Eating disorders are complex and potentially life-threatening psychiatric illnesses, characterised by disturbances in eating or eating-related behaviour leading to impairments in physical health and/or psychosocial functioning. 1,Reference Hambleton, Pepin, Le, Maloney and Aouad2 Globally, the lifetime prevalence rate for formally diagnosed eating disorders is estimated to be 8.4% (range 3.3–18.6%) for women and 2.2% (range 0.8–6.5%) for men. Reference Galmiche, Déchelotte, Lambert and Tavolacci3 Treatment for eating disorders is typically provided along a continuum of care, often commencing with regular out-patient consultations involving psychologists, primary healthcare providers and/or dietitians. Reference Crone, Fochtmann, Attia, Boland, Escobar and Fornari4 Instances of medical instability, suicidality or low treatment engagement may necessitate more intensive interventions, such as intensive out-patient treatment or in-patient hospital admission. Despite the development of evidence-based interventions, such as enhanced cognitive–behavioural therapy Reference Fairburn5 and family-based therapy, Reference Lock and Grange6 the course of eating disorders is commonly protracted with high rates of remission. Reference Miskovic-Wheatley, Bryant, Ong, Vatter and Le7 Long-term follow-up studies indicate that 30–64% of individuals who received in-patient treatment for an eating disorder still met diagnostic criteria 10–20 years following treatment. Reference Fichter, Quadflieg, Crosby and Koch8,Reference Quadflieg, Naab, Voderholzer and Fichter9
Current evidence indicates that, without improvements in both physiological and psychological aspects of an eating disorder, there exists a risk of a pseudo-recovery – that is, physical recovery in the absence of psychological recovery – and increased risk of remission. Reference Bardone-Cone, Hunt and Watson10 Thus, although medical safety is essential in ameliorating both psychological and psychosocial symptoms of an eating disorder, Reference Hay, Touyz, Claudino, Lujic, Smith and Madden11,Reference Voderholzer, Haas, Correll and Körner12 individual aspects are important to consider in predicting treatment adherence and patient outcomes. Reference Murray, Quintana, Loeb, Griffiths and Le Grange13 For example, stigma, shame and guilt are frequently identified as the most impactful barriers to individual motivation and subsequent treatment engagement, alongside practical barriers such cost of treatment and location. Reference Hamilton, Mitchison, Basten, Byrne, Goldstein and Hay14,Reference Daugelat, Pruccoli, Schag and Giel15 Furthermore, although many individuals with longstanding eating disorders are labelled as ‘treatment resistant’, Reference Kotilahti, West, Isomaa, Karhunen, Rocks and Ruusunen16 it is also possible these individuals may have been unable to access treatment tailored to their needs and preferences. Reference Hay and Mitchison17
Lived experiences of treatment
The gap between in-patient and out-patient treatment for eating disorders is substantial. Reference Miskovic-Wheatley, Bryant, Ong, Vatter and Le7,Reference Fichter, Quadflieg, Crosby and Koch8,Reference Hamilton, Mitchison, Basten, Byrne, Goldstein and Hay14 In-patient treatment programmes have traditionally centred on models of refeeding and medical stabilisation and weight restoration, employing a ‘one-size-fits-all’ approach to care. A recent review Reference Rankin, Conti, Ramjan and Hay18 exploring patients’ lived experiences of in-patient treatment for anorexia nervosa found that, although many individuals recognise the necessity of medical intervention, they often express feeling marginalised by the restrictive treatment environment and biomedical focus of in-patient treatment facilities. Reference Sibeoni, Orri, Valentin, Podlipski, Colin and Pradere19 Conversely, day- and out-patient treatment offers greater flexibility, but frequently lacks the resources and intensity needed to support recovery. This disparity underscores the need for integrated care models that facilitate continuity of support in this transition. Reference Hay, Touyz, Claudino, Lujic, Smith and Madden11,Reference Hamilton, Mitchison, Basten, Byrne, Goldstein and Hay14,Reference Hay and Mitchison17 The review Reference Rankin, Conti, Ramjan and Hay18 also highlighted the multifaceted nature of treatment experiences, and acknowledged the ‘inherent conflicts’ in balancing the necessity of medical and psychological intervention with person-centred approaches.
