Introduction
Pandemic restrictions have imposed both hardships and inconveniences in everyday life. People have entered a new ‘normal’ life with masks and social distances, hoping for the arrival of a vaccine. However, potential risks are everywhere and cannot be ignored. As the largest group of health care workers, nurses are on the frontline of the health care system's response to COVID-19 and experience several potential risks during nursing operations (WHO, 2020a). Due to nurses providing care in close physical proximity, they experience an increased risk of developing the disease because they are often directly exposed to viruses. Unfortunately, they have no choice but to confront inherent threats; otherwise, an unescapable tragedy would happen.
Risk perceptions of nurse clinicians
Nurses' risk perceptions are a crucial factor affecting their work attitudes, willingness, quality of nursing care, job satisfaction, and prosocial behaviors. The notion of perceived risk to health professionals during pandemics has been explored in the literature (Koh et al., Reference Koh, Hegney and Drury2011), yet fewer studies report data about nurse clinicians, as distinct from other health professionals. Nurses' risk perceptions refer to their knowledge, feelings, and understanding of risk factors or risk characteristics in the profession. Generally, it is a suitable mental and behavioral reaction for nurses. To some extent, individuals must be aware of the disease, acknowledge their vulnerability to it, and safeguard themselves with prevention methods or treatment (Homko et al., Reference Homko, Santamore, Zamora, Shirk, Gaughan, Cross, Kashem, Petersen and Bove2008). Referring to the health belief model (Rosenstock, Reference Rosenstock1974; Janz and Becker, Reference Janz and Becker1984; Champion and Skinner, Reference Champion and Skinner2008), risk perception is deemed personal beliefs about the likelihood of suffering a disease. Individuals who perceive a high level of susceptibility to a particular disease will adopt necessary measures to reduce the risk of developing it; individuals with low perceived susceptibility may deny that they are at risk for contracting a particular illness (Janz and Becker, Reference Janz and Becker1984). In other words, risk perceptions could prevent people from engaging in risky behaviors. For example, people show various levels of risk perceptions that could predict their preventive behaviors, and with risk exaggerators describe high preventive behaviors (Wang et al., Reference Wang, Chen, Chang, Wu, Lu and Yen2021). However, for those occupied in high-risk work environments such as nurse clinicians, the risk perceptions of health problems or other potential dangers would, either subconsciously or consciously, disrupt their work or discourage them. Therefore, risk perceptions about the pandemic can play a critical role in medical practices.
The risk perceptions of nurse clinicians for COVID-19
During the pandemic, nurses' knowledge of the disease was messy, and their attitudes and practices were disrupted; therefore, their risk perceptions were affected. Being infected, transmitting the infection to family members, acknowledging the stigma about the vulnerabilities of their job, and restrictions on personal freedom have been reported as key concerns in previous studies (Chiang et al., Reference Chiang, Chen and Sue2007; Seale et al., Reference Seale, Leask, PoC and MacIntyre2009; Hope et al., Reference Hope, Massey, Osbourn, Durrheim and Turner2011; Koh et al., Reference Koh, Hegney and Drury2012). Complicating the situation for nurses working in clinics during COVID-19 are the logistical issues related to the supply of personal protective equipment and shortages of other necessary resources to support service delivery (Xie et al., Reference Xie, Tong, Guan, Du, Qiu and Slutsky2020). For nurses who remain in clinical practice, an obvious impact relates to psychosocial ramifications. As a repeated cross-sectional study on frontline workers in a COVID-19 hub-hospital reported, during the first wave, workload and compassion fatigue increased (Magnavita et al., Reference Magnavita, Tripepi and Prinzio2020); with the development of the crisis, the heavy workload, isolation at work, uncertainty about safety procedures, and the abrupt decline in the time devoted to meditation and relaxation evolved to become prevalent causes of occupational stress (Magnavita et al., Reference Magnavita, Soave and Antonelli2021a); one year after the baseline, an increased workload, isolation at work and in social life, lack of time for physical activity and meditation, and compassion fatigue are still reported in health workers and coexist with new worries for justice in safety procedures (Magnavita et al., Reference Magnavita, Soave and Antonelli2021b). However, there is a significant variation in the extent to which nurses perceive risk in the clinical environment or events. Surveys have reported that fewer people have a high perception of risk related to the virus itself, while more people indicate stress caused by concerns related to pandemic-associated responses (Cornelia et al., Reference Cornelia, Wieler and Katrine2020). Moreover, some nurses on the frontline may show fewer worries and fears for their safety since they believe in the effectiveness of their protective equipment, while many nurse clinicians, not at the frontline, that encounter issues with ineffective and insufficient medical protection, fidget and become discomposed (Risti et al., Reference Risti, Hini, Bankovi, Koovi and Gavrilovi2020). Risk perception is a mental psychological construct that is subject to cognitional, emotional, sociocultural, political, and personal variabilities (Linden, Reference Linden2014, Reference Linden2015; Samadipour et al., Reference Samadipour, Ghardashi and Aghaei2020). Moreover, potential risks are not all concurrent. This has led to an increased interest in understanding how nurse clinicians perceived their risks for COVID-19. Are there subgroups of nurse clinicians who present with similar patterns of perception co-occurrence? If so, do these subgroups share characteristics that can be identified as indicators for their risk perceptions patterns and extent? Notably, the extent of risk perceptions closely related to the nurses' motivation for their clinic work and practice could have important implications for health care defense. Hence, assessing the risk perceptions of nurse clinicians for COVID-19 and its factors is indispensable.
