The eradication of hunger, achieving food security and promoting adequate nutrition, is the ultimate aim of the Sustainable Development Goal 2, yet it remains a major challenge worldwide(1). Since 1996, food security is declared a human right and ‘exists when all people, at all times, have physical and economic access to sufficient, safe and nutritious food to meet their dietary needs and food preferences for an active and healthy life’(2). Food insecurity (FI) and malnutrition continue to affect hundreds of million people and may be both a cause and a consequence of conflicts and protracted crises(3–5). While hunger may be associated with severe FI, moderate FI reflects uncertainties about the ability to obtain food and may compromise diet quality and diversity(6,Reference Ghattas7) .
Food-coping strategies may be employed to decrease food consumption in the face of emerging shortfalls(8). Households may resort to rationing strategies such as reducing the number of meals, limiting portion sizes, restricting consumption by adults in favour of children or even skipping entire days without eating. Other strategies involve dietary changes such as eating fewer kinds of food groups and relying on less preferred or inexpensive foods(Reference Maxwell and Caldwell9). As households and individuals may attempt to cope with household FI, women may be particularly consuming a more monotonous diet and be exposed to a higher risk of malnutrition due to the maternal buffering to feed children first, their roles within households and sex inequalities within societies. Intra-household differences in food allocation and choices may be masked by the measure of FI at the household level, indicating a need to assess at the individual level(Reference Ghattas7). In fact, the perception of the concept of ‘being out of food’ is different between men and women. While men tend to interpret it as not being able to feed the family, women associate it more with a monotonous diet(Reference Ballard, Kepple and Cafiero10).
Poor dietary diversity has an exacerbating effect on the nutritional status of children and women of reproductive age, particularly pregnant mother (PM) and lactating mother (LM)(6,11) . Proper nutrition during the first 1000 d, since conception to the child’s second birthday, lays the foundations for optimal growth and healthy life for more than just a generation(Reference Langley-Evans12–Reference Christian and Stewart14). Paradoxically, undernutrition and overweight can both emerge from FI and poverty(Reference Ghattas7). This paradox exists due to the compromise in the diet quality by consuming foods with higher energy density, often less expensive, rather than foods with higher nutrient density, which contributes to nutrient inadequacies and excessive energy intake(Reference Tanumihardjo, Anderson and Kaufer-Horwitz15,Reference Drewnowski16) . Furthermore, FI and depression have been previously linked in many contexts(Reference Sparling, Waid and Wendt17). Feelings of deprivation, anxiety and poor mental health may emerge due to the struggle to provide food regularly in the context of poverty(Reference Ghattas7,Reference Emerson, Tol and Caulfield18) . Poor maternal mental health may ultimately have a negative effect on caregiving and the child’s development, especially in low socio-economic contexts(Reference Stein, Malmberg and Sylva19–Reference Woldetensay, Belachew and Ghosh21).
More than a decade ago, the Arab Spring surged in the Middle East and North Africa region with poverty and FI being the main drivers and outcomes of the protests and wars that followed(Reference Breisinger, Ecker and Al-Riffai22,Reference Żuber and Moussa23) . The Syrian war, a protracted conflict that is currently in its eleventh year, remains one of the major challenges of the twenty-first century, with more than 5·5 million refugees still residing in neighbouring countries, including Lebanon, Turkey, Jordan, Egypt and Iraq(Reference Żuber and Moussa23,24) . Lebanon hosts more than 1·5 million Syrians and remains the country with the highest refugee per capita concentration worldwide(25). Despite large-scale assistance programmes, about half of the Syrian refugee households in Lebanon were living in extreme poverty in 2018 and 2019. They continue to face tremendous challenges that affect their FI status and increase vulnerabilities associated with their legal status, restricted mobility, access to services and limited employment opportunities(26). With few informal settlements in Greater Beirut, the vast majority of Syrian refugees are living in rented accommodation(27) and are suffering from high costs of living, household debts and dependency on food assistance (e-vouchers). Recent findings among Syrian refugee mothers in Greater Beirut showed that high levels of overweight and obesity coexist with anaemia, in addition to poor maternal diet and nutritional inadequacies(Reference Abou-Rizk, Jeremias and Nasreddine28).
Despite numerous surveys conducted annually by the UN High Commission on Refugees (UNHCR) and the World Food Programme (WFP) on the household level of FI and food consumption among Syrian refugees in Lebanon(25), limited data explore FI at the individual level and dietary diversity among female refugees in urban settings of a humanitarian crisis. The present study aims to: (1) assess the prevalence of FI, maternal low dietary diversity (LDD) and poor mental health of Syrian refugee mothers of children under 5 years, (2) explore the associations between dietary diversity, FI, mental health, anaemia and nutritional status of mothers and (3) examine the consumption food groups according to household monthly income among Syrian refugee mothers in Greater Beirut following years into the crisis.
Methods
Study design and sampling method
A cross-sectional survey was carried out in July–September 2018 among Syrian refugee mothers with at least one child below 5 years living in vulnerable areas of Greater Beirut, Lebanon. A two-step purposeful sampling was used to select primary healthcare centres (PHCC) in localities in Greater Beirut with the highest vulnerability level(29), which included Baouchriyeh, Bourj Barajneh, Bourj Hammoud, Chiyah, Mazraa and Mousaytbeh. Greater Beirut is considered to be the melting pot of the country; therefore, the catchment area of PHCC in Greater Beirut covers the capital city Beirut and adjacent urban surroundings of Mount Lebanon Governorate(30). Inclusion criteria included women of reproductive age (15–49 years) from Syrian households with at least one child (0–59 months) that is not suffering from any inborn errors of metabolism or physical malformations. Mother–child dyads were identified through three approaches, via: (1) the nurses at PHCC, (2) direct contact by the research assistant in the waiting rooms and (3) flyers with a brief description of the study made available in PHCC locations. A detailed methodology of this survey has been described elsewhere(Reference Abou-Rizk, Jeremias and Nasreddine28).
The present study is part of a larger cross-sectional survey among Syrian refugee mothers and their children under 5 years in Greater Beirut that explored anaemia as one of the key outcomes. Sample size calculations were based on previous estimates of anaemia of 26·1 % among Syrian refugee women in Lebanon(31). A minimum of 296 participants were needed to provide a power of 80 % and a margin of error of 5 % at 95 % CI. Accounting for a study design effect of 1·5, non-response rate of 15 % and dropout rate of 10 %, we aimed for a sample size of 555 mothers. Out of the 665 women approached, 590 mothers with at least one child under the age of 5 years from Syrian households were eligible and 489 mothers (82·9 %) consented to participate in the survey. A total of 433 mothers (88·6 %) completed the interview and were included in the present study.
Ethical approval and consent to participate
The original study was approved by the Institutional Review Board for Social and Behavioral studies at the American University of Beirut in Lebanon (IRB ID: SBS-2017-0294) and the Freiburg Ethics Commission International in Germany (FEKI code: 017/1434). The Primary Health Care (PHC) Department at the Ministry of Public Health (MoPH) granted with an approval letter access to PHCC in Greater Beirut, which is part of the National PHC Network overseen by the MoPH. Directors of PHCC selected for the survey also granted approval letters prior accessing their premises. Consent forms and questionnaires written in North Levantine Arabic dialect were used. Written informed consent was obtained prior enrolment in the study, and a copy of the consent form was given to each participant. A parental consent and an informed assent were sought from mothers aged below 18 years. In case of illiteracy, a witness or the nurse on duty signed on the behalf of the participant after reading and explaining the consent form. Confidentiality and voluntary participation were assured by the data collectors by assigning random identifiers and allowing access to the data only to the investigators.