Residential treatment for eating disorders
Residential treatment programmes for eating disorders have gained popularity in recent years, expanding from the USA to countries such as Canada, Italy and Australia as well as the UK. Reference Fisher, Henretty, Cox, Feinstein, Fornari and Moskowitz20 These programmes offer intensive 24/7 treatment in a ‘home-like’ environment and are designed to support individual recovery over several weeks to months. A critique highlighted in the literature regarding in-patient and intensive treatment facilities is the presence of a dominant biomedical discourse that often disqualifies the voice and identity of the individual seeking treatment. Reference Eldal, Natvik, Veseth, Davidson, Skjølberg and Gytri21,Reference Twohig, Bluett, Torgesen, Lensegrav-Benson and Quakenbush-Roberts22 Residential treatment programmes typically place a stronger emphasis on fostering individual autonomy and psychological recovery than in-patient settings and, as such, are intended for individuals who are medically stable, but require a higher level of treatment intensity than what may be offered in the out-patient or day programme settings. Reference Peckmezian and Paxton23 Treatment in the residential setting is commonly provided by a multidisciplinary team and involves regular meal support, low-intensity medical monitoring, and individual and group psychotherapy using traditional evidence-based approaches such as cognitive–behavioural therapy, as well as adjunctive therapies such as yoga. Reference Peckmezian and Paxton23,Reference Clague, Conti and Hay24
A systematic review of 19 open-label trials Reference Peckmezian and Paxton23 and a large (n = 1421) retrospective clinical outcomes trial reported positive outcomes associated with residential-based treatments. A more recent scoping-review (n = 12) of outcomes associated with residential programmes for eating disorders found moderate to strong evidence to support positive outcomes for patients, such as eating disorder psychopathology, weight restoration, quality of life, anxiety, depression and cognitive functioning. Reference Clague, Conti and Hay24 Despite the growing number of residential programmes and evidence suggesting that residential facilities may be an effective modality of eating disorder treatment, there is a paucity of published literature exploring participants’ lived experiences of residential treatment for an eating disorder.
Study aims
Given the limited clinical evaluation in the literature, it is unclear if the aspirations of the residential model are meeting the perceived needs of those seeking treatment. As such, understanding participant lived experiences is crucial for the ongoing development of this model of care and improving treatment outcomes. This study aimed to explore the participant lived experiences of care at Australia’s first residential facility for the treatment of eating disorders.
Method
Ethics
The current study is a component of a wider clinical evaluation of the first residential treatment facility for the treatment of eating disorders in Australia. This study was registered with the Australian New Zealand Clinical Trials Registry (identifier ANZCTR12621001651875p). The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2013. All procedures involving human patients were approved by the Western Sydney University Human Research Ethics Committee (approval number H14742). All participants provided written and verbal informed consent.
Facility
Participants were recruited from a single residential facility for the treatment of eating disorders in Australia. The purpose-built facility is staffed by a multidisciplinary team who provide 24/7 residential care and support for up to 13 individuals in a home-like environment. The facility employs the Butterfly Foundation Residential Eating Disorder Treatment (BFREEDT) Model of Care, which is a six-phase treatment structure based on the work of Carolyn Costin Reference Costin and Grabb25 and underpinned by the principles of best practice outlined in The Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of eating disorders. Reference Hay, Chinn, Forbes, Madden, Newton and Sugenor26 Full admission criterion for the facility are outlined in Supplementary File 1.
Recruitment
All (n = 84) patients admitted for treatment during a 25-month period (July 2021 to August 2023) were invited to participate in a clinical evaluation of the residential facility. Consenting participants were contacted by the first author, following discharge, and invited to participate in an interview about their experiences of residential treatment. This was done to ensure equitable participation opportunities.
For pragmatic purposes, the authors anticipated a sample size of approximately 10% of admissions would be sufficient to generate adequate data to depict a nuanced and multifaceted picture of the patterns pertaining to participants’ lived experience of residential treatment. Reference Conti, Calder and Rankin27 Once this number was reached, recruitment continued in a reflexive manner until the researchers were confident there were multiple representations of a range of possible participant experiences – positive, mixed and negative – resulting in a sample of 17.86% of the total admissions. Recruitment and participation rates are shown in Fig. 1.

Fig. 1 Flow of participant recruitment.
Participants
Fifteen women (mean age 27.9 years, s.d. = 5.12) consented to participate in an interview about their residential treatment experience. The majority (n = 12) of participants identified as being Australian of Anglo European descent. Mean illness duration was 11.5 years from diagnosis (s.d. = 4.26; range 4–19 years) and mean length of admission was 74.89 days (n = 17; s.d. = 48.52 days). Approximately two-thirds of those interviewed (n = 9) described themselves as being actively engaged in recovery, with the remaining participants describing themselves as having experienced a setback or considering in-patient admission because of relapse. Two-thirds of participants were diagnosed with anorexia nervosa (majority 80% restrictive subtype) and a third with atypical anorexia nervosa. All participants reported multiple prior in-patient admissions for treatment related to their eating disorder diagnosis.