Psychological impacts of COVID-19 on nurses
In addition, the pandemic has affected nurses' risk perceptions through their mental and psychological constructions. Individuals' emotions and instincts affect their perceptions, and they acquire these perceptions through observations, analysis of circumstances, and scientific consultations (Aakko, Reference Aakko2004). It is well-established that the pandemic and its restrictions have led to psychosis and have harmed the well-being and mental health of many nurses without exception. Worse still, people already experiencing distress are affected even more negatively (Osofsky et al., Reference Osofsky, Osofsky and Mamon2020; Yancy, Reference Yancy2020). Risk perception has its roots in psychological constructures and lies in continuity between no risk and high risk, positively and negatively affecting the decision-making (Chaiklin, Reference Chaiklin1987; Aakko, Reference Aakko2004; Kendra and George, Reference Kendra and George2010). Furthermore, the cognitive and decision-making abilities of nurses are influenced by their own emotions (Shirey, Reference Shirey2010; Standing, Reference Standing2010; Radtke et al., Reference Radtke, Tate and Happ2012; Magnavita et al., Reference Magnavita, Tripepi and Prinzio2020), which informs us of the potential relationship between nurses' psychological status and their risk perceptions. Initial psychological studies of COVID-19 showed that symptoms of depression and anxiety were present in most health care workers (Magnavita et al., Reference Magnavita, Tripepi and Prinzio2020; Que et al., Reference Que, Shi, Deng, Liu, Zhang, Wu, Gong, Huang, Yuan and Yan2020; Santamaria et al., Reference Santamaria, Jauregizar, Redondo, Etxebarria and Picaza2020). A systematic review and meta-analysis of articles related to COVID-19 identified poor sleep quality, stress, psychological distress, insomnia, post-traumatic stress disorder (PTSD), anxiety, and depression (Kontoangelos et al., Reference Kontoangelos, Economou and Papageorgiou2020). Moreover, a one-year prospective study also found that 73% of investigated doctors reported high levels of distress, 64% reported depression, 28% reported sleep problems, and 25% reported anxiety (Magnavita et al., Reference Magnavita, Soave and Antonelli2021b). Notably, stress and anxiety can evolve into acute stress disorder and precede chronic PTSD. Depressive symptoms are likely to follow chronic unresolved anxiety. Anxiety and depressive symptoms may include constant fear, excessive worrying, poor concentration, disturbances in sleep or appetite, low energy or fatigue, and decreased motivation (Skarl, Reference Skarl2015). To our knowledge, worsened psychological states could impair cognitive processes and individual characteristics, which are elements of risk perceptions. However, the psychological impacts of COVID-19 on nurse clinicians and their association with nurses' risk perceptions are scarcely reported. Therefore, advancing our understanding of the relationship between the prevalent psychological outcomes (including PTSD, depression, anxiety, and insomnia) and characteristics of risk perceptions has significant clinical references.