Data collection
A culture-specific multi-component questionnaire was carried out during face-to-face interviews by Collaborative Institutional Training Initiative certified and well-trained enumerators. Data quality control was performed on a regular basis to ensure an increased accuracy of data and to limit risks of reporting bias. Data on socio-economic and household characteristics such as parents’ education level and employment status, household monthly income, size of the household, registration with the UNHCR as refugees, receiving food assistance (e-vouchers) from the WFP and healthcare services utilisation were collected. Mental health status of mothers was assessed using the Patient Health Questionnaire-9 to measure depression(Reference Kroenke, Spitzer and Williams32), validated among Lebanese adults(Reference Sawaya, Atoui and Hamadeh33) and the Arabic version of the Mini International Neuropsychiatric Interview (MINI) to measure post-traumatic stress disorder (PTSD)(Reference Kadri, Agoub and El Gnaoui34). Crowding index was defined as the total number of co-residents per household divided by the number of rooms, excluding kitchens, bathrooms, hallways, balconies and garage(35). The income group classification was based on the legal minimum wage in Lebanon, approximately equal to 675 000 LBP (450 USD in 2018)(36). Therefore, low-income household was defined as ≤ 750·000 LBP and high-income household as > 750·000 LBP (500 USD in 2018).
FI was measured at the individual level for the mother using the global Food Insecurity Experience Scale. The prevalence of moderate and severe FI in the total study population represents the Sustainable Development Goal indicator 2.1.2. The Food Insecurity Experience Scale generates two indicators, the FI prevalence rates at the moderate and severe level and at the severe level only, by computing the probability of being food insecure for each individual(37). The probability of belonging to a food security class was extracted to be used in the analysis as such: probability of being moderately and severely food insecure and probability of being severely food insecure. Food Insecurity Experience Scale was internally validated using statistical methods based on the Rasch measurement model. The development of the score and validation process is published elsewhere(38,Reference Cafiero, Viviani and Nord39) .
Anthropometric and biochemical assessment
Mid-upper arm, waist and hip circumference were measured among mothers with light clothing using a non-elastic measuring tape (SECA 201). An average of two measurements was recorded to the nearest decimal using standardised protocols(40). The classification of malnutrition using the mid-upper arm circumference was applied for all mothers as follows: < 23·0 cm for undernourished, 23·0–27·9 cm for normal weight and ≥ 28·0 cm for overweight and obese mothers(Reference Fakier, Petro and Fawcus41–44). For non-PM, the BMI was computed as the weight (kg) divided by the height squared (m2). BMI classification was categorised into two groups ‘Underweight’ (BMI < 18·5 kg/m2), ‘Normal weight’ (BMI 18·5–24·9 kg/m2) and ‘Overweight/Obese’ (BMI ≥ 25·0 kg/m2)(45). Hb concentrations were measured using the ‘HemoCue Hb301 System’ by certified phlebotomists. The accuracy of the measurement was routinely ensured with the use of control solutions. A small drop of blood was collected by conducting a finger prick on mothers. Anaemia cut-offs were defined using the WHO criteria. Total anaemia was set at Hb < 12·0 g/dl for non-pregnant non-lactating and LM and at Hb < 11·0 g/dl for PM at sea level(46).
Dietary assessment
Data were collected on the characteristics of daily meal patterns and the dietary intake of the mother using two dietary assessment methods: (1) a 24-h dietary recall during the previous day and (2) a FFQ during the past 12 months. The 24-h dietary recall was used for the assessment of maternal dietary diversity and nutrient inadequacies, whereas the FFQ method was used to assess the percentage contribution of food groups to total energy consumption. Both dietary assessment methods were conducted by trained nutritionists using the 2D food portion visual(Reference Millen and Morgan47) and standardised reference portions to facilitate the collection of dietary data and ensure standardisation. The five-step multiple-pass 24-h dietary recall method was used to assess the dietary intake during the previous day, which included the following steps: (1) start with a quick uninterrupted listing of foods by the interviewee, (2) probe for forgotten foods list, (3) collect the time and occasion, (4) gather a comprehensive description of foods and amounts eaten in the detailed cycle and (5) end with a final probe review(Reference Conway, Ingwersen and Moshfegh48,Reference Johnson49) . Furthermore, a ninety-four-item semi-quantitative context-specific FFQ, validated among adults in Lebanon(Reference El Sayed Ahmad, Baroudi and Shatila50), was used to assess the dietary intake of mothers over the past 12 months. Dietary data stemming from the FFQ were combined into numerous food groups and subgroups in order to examine their contribution to the percentage energy intake (% EI). Dietary data were analysed using the United States Department of Agriculture (USDA) database (SR 28, version: May 2016) which was complemented with single food items from local food composition tables available for specific Lebanese foods, given the similarities between Eastern Mediterranean cuisines(Reference Pellett and Shadarevian51,Reference Issa, Alghanim and Obeid52) . Standardised recipes were added to analyse composite and traditional Lebanese and Syrian dishes. NutriSurvey 2007 software was used for the analysis of macro- and micronutrients’ intake from the 24-h recalls(Reference Erhardt53).
Minimum Dietary Diversity for Women of reproductive age
Based on the 24-h dietary recalls, maternal dietary diversity was assessed using the Minimum Dietary Diversity for Women (MDD-W) of reproductive age. Food items were aggregated into sixteen food groups as follows: (1) grains, white roots and tubers, (2) pulses (beans, peas and lentils), (3) nuts and seeds, (4) dairy products, (5) meat, poultry and fish, (6) eggs, (7) dark green leafy vegetables, (8) other vitamin A-rich fruits and vegetables, (9) other vegetables, (10) other fruits, (11) other oils and fats, (12) fried and salty foods, (13) sweet foods, (14) sugar-sweetened beverages, (15) condiments and seasonings and (16) other beverages and foods. Food items consumed in very small quantities (<15 g) were placed in the ‘Condiments and seasonings’ category. Sweetened coffees, teas and milk were placed in the ‘Sweetened beverages’ category. Mixed and traditional dishes (e.g. stews, soups, vegetable dishes, sandwiches) were carefully evaluated to classify main ingredients consumed in large quantities in their respective food groups and minor ingredients to other groups such as groups 11 and/or 15. Composite dishes and food items (e.g. bread, pizza, porridge, fried savoury, sweets and pastries, sweet drinks) were assigned to a single food group based on the major ingredient. Food group diversity score was computed by summing up the first ten MDD-W food groups consumed yesterday into a score ranging from 0 to 10. The MDD-W indicator defined achieving MDD-W as a food group diversity score ranging from 5 to 10 and LDD as not achieving MDD (< 5 food groups yesterday)(11).
Nutrient inadequacies
Nutrient intakes stemming from the 24-h dietary recalls were used to assess the prevalence of inadequate intakes by comparing the intakes of a nutrient to the estimated average requirements (EAR) according to the Institute of Medicine. The EAR is the average daily nutrient intake level estimated to meet the requirements of half of the mothers according to their age and reproductive status groups (pregnant, lactating or non-pregnant non-lactating). The adequate intake was used in the absence of an EAR, as for dietary fibres(54). The analysed micronutrients represent those for which the MDD-W indicator was validated against(11). Further analysis was conducted using the criterion of two-thirds of the Dietary Reference Intakes which has been commonly used by researchers as a target(Reference Ponza, Ohls and Millen55) and in previous national studies in Lebanon(Reference Jomaa, Naja and Cheaib56–Reference Hwalla, Adra and Jackson58). Dietary Reference Intakes refer to the RDA and adequate intakes for selected macro- and micronutrients(54). This criterion represents the proportion of mothers failing to meet two-thirds of the RDA or adequate intake for key macro- and micronutrients taking into account their age and reproductive status.
Statistical analysis
Data entry was completed with the support of KOBO Technology provided by Harvard Humanitarian Institute(59). Data analysis was carried out using the Statistical Package for Social Sciences, version 27.0 (SPSS Inc.). Descriptive statistics were expressed as mean and standard deviation for continuous variables or as number of subjects and percentages (n, %) for nominal variables. Reproductive status of the mother was categorised as PM, non-pregnant LM and non-pregnant non-lactating mothers (NPNLM). Associations were investigated between the reproductive status of the mother and the MDD-W indicator and food group diversity score using χ 2 test for categorical variables and one-way ANOVA test to compare means. Simple and multiple binary logistic regressions were used to examine the association between maternal LDD (dependent variable) and socio-economic and household characteristics, healthcare service utilisation, anaemia, nutritional and mental health status of the mothers, daily meal patterns of mothers and nutrient inadequacies. Regression models were assessed for significance by evaluating the R 2, overall percentage and Hosmer and Lemeshow test. Crude odds were expressed as OR and adjusted OR as aOR with 95 % CI. Point biserial and Pearson’s correlation tests were used to examine the association between the probability of being food insecure and key variables in the study. Independent-samples t test was used to examine the associations between the main food groups and subgroups from the FFQ and the low- and high-income group. Statistical significance was defined as P-value <0·05. Correlation coefficients, tolerance, variance inflation factors and the condition index were used to measure multicollinearity on all the independent variables.
Results
A total of 433 subjects were included in the final analysis of the study, of which 17·8 % were PM, 35·1 % NPNLM and 47·1 % LM. The prevalence of moderate and severe FI in the total study population was 34·4 % (sd 0·1), whereby the prevalence of severe FI reached 12·5 % (sd 0·1). No significant differences were found between the prevalence of FI and the reproductive status groups of mothers (data not shown in table). Nearly two out of three Syrian refugee mothers had a LDD (63·3 %) in the present study, while only 36·7 % of the mothers achieved MDD-W. On average, mothers with LDD consumed 3·2 (sd 0·8) food groups per day, while mothers with MDD-W consumed 5·6 (sd 0·8) food groups, with scores ranging from 1 to 9 food groups (Table 1).
Table 1. MDD-W indicator among Syrian mothers according to their reproductive status based on 24-h dietary recalls
(Mean values and standard deviations)

MDD-W, Minimum Dietary Diversity for Women; NPNLM, non-pregnant non-lactating mothers; LDD, low dietary diversity.
* Categorical variables are expressed as n (%) and continuous variables are expressed as mean values and standard deviations.
** The variable ‘fruits and vegetables’ is the sum of food groups 7, 8, 9 and 10.
† Significantly different at P-value <0·05; P-value was derived using one-way ANOVA test for continuous variables and χ 2 analysis for categorical variables.
‡ Food group diversity score is the sum of the first ten MDD-W food groups consumed yesterday.
§ The MDD-W indicator defined LDD as a food group diversity score < 5 and MDD-W as ≥ 5 out of ten food groups.
‖ The variable ‘pulses, nuts and seeds’ is the sum of food groups 2 and 3.
¶ The variable ‘animal-source foods’ is the sum of food groups 4, 5 and 6.
As shown in Table 1, the MDD-W indicator and food groups consumed yesterday by mothers were presented according to their reproductive status and based on the 24-h dietary recalls. Overall, no significant differences in the MDD-W indicator were observed among PM, LM and NPNLM. Nearly two-thirds of the mothers consumed less than five food groups over the previous day (PM: 62·3 %, LM: 62·7 %, NPNLM: 64·5 %), with an average consumption of 4·1 (sd 1·4) food groups. Almost all mothers in the study sample consumed grains, white roots and tubers (99·5 %). Sugar-sweetened beverages (82·0 %) and oils and fats (79·7 %) were consumed by a majority and nearly half of the mothers had eaten sweets (42·7 %) during the previous day. The consumption of fruits and vegetables was reportedly high (86·8 %); however, dark green leafy vegetables and vitamin A-rich fruits and vegetables were rarely included in their diet (11·8 and 13·4 %). Mothers consumed largely other vegetables (74·8 %) and moderately other fruits (39·0 %). Similarly, animal-source foods were widely consumed (86·6 %), yet less than 50 % ate meat, poultry and fish (44·6 %) or eggs (29·8 %) while dairy products were more prevalent in their diet (68·4 %). The lowest consumption was observed for pulses, nuts and seeds (27·3 %) among all mothers. LM consumed more dairy products and other beverages and foods than PM and NPNLM, while PM had a higher intake of eggs as compared with LM and NPNLM (P < 0·05). Furthermore, even though it did not reach a statistical difference, a higher proportion of LM consumed sweets, sugar-sweetened beverages, other fats and oils, as compared with PM and NPNLM.
Nutrient inadequacies of key macro- and micronutrients according to maternal LDD, based on 24-h dietary recalls, are shown in Table 2. High prevalence of inadequate intakes was found among mothers for proteins, fibres, folate, vitamins B12, B6, C and A, Zn and Ca ranging from 70·8 to 89·6 %. Moreover, more than half of the mothers did not meet the EAR for riboflavin (64·7 %), Fe (59·5 %) and niacin (55·7 %). Simple regressions showed that maternal LDD was significantly associated with nutrient inadequacies (< EAR) for key vitamins, minerals and macronutrients studied. After adjusting for the energy intake of mothers, significant associations between LDD and nutritional inadequacies persisted for vitamins B12, C and A and riboflavin. The odds of nutrient inadequacies increased by two to three times among mothers with LDD as compared with mothers who achieved MDD-W. Further analysis displaying the proportion of mothers failing to meet two-thirds of the RDA or adequate intake for key macro- and micronutrients is shown in online Supplementary Table S1. Findings showed a high prevalence of nutrient intake below two-thirds of Dietary Reference Intake for the majority of the studied macro- and micronutrients. After adjusting for energy, significant associations remained between LDD and intake below two-thirds of Dietary Reference Intake for a wide array of vitamins and minerals as well as protein and dietary fibres.
Table 2. Nutrient inadequacy of key macro- and micronutrients according to maternal low dietary diversity based on 24-hour dietary recalls
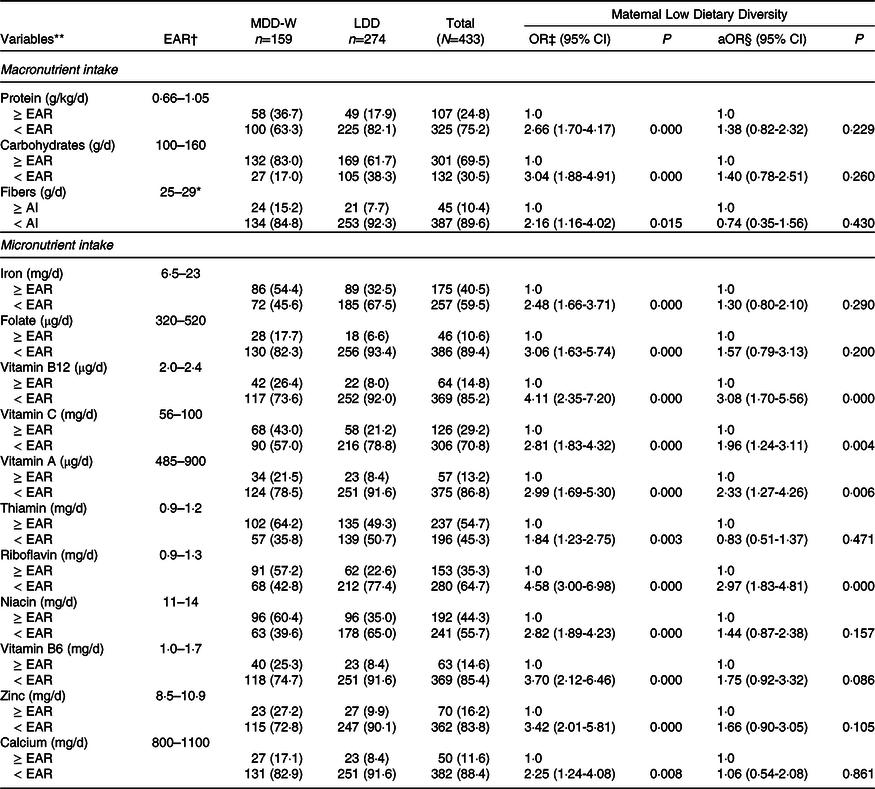
LDD, low Dietary Diversity; EAR, estimated average requirements; MDD-W, Minimum Dietary Diversity for Women; aOR, adjusted OR; AI, adequate intake.
AI is presented in ordinary types followed by an asterisk (*)(54).
** Categorical variables are expressed as n(%).
† EAR is the average daily nutrient intake level estimated to meet the requirements of half of the mothers according to their age and reproductive status groups.
‡ OR of the dependent variable (MDD-W vs. LDD) are presented with 95% CI using simple logistic regression. aOR are presented with 95% CI using multiple logistic regression analysis.
§ Model 1: adjusted for total energy intake.
Statistical significance was defined as P-value < 0·05.
Key determinants of LDD among Syrian mothers of children under 5, including socio-economic and household characteristics, healthcare service utilisation, maternal daily meal pattern, anaemia and nutritional status, are presented in Table 3. Simple logistic regression analysis showed that LDD among mothers was significantly associated with mother’s education, father’s employment status, household monthly income, UNHCR registration status as a refugee, being a beneficiary of WFP food assistance, crowding index score, mother’s use of micronutrient supplements, number of antenatal care visits during the previous pregnancy and sources of health and nutrition messages from healthcare professionals (P < 0·05). Using the multiple logistic regression model, mothers in households with a monthly income ≤ 750 000 LBP had a two times higher odds of having LDD (aOR = 2·09; 95 % CI 1·19, 3·67) than those in households with a higher income. In addition, LDD was significantly associated with higher odds of being registered as a refugee with the UNHCR (aOR = 2·13; 95 % CI 1·07, 4·24), receiving WFP food assistance (e-vouchers) (aOR = 3·70; 95 % CI 1·09, 12·53) and a higher crowding index score (aOR = 1·32; 95 % CI 1·07, 1·64). On the other hand, mothers with LDD were less likely to use micronutrient supplements (aOR = 0·49; 95 % CI 0·27, 0·88). LDD was also inversely associated with receiving health and nutrition messages from a community healthcare worker and from multiple healthcare professionals (aOR = 0·27; 95 % CI 0·08, 0·84 and aOR = 0·04; 95 % CI 0·00, 0·43, respectively) as compared with mothers who did not receive any messages. Mother’s education, father’s employment and number of antenatal care visits were no longer statistically significantly associated with LDD after adjusting for socio-economic variables. Mothers consuming a daily breakfast and a higher number of snacks per day were significantly less likely to have LDD (P < 0·05). No significant associations were found between maternal dietary diversity, anaemia and nutritional status of the mother.
Table 3. Key determinants of maternal low dietary diversity among Syrian mothers

LDD, low dietary diversity (< 5 out of 10 food groups); MDD-W, Minimum Dietary Diversity for Women (≥ 5 out of 10 food groups); WFP, World Food Programme; aOR, adjusted OR; PM, pregnant mothers.
* Categorical variables are expressed as n (%) and continuous variables are expressed as mean ± sd. Lack of corresponding sum of frequencies with total sample size is due to missing data.
** OR of the dependent variable (MDD-W vs. LDD) are presented with 95% CI using simple logistic regression.
† aOR are presented with 95% CI using multiple logistic regression analysis. Model 2: adjusted for age of the mother and child, sex of the child, reproductive status of the mother, marital status, education and employment status of the parents, household monthly income, crowding index, UNHCR registration status, perception of safety, receiving cash or food assistance, reliance on savings, household type, head of household, total number of under-five children, health insurance coverage, healthcare type, sources of health messages, the probability of being moderately and severely food insecure, and maternal anemia.
‡ Model 3: Model 2 without receiving cash or food assistance.
§ Healthcare professionals included physicians, nurses, dietitians, and pharmacists.
‖ Non-PM include lactating mothers and non-pregnant non-lactating mothers.
¶ Model 4: Model 2 without the age/marital status/physiological status of the mother.
Statistical significance was defined as P-value < 0·05.
The mental health status of mothers according to maternal LDD and its associations are displayed in Table 4. The prevalence of PTSD was 13·2 %, 16·2 % for mild depression, 11·1 % for moderate depression and 9·9 % for severe depression. In total, 27·1 % of the mothers suffered from PTSD and/or moderate/severe depression. Simple logistic regressions showed that mothers with PTSD, mild depression or severe depression had significantly higher odds of LDD (P < 0·05). Similarly, mothers with PTSD and/or moderate/severe depression combined had 1·6 times higher odds of LDD as compared with those not suffering from PTSD or depression. However, these associations did not remain significant after adjusting for socio-economic characteristics and maternal anaemia. Additional analysis showed that mothers with a higher crowding index had 1·2 times higher odds of suffering from PTSD and/or moderate/severe depression (aOR = 1·24, 95 % CI 1·01, 1·52). Furthermore, a higher proportion of mothers suffering from the flu were found to have a crowding index higher than 2 as compared with those without the flu (97·4 % v. 81·3 %, P < 0·05) (data not included in table).
Table 4. Mental health status of Syrian mothers by maternal low dietary diversity and its associations
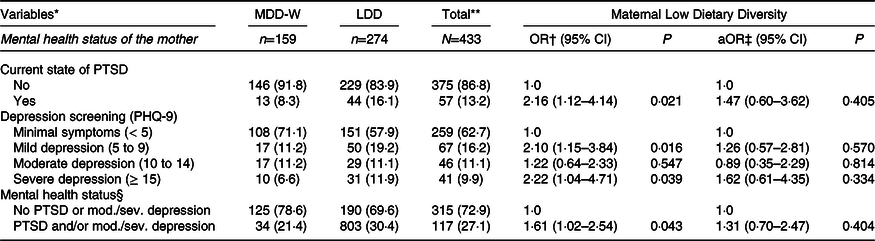
MDD-W, Minimum Dietary Diversity for Women; LDD, low dietary diversity; aOR, adjusted OR; PTSD, post-traumatic stress disorder; PHQ-9, Patient Health Questionnaire-9.
* Categorical variables are expressed as n(%).
** Lack of corresponding sum of frequencies with total sample size is due to missing data.
† OR of the dependent variable (MDD-W vs. LDD) are presented with 95% CI using simple logistic regression.
‡ aOR are presented with 95% CI using multiple logistic regression analysis. Model 2: adjusted for age of the mother and child, sex of the child, reproductive status of the mother, marital status, education and employment status of the parents, household monthly income, crowding index, UNHCR registration status, perception of safety, receiving cash or food assistance, reliance on savings, household type, head of household, total number of under-five children, health insurance coverage, healthcare type, sources of health messages, the probability of being moderately and severely food insecure, and maternal anemia.
§ Moderate/severe (mod./sev.) depression was defined as PHQ-9 score ≥ 10(Reference Kroenke, Spitzer and Williams32).
Statistical significance was defined as P-value < 0·05.
Table 5 displays correlations analyses between FI and dietary indicators, mental health, anaemia, nutritional status and socio-economic characteristics. A moderately strong significant negative correlation was found between the food group diversity score and the probability of being moderately and severely food insecure (r = -0·283; P < 0·000) as well as severely food insecure (r = -0·251; P < 0·000). Furthermore, the number of meals and snacks consumed per day was also negatively correlated with FI. As for the mental health indicators, suffering from PTSD, depression and PTSD and/or moderate/severe depression were significantly correlated with the probabilities of being food insecure (P < 0·000). The strongest correlation was found between the depression screening and the probability of being moderately and severely food insecure (r = -0·353; P < 0·000). Noticeable significant correlations were also found between the probability of being food insecure and the household monthly income level, employment status of the father and the crowding index. Very weak correlations were found with the education level and employment status of the mother, number of children under the age of 5 years, the reliance on savings and subsidies, registration status as refugee, head of the household and receiving health messages from healthcare professionals only. No associations were found between the probability of being food insecure and anaemia, nutritional status of the mother and the mother’s use of micronutrient supplements. Further analysis showed that receiving WFP food assistance was significantly associated with a higher mean crowding index and a higher number of children aged under 5 in the household compared with not receiving WFP food assistance (4·7 (sd 1·8) v. 3·6 (sd 1·6) and 4·5 (sd 1·6) v. 2·5 (sd 1·4), respectively; P < 0·000) (data not shown in table).
Table 5. Correlations between food insecurity and dietary, health and socio-economic characteristics of Syrian mothers
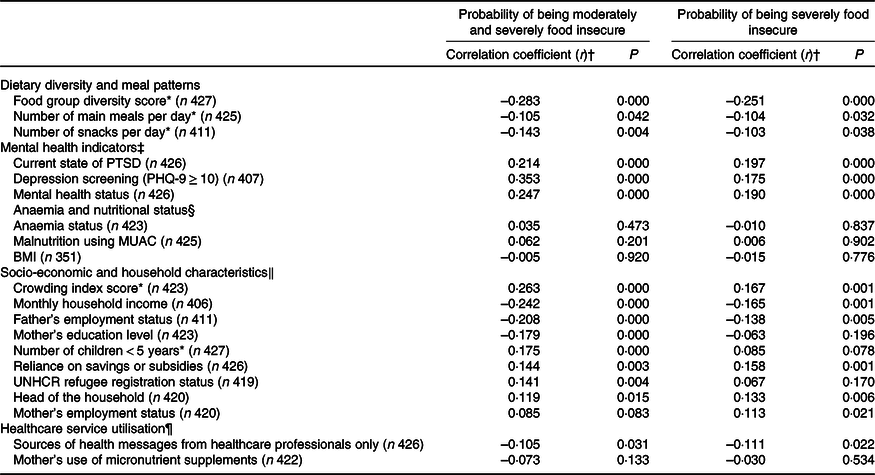
PTSD, post-traumatic stress disorder; PHQ-9, Patient Health Questionnaire-9; MUAC, mid-upper arm circumference.
* Indicate continuous variables.
† Point biserial correlation test was used for continuous and dichotomous variables. Pearson’s correlation test was used for continuous variable. The strength of correlation is interpreted as follows: up to 0 2 (very weak), up to 0 5 (weak), up to 0 7 (moderate) and up to 0 9 (high). Significantly different at P-values < 0·05.
‡ Current state of PTSD (no v. yes), depression screening (minimal or mild depression (PHQ-9 < 10) v. moderate or severe depression (PHQ-9 ≥ 10)(Reference Kroenke, Spitzer and Williams32)), mental health status (no PTSD and/or moderate/severe depression v. PTSD and/or moderate/severe depression).
§ Anaemia status (no v. yes), classification of malnutrition using MUAC (undernourished/normal weight v. overweight/obese), BMI (underweight/normal weight v. overweight/obese).
‖ Monthly household income (≤ 750 000 LBP v. > 750 000 LBP), father’s employment status (full-time job v. no job/part-time job), mother’s education level (intermediate school or lower v. secondary school or higher), reliance on savings or subsidies (no v. yes), UNHCR refugee registration status (no v. yes), head of the household (father/family-in-law v. mother/both parents), mother’s employment status (no paid job/housewife v. paid job).
¶ Sources of health messages from healthcare professionals only (no v. yes), mother’s use of micronutrient supplements (no v. yes).
Food groups consumption of mothers based on dietary data from the FFQ according to the household monthly income is shown in Table 6. Overall, grains and starchy staples constituted the highest share of the total energy intake reaching 45·2 % EI (sd 16·3) followed by 15·7 % EI (sd 0·6) from fats and oils and 7·8 % EI (sd 6·3) from sweets and sugar derivatives. On average, dairy products, pulses, nuts, seeds and fruits contributed from 3·2 to 5·8 % to energy consumption, while very low contributions were observed from eggs and flesh foods (2·0 % EI (sd 2·2) and 2·3 % EI (sd 2·3), respectively). The lowest contribution to energy consumption was noted from the vegetables group. Other food groups such as mixed dishes, pizzas and pies, salty snacks, beverages and condiments and pickles also had a limited share in the total energy intake of about 1·7 % EI to 2·7 % EI.
Table 6. Percentage contribution of food groups to total energy intake (% EI) by income groups based on dietary data from the FFQ
(Mean values and standard deviations)
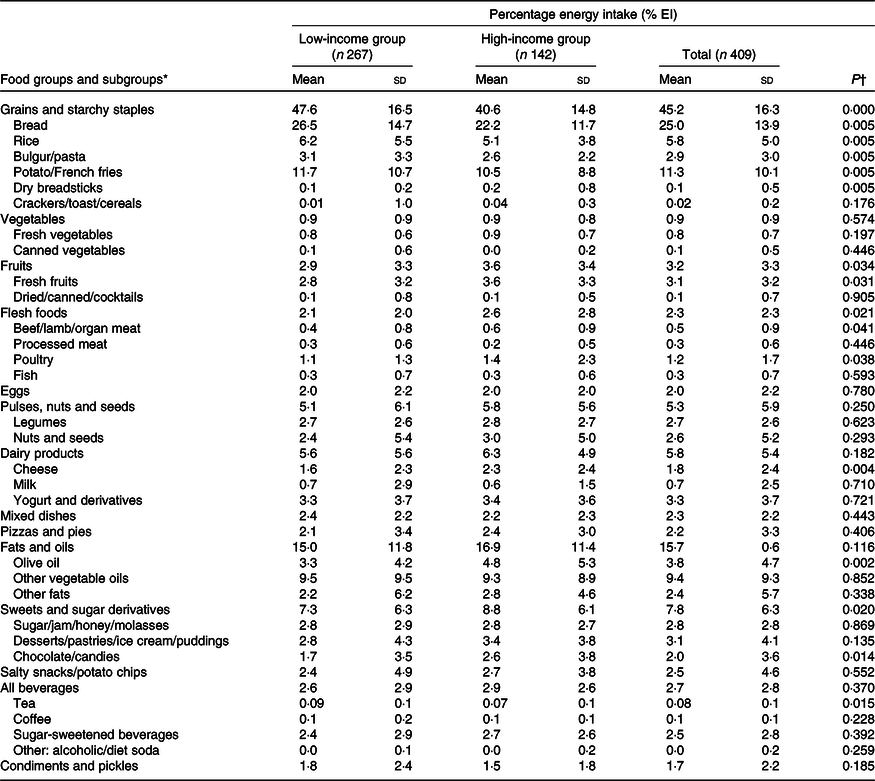
% EI, percentage energy intake.
* Continuous variables are expressed as mean values and standard deviations.
† Significantly different at P-value < 0·05; P-value was derived using one-way ANOVA test.
Mothers from the low-income households had a significantly higher contribution to energy consumption from grains and starchy staples when compared with those from the high-income households, such as bread (26·5 (sd 14·7) % EI v. 22·2 (sd 11·7) % EI, P < 0·05) and rice (6·2 (sd 5·4) % EI v. 5·1 (sd 3·8) % EI, P < 0·05). In contrast, the contribution to energy consumption from highly nutritious food groups was significantly lower among mothers from low-income households than those from high-income households, including fruits and fresh fruits, cheese, olive oil and flesh foods, in particular beef, lamb, organ meat and poultry (P < 0·05). On the other hand, it was observed that the high-income households had a significantly higher contribution to energy consumption from sweets and sugar derivatives, especially chocolate and candies, as compared with the low-income households (P < 0·05). Tea consumption contributed significantly more to the dietary intake of the low-income households, as compared with high-income households (P < 0·05). No significant differences between the income groups were observed for vegetables, processed meat, fish, eggs, pulses, nuts, seeds, milk, yogurt, pizzas and pies, other vegetables oils and fats, salty snacks, condiments, pickles, sugar-sweetened beverages and other drinks (Table 6).
Discussion
The present study aimed to assess and examine the associations between maternal FI and dietary diversity, and mental health, anaemia and nutritional status of Syrian refugee mothers living in Greater Beirut, Lebanon. The study’s main findings showed that one out of three mothers was moderately to severely food insecure (34·4 %), with 12·5 % being severely food insecure, and almost two-thirds of the mothers had a LDD (63·3 %). A large body of literature recorded a wide range of FI and LDD prevalence among women(Reference Chakona and Shackleton60–Reference Aliwo, Fentie and Awoke67) and refugees(Reference Morseth, Grewal and Kaasa68,Reference Henjum, Caswell and Terragni69) in low- and middle-income countries. Rates of FI in our study were close to those among registered Syrian refugee households in 2018–2019 across Lebanon, with one of the highest recorded in Mount Lebanon, as reported by the WFP and UNHCR(26,70) . However, higher rates of moderate to severe FI were previously found among urban Lebanese households in Greater Beirut as well as households of Palestinian and Iraqi refugees in Lebanon-(42, 61 and 80 %, respectively)(Reference Jomaa, Naja and Cheaib56,Reference Ghattas, Sassine and Seyfert71,Reference Ghattas, Sassine and Seyfert72) . Lower FI rates reported in the present study may be attributed to the extensive humanitarian assistance targeting primarily Syrian refugees across Lebanon since the start of the war in 2011 and the large displacement of refugees from Syria(70). The prevalence of LDD in our study was found to be comparable to those from low- and middle-income countries such as mothers in Lebanon (61·8 %)(Reference Jomaa, Naja and Kharroubi73) and women refugees in Algeria (69 %)(Reference Morseth, Grewal and Kaasa68). Yet, it remained much higher compared with women asylum seekers in Norway, a high-income country (49 %)(Reference Henjum, Caswell and Terragni69). Hanley-Cook et al. showed evidence of overreporting of food groups by 10–16 % for assessing the prevalence of MDD-W of reproductive age using the list-based or open recall methods(Reference Hanley-Cook, Tung and Sattamini74). This suggests that the prevalence of LDD can be even higher in our study. Our findings are alarming and indicate that a significant proportion of women of reproductive age have a poor diet quality and are far from reaching the recommendations for nutrient requirements and dietary diversity.
FI and poor dietary diversity among mothers were significantly correlated in our study. This link has been well documented in the literature(Reference Kang, Hurley and Ruel-Bergeron63,Reference Singh, Ghimire and Upadhayay64,Reference Na, Mehra and Christian75) . Our findings showed that a household monthly income below or approximately equal to the legal minimum wage and a higher crowding index were significantly associated with FI and LDD. It is no surprise that both indicators share common underlying determinants as a result of their leading denominator: a low socio-economic status. Similar findings were also reported by a national study among Lebanese mothers(Reference Jomaa, Naja and Kharroubi73). Furthermore, receiving WFP food assistance was significantly associated with LDD among Syrian refugee mothers in Greater Beirut in our study. This suggests that WFP food assistance may not necessarily ensure a diverse diet. Staple foods accounted for 42 % of total food expenditure among Syrian refugees in Lebanon, while only 13 % was spent on fruits and vegetables and 8 % on fresh meat(70). This indicates that a more monotonous diet was consumed by the refugees. In fact, Beirut witnessed a drawback in food consumption scores and Mount Lebanon continued to have the poorest food consumption scores, despite a nationwide improvement in poor and borderline food consumption levels among Syrian refugees in Lebanon in 2018–2019(26). Moreover, poor dietary diversity and low meal frequency emerged as potential coping mechanisms against FI among mothers in our study. Syrian refugees, notably in Mount Lebanon, were increasingly reducing the number of meals eaten per day and portion sizes but also restricting food consumption by adults for the sake of children(26).
