Following congenital heart surgery, infants often remain endotracheally intubated on mechanical ventilatory support upon arrival to the cardiac ICU. These patients undergo a trial of extubation when deemed safe. The decision-making process for extubation is quite complex. Reference Miura, Hamamoto, Osaki, Nakano and Miyakoshi1,Reference Chang, Hanley, Lock, Castaneda and Wessel2 Upon extubation, additional non-invasive modes of respiratory support such as high-flow nasal cannula and non-invasive positive pressure ventilation are commonly used to support these infants. Reference Richards-Belle, Davis and Drikite3,Reference Jayashankar, Rajan, Kottayil, Jayant and Balachandran4 Studies have shown approximately 3–27% of patients with CHD fail extubation after cardiac surgery. Reference Miura, Hamamoto, Osaki, Nakano and Miyakoshi1,Reference Gupta, Kuperstock and Hashmi5–Reference Gupta, McDonald and Goyal11 Risk factors for extubation failure are numerous such as complex surgical repair, younger age, smaller patients, presence of airway anomalies, genetic abnormalities, pulmonary hypertension, and phrenic and diaphragmatic nerve injury to name a few. Reference Jayashankar, Rajan, Kottayil, Jayant and Balachandran4–Reference Mastropietro, Cashen and Grimaldi7,Reference Sağıroğlu, Baysal, Copuroğlu, Gül, Karamustafaoğlu and Dogukan12–Reference Thiagarajan, Bratton, Martin, Brogan and Taylor14 Patients with CHD successfully extubated using non-invasive positive pressure ventilation have been shown to have shorter lengths of stay, Reference Gupta, Kuperstock and Hashmi5,Reference Kloth and Baum15–Reference Davis, Worley, Mee and Harrison17 while studies in preterm infants without CHD showed non-invasive positive pressure ventilation reduced extubation failure compared to high-flow nasal cannula. Reference Ferguson, Roberts, Manley and Davis18 Other studies have shown high-flow nasal cannula to decrease the need for intubation in infants with respiratory failure and may improve respiratory mechanics through unidirectional flow in the upper airway, decreasing dead space, improving minute ventilation, pulmonary compliance, and distending airway pressure. This support ultimately reduces the work of breathing and oxygen consumption, while enhancing oxygen delivery and gas exchange. Reference Mikalsen, Davis and Øymar19–Reference Mikalsen, Davis and Øymar23
Despite the use of high-flow nasal cannula and non-invasive positive pressure ventilation to support patients following extubation, there is limited data on the efficacy and superiority of either mode to prevent extubation failure in infants with CHD following cardiac surgery. We hypothesise that the use of non-invasive positive pressure ventilation will be associated with lower rates of extubation failure and a shorter length of stay when compared to high-flow nasal cannula. Our aims are to examine which mode of respiratory support (high-flow nasal cannula versus non-invasive positive pressure ventilation) after extubation is associated with lowest rates of extubation failure and examine risk factors that are associated with extubation failure in patients with CHD following cardiac surgery.
Materials and methods
Cohort selection
This single-centre retrospective cohort study included all infants (<1 year) and/or <10 kg who underwent CS for CHD from March 1st 2019, to March 31st 2020, at Children’s Healthcare of Atlanta, a free-standing university-affiliated quaternary hospital. An internal surgical database was queried, and eligible surgical encounters were identified. Preterm neonates with corrected gestational age of <35 weeks were excluded. All patients were admitted to the cardiac ICU post-operatively. This project was reviewed and approved by the Children’s Healthcare of Atlanta Institutional Review Board (study # 00000706). Informed consent was waived.
