton, Cowley, Tempest, Mann and Kemp2015). Interestingly, child physical abuse was associated with internalizing behavior problems at earlier ages (i.e., ages 3 and 5) and with externalizing behavior problems at later ages (i.e., aged 9 and 15). It may be that for young children, their emotional distress and symptoms associated with physical abuse manifest as externalizing behaviors. Drawing from social learning theory (Bandura & Walters, Reference Bandura and Walters1977), young children who have been exposed to physical violence are likely to model and mimic aggressive and violent behaviors. It is noteworthy that, in addition to the within-time effects, physical abuse and emotional abuse at age 3 had lagged effects on child externalizing behavior problems at age 5 and at age 9, respectively. Surprisingly, age 3 physical abuse was associated with lower levels of externalizing behavior problems at age 5. It may be that children who experienced physical abuse at age 3 received early interventions, such as behavioral health services, which prevented externalizing behavior problems at age 5. More research is needed to untangle the complex associations between different forms of abuse and externalizing behavior problems at different developmental stages.
Another interesting finding was that maternal depression was consistently associated with greater internalizing behavior problems, but not with externalizing behavior problems, at ages 5, 9, and 15. The findings corroborate previous studies that provided empirical support for the intergenerational transmission of depression (Goodman, Reference Goodman2020). While the mechanisms underlying the link between maternal depression and children’s internalizing problems, including depression and anxiety, remain unclear, it might be that maternal depression indirectly affects children’s internalizing symptoms via ineffective parenting (Kuckertz et al., Reference Kuckertz, Mitchell and Wiggins2018), maternal and children’s cognitive vulnerability (Dunning et al., Reference Dunning, McArthur, Abramson and Alloy2021), and children’s difficulties in interpersonal relationships (Gotlib et al., Reference Gotlib, Goodman and Humphreys2020). Finally, maternal substance use had a significant within time association with adolescent externalizing behavior problems at age 15. Considering that externalizing behavior problems during adolescence include substance use and other delinquent behaviors, maternal substance use may be an especially pertinent risk factor at this developmental stage. That is, youths whose mothers use substances may have poorer quality in the parent-child relationship, lower parental monitoring, and easier access to alcohol and drugs at home, all of which are associated with increased risk for adolescent substance use and other risk-taking behaviors (Rusby et al., Reference Rusby, Light, Crowley and Westling2018). It is noteworthy that maternal substance use at child age 9 predicted higher levels of internalizing behavior problems at age 15. Although it is not clear why maternal substance use at age 9 did not have any within-time associations with children’s behavior problems and only a significant lagged effect on internalizing behavior problems at age 15, this finding suggests a delayed or sleeper effect of maternal substance use on child behavior problems, highlighting the importance of ongoing screening and monitoring of internalizing symptoms among children whose mothers have a history of substance use. Overall, these findings are consistent with prior research suggesting a significant link between adverse childhood experience and child behavior problems (Clarkson Freeman, Reference Clarkson Freeman2014; Hunt et al., Reference Hunt, Slack and Berger2017), and highlight family adversity as a robust risk factor for child behavior problems regardless of developmental stage.
At the neighborhood level, social cohesion and neighborhood poverty had significant associations with child behavior problems. Of the two aspects of collective efficacy, social cohesion appears to have a more salient influence on internalizing and externalizing child behavior problems than informal social control does. Social control did not have any immediate or lasting effects on child behavior problems in this study. Conversely, social cohesion had significant inverse associations with child behavior problems across various developmental stages, though differential effects (e.g., concurrent vs. lagged) were observed at different developmental stages. Specifically, social cohesion has significant within-time associations with internalizing child behavior problems at ages 3, 5, and 15 and with externalizing behavior problems at age 3. Our findings corroborate prior research demonstrating the protective effects of social cohesion on child behavior problems (Kingsbury et al., Reference Kingsbury, Kirkbride, McMartin, Wickham, Weeks and Colman2015; Ma & Klein, Reference Ma and Klein2018; Mrug and Windle, Reference Mrug and Windle2009). A strong sense of connectedness/trust and bond among members of the community may serve as a protective factor for internalizing and externalizing child behavior problems through various pathways, such as better parental well-being, higher quality parenting (e.g., less child maltreatment), or reduced neighborhood violence (Maguire-Jack & Showalter, Reference Maguire-Jack and Showalter2016; McCloskey & Pei, Reference McCloskey and Pei2019; Pei et al., Reference Pei, Yoon, Maguire-Jack and Lee2022; Sampson et al., Reference Sampson, Raudenbush and Earls1997). The null finding of the within-time associations between social cohesion and behavior problems at age 9 may be explained by the fact that children at this developmental stage (middle childhood) spend the bulk of their time at school. As such, the effects of the neighborhood contexts may decrease while the effects of the school contexts are maximized during this period.