The present study
Understanding the factors that impact the risk perceptions of nurse clinicians is essential to inform future workforce policy and institutional responses. Hence, this study sought to extend on previous work to examine the relationship between the psychological impact of COVID-19 and the pandemic-associated risk perceptions of nurse clinicians. We proposed our hypotheses that poor psychological responses to COVID-19 in nurses could relate to high-risk perceptions and that people with a similar level of risk perceptions may complain of psychological problems to varying degrees. Additionally, risk perception is one of the vital factors related to nurses' willingness to perform clinical care (Chaffee, Reference Chaffee2009; Khalid et al., Reference Khalid, Khalid, Bhimani, Bhimani, Khan, Choudry and Mahmood2021). Therefore, we speculated that poor psychological responses and high-risk perceptions indicated a high likelihood of being discouraged to perform clinical care duties and that immediate intervention should be considered. Meanwhile, previous studies have identified individual characteristics, and sociodemographic and exposure-related variables that differentially predict risk perceptions (Rosenstock, Reference Rosenstock1974; Champion and Skinner, Reference Champion and Skinner2008), and our analyses also considered these factors.
Methods
Participants and procedures
This cross-sectional study was conducted in Jiangsu Province, China. Data were collected in early January 2021, one year after the outbreak of the COVID-19 infection. Nurse clinicians from five local hospitals in Jiangsu Province were recruited with the help of nursing clinical directors, who distributed the survey website in their working groups. Therefore, a random cluster sampling was used in the study. All the hospitals had admitted COVID-19 confirmed or suspected patients during the peak of the epidemic and no COVID-19 patients at the time of the survey. Finally, a total of 707 nurses voluntarily participated in the study and finished the survey. The inclusion criteria for valid questionnaires were as follows: the nurse clinician should (a) be a nurse in the hospital in the COVID-19 pandemic year (2020–2021); (b) have no history of mental disorder including depression or anxiety disorders diagnosed before the COVID-19; and (c) be at least 18 years old. These three questions were presented on the first page of our online survey, and only those who answered ‘yes’ to these questions could continue to the next page. The exclusion criterion included those with missing values in any studied variables. Finally, 668 participants were included in the analysis, and their working experiences were also collected. Ethical approval was obtained from the Second Military Medical University before the initiation of the research project. Before the online survey, all participants received informed written consent and were told that they could withdraw at any time. Additionally, anonymity and confidentiality were assured.
Measures
Demographic questionnaire
This questionnaire included question information regarding gender, age, education level, marriage, departments. Additionally, considering COVID-19 exposure, we also asked whether they contacted the confirmed patients.
Nurses' risk perceptions questionnaire
The questionnaire for risk perceptions was referred to the questionnaire revised by the Chinese researchers (Zhang et al., Reference Zhang, Cao, Xu, Chen, Zhang and Cao2016), including 26 questions pertaining to six domains of risk: personal safety risk (R1–R5; e.g. worries about fights, unsafe night commute, disgruntle or manic patients); physical function risk (R6–R9; for instance, occupational diseases, gastritis, or varicose veins), occupational exposure risk (R10–R13; e.g. infection or work environment), psychosocial evaluation risk (R14–R18; patients' complains, colleagues' judgment or superiority of doctors), organizational risk (R19–R22; e.g. security hole, shortage of staff or facilities), and time pressure risk (R23–R26; e.g. less time for family union or less leisure time). The frequency of the worries, equal to the potentiality of perceived risk, is divided into five grades from ‘never’ to ‘almost always’ and then assigned 1–5 points in turn. The higher the score for each item indicated the higher awareness of the risk. The α coefficients for the subscales ranged from 0.908 to 0.970.
Questionnaires for psychological outcomes
Psychiatric questionnaires were conducted to measure the psychological outcomes. The impact of Event Scale-Revised (IES-R) was adopted as it is not diagnostic for PTSD but an appropriate instrument to measure the subjective response to a specific traumatic event in the senior population, as well as a total subjective stress IES-R score recognized as the proper self-report tools to assess post-traumatic stress after COVID-19 (Christianson and Marren, Reference Christianson and Marren2012; Chew et al., Reference Chew, Lee, Tan, Jing, Goh, Ngiam, Yeo, Ahmad, Khan and Shanmugam2020). IES-R has three subscales (Intrusion, Avoidance, and Hyperarousal), which are closely affiliated with PTSD symptoms. Items have all turned the focus on the event of the COVID-19 pandemic outbreak. Participants were required to rate their distress brought by COVID-19. Simultaneously, their current sleep quality, anxiety, and depression were also measured respectively by Insomnia Severity Index (ISI) (Bastien et al., Reference Bastien, Vallières and Morin2001), The Generalized Anxiety Disorder Scale (GAD-7) (He et al., Reference He, Li, Qian, Cui and Wu2010), and Patient Health Questionnaire (PHQ-9) (Kroenke et al., Reference Kroenke, Spitzer and Williams2001). Likewise, for our purpose of evaluating the psychological fallout of the COVID-19 pandemic, we added the sentence – ‘Comparing to before, this pandemic year makes you feel…’ – to the original symptom items. The total score of each questionnaire evaluated the psychological state during the recent year.