Data collection
Data were collected through a semi-structured interview following discharge from the facility. This approach was employed to safeguard participant confidentiality because of the limited number of eligible individuals, and to foster an environment conducive to open, reflective sharing of experiences, including challenges faced in the facility or milieu. The interview was purposefully designed by the authors in collaboration with a lived experience advisory group (see Supplementary File 2). The interview schedule was informed by a narrative therapy framework Reference White28 as outlined in the Experience and Identity Interview. Reference Burr29 This framework allowed participants to raise experiences, meanings and self-reflections that were pertinent to their lived experience of the service through a process of self-narration. Clinical diagnostic data were obtained from the electronic medical record.
All interviews were conducted by the first author, a clinical psychologist and researcher external to the facility, and lasted approximately 60 min (mean 60.47 min; s.d. = 2.25). To accommodate participant locations and scheduling preferences, interviews were conducted via Zoom (version 5.10.6–5.15.13 for Mac iOS, Zoom Communications, Denver, CO, USA; https://www.zoom.com) and audio recorded. Following the interview, participants were debriefed by the first author and reimbursed $50 for their participation.
Analysis
Interview recordings were transcribed and de-identified with participant-chosen pseudonyms. Further identifying information was removed (e.g. locations, dates, affiliations) following participants’ review of their interview transcript. De-identified transcripts were exported to NVivo (version 14 for Mac iOS, Lumivero, Denver, CO, USA; https://www.lumivero.com) and analysed with inductive reflexive thematic analysis within a social constructionist framework. Reference Braun, Clarke, Hayfield, Terry and Liamputtong30 This approach assumes a bidirectional relationship between language and experience, viewing language as integral to the social (re)production of participants’ meaning and experiences. The authors’ choice of a narrative therapy informed interview schedule was consistent with the reflexive analytic approach.
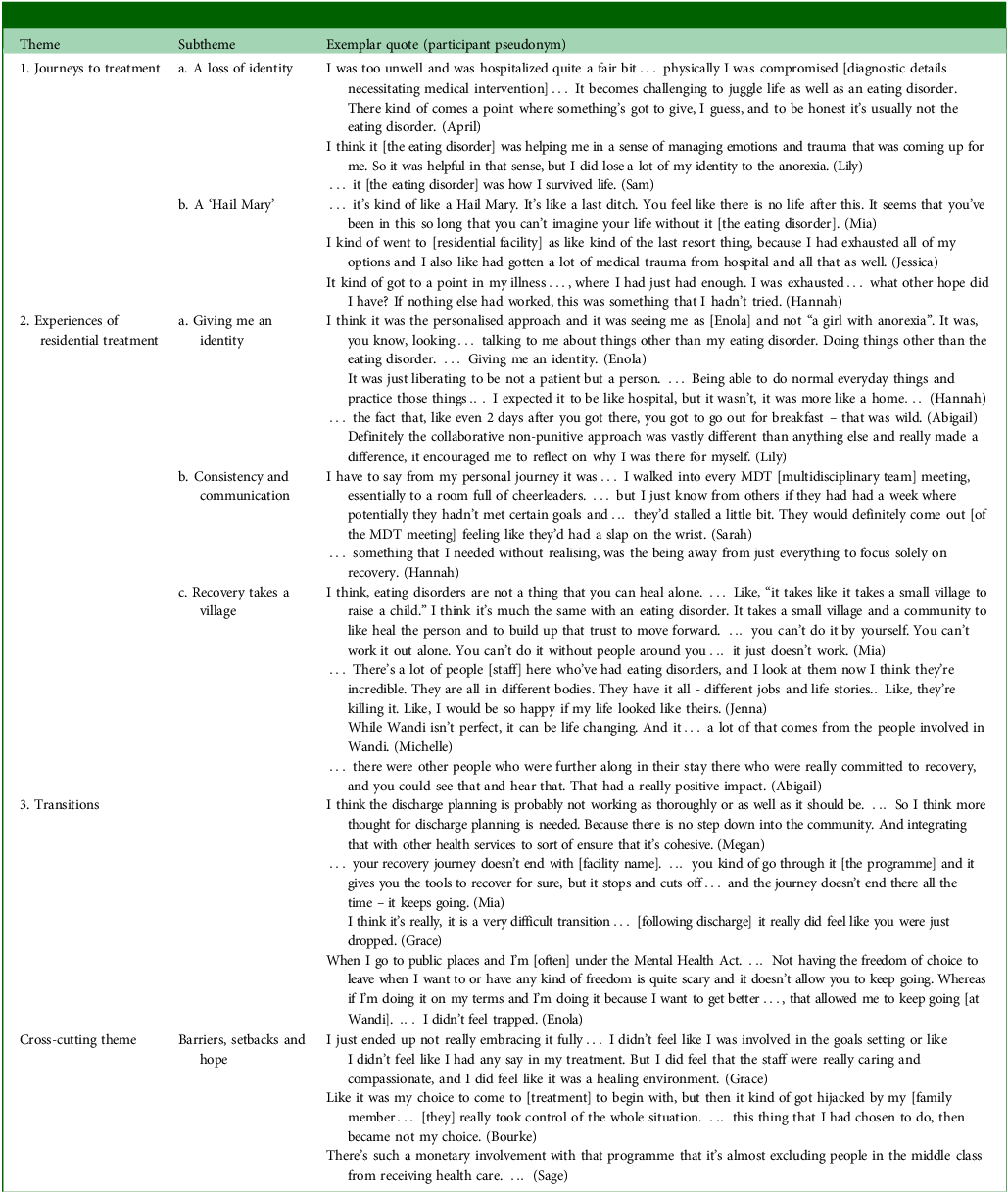
Transcripts were coded and a set of themes and subthemes developed (by R.R.) according to Braun and Clarke’s Reference Conti, Calder and Rankin27 six-phase approach to thematic analysis and reported in line with the Reflexive Thematic Analysis Reporting Guidelines. Reference Braun and Clarke31 Because of the exploratory nature of the research, an inductive coding approach was adopted that was driven by participant experiences rather than influenced by pre-existing theories or researcher preconceptions. Coding notes underwent collaborative review for overlapping and repetitive codes by the authors (R.R., J.C., L.R., P.H.) before being consolidated into themes. Similar themes were grouped together to identify major patterns in the data, thus forming overarching themes and subthemes. Extracts that most accurately represented the final set of themes (see Table 1) were incorporated into the analytical narrative to create a meaningful representation of participants’ experiences.
Positionality