Notably, in addition to the concurrent relationships, social cohesion showed longitudinal relationships with child behavior problems. Social cohesion at age 9 was associated with lower levels of externalizing problems at age 15. This longitudinal finding is in line with prior studies that found long-term associations between social cohesion in earlier developmental stages and child outcomes at later developmental stages (Kingsbury et al., Reference Kingsbury, Kirkbride, McMartin, Wickham, Weeks and Colman2015; Newbury et al., Reference Newbury, Arseneault, Caspi, Moffitt, Odgers and Fisher2016), and highlights the lasting protective effects of social cohesion on child behavioral health outcomes. While the current study found that age 9 social cohesion was protective against externalizing behavior problems at age 15, there was no significant concurrent association at age 9. The age 15 externalizing measure includes certain behaviors that are considered delinquent acts, which may be a key behavior affected by neighborhood-level factors because of exposure to crime and the delinquency of peers and young adults within the neighborhood. Such behaviors may not appear until later adolescence when youth are more likely to engage in delinquent and rebellious behaviors.
Neighborhood poverty is another key neighborhood factor that appears to play a crucial role in early childhood (age 3). Neighborhood poverty during this developmental stage had cross-sectional associations with both internalizing and externalizing behavior problems. In other words, greater neighborhood poverty at age 3 was associated with higher levels of internalizing and externalizing behavior problems at age 3. Our findings corroborate a robust body of research suggesting neighborhood poverty as a risk factor for child behavior problems (Church et al., Reference Church, Jaggers and Taylor2012; Kim et al., Reference Kim, Lee, Jung, Jaime and Cubbin2019; Xue et al., Reference Xue, Leventhal, Brooks-Gunn and Earls2005). Children living in a neighborhood with high poverty rates may be exposed to unsafe neighborhood environments, such as community violence, which may affect children’s behavioral health outcomes both directly (e.g., increased anxiety, learned aggressive behavior) and indirectly via increased parenting stress and decreased parenting quality (Mrug & Windle, Reference Mrug and Windle2009; Wang et al., Reference Wang, Choi and Shin2020). The neighborhood context may be particularly impactful in early childhood due to limited interaction of children in other contexts. Prior to entering school, children’s ecological context is limited to their immediate surroundings, including their family and neighborhood. Their interactions occur primarily within these two contexts, and individuals within their circles are likely to come from these two contexts. Additionally, the early years of a child’s life are critical for children’s behavioral functioning. From the period of birth to age 3, children’s brains grow faster than at any other time, with the brain doubling in size by age 1 and reaching about 80% of its adult volume by age 3 (Gilmore et al., Reference Gilmore, Lin, Prastawa, Looney, Vetsa, Knickmeyer and Gerig2007; Nowakowski, Reference Nowakowski2006; Rakic, Reference Rakic2006). If children witness violence and disruption within their immediate neighborhood context when they are very young, they may not have an outside context to help them make sense of it. These early experiences may then have lasting impacts on the child. Children may perceive the outside world as unsafe and consequently act out (externalizing) or retreat from the environment (internalizing). In addition to violence and safety concerns, neighborhoods with high rates of poverty may also lack resources and infrastructure to provide a rich environment for the child, such as green spaces, social services, and libraries. Due to the lack of resources, children in disadvantaged neighborhoods may be unable to meet their needs related to physical activity, food and nutritional security, and education.
In addition to the family and neighborhood contexts, the school context played an important role in explaining child behavior problems during middle childhood and adolescence. School connectedness and peer bullying had significant concurrent associations with both internalizing and externalizing behavior problems at ages 9 and 15. As children get older and spend significant amounts of time in school, school environments become a prime setting for their behavioral development and well-being. Our findings support previous results that indicate peer bullying is a significant threat to child behavioral well-being, while school connectedness is a protective factor associated with positive behavioral health outcomes (Arslan, Reference Arslan2021; Rijlaarsdam et al., Reference Rijlaarsdam, Cecil, Buil, Van Lier and Barker2021; Shochet et al., Reference Shochet, Dadds, Ham and Montague2006).
We also found evidence for the lasting impact of the school context on child behavioral problems. Specifically, peer bullying at age 9 was associated with higher levels of internalizing behavior problems at age 15. Peer bullying during middle childhood may have long-lasting detrimental effects on internalizing child behavior problems due to developmental cascades of peer bullying/victimization and behavior problems, whereby these two domains interact with each other, producing reciprocal relations and cumulative consequences (Vaillancourt et al., Reference Vaillancourt, Brittain, McDougall and Duku2013). The findings regarding peer bullying should be interpreted with caution though, given that the peer bullying scale had poor internal consistency reliability in this study.
In addition to the environmental contexts, several demographic characteristics were found to play important roles in determining child behavior problems at different developmental stages. At ages 3 and 9, boys showed higher levels of externalizing behavior problems whereas girls showed higher levels of internalizing behavior problems at age 15. These findings are generally in line with prior work that found higher levels of externalizing symptoms in boys and higher levels of internalizing symptoms in girls (Ara, Reference Ara2016). Regarding children’s race, Black, Hispanic, and multi-racial children tended to show lower levels of internalizing and externalizing behavior problems at ages 9 and 15, compared to White children. Prior research on racial/ethnic differences in internalizing and externalizing behavior problems has been inconsistent. Some studies found higher levels of behavior problems in children of color (e.g., McLaughlin et al., Reference McLaughlin, Hilt and Nolen-Hoeksema2007: Hispanic girls experiencing higher levels of internalizing symptoms; López et al., Reference López, Andrews, Chisolm, de Arellano, Saunders and Kilpatrick2017; Thyberg & Lombardi, Reference Thyberg and Lombardi2022: Black children experiencing more externalizing symptoms) while others found higher levels of internalizing symptoms in White children (Elkins, Reference Elkins2018) or reported no racial/ethnic differences (Formoso et al., Reference Formoso, Gonzales and Aiken2000; Godinet et al., Reference Godinet, Li and Berg2014). The discrepancies in findings may be due to differences in sample characteristics (e.g., age), measures, and informants (e.g., caregivers, youths, teachers). However, further investigation is warranted to fully understand the role of race/ethnicity in internalizing and externalizing behavior problems throughout childhood and adolescence. Higher maternal education was associated with lower levels of internalizing and externalizing behavior problems when children were younger (e.g., ages 3 and 5). These findings affirm Meyrose et al.’s (Reference Meyrose, Klasen, Otto, Gniewosz, Lampert and Ravens-Sieberer2018) findings that the effects of maternal education on children’s behavior problems decrease as children age. Similarly, economic hardship was significantly associated with greater internalizing and externalizing behavior problems when children were 5 years old, but they had no significant associations with behavior problems at later developmental stages (e.g., ages 9 and 15).
Limitations
As with all empirical research, this study had various limitations that should be considered when drawing from these findings. First, the study sample is comprised of children and adolescents from urban cities. Thus, the generalizability of the findings is limited to similar populations. Additionally, since we used a secondary dataset and could not dictate which measures were used during data collection, some measures had slight item differences at time points. Specifically, the number of items used to measure physical abuse and emotional abuse was reduced at age 15 because some items were no longer developmentally relevant (e.g. “shaking a child” is a much more serious act on a young child compared to a teenager) and were dropped at age 15. While overall, the differences between measures at each wave were relatively small and the findings indicate that both physical abuse and emotional abuse at age 15 still showed significant effects on the outcomes despite the reduction in the number of items, it is possible that the differences in abuse measures at age 15 had an unknown effect on our results. Another measurement issue was that the peer bullying scale showed poor internal consistencies (Cronbach’s alpha values .67 at age 9, .62 at age 15). The peer bullying findings from the current study should be further examined and validated in future research using a more robust and reliable bullying measurement. Further, school context data were not available for younger children (i.e., ages 3 and 5); thus we could not test the relative influence of early school contexts, such as preschool and daycare, on behavior problems during early years or over time. Given some of the other known benefits of preschool involvement on later outcomes, future research endeavors may consider further exploring this area. Finally, we did not examine the interaction effects between contextual factors on child behavioral health as this was beyond the scope of our study. However, considering that context factors will likely influence each other and work together to affect children’s behavioral health, future research should test interactions between predictors nested within a broader social ecological framework.
Implications
The results of the study underscore the need for child behavioral health policies to consider multilevel contexts across the social ecology (i.e., family, neighborhood, school) in interrupting the adverse pathways that can create barriers to healthy development and lead to externalizing and internalizing behavior problems. For example, based on our findings that highlighted greater social cohesion and lower neighborhood poverty rates as key community-level protective factors for child behavior problems, it would be advantageous for policies and programs aimed at fostering positive child behavioral health to allocate more funds to increase neighborhood connection and resources.
Results from this study can also be applied to direct practice with children. Child physical abuse and emotional abuse were directly correlated with internalizing and externalizing behaviors at each developmental stage with varying influences. These findings highlight the crucial need for the early detection of child abuse as a mediating intervention for maladaptive child behavior and coping. Primary care providers and other healthcare professionals may be uniquely positioned to provide enhanced screenings for child abuse and identify a high-risk group of children to prompt further action and referrals for preventive services. Further, given that maternal depression was identified as a salient risk factor for child internalizing behavior problems, practitioners working with children with internalizing symptoms may benefit from collaborating with other programs/organizations to screen for maternal depression and provide support for mothers in need of mental health services
Finally, this study also provides practical applications for targeting specific populations, developmental timing, and settings. Based on our findings, school-based bullying prevention programs and interventions that increase students’ sense of connectedness to school may serve as a level of protection during middle childhood and adolescence. Further, as our results indicate that peer bullying during middle childhood has lasting effects on youth internalizing behavior problems, targeting this age group specifically may serve as a preventive method. Additionally, like health care providers, schools are uniquely positioned to create effective behavior changes in youths. Professionals within schools, including teachers, guidance counselors, and other school-affiliated staff members, may benefit from trauma-informed training to understand how traumatic experiences (e.g., child abuse, maternal depression and substance use, peer bullying) influence behavioral health outcomes, and how trauma-informed practices can be used to provide more effective guidance and support to their students.
Funding statement
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.