Statistical analysis
Latent profile analysis (LPA) was conducted in Mplus version 8.3 (Muthén and Muthén, 1998–2017) to identify and describe unobserved classes of risk perceptions among HCWs (Hagenaars and Mccutcheon, Reference Hagenaars and Mccutcheon2002). LPA is a person-centered methodological approach that helps to elucidate population heterogeneity within observed data through the identification of underlying subgroups of individuals, thus allowing the empirical examination of a distinct complex construct. The modified approach to modeling was applied as ratings of HCW's risk perceptions were scored as continuous variables, which could be appropriately tested by the method (Vermunt, Reference Vermunt2010). Since the exact number of latent classes representing risk perceptions was unknown, an exploratory approach was used firstly, which started with the most one-class model and fitted successive models with increasing numbers of classes. Each latent class solution was replicated 20 times beginning at random starting values. This method included a close examination of item loadings and model fit indices for estimated latent classes (Vermunt, Reference Vermunt2010; Asparouhov and Muthén, Reference Asparouhov and Muthén2014). The final number of classes was determined based on the conceptual meaning, smallest estimated class proportions, entropy, and statistical model fit indices such as the Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), and adjusted BIC (Nylund et al., Reference Nylund, Asparouhov and Muthén2007; Asparouhov and Muthén, Reference Asparouhov and Muthén2014). Latent classes with <5% of the total sample were not considered due to the possibility of class over-extraction in the presence of non-normal data and poor generalizability (Bauer and Curran, Reference Bauer and Curran2003; Grimm, Reference Grimm2017). Maximum likelihood estimation with robust standard errors incorporating all available data was used to deal with missing data and to estimate parameters. Mplus accounted for the complex survey design by correcting the standard errors and χ 2 tests of model fit (Hagenaars and Mccutcheon, Reference Hagenaars and Mccutcheon2002).
Descriptive statistics for the demographic characteristics and psychological reactions to COVID-19 of the study sample and comparisons across groups were analyzed using SPSS version 26.0. Meanwhile, the distribution of identified classes and their associations with psychological reaction and demographic characteristics were examined by the one-way analysis of variance (ANOVA) and χ 2 analysis. Further, the Multinomial Logit Model was built with the Wald tests for the effects of covariates on class membership. Regression was performed using the psychological reactions to predict the contingent probability of the identified classes of HCW's risk perceptions. Statistical significance was taken as a two-sided p < 0.05.
Results
LPA for risk perceptions
Table 1 presents the fit indices for the LPA. Based on fit indices and interpretability of class solutions, a four-class solution was the optimal solution. The five-class solution yielded a slightly lower adjusted BIC and AIC with the bigger value of entropy than the three-class model; however, the value of entropy was not improved and the non-significant Lo–Mendell–Rubin (LMR) test indicated that this model failed to fit the data significantly better than a four-class model. Therefore, a four-class solution was judged as the optimal solution. This solution comprised four classes of nurses with different levels of risk perceptions which could be classified as high (class 4), moderate (class 3), mild (class 2), and low (class 1). Conditional means of each risk for the four-class solution are displayed in Fig. 1. Values >3.5 were considered to represent a high level of perceived risk in the class (i.e. the weighted average rating of this group was estimated to be 3.5 points on the item), values between 3.5 and 2.5 presented a moderate level, values between 2.5 and 1.5 a mild level, and below 1.5 were low-risk level. As can be seen in Fig. 1, all classes presented the same patent for risk perceptions. Class 4 evidenced a high probability of rating high scores for physical function, organizational risks, and time pressure risks, only slightly low in threats from patients to their safety; class 3 and class 2 also showed similar sