Ebstein anomaly is a rare and heterogenous disease often managed medically in neonates and infants, while surgery is often deferred due to high mortality and morbidity in early age. Reference Sharma, Habash and Mounsey1 Right ventricular dysfunction is a predictor of early mortality following surgery.
In patients with associated right ventricular outflow obstruction, the mortality increases up to 10% due to severe right ventricular failure. Reference Zack, Fender and Chandrashekar2,Reference Rankin, He and O’Brien3
Although complications during reoperations are very common, transcatheter procedures are very rare in children. Some limited numbers of adult cases have been published, but there is no data regarding transcatheter tricuspid and pulmonary valve implantation in children. We present a patient who was treated with a percutaneous tricuspid valve implantation followed by percutaneous pulmonary valve implantation in early childhood.
Clinical summary
An infant diagnosed to have Ebstein’s anomaly of tricuspid valve with severe pulmonary stenosis underwent balloon pulmonary valvotomy at the first month of life at another centre. A recurrence of severe outflow obstruction with tricuspid regurgitation warranted a surgical transannular patch repair of outflow with tricuspid ring annuloplasty using a 25-mm ring at 1 year of age (Ring brand did not specify in the operation report).
When the child aged 2 years and 10 months, he was symptomatic due to heart failure and presented to our clinic with tachycardia, tachypnoea, and hypotension. He was 11 kg (less than 3rd centile). On physical examination, liver was enlarged remarkably 4 cm below the costal margin. The gallop rhythm and diastolic murmur at left lower sternal edge were present. Cardiac enlargement was detected on chest radiography. Severe tricuspid and pulmonary regurgitation were detected on echocardiography. Tricuspid annulus measured 25 x 22 mm. Right atrium and right ventricle were dilated, and left ventricle was also diminutive (Fig 1). Cardiac MRI revealed right ventricular end-diastolic volume of 473 ml/m2 and right ventricular end-systolic volume of 352 ml/m2. The right ventricular ejection fraction was 25%, and the left ventricular ejection fraction was 46%. Left ventricular end-diastolic volume was 48 ml/m2 and end-systolic volume was 25 ml/m2.
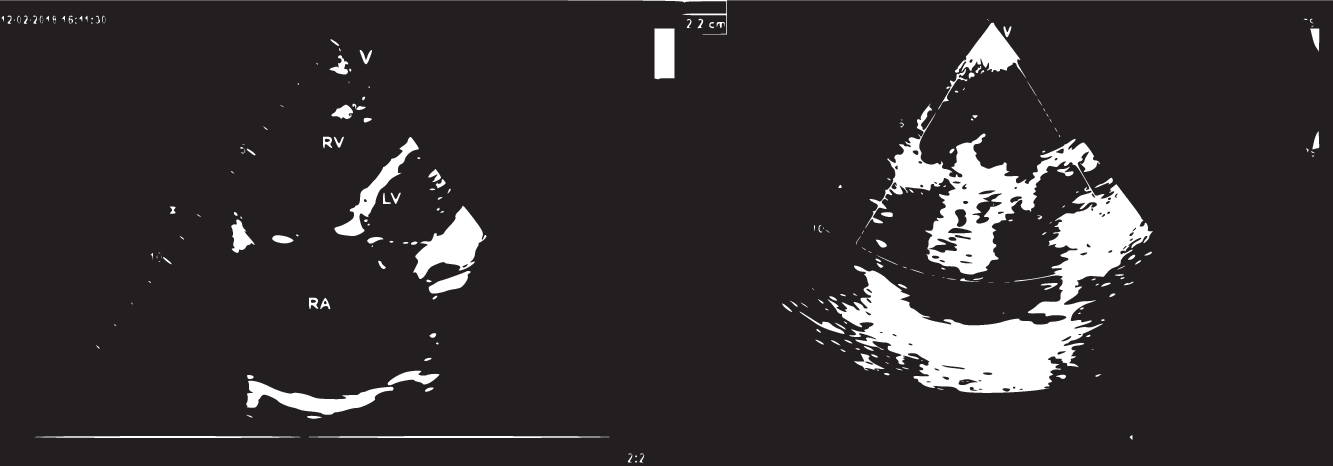
Figure 1. Transthoracic echocardiography reveals severe right atrial dilatation and severe tricuspid regurgitation by colour Doppler.
Since he had a medical history of previous surgery and unfavourable clinical evaluation for the open heart surgery, we decided to implant tricuspid valve by transcatheter approach. In view of high surgical risks posed by severe biventricular dysfunction during a redo sternotomy, we decided on a transcatheter tricuspid valve-in-ring implantation.
Under general anaesthesia, we surgically explored jugular vein by cutdown and placed 6F introducer sheath. Mean right atrium pressure was 14 mm Hg, and right ventricle systolic pressure was 25 mm Hg. Then by using Right Judkins catheter, a hydrophilic guide wire was placed in right pulmonary artery which was exchanged with a Lunderquist wire. The 14-F expandable sheath (e-sheath) (Edwards Lifesciences, Irvine, CA) was introduced into the superior vena cava and 26 mm SAPIEN S3 valve (Edwards Lifesciences, Irvine, CA) was advanced throughout the e-sheath over the Lunderquist wire up to tricuspid position, confirmed by transthoracic echocardiography. The valve was expanded by inflating the balloon under transthoracic echocardiographic guidance. The radiopaque ring which was implanted at the tricuspid position at previous surgery served as the landing zone during the procedure (Fig 2).
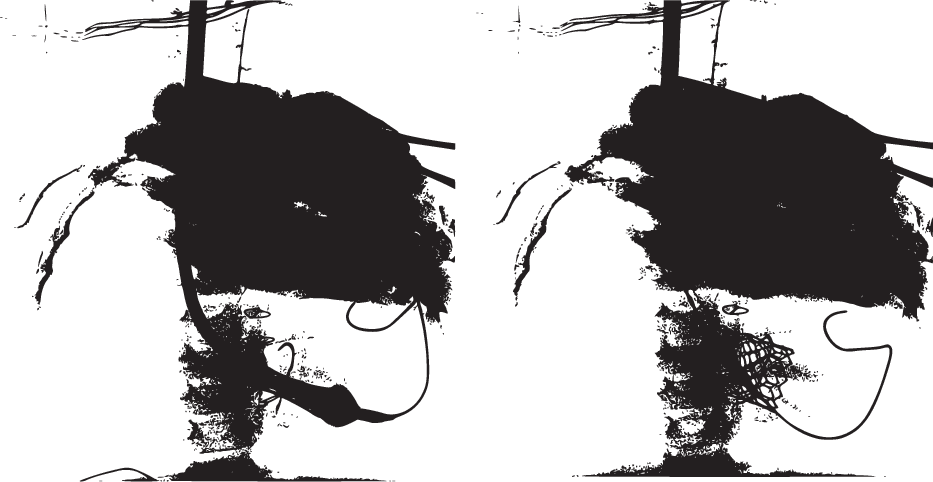
Figure 2. Inflating of the balloon valve assembly on the tricuspid valve position and Edwards S3 SAPIEN valve after implantation.
After the procedure, no complication occurred, and mild tricuspid valve regurgitation was detected by echocardiography. The patient was discharged on the second day of the procedure. 5 mg per kilogram of acetylsalicylic acid was started after implantation for antiaggregation.
At 1 year follow-up, the patient was asymptomatic and gained weight up to 14 kg. The right ventricular end-systolic volume, end-diastolic volume, and ejection fraction on cardiac MRI were 248.9 ml/m2, 333.0 ml/m2, 25.3%, respectively. Pulmonary regurgitation fraction was 42% on MRI. In view of right ventricular dilatation and dysfunction, we decided to implant a valve into the pulmonary position by transcatheter approach.
Under general anaesthesia, the procedure began with the exploration of jugular vein, and we introduced the catheter through the tricuspid valve. Mean right atrium pressure was 9 mmHg and right ventricle systolic pressure was 31 mmHg. Pulmonary artery systolic pressure was 28 mm Hg. Sizing balloon interrogation excluded compression of the coronary arteries. The waist on the balloon was measured 16 mm. The hydrophilic guide wire was advanced into the right pulmonary artery and exchanged with a Amplatz stiff wire. As there was no stenosis in the outflow, the valve implantation was planned without a prestent. The Melody® transcatheter heart valve (Medtronic, Minneapolis, MN) was advanced using a 20-mm ensemble delivery system until the appropriate position and expanded. After the procedure, there was no stenosis or regurgitation in the pulmonary valve (Fig 3). Patient has been followed for 2 years after percutaneous pulmonary valve implantation, and echocardiography shows still functional tricuspid valve and pulmonary valve without regurgitation. Patient reached 19 kg weight, and he is doing well.

Figure 3. Coronary interrogation by balloon testing, İnflation of the Valve Balloon assembly on pulmonary valve position, and competent Melody valve functions after implantation.
Discussion
In case of multiple surgery, Ebstein anomaly has high surgical mortality. Post-operative patients after surgical repair of Ebstein anomaly with severe tricuspid and pulmonary regurgitation and biventricular dysfunction have high surgical mortality during redo surgeries. Alternatively, transcatheter intervention avoids redo sternotomy and cardiopulmonary bypass. Reference Zack, Fender and Chandrashekar2–Reference Connolly, Schaff and Abel4
Percutaneous valve implantation is very rarely performed in children weighing under 20 kg. As far as we know, this was the smallest case in the literature who underwent percutaneous tricuspid valve implantation and percutaneous pulmonary valve implantation. Considering the patient’s low body weight, we preferred jugular vein access because of its larger size than the femoral vein and a shorter and straighter catheter course. Based on this experience, jugular vein approach offers an appropriate solution for small children.
Established 1-year mortality of after surgical pulmonic and tricuspid valve replacement in adult patients is around 30%. Reference Mokhles, van Herwerden and de Jong5–Reference Small, Aksoy and Levi7 . The follow-up in 3 years of the patient have revealed that transcatheter approach is a feasible and safe alternative to surgery in children. Since limited data exist about follow-up of the transcatheter valve replacement in children, this case is important to show alternative options for a high-risk redo surgery in small children. Tricuspid valve replacement as compared to repair has higher mortality rate and reoperation (12). In this case, transcatheter approach is also superior to surgical replacement. Even though the patient presented in extremis with cardiogenic shock, the outcome was rewarding, and symptoms disappeared soon after the procedure.
According to adult case series, the technical success and favourable clinical outcomes described here with combined percutaneous tricuspid valve implantation/percutaneous pulmonary valve implantation strongly suggest that this is a reasonable alternative to surgery. Reference Small, Aksoy and Levi7
We could have implanted both valves at the same session but since the clinical condition of the patient was not stable, we preferred to postpone the pulmonary valve implantation. On the other hand, we wanted to see the clinical and magnetic resonance improvement of the right ventricle in order to comprehend the optimal timing for the pulmonary valve implantation.
Valve choice for the tricuspid position was Edwards SAPIEN S3 valve obligatory, regarding larger size than Melody valve. Edwards SAPIEN S3 also has an advantage due to its smaller sheath size which is crucial for a small child. It is obvious that valvular ring which is used for the previous surgical annuloplasty created a safe landing zone for Edwards SAPIEN S3. Therefore, we did not perform stenting implantation for percutaneous tricuspid valve implantation. During tricuspid valve implantation, we are concerned of complete heart block due to compression of the conduction bundle. However, due to the existence of the previous ring in the tricuspid position, we have selected a smaller size of valve than the ring’s outer diameter to avoid this complication. In case of any AV block, we had transient pacemaker beside us for backup strategy. As for as the transcatheter pulmonic valve, we have chosen the Melody valve because it does not require stenting before valve implantation. Even though Melody valve fractures may be a complication without presetenting, since we have implanted the valve into the main pulmonary artery and transannular patch which is not strongly contractile we thought that the risk of fracture is negligible. The region of the transannular patch that created an indentation on balloon interrogation was the landing zone for Melody valve.
We should mention that the patient will need reintervention in the long term. However, the valve-in-valve procedure for both valves is still an available option in the future. Data regarding the longevity of transcatheter pulmonary and tricuspid valves are limited.
In conclusion, combined transcatheter tricuspid and pulmonary valve replacement can be performed successfully, even in small-weight children. Given the risk of operative intervention, this strategy is a reasonable alternative to surgery for appropriately selected patients.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conficts of interest
None.
Ethical standards
Informed consent form was obtained from the patient. Ethical committee approval was achieved from the Koc University Faculty of Medicine