Demographics (age, weight, gender, and race), clinical characteristics (cardiac diagnosis, cardiac ICU length of stay, post-operative length of stay, hospital length of stay, duration of mechanical ventilation, respiratory support following extubation (high-flow nasal cannula versus non-invasive positive pressure ventilation), genetic syndrome, chromosomal abnormalities), and operative variables (cardiopulmonary bypass and cross-clamp times) were collected. Surgical procedures were categorised by complexity based on the Society of Thoracic Surgeons and the European Association for Cardio-Thoracic Surgery (STAT) Mortality Scores. Reference OʼBrien, Clarke and Jacobs24 Duration of mechanical ventilation was defined as the duration of time from intubation to the first extubation attempt. Extubation failure was defined as the need for reintubation within 48 hours from the initial extubation attempt. Respiratory support following extubation was dichotomised to high-flow nasal cannula versus non-invasive positive pressure ventilation. Patients remained assigned to the initial mode of respiratory support at time of extubation even if they required escalation to the alternative modality prior to reintubation. Mortality was defined as all deaths occurring during the hospitalisation in which the operation was performed; and all deaths occurring after discharge from the hospital, but before the end of the thirtieth post-operative day. Reference OʼBrien, Clarke and Jacobs24
Airway Management: All patients were endotracheally intubated with cuffed endotracheal tubes and placed on mechanical ventilation and on a standardised analgosedation protocol on admission from the operating room. Once spontaneously breathing, and extubation readiness determined, patients were placed on a spontaneous breathing trial using continuous positive airway pressure with pressure support. Following a successful spontaneous breathing trial, patients were extubated to non-invasive respiratory support at the discretion of the cardiac ICU physician ranging from high-flow nasal cannula to non-invasive positive pressure ventilation, with RAM interface (Neotech Products LLC. Valencia, CA). The analgosedation protocol is a standard of care where sedation is adjusted in a uniform way to avoid inherent bias related to sedation and optimise sedation use and avoid over-sedating patients following extubation and minimising sedation-related extubation failure.
Statistical analysis
Demographics were compared for patients with non-invasive positive pressure ventilation versus high-flow nasal cannula using chi-square and Fisher’s exact tests for categorical variables and using t-test and Wilcoxon rank sum tests for continuous variables. Logistic regression was conducted to determine the crude and adjusted odds ratios for extubation failure when comparing non-invasive positive pressure ventilation versus high-flow nasal cannula. Logistic modelling was also conducted stratifying the data into the following categories: weight ≤ or >5 kg and neonate versus non-neonate. All demographic and clinical variables were entered into a multivariable logistic regression model and eliminated one at a time using backward selection to produce the final adjusted model. A p-value of 0.05 was considered the cut-off for statistical significance. Statistical analyses were performed in SAS Enterprise Guide version 7.15 (SAS Institute, Inc., NC).