Our previous study showed evidence of higher proportions of nutritional inadequacies among PM and LM as well as an overall maternal diet rich in sugar and fat and poor in protein, fibres and micronutrients(Reference Abou-Rizk, Jeremias and Nasreddine28). Further analysis showed that the consumption of food groups was also consistent with the ‘Western diet’ in the present study, characterising the nutrition transition in low- and middle-income countries(Reference Popkin, Adair and Ng76). Overall, high contributions to energy intake from grains, starchy staples, and oils and fats were recorded over the past year with poor incorporation of nutrient-rich foods. Contribution of legumes, nuts, seeds, fruits and vegetables was low, particularly of vitamin A-rich fruits and green leafy vegetables. Similar nutritional habits and monotonous diets were found among asylum seekers living in Germany(Reference Khan, Fischer and Ghaziani77,Reference Schmitt, Fülle and Abou-Rizk78) and Norway(Reference Henjum, Caswell and Terragni69). Nasreddine et al. (Reference Nasreddine, Ayoub and Hachem79) also highlighted a shift in consumption towards refined grains, highly processed foods and added fats and oils and deviating from nutritious foods in Lebanon. Food systems and environments are well-known to influence food choices, customs and diets as well as to a great extent food security and nutrition. Key aspects include the physical, economic, political and socio-cultural context. Food customs are also shaped by religions and beliefs, traditions, cultures and social norms(80). According to a recent study, food played a central role in the social integration among Syrian refugees in Germany and was considered essential to their cultural value and psychological well-being despite challenges associated with food-related autonomy and environment. However, the authors also highlighted that, while Syrian refugees in the Middle East might benefit from a similar food environment to the one in Syria, refugees in Lebanon might be confronted with higher economic hardships hindering their purchasing power and access to food(Reference Al-Sayed and Bieling81).
Socio-economic disparities, such as the income, shape the diet structure to a great extent among vulnerable populations. Higher contributions to energy intake from grains and refined starchy staples such as bread and rice were found among low-income households in our findings. Lower income groups usually spend a higher share of money on food, influencing their food choices. The higher cost of a healthy diet may be a significant barrier, especially that lean meats, fish and fresh produce are more expensive energy sources compared with grains, fats and sweets(Reference Darmon and Drewnowski82). Syrian refugee households in Mount Lebanon recorded the highest percentage of food expenditures on bread and pasta (47 %) compared with other governorates in Lebanon(70). Inversely, high-income households in our study had a more diverse diet with significantly higher contributions of fruits, cheese, olive oil and flesh foods but also of sweets and sugar derivatives to total energy consumption. Lopez et al. (Reference Lopez, Gonzalez and Villegas83) also found that other vegetable oils were consumed more than olive oil to lower the total costs of the diet. A Mediterranean dietary pattern was found to be more expensive than a Western dietary pattern, as it is mostly based on the consumption of local fruits and vegetables, beans, nuts and seeds, dairy products and olive oil(Reference Hachem, Capone and Yannakoulia84). With increasing economic vulnerabilities and FI, poor diet quality and diversity are often the result of an increased consumption of cheap and high energy-dense foods rather than nutrient-dense foods as a strategy to stretch the energy cost and reduce food expenditures(Reference Darmon and Drewnowski82). An inadequate intake of vitamins and minerals and distorted contribution of fats and sugars to energy can lead to under- and overnutrition alongside persisting micronutrient deficiencies(Reference Tanumihardjo, Anderson and Kaufer-Horwitz15,Reference Hwalla, Al Dhaheri and Radwan85,Reference Perez-Escamilla, Bermudez and Buccini86) . The co-occurrence of overnutrition and anaemia among mothers and undernutrition among children was reported in our previous study among Syrian refugees from the same household in Greater Beirut(Reference Abou-Rizk, Jeremias and Nasreddine28).
Regarding the mental health status of the mothers, nearly one-third were suffering from PTSD and/or moderate to severe depression in our study. Comparable and higher prevalence rates were reported among Palestinian and Syrian refugees in Lebanon(Reference Ghattas, Sassine and Seyfert72,Reference Hyland, Ceannt and Daccache87–Reference Naal, Nabulsi and El Arnaout90) . A strong relationship was observed between poor maternal mental health, FI and a high crowding index in our findings. Poverty and FI are well documented as factors associated with psychological distress and depression symptoms. The struggle to provide food on a day-to-day basis and worrying about living expenses can exacerbate effects on mental health(Reference Emerson, Tol and Caulfield18,Reference Elgar, Pickett and Pförtner91) . Certainly, overcrowding, poor living conditions and lack of resources can accumulate the risk of deterioration of the health status(35). Furthermore, evidence on the association between depression, FI and poor dietary diversity is found in the literature, suggesting a relationship between micronutrient deficiencies and mental health disorders(Reference Sparling, Waid and Wendt17,Reference Poorrezaeian, Siassi and Milajerdi92,Reference Woldetensay, Belachew and Biesalski93) . However, the lack of association between the mental health status and LDD in our study could be due to the fact that the MDD-W indicator does not assess the intake of certain nutrients or food groups related to mental health outcomes.
As for the nutritional status of the mothers, the lack of association with LDD and FI observed in our survey was in line with the literature(Reference Jomaa, Naja and Kharroubi73,Reference Gómez, Fisberg and Nogueira Previdelli94–Reference Kehoe, Wrottesley and Ware96) , even though a relationship between FI and obesity was documented among Lebanese mothers(Reference Jomaa, Naja and Cheaib56). One explanation could be that the food group diversity score does not account for the amounts of food consumed, physical activity levels and total energy expenditure(Reference Gómez, Fisberg and Nogueira Previdelli94). We also suggest it could be explained by the exclusion of the nutrient-dense food groups from the score, such as oils and fats, sweets, snacks and sugar-sweetened beverages. Furthermore, anaemia was not associated with maternal LDD and FI in our survey, similar to findings from pregnant women in Ghana(Reference Saaka, Oladele and Larbi97) and Pakistan(Reference Ali, Thaver and Khan98). Other studies were able to demonstrate a relationship between anaemia and LDD as well as FI(Reference Ghose, Tang and Yaya99,Reference Zerfu, Umeta and Baye100) . The multifactorial nature of anaemia can provide an explanation to these controversial findings as several factors may act as causes or contributors. These may be related not only to poor dietary practices, low bioavailability of nutrients, high intake of inhibitors, genetic disorders, infections and inflammation but also to environmental and socio-economic factors including women’s empowerment, poverty, education and access to healthcare(101). In fact, a very plausible explanation regarding the lack of association in our study could be related to the role of health and nutrition awareness programmes. While our previous study showed that receiving health and nutrition messages and access to the free or subsidised healthcare in place for refugees in Lebanon could have played a role in reducing anaemia(Reference Abou-Rizk, Jeremias and Nasreddine28), our present findings also shed light on the role of healthcare professionals. Once more, an indication on the beneficial impact of health services offered to refugees is found and emphasises the crucial role of counselling on improving dietary diversity and anaemia.
New threats to food security and nutrition were rising in Lebanon since October 2019 due to the strong socio-political unrest and severe financial crisis involving spiralling food inflation rates and strong currency depreciation. With the combination of containment measures for the COVID-19 pandemic, unemployment rates and reduced income soared across Lebanon for the population and refugees(102). In addition, Lebanon relies heavily on imported commodities and food to cover domestic needs; for instance, 80 % of cereals consumption is met through imports. Long-term effects of the Beirut port explosion on 4 August 2020 will reflect on the economy and supply chain, particularly in Beirut and Mount Lebanon(103). As the ability to access and purchase food is compromised even further, food security and nutrition are expected to worsen and the risk of deterioration of the health and nutritional status of vulnerable groups is higher among both the host population and refugees in Lebanon(25).
Double-duty actions and multicomponent strategies targeting multiple forms of malnutrition simultaneously are a priority and need to tackle social determinants of health and nutrition disparities(Reference Perez-Escamilla, Bermudez and Buccini86). Economic interventions, subsidies and fiscal incentives should be considered to encourage changes in dietary behaviours towards a healthier and sustainable diet. For instance, financial and food assistance programmes should be strengthened and provide additional support to the most vulnerable groups among refugees and the host population. Our findings also shed light on the crucial role of a multidisciplinary approach with a diverse team of healthcare professionals to improve nutrition knowledge, family planning and mental health of women of reproductive age through counselling and awareness-raising sensitive to cultural norms. In light of increasing vulnerabilities, Syrian refugees lack resources to cover essential needs(25). Admittedly, recent studies showed that Syrian women are willing to overcome sex barriers and cultural norms to accessing economic participation when working conditions are decent and safe(104). Policy efforts should target to improve women’s access to economic resources. Strategies need to consider the role of women as both a caregiver and a provider to combat FI and LDD among mothers in poor and vulnerable settings(Reference Schmeer, Piperata and Herrera Rodríguez105).
Limitations
Few limitations should be considered when interpreting the study findings. First, the design of the study is cross-sectional; hence, it cannot infer causality but rather associational relationships. The study was narrowed to the most vulnerable areas of Greater Beirut and to mothers attending PHCC. This may limit the findings to be representative of Syrian refugees in rural settings and at a national level. Recruitment took place in Greater Beirut, covering Beirut and adjacent districts of Mount Lebanon. It is considered to be the melting pot of the country with more than half of the Lebanese population and over 305 000 refugees(30,106) . Second, our measure of FI at the individual level could limit the comparison with other findings measuring household FI using different scales. However, the Food Insecurity Experience Scale has demonstrated its robustness and provides the opportunity to generate internationally comparable measures of FI(Reference Saint Ville, Po and Sen107). Third, the Patient Health Questionnaire-9 was shown to have a good sensitivity but poor specificity in capturing depressive symptoms among adults in Lebanon. The tool was found to be useful in screening for depression in settings lacking sufficient psychiatric care to determine the need for psychiatry referral(Reference Sawaya, Atoui and Hamadeh33). Lastly, dietary data may be subjected to possible recall bias. Enumerators underwent extensive trainings and used standardised protocols to limit the social desirability bias and overcome the memory bias. The 24-h dietary call was collected using the five-step multiple pass recall method, which may improve the accuracy of dietary estimates among adults; however, underreporting under field conditions and among overweight and obese adults remains a constraint(Reference Conway, Ingwersen and Moshfegh48,Reference Conway, Ingwersen and Vinyard108,Reference Moshfegh, Rhodes and Baer109) . The 24-h dietary recall may not take into account seasonal variations; however, the latter is compensated for by the use of FFQ over the past 12 months(110). The FFQ used in our study encompassed a wide range of food groups, including ultra-processed foods. This is an advantage in measuring changing dietary patterns in the context of the nutrition transition(Reference Walls, Johnston and Mazalale111). Another limitation worth mentioning is the absence of an extensive food composition database in Lebanon. So, the USDA database was used, and specific food items were added from the local food composition tables available for a limited number of local foods. Although the absolute estimates of dietary intake could have been affected, its effects on the observed inadequate intakes among mothers would have been limited.
Conclusion
The present study shows evidence of poor dietary diversity and mental health as well as FI among Syrian refugee mothers in an urban setting of a humanitarian crisis. Findings demonstrate poor nutritional practices and low diet quality among women of reproductive age. With increasing economic vulnerabilities and FI, inadequate dietary habits often take place and compromise the quality of the diet. Multifaceted interventions are needed to address the situation holistically, including nutrition-specific interventions and assistance programmes, which can be developed or strengthened at the local and national level, in addition to psychosocial support and family planning. Both, the women’s roles as a caregiver and as provider need to be considered in order to reduce FI and improve dietary diversity among vulnerable groups. Further research is needed to examine the impact of suboptimal maternal nutrition during the first 1000 d on the diet quality and health of children in a humanitarian context. The relationship between poor maternal mental health, breast-feeding practices and maternal nutrition needs to be further explored among Syrian refugee mothers in Lebanon.
Acknowledgements
The authors are deeply grateful to all the participants for participating in the survey. We would like to thank the directors of primary health care centres for granting us access to their premises to conduct the interviews. The centres included Howard Karagheusian Commemorative Corporation and Armenian Relief Cross of Lebanon in Bourj Hammoud, Makhzoumi Foundation PHC in Mazraa, Child & Mother Welfare Hospital in Msaytbeh, Mar Antonious PHC in Baouchriyeh and Maternal Childhood Center in Chiyah and Bourj Barajneh. We would like to extend our gratitude and deep appreciation to our volunteers, field workers and research assistants for their hard work during data collection. We are sincerely grateful to the Medical Research Volunteer Program for their supply of assistance during data collection and entry. We would like to acknowledge the help of Dr Yitbarek Kidane Woldetensay for advancing the analysis of mental health indicators. Last but not least, we would like to extend our thanks to Hisham Kanaan for his support in the use of statistical software.
The publication is an output of a PhD scholarship from the Food Security Center from the University of Hohenheim which is part of the DAAD (German Academic Exchange Service) programme ‘exceed’ and is supported by DAAD and the German Federal Ministry for Economic Cooperation and Development (BMZ) and in cooperation with the hosting Institute of Nutritional Sciences (140). Support was also received by the Fiat Panis Foundation, the BCFN YES! 2017 Research Grant Award from the Barilla Center for Food & Nutrition (BCFN) Foundation and by the University Research Board at the American University of Beirut (award number: 103366). The funding organisations had no role in the design, data collection, analysis or writing of this manuscript.
J. A., T. J. and V. S. conceptualised the research design and led the parent study. L. N., L. J. and N. H. provided support in designing the parent study. J. A., T. J., V. S. and L. N. sought after ethics approval. J. A. and T. J. organised, implemented and supervised the study during data collection and entry. J. A. conducted data analysis, conceptualised and wrote the original draft of the manuscript. G. C. supported data analysis. T. J., V. S., J. F., L. N., L. J. and N. H. critically reviewed the manuscript. All authors have read and agreed to the published version of this manuscript.
The authors declare no conflict of interest.
Supplementary material
For supplementary material referred to in this article, please visit https://doi.org/10.1017/S0007114521004724









