The application of neuropsychology is relevant to the majority of psychiatric subspecialties. This is affirmed in various national clinical guidelines: old age psychiatry in relation to the neurodegenerative disorders 1–3 as well as psychiatry of learning disability and child and adolescent psychiatry in relation to the neurodevelopmental conditions that are clinically eloquent early in life. 4–8 Specialists in general adult psychiatry and forensic psychiatry may encounter individuals affected with the aforementioned conditions. 9 They also treat people with severe and enduring mental illness with neuropsychological sequelae, particularly the chronic psychotic disorders. It is important to distinguish the latter from other neurodegenerative condition, especially in senescence. 10 The neuropsychological assessment of those with suspected alcohol-related brain damage is imperative in their diagnosis and treatment by the various relevant specialties, particularly liaison psychiatry and psychiatry of substance misuse. 10,11
The Scottish Intercollegiate Guidelines Network (SIGN) guideline 86, Management of Patients with Dementia, 2 recommends that neuropsychological testing should be used in the diagnosis of dementia, especially in individuals where dementia is not clinically obvious. The guideline acknowledges that the provision of neuropsychology services is variable and in some places nonexistent, suggesting psychiatrists often have to perform neuropsychological assessments by default. Postgraduate specialist psychiatric training courses appear to offer only rudimentary formal neuropsychology training to career psychiatric trainees. The only postgraduate neuropsychology training course in Scotland is offered by Glasgow University, but only clinical psychologists are eligible to enrol for training beyond a limited set of continuing professional development (CPD) modules.
Method
A questionnaire was designed to establish estimates of neuropsychology service provision, the level of neuropsychology training psychiatrists have received, and to elicit their views on formal postgraduate neuropsychology training (the questionnaire is available in full from the author).
At the time of the survey, the Scottish division of the Royal College of Psychiatrists had 1063 members. The Registrar supplied the contact details of the actively practising members who had consented to their details being made available. Questionnaires were posted in winter 2007 and a reminder was sent to nonrespondents. Data were managed and analysed with the assistance of the NHS Forth Valley Clinical Effectiveness Support Service.
Results
A total of 658 surveys were despatched and a 61.39% (n = 404) response rate was achieved. Overall, 288 consultants responded to this questionnaire, which equates to 71% of the total number of questionnaires returned. At the time of the survey, 538 consultants were working in Scotland, resulting in a consultant response rate of 54%. As there was a relatively low response rate from non-consultant grades, it was decided to analyse the responses of consultants within their stated subspecialties (Appendix). Ninety-five per cent (n = 276) of consultants indicated that they have at least achieved MRCPsych level as their postgraduate psychiatric qualification. Training had been completed in its entirety in Scotland for 77% (n = 222) of the participants, 8.5% (n = 25) partially in Scotland and 12.5% (n = 36) completed their full training in other parts of the UK.
With regard to neuropsychology service provision in health board areas, 32% (n = 99) of consultants indicated that a consultant neuropsychologist and 34% (n = 99) that a psychologist with specialist interest in neuropsychology was available, and 13% (n = 36) had access to both; 14% (n = 40) indicated there was no service provision within their health board area, which included 12.5% (n = 9) of old age psychiatrists. Table 1 illustrates by the consultants’ subspecialty their rating of the sufficiency of the neuropsychology service available to them to deal with clinical demand.
Table 1. Consultants’ rating of the sufficiency of the neuropsychology service available to them to deal with clinical demand

| %, n | ||||||||
|---|---|---|---|---|---|---|---|---|
| General adult (n = 78) | Old age (n = 52) | Liaison (n = 12) | Forensic (n = 16) | Rehabilitation (n = 10) | Child and adolescent (n = 31) | Learning disability (n = 11) | Addiction (n = 7) | |
| Very good | 2.5 (2) | 23 (12) | 8 (1) | 6 (1) | 0 | 3 (1) | 0 | 0 |
| Good | 20.5 (16) | 13 (7) | 8 (1) | 12.5 (2) | 0 | 23 (7) | 18 (2) | 0 |
| Fair | 29.5 (23) | 19 (10) | 33 (4) | 44 (7) | 20 (2) | 39 (12) | 55 (6) | 14 (1) |
| Poor | 23 (18) | 29 (15) | 25 (3) | 25 (4) | 10 (1) | 10 (3) | 0 | 43 (3) |
| Very poor | 4 (3) | 4 (2) | 25 (3) | 0 | 10 (1) | 19 (6) | 0 | 14 (1) |
| Spoiled | 20.5 (16) | 12 (6) | 0 | 12.5 (2) | 60 (6) | 6 (2) | 27 (3) | 29 (2) |
Table 2 indicates that consultant old age psychiatrists have the highest level of confidence in using and interpreting common neuropsychological assessment tools (e.g. the Addenbrooke's Cognitive Examination recommended in SIGN 86), although only 62% of them indicated their level of confidence as ‘good’ or ‘very good’. The consultants’ in other subspecialties fairly average or low confidence in their basic clinical neuropsychological skills could be related to 5.5% (n = 15) of consultants rating the availability of training in neuropsychology for psychiatrists as good to very good, 15.5% (n = 45) as ‘fair’ and 73.5% (n = 212) as ‘poor’ or ‘very poor’.
Table 2. Consultants’ level of confidence in using and interpreting common neuropsychological assessment tools
| %, n | ||||||||
|---|---|---|---|---|---|---|---|---|
| General adult (n = 102) | Old age (n = 63) | Liaison (n = 15) | Forensic (n = 22) | Rehabilitation (n = 12) | Child and adolescent (n = 34) | Learning disability (n = 15) | Addiction (n = 9) | |
| Very good | 2 (2) | 24 (15) | 20 (3) | 9 (2) | 0 | 0 | 0 | 11 (1) |
| Good | 15 (15) | 38 (24) | 20 (3) | 9 (2) | 0 | 3 (1) | 0 | 11 (1) |
| Fair | 26 (27) | 25 (16) | 27 (4) | 32 (7) | 50 (6) | 21 (7) | 27 (4) | 0 |
| Poor | 44 (45) | 13 (8) | 20 (3) | 32 (7) | 42 (5) | 35 (12) | 33 (5) | 56 (5) |
| Very poor | 10 (10) | 0 | 7 (1) | 9 (2) | 0 | 32 (11) | 20 (3) | 22 (2) |
| Unanswered/spoiled | 3 (3) | 0 | 7 (1) | 9 (2) | 8 (1) | 9 (3) | 20 (3) | 0 |
A total of 35% (n= 101) of consultant psychiatrists stated they had received training in neuropsychology, 4% (n = 11) indicated that the method of training was through participation in research. Of these respondents, 56.5% rated the value of this training in terms of their role as a psychiatrist as ‘good’ or ‘very good’, 30.5% as ‘fair’ and only 6% as ‘poor’ or ‘very poor’. However, 49.5% of these consultants (n = 50), indicated that the method (or one of the methods) of their training in neuropsychology was self-directed.
Figure 1 illustrates the perceived value that consultants of all subspecialties hold for different levels of formal and accredited neuropsychology training for psychiatrists.
Of the 74% (n = 212) of consultants who rated the availability of neuropsychology training for psychiatrists as ‘poor’ or ‘very poor’, 93% (197) indicated that access to CPD modules would be of value and 47% (99) indicated the opportunity of postgraduate diploma or masters level training as valuable. Of the 182 consultants who stated they had no training in neuropsychology, 75% (n = 158) regarded CPD modules as potentially valuable and 37% (n = 79) potential postgraduate diploma or masters level training as valuable. Within subspecialties, all 15 liaison psychiatrists, 92% of old age psychiatrists (n = 58) and 90% of general adult psychiatrists (n = 92) indicated that CPD modules would be of value. In addition, 74% (n = 11) of the liaison psychiatrists and 67% (n = 42) of the old age psychiatrists indicated that postgraduate diploma-level training would be of value. In total, 66% (n = 6) of addictions psychiatrists, 50% (n = 17) of child and adolescent psychiatrists and 38% (n = 24) of old age psychiatrists suggested masters degree training would be valuable.
At the end of the questionnaire an ‘other comments’ box was provided. There were three distinct themes of responses (from all 404 respondents). Twenty respondents commented that they would not be interested in additional training in neuropsychology, as they did not view neuropsychological assessment as part of their clinical work. However, 63 respondents used the opportunity to express a desire to have access to further training. Twenty-six respondents used the ‘other comments’ box to express their frustrations at the dearth of neuropsychological service provision.
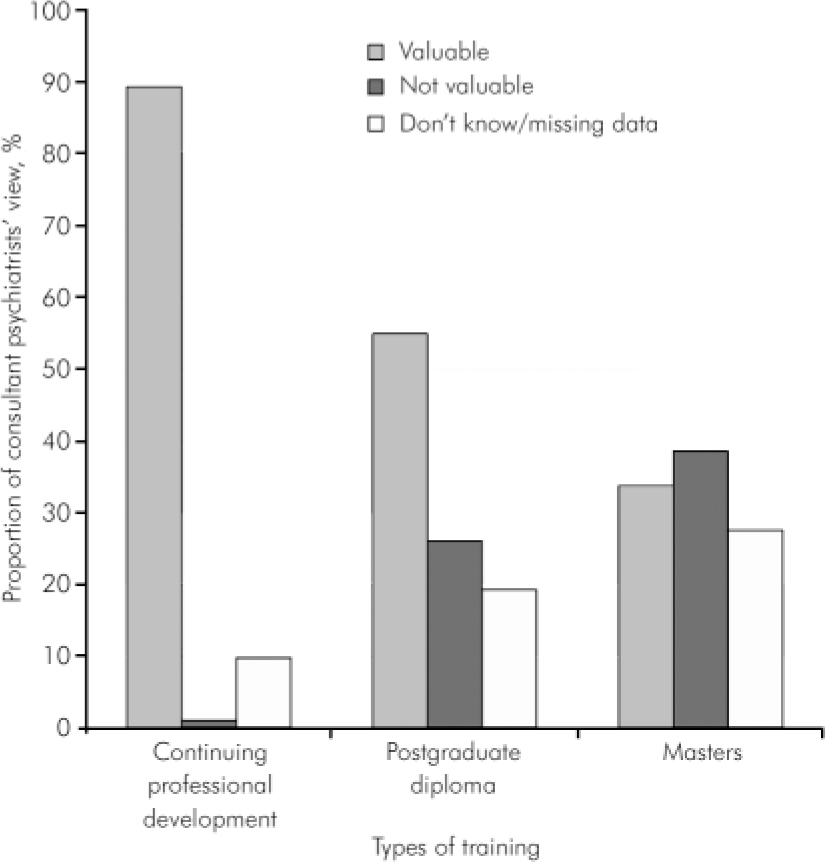
Fig. 1. Perceived value that consultants hold for different levels of potential neuropsychology training.
Discussion
The rationale for psychiatrists having training and knowledge in neuropsychology is endorsed and recommended by national and Royal College of Psychiatrists clinical guidelines, national integrated care pathways and by the Mental Welfare Commission for Scotland. This survey of Scottish consultant psychiatrists suggests that where specialist neuropsychology services exist, they are not perceived to be sufficient to deal with clinical demand. Consultant psychiatrists indicated that there are limited training opportunities in neuropsychology for psychiatrists and this seems reflected in their limited confidence in interpreting basic recommended neuropsychological assessment tools. There is a definite desire among consultant psychiatrists for postgraduate training opportunities, mostly for CPD modules, although various consultants of relevant subspecialties indicated that training at postgraduate diploma and masters’ degree level would be valuable. The authors share the recommendations made by the Mental Welfare Commission for Scotland that ‘Medical Directors of the Health Boards must ensure that all psychiatrists dealing with patients over the age of 18 are competent in the assessment and diagnosis of the full range of dementias they may encounter’ and their final recommendation that ‘all organisations providing medical education in mental health (Royal College of Psychiatrists, the Postgraduate Medical Education and Training Board and NHS Education Scotland) . . . should ensure that educational programmes address the issues of diagnosis, cognitive testing and the attitudes we have identified’. 9 Clinical guidelines and the results of this survey affirm that these recommendations should be relevant to all subspecialties of psychiatry. Tertiary educational institutions should consider broadening the access of formal neuropsychology training to psychiatrists.
Appendix
Consultant respondents (n = 288) per subspecialty (of which seven had ‘split posts’ involving two subspecialties)
| General adult and community psychiatry ………. | 102 |
| Psychiatry of old age …………………… | 63 |
| Liaison psychiatry ……………………… | 15 |
| Forensic mental health …………………… | 22 |
| Rehabilitation ………………………… | 12 |
| Child and adolescent psychiatry ……………. | 34 |
| Learning disability ……………………… | 15 |
| Addictions …………………………. | 9 |
| Other ……………………………… | 9 |
| Unanswered/spoiled ……………………. | 14 |
Declaration of interest
None.






eLetters
No eLetters have been published for this article.