Results
Demographic data
There were 424 eligible patients during the study period. Patient characteristics are presented in Table 1. The median age was 97 days [interquartile range (IQR) 9–166], and median weight was 4.6 kg (IQR 3.3–6.1). Operations with STAT scores of 4 or 5 comprised 143 (34%) of all surgeries. The median duration of cardiopulmonary bypass and cross-clamp times were 109 minutes (IQR 78–143) and 65 minutes (IQR 39–91), respectively. The median cardiac ICU length of stay was 5 days (IQR 2–10), post-operative length of stay 8 days (IQR 5–18), and the median duration of mechanical ventilation was 21 hours (IQR 12–64). Chromosomal abnormalities were present in 27% and diagnosed genetic syndromes in 36% (Table 1).
Table 1. Patient characteristics stratified by type of respiratory support following extubation.
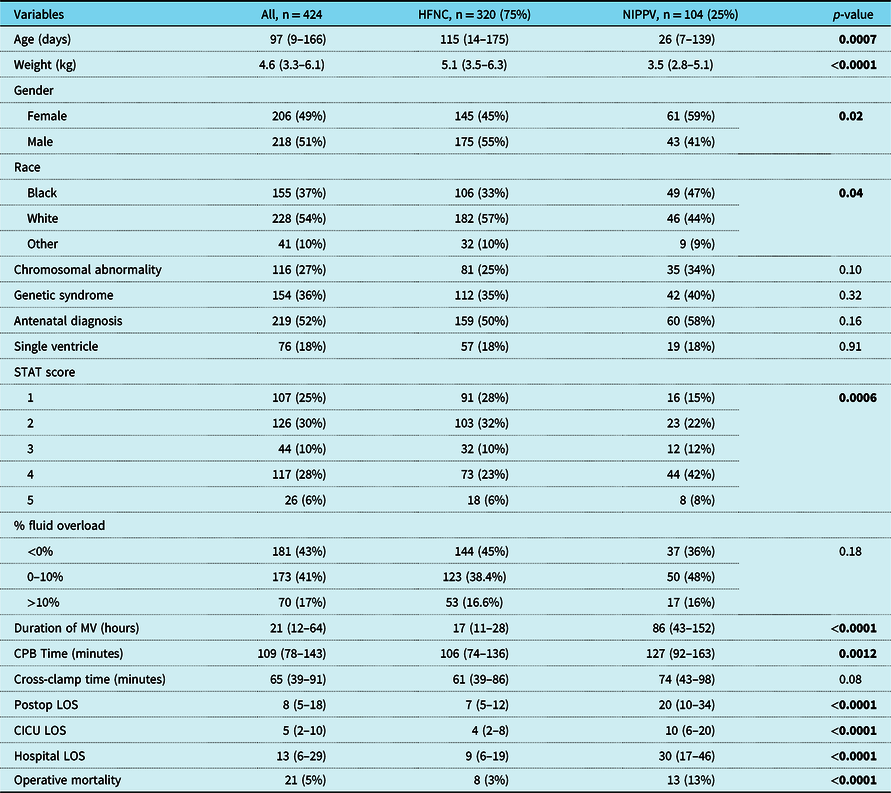
Results are depicted in n (per cent), median (interquartile range)
CICU LOS: Cardiac Intensive Care Unit Length of Stay; HFNC: High-Flow Nasal Cannula; LOS: Length of Stay; MV: Mechanical Ventilation; NIPPV: Non-invasive Positive Pressure Ventilation
Bold p-values are significant
Patients stratified by respiratory support after extubation
The 2 groups were high-flow nasal cannula versus non-invasive positive pressure ventilation. There were 320 (75%) patients in the high-flow nasal cannula group versus 104 (25%) patients in the non-invasive positive pressure group. The non-invasive positive pressure group were younger (median age 26 versus 115 days, p < 0.0007) and smaller (median weight 3.5 versus 5.1 kg, p < 0.0001) than the high-flow nasal cannula group (Table 1). The patients in the non-invasive positive pressure group had longer cardiopulmonary bypass time (median 127 versus 106 minutes, p 0.0012), longer cardiac ICU and hospital length of stay, and longer duration of mechanical ventilation (Table 1).
Of the 320 patients in the high-flow nasal cannula group, 34 (11%) failed extubation. Those who failed extubation were younger (median age 8 versus 125 days, p < 0.0001) and smaller (median weight 3.2 versus 5.3 kg, p < 0.0001), had longer cardiopulmonary bypass times (median 150 versus 103 minutes, p < 0.0001), longer cross-clamp time (median 93 versus 58 minutes, p = 0.0017), longer cardiac ICU and hospital length of stay, and longer duration of mechanical ventilation (Table 2). They were also more likely to have a higher STAT score of 4 and 5 (47% versus 20%, and 15% versus 5%, p < 0.0001 respectively), and antenatal diagnosis (71% versus 47%, p 0.01). Those who failed extubation in the high-flow nasal cannula group had a higher mortality rate (12% versus 1%, p = 0.0003) when compared to those who did not fail (Table 2).
Table 2. Patient characteristics in the high-flow nasal cannula (HFNC) group stratified by extubation failure.
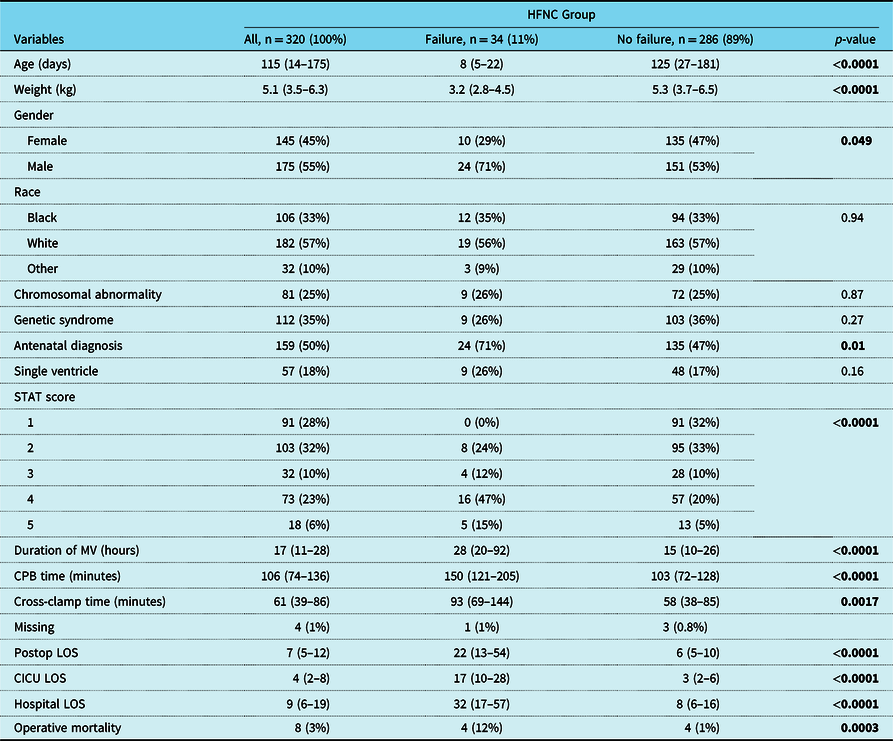
Results depicted in n (per cent), median (interquartile range)
CICU LOS: Cardiac Intensive Care Unit Length of Stay; HFNC: High-Flow Nasal Cannula; LOS: Length of Stay; MV: Mechanical Ventilation
Bold p-values are significant
Of the 104 patients in the non-invasive positive pressure group, 30 (29%) failed extubation. Those who failed extubation had longer duration of mechanical ventilation (median 137 hours versus 72, p = 0.03), longer cardiac ICU length of stay (median 24 versus 9, p = 0.0004), longer post-operative length of stay (median 36 versus 16, p = 0.0001), and higher mortality (30% versus 5%, p = 0.0006) (Table 3).
Table 3. Patient characteristics in the non-invasive positive pressure ventilation (NIPPV) group stratified by extubation failure.
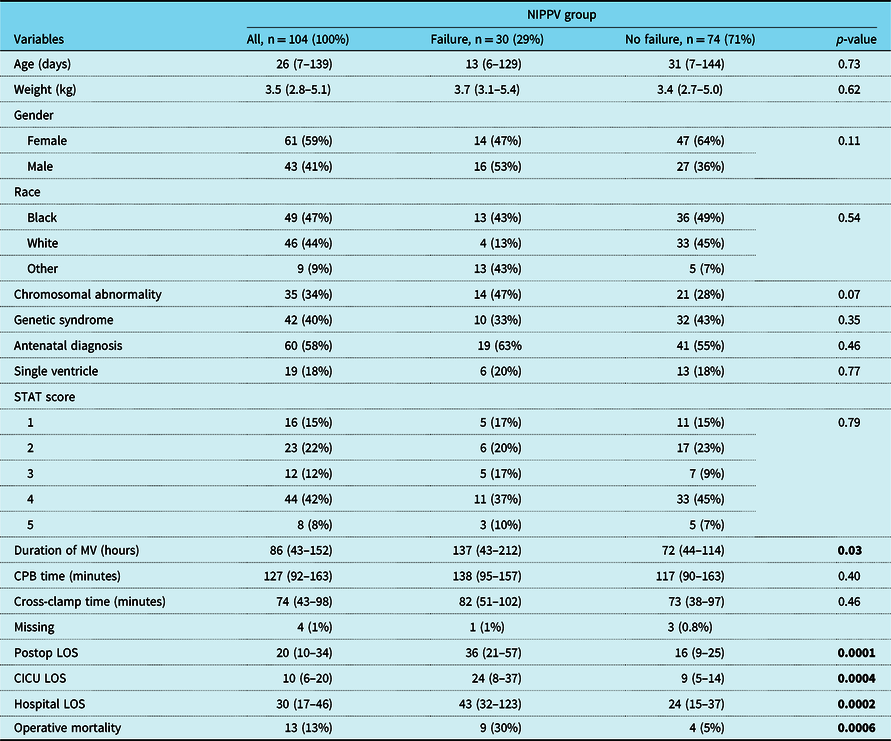
Results depicted in n (per cent), median (interquartile range)
CICU LOS: Cardiac Intensive Care Unit Length of Stay; HFNC: High-Flow Nasal Cannula; LOS: Length of Stay; MV: Mechanical Ventilation
Bold p-values are significant
The most common aetiology of extubation failure was upper airway obstruction 69%, followed by deconditioning/weakness 23%, and atelectasis 11% in the entire cohort (Table 4). These findings were similar in both the high-flow nasal cannula and non-invasive positive pressure ventilation groups respectively (Table 4).
Table 4. Etiology of extubation failure.

Results depicted in n (per cent)
HFNC: High-Flow Nasal Cannula; NIPPV: Non-invasive Positive Pressure
Bold p-values are significant
Logistic regression analysis
Using a multivariable regression analysis controlling for age, gender, race, cardiopulmonary bypass times, STAT category, and duration of mechanical ventilation to compare outcomes of extubation failure between both groups (high-flow nasal cannula versus non-invasive positive pressure ventilation), we found that patients extubated to non-invasive positive pressure ventilation had 3.30 higher odds (95% CI 1.56–6.96, p < 0.0001) to fail extubation when compared to high-flow nasal cannula group (Table 5).
Table 5. Crud and adjusted odds ratio for extubation failure by support type.
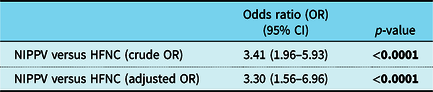
Adjusted for age, race, gender, STAT score, duration of mechanical ventilation, and CPB time
Bold p-values are significant
Logistic regression model demonstrated patients extubated to non-invasive positive pressure ventilation and >5 kg had 14.7 greater odds (95% CI 2.88–75.39, p = 0.0012) to fail extubation when compared to high-flow nasal cannula (adjusting for race, gender, STAT score, duration of mechanical ventilation, and cardiopulmonary bypass time). Non-neonates supported with non-invasive positive pressure ventilation had 21.7 higher odds (95% CI 5.16–91.20, p < 0.0001) to fail extubation when compared to high-flow nasal cannula (adjusting for race, gender, STAT score, duration of mechanical ventilation, and cardiopulmonary bypass time) (Table 6).
Table 6. Crude and adjusted odds ratio for non-invasive positive pressure ventilation (NIPPV) versus high-flow nasal cannula (HFNC) respiratory support type, stratified by weight, and neonates.

Adjusted for race, gender, STAT score, duration of mechanical ventilation, and CPB time
Bold p-values are significant
Discussion
Our study showed an association between high-flow nasal cannula and lower rates of extubation failure compared to non-invasive positive pressure ventilation when adjusting for patient factors in a multivariate analysis. There was an extubation failure rate of 15% (64/442) within 48 hours in our cohort. Risk factors associated with extubation failure were smaller, younger, and higher risk surgery patients, with longer cardiopulmonary bypass and cross-clamp time which contributed to longer length of stay and mortality.
At the outset of this study, our hypothesis was that non-invasive positive pressure ventilation would be associated with lower extubation failure. This was based on an assumption that higher pressures would provide adequate distending pressures and support these patients through the extubation process. However, after adjusting for age, race, gender, STAT score, duration of mechanical ventilation and cardiopulmonary bypass times, we found patients extubated to non-invasive positive pressure ventilation had 3.30 higher odds of failing extubation when compared to high-flow nasal cannula after extubation. This surprising finding was contrary to other studies reporting less extubation failure with non-invasive positive pressure ventilation, although these studies excluded critically ill cardiac neonates and children. Reference Aghai, Saslow and Nakhla25,Reference Lemyre, Davis, De Paoli and Kirpalani26 Our report is the largest cohort of neonates and infants studying high-flow nasal cannula versus non-invasive positive pressure ventilation to prevent extubation failure. Jayashankar et al showed high-flow nasal cannula was comparable to non-invasive positive pressure ventilation (bi-level ventilation in particular) in preventing extubation failure in patients following cardiac surgery. Reference Jayashankar, Rajan, Kottayil, Jayant and Balachandran4 However, this report examined 100 patients (50 patients in each group). While this study was a well-designed retrospective study, the lack of similar findings could be due to the smaller sample size. Our study included a total of 424 patients (320 patients in the high-flow nasal cannula group, and 104 patients in the non-invasive positive pressure group).
Further analysis of each group, controlling for patient variables and stratifying by weight (<5 kg versus >5 kg), showed patients >5 kg extubated to non-invasive positive pressure had 15 times higher odds of extubation failure compared to high-flow nasal cannula group and 22 times higher odds in non-neonates, further suggesting that larger patients may fare better being extubated to high-flow nasal cannula rather than non-invasive positive pressure ventilation. It is possible there may be physiological benefits of high-flow nasal cannula for these patients such as the delivery of high gas flow to washout pharyngeal dead space, reducing nasopharyngeal resistance, improves lung compliance by providing positive airway pressure, all of which improve work of breathing and support respiratory dynamics.
Prior reports described extubation failure rates of 15–20% in critically ill children and 3–27% following cardiac surgery. Reference Miura, Hamamoto, Osaki, Nakano and Miyakoshi1,Reference Gupta, Kuperstock and Hashmi5,Reference Mastropietro, Cashen and Grimaldi7–Reference Gupta, McDonald and Goyal11,Reference Harrison, Cox, Davis, Piedmonte, Drummond-Webb and Mee27 Neonates and infants with higher mortality after extubation failure were likely due to these patients with more vulnerable physiology. Reference Miura, Hamamoto, Osaki, Nakano and Miyakoshi1,Reference Jayashankar, Rajan, Kottayil, Jayant and Balachandran4,Reference Laudato, Gupta, Walters, Delius and Mastropietro13,Reference Fontela, Piva, Garcia, Bered and Zilles28 In our cohort, the overall mortality rate was 5% (21/424) with a mortality rate of 8% (8/320) in the high-flow nasal cannula group and 13% (13/104) in the non-invasive positive pressure group. Those who failed extubation had a much higher mortality rate 12% (4/34) and 30% (9/30), respectively. It is unclear if extubation failure is a sign of mortality risk versus an antecedent cause as it relates to severity of illness and complexity of patient hospital course. Also, consistent with our findings, previous studies have also shown smaller and younger patients with longer duration of mechanical ventilation and length of stay were at higher risk of extubation failure. Surgical risk factors associated with extubation failure in our cohort likely reflected the fragile state and tenuous physiology of this age group and were consistent with previous studies. Reference Miura, Hamamoto, Osaki, Nakano and Miyakoshi1,Reference Laudato, Gupta, Walters, Delius and Mastropietro13,Reference Davis, Worley, Mee and Harrison17,Reference Harrison, Cox, Davis, Piedmonte, Drummond-Webb and Mee27–Reference Baisch, Wheeler, Kurachek and Cornfield29
This study is subject to the typical limitations inherent to single-centre retrospective cohort studies. As a single-centre study, the demographics, clinical characteristics, as well as surgical and medical management of these patients are specific to our institution and might not be generalisable to other healthcare systems. Ventilation weaning protocols and extubation readiness testing may be institution-specific. Also, we compare in our study high-flow nasal cannula versus non-invasive positive pressure ventilation using nasal RAM interface, which is a common practice in some cardiac ICU, but not a widely adapted respiratory interface. Also, the choice of respiratory support mode was at the discretion of the cardiac ICU team taking care of the patients and this might have added bias in the selection of one mode over the other. This is a difficult property to control for when conducting retrospective studies as personal training, and clinical experiences, and patient clinical condition and complexity of hospital course all factor in when deciding which mode to use after extubation adding the potential for selection bias. Despite these limitations, this large cohort of patients with CHD can shed light on post-cardiac surgery respiratory support.
In conclusion, extubation failure is common in infants following cardiac surgery with smaller, younger infants, and those with higher risk surgical procedures at highest risk. There were no racial, ethnic, or socio-economic risk factors associated with extubation failure. Overall, patients extubated to non-invasive positive pressure ventilation had 3.30 higher odds of failing extubation versus patients extubated to high-flow nasal cannula. Furthermore, patients weighing >5 kg and non-neonates who were extubated to non-invasive positive pressure ventilation had even higher odds of failing extubation when compared to similar patients extubated to high-flow nasal cannula. Based on these findings, clinicians may need to re-evaluate their extubation practices. It is difficult to draw a definitive conclusion regarding the optimal type of respiratory support in these patients; however, these findings contribute to the literature and make a compelling case for a prospective trial in this fragile population. Currently, our institution is undergoing such a study to further clarify this important aspect of critical care support following cardiac surgery.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and have been approved by the institutional committees (Institutional Review Board at the Children’s Healthcare of Atlanta).