In adopting reflexive thematic analysis within a social constructionist perspective, the authors acknowledge the influence of researcher positionality in the processes of data generation, analysis and presentation. Detailed author positioning statements can be found in Supplementary File 3.
Results
In exploring participants’ lived experiences of treatment at Australia’s first residential treatment facility for eating disorders, three themes and one cross-cutting theme were generated from the data. As depicted in Fig. 2, these themes are explored in narrative sequence following participants’ journeys to treatment (theme 1), experiences of residential treatment (theme 2) and the transitions associated with and following discharge (theme 3). Throughout their journey, participants encountered barriers, setbacks and hopes (cross-cutting theme 1). Exemplar participant extracts are presented in Table 1.

Fig. 2 Thematic map of participant experiences. CCT, cross-cutting theme.
Theme 1: journeys to treatment
Participants’ journeys to treatment were unique and varied. All participants reported complex and extensive treatment histories along the continuum of care, spanning several years to decades. Participant treatment histories were punctuated by in-patient treatment and experiences of restrictive practice, encapsulating a cycle akin to a ‘revolving door’ (Daphanie) of steps toward recovery followed by episodes of medical instability. Inherent within participant narratives was an acknowledgment of the necessity of medical in-patient interventions as part of their treatment journey. However, the treatment environment and biomedical focus of these facilities were often experienced as restrictive, leading to the disqualification of participants’ voices, individual identities, lived experiences, personal values and understandings of eating disorder symptoms. Thus, participants described a loss of identity along their treatment journeys and saw residential treatment as being a ‘Hail Mary’ (Mia).
Theme 1a: a loss of ‘identity’
When asked to share the story of their eating disorder, participants frequently reflected on the pervasive influence the eating disorder had on their lives. Participants frequently spoke of the perceived totality of the eating disorder, particularly when speaking to their treatment histories. Within these treatment histories, participants described a complex interplay between the disorder and their sense of self. Individual narratives painted a picture of complex and recursive identity negotiations as they sought to navigate a life that had become dominated by the eating disorder. In speaking on the impact of the eating disorder on their time, relationships, hobbies and careers, participants frequently reflected on how their identity became lost to the eating disorder identity. This sentiment was effectively encapsulated in Lily’s reflection: ‘… I did lose a lot of my identity to the anorexia’. Despite recognising the detrimental effects of the eating disorders, all participants outlined the struggle to imagine or contemplate the concept of a life without the eating disorder. These discussions highlighted participants’ perceived absence of personal agency to act on their own behalf in the face of their eating disorder and its effects on their life.
Theme 1b: a ‘Hail Mary’
Paralleling the participants’ experiences of the dominance of the eating disorder were narratives of resistance, for example having ‘had enough’ (Hannah) of the eating disorder and its increasingly untenable effects. Within the broader context of recursive treatment attempts, participants described looking for something ‘different’ from the continuum of treatment options available to them. Many individuals described having followed the development of the residential facility since its inception, several years before their admission, in the hopes that they would not need to access the treatment service. Within the broader context of their treatment journeys, participants viewed residential treatment as being like a ‘Hail Mary’ or ‘last ditch’ (Daphanie) attempt at holding on to hope for recovery and finding a life beyond the eating disorder.
Theme 2: experiences of residential treatment
As with their journeys to treatment, participants’ experiences of residential treatment for an eating disorder were unique and varied. In reflecting on their treatment experiences, participants rarely commented on a specific treatment modality, evidence-based intervention or behavioural changes. Rather, they almost exclusively reflected on themes of self, identity, connection and hoped-for futures.
Theme 2a: ‘giving me an identity’
A central tenet of the service’s treatment philosophy was the concept that each individual embodies both a ‘healthy self’ and an ‘eating disorder self’. As such, pivotal objectives of the programme enhanced participant recognition of these selves, with the aim of acknowledging the function of the eating disorder self and strengthening the healthy self. Reference Costin and Grabb25 When asked to reflect on their treatment experiences, participants rarely reflected on the language of healthy self or eating disorder self, but rather reflected on treatment as ‘giving me an identity’ (Enola). As such, individual experiences of treatment appeared to be less about the illness process and more about the reclamation of self and identity outside of the eating disorder.
Participants also spoke of treatment as being ‘collaborative’ and ‘non-punitive’. This approach, in combination with consistent and compassionately supported meal exposure, was experienced as helpful, particularly in the context of previous treatment experiences that were perceived as being ‘restrictive’ and ‘punitive’. Participants reflected that the individualised approach was empowering and had them feeling seen a person rather than ‘[just] a girl with anorexia’ (Enola).
Participants also frequently reflected on the value of being afforded the dignity of normality. For example, when participants spoke of the treatment environment, they frequently spoke of the value of normality in the small things such as being able to wear ‘normal clothes’ (Enola), the casual dress of staff, food being presented on ‘normal plates’ and in an aesthetically pleasing manner, being able to access the outdoors and the general warm home-like environment – ‘We called it the house’ (Hannah). Not only did the environment implicitly communicate safety, but it also allowed participants to communicate and experiment with the expression of their own unique identity through personal dress, interpersonal engagement and engagement in adjunctive therapies (e.g. equine, art, exercise and nature-based therapies).
Theme 2b: communication and consistency
As participants discussed communication and consistency in care, tensions emerged in their narratives between individual freedom and a desire for consistency and structure within treatment. Although all participants acknowledged the value of the personalised approach, a number also described how consistency in treatment approaches, including adherence and delivery of treatment non-negotiables Reference Geller and Srikameswaran32 and the quality of care received between staff members, created a sense of uncertainty. For example, although many participants expressed an initial disdain of treatment non-negotiables and aspects of the treatment environment they perceived as restrictive (e.g. limited access to telephones, only being permitted three disliked foods and the busy schedule), they also described the same environment as being instrumental in removing barriers and creating a space that allowed them to engage in treatment.
The weekly multidisciplinary team meetings were an area where inconsistencies in treatment experience were frequently noticed. Some participants found them to be ‘punitive’ and ‘disorganised’ (Bourke), whereas others felt they were walking into a ‘room of cheerleaders’ (Sarah). Several participants felt the feedback provided in the multidisciplinary team meeting was, at times, incongruent with the messaging they had received throughout the week. Numerous individuals voiced a desire to receive more regular feedback from staff throughout the week to help them understand their progress in relation to goals. Participants stressed the need for consistent communication, particularly in relation to treatment non-negotiables, progress and programme implementation, to foster a ‘safe’ environment. Thus, within participant narratives were ideological dilemmas Reference LaMarre and Rice33 that were embedded in the divergent philosophies that informed the endeavour to implement replicable standardised phase-based treatment protocols across the collective of participants and individualised and person-centred care.
Theme 2c: ‘recovery takes a village’
In speaking to their experience of residential treatment, participants most frequently commented on the value of relationships. A unique aspect of residential treatment for an eating disorder is living in a home-like environment and interacting with others experiencing similar difficulties. For many participants, the milieu and staff functioned as a formative experience that was central to the narrative of their treatment experience.
Participants frequently highlighted differences between their experience of the residential milieu and previous in-patient treatments. Several described residential care as offering community that fostered participant solidarity in their recovery while mitigating unhelpful comparisons that invited competitiveness around eating and body weight/shape. However, participants also described challenging aspects of the milieu, such as proximity to other participants who were at a lower weight and the everchanging dynamic within the milieu as participants entered and left the programme. Many participants also reflected on the pivotal role of the core process group. Offered three times per week, this psychotherapy group enabled participants to share recovery successes and challenges and address dynamics within the milieu, including managing interpersonal challenges and conflicts.
Participants also spoke on the value of the lived experience of others – including peers and lived experience staff members – in providing hope for recovery and snapshots of the many possible versions of recovery. The high level of lived experience personnel at the facility was universally seen as helpful, particularly the unique position of recovery navigator – peer support workers with lived experience of eating disorders who assist participants in navigating the programme by providing daily individual and group support, including meal assistance and engagement in therapeutic activities. Participants described recovery navigators as providing hope with their presence – ‘Seeing that they had existed past the point of having an eating disorder… that blew my mind’ (Lily) – in addition to being a ‘safe’, non-clinical person they could approach for practical advice and support.
Theme 3: transitions
Participants unanimously emphasised the necessity for enhanced discharge planning and community transition pathways. Discharge from residential treatment was described as ‘very difficult’ (Grace). Many participants reported finding it difficult or being unable to access and/or link-in with sufficient community treatment supports upon returning to their community. This was particularly evident for individuals who were interstate or from rural and remote regions.
Furthermore, all participants reflected on the loss of community and at times feeling ‘homesick’ (Michelle) for the residential treatment community, with several participants attributing the sense of ‘isolation’ (Mia) and lack of community as contributing factors to relapse following discharge. Within this context, participants unanimously expressed the need for continuity of care and collaborative discharge planning throughout the residential treatment journey. They advocated for improved discharge planning and community transition pathways. For example, having a step-down programme with reduced supports, moving to a community day programme on discharge or planned telephone check-ins following discharge.
Cross-cutting theme: barriers, setbacks and hopes
Treatment barriers were most frequently talked about in relation to financial barriers. Almost all participants spoke of only being able to access the facility through the financial support of their carers/family members, health insurance and/or a bursary. Individuals who left early, due to medical advice, or experienced relapse following discharge often cited finances as being a key barrier to either an extension of their stay – to complete higher phases of care – or considering readmission. Furthermore, interstate participants commented on logistical barriers, such as the location of the facility, being a significant consideration and barrier to access.
Treatment narratives were marked by internal conflict as individuals navigated a sense of liminality in their relationship with themselves and the eating disorder toward a rediscovery of self and identity. Participants consistently acknowledged their experience of residential treatment was shaped by their own motivation, readiness to change and hopes for a life lived differently. Participants who felt ‘forced’ to engage in treatment reported difficulty engaging in the programme. Conversely, those who independently made the decision to seek residential treatment were more likely to embrace the programme and report treatment goals being aligned with their own personal values and goals. Participants who discharged early spoke about the experience in ways that highlighted autonomy. For example, in reflecting on her decision to decline a treatment extension, Enola reflected on the dignity afforded by ‘doing’ treatment ‘on my own terms’, with the opportunity to leave ameliorating the sense of entrapment previously experienced in treatments.
Discussion
In contrast with people experiencing hospital care as disqualifying their identity, Reference Hamilton, Mitchison, Basten, Byrne, Goldstein and Hay14,Reference Rankin, Conti, Ramjan and Hay18 the present study found participants’ perceived residential treatment to be ‘giving identity’. This finding aligns with literature advocating for patient-centred and recovery-oriented care, 34 emphasising the importance of ‘seeing the person’ Reference Eldal, Natvik, Veseth, Davidson, Skjølberg and Gytri21,Reference Håkansson Eklund, Holmström, Kumlin, Kaminsky, Skoglund and Höglander35 , acknowledging the individual beyond their illness, and considering the roles of identity, relationships and environment.
Drawing on social constructionist frameworks, Reference Braun, Clarke, Hayfield, Terry and Liamputtong30 this study highlights the potential influence of social and environmental contexts on individual learning and identity within eating disorder treatment. Participant accounts echoed the growing body of literature suggesting that finding one’s identity outside of the eating disorder may be central to recovery, Reference Croce, Malcolm, Ralph-Nearman and Phillipou36 with participants stressing the value of collaborative care, consistency, communication and community within the residential setting in fostering identity. For many, the treatment milieu was experienced as a recursive source of hope. Participants spoke to finding hope for recovery in witnessing the recovery journeys of peers and having access to staff members with lived experience. These findings align with previous research suggesting the presence of lived-experience staff members and peer support workers may enhance individuals’ sense of hope or optimism for recovery, reduce stigma and improve motivation for treatment engagement. Reference Smit, Miguel, Vrijsen, Groeneweg, Spijker and Cuijpers37
Building on previous literature, Reference Fisher, Henretty, Cox, Feinstein, Fornari and Moskowitz20,Reference Peckmezian and Paxton23,Reference Clague, Conti and Hay24 this study found that although the core foundations of residential treatment may be similar to those provided in intensive out-patient or in-patient treatment programmes (e.g. psychoeducation, psychological therapy, nutritional rehabilitation, groups), the home-like environment distinguishes this model of care. Additionally, the non-punitive, relationally centred approach to treatment delivery further sets it apart. Moreover, this study underscores the significance of seemingly ‘small things’, such as clothing, presentation of food and facility furnishings, in fostering a sense of normality and safety within the treatment environment. Participants not only perceived the treatment environment as conveying safety, but also appreciated the opportunities it provided for expressing their identity through personal attire and participation in adjunctive therapies. These findings build on Verschueren and colleagues’ Reference Verschueren, Claes, Palmeroni, Raemen, Moons and Bruckers38 assertation that the treatment context and environment may facilitate patients in exploring and discovering their own identity.
Furthermore, similar to in-patient treatment, narratives revealed a tension between individual autonomy and standardised phase-based treatment protocols in a residential setting. Although participants acknowledged the necessity of treatment non-negotiables, they emphasised that the communication and consistency in their application profoundly influenced their treatment experience. As Geller and Srikameswaran Reference Geller and Srikameswaran32 noted, when ‘non-negotiables appear arbitrary, clients may view treatment providers as careless’, undermining confidence in the care team and negatively affecting the therapeutic alliance. Therefore, treatment non-negotiables, in a residential setting, may be best developed in response to the client population, treatment context and organisational values, with reflexive input from participants and clinicians. Integrating constant treatment protocols with individualised care and timely feedback may better support client autonomy while maintaining essential structure.
Residential care offers a unique opportunity to facilitate person-centred and recovery-oriented treatment that promotes self-determination and autonomy in the context of individualised, holistic and evidenced-based person-centred treatment, with participants in this study, for the most part, reporting feeling ‘seen’ and ‘empowered’ to be a part of their own treatment team. However, residential treatment remains only one option along the continuum of care. As such, identifying individuals who may benefit most from this form of treatment is critical given the significant financial and time-related barriers associated with residential care. Furthermore, as with in-patient treatment settings, Reference Voderholzer, Haas, Correll and Körner12,Reference Rankin, Conti, Ramjan and Hay18 inherent tensions arise between administering replicable standardised phase-based treatment protocols and participants’ desire for individualised person-centred care (e.g. treatment non-negotiables versus personalised care). Further research is needed to determine how these tensions may be navigated. Additionally, recovery – irrespective of its definition – does not exist in a vacuum. Reference LaMarre and Rice33,Reference Kenny and Lewis39 As such, intentionally integrated stepped care models of discharge planning may support individuals in receiving continuity of care and community upon transition to community care.
Limitations and future directions
A strength of this study was the recruitment from multiple participant cohorts over 2 years of service operation. However, the findings need to be interpreted in the context of participants being recruited from a single service, meaning they were required to meet specific intake criteria, such as medical stability. Additionally, there was limited diversity in eating disorder diagnoses, with two-thirds of participants diagnosed with anorexia nervosa, which reflects the broader demographics of those admitted. Furthermore, individuals who chose to participate may have experienced a heightened level of participant satisfaction or dissatisfaction with the service. Despite these limitations, by drawing on the voices of participants, this study offers new insights into individual lived experiences of residential treatment. Being a qualitative study, findings in this study should not be interpreted as a solution or diagnostic answer but seen as a representation of a set of individuals’ experiences. Reference Ho, Chiang and Leung40
Further research is needed to explore participant experiences in other residential services and should include diverse samples to better understand the impact of gender, culture, illness duration and diagnostic factors on treatment experiences. This may provide insight into who may benefit most from this model of care and how residential care may be further tailored to meet the needs of each individual. Additionally, exploring the perspectives of healthcare professionals, lived-experience staff members and caregivers may further enrich current understandings of residential treatment. An analysis of these experiences may play an important role in the future development of the model of care, with a view to improving treatment outcomes.
In conclusion, this study gives voice to the lived experience of those who engage in residential treatment for an eating disorder. Findings highlight the unique opportunity presented by the residential model as well as the inherent ideological dilemmas that arise when balancing replicable standardised phase-based treatment protocols with person-centred and recovery-oriented care. This study found that the residential model offers a unique opportunity to facilitate person-centred and recovery-oriented treatment that promotes self-direction and autonomy in the context of individualised, holistic and evidenced-based, person-centred treatment. However, residential treatment remains only one option along the continuum of care. As such, the importance of identifying individuals who may benefit most from this form of treatment is critical, given the significant financial and time-related barriers associated with residential care.
Supplementary material
The supplementary material is available online at https://doi.org/10.1192/bjo.2024.849
Data availability
The additional files contain the following data and materials for study: criterion of admission for treatment at time of study (Supplementary File 1), a summary of the lived experience advisory group (Supplementary File 2) and author reflexivity statements (Supplementary File 3). Exemplar data extracts for the themes and meta themes are presented in the findings (Table 1). In line with the ethics approvals for this study, original data that support the findings of this study are not publicly available as they contain information that could compromise the privacy and confidentiality of research participants.
Acknowledgements
The authors extend their sincere gratitude to the participants for sharing their experiences. Special acknowledgement is owed to the lived experience advisory group for their invaluable contributions. Furthermore, recognition is extended to the wider clinical evaluation research team, comprising individuals such as Deborah Mitchison, Sinead Day, Kathy Tannous, Warren Ward, Haider Mannan, Aunty Kerrie Doyle (First Nations Advisor), Elizabeth Dale (First Nations Advisor), Katherine Gill (Lived Experience Advisor), Natalie Valentine (Research Assistant) and various others, whose support was indispensable to this study.
Author contributions
R.R. assumed primary responsibility for study design, data collection, data analysis and manuscript composition, including development of all tables and figures. J.C. and L.R. functioned as consultants/supervisors to R.R. through all aspects of the study, including design, analysis and manuscript editing. P.H., serving as the Chief Investigator of the clinical evaluation, provided oversight for all phases of the study, from inception to final manuscript editing. All authors were active participants in the study design, analysis, editing and review of the manuscript.
Funding
The present study received funding from the Butterfly Foundation, including co-funding of two postgraduate research scholarships. The funding body was not directly involved in the design of the study, nor were they involved in the collection, analysis and interpretation of data, or in the writing of the manuscript.
Declaration of interest
R.R. is a doctoral student currently supported by the Western Sydney University Butterfly Foundation Postgraduate Research Scholarship, which is jointly funded by Western Sydney University and the Butterfly Foundation. She is also the recipient of a top-up scholarship from the Digital Health Cooperative Research Centre. P.H., J.C. and L.R. received funding from the Butterfly Foundation for the clinical evaluation of the Wandi Nerida programme. P.H. receives/has received sessional fees and lecture fees from the Australian Medical Council, Therapeutic Guidelines publication and Health Education and Training Institute (New South Wales and the former NSW Institute of Psychiatry). She has received royalties/honoraria from Hogrefe and Huber, McGraw Hill Education, Blackwell Scientific Publications, Biomed Central and PloS Medicine and research grants from the National Health and Medical Research Council and Australian Research Concil. She is Chair of the National Eating Disorders Collaboration Steering Committee in Australia (beginning 2019), was a Member of the International Classification of Diseases 11th Revision (ICD-11) Working Group for Eating Disorders and was Chair of the Clinical Practice Guidelines Project Working Group (eating disorders) of The Royal Australian and New Zealand College of Psychiatrists (2012–2015). She has been a consultant for Takeda Pharmaceuticals and has prepared a report under contract for Takeda (formerly Shire) Pharmaceuticals in regard to binge eating disorder (July 2017). All views in this paper are her own.







eLetters
No eLetters have been published for this article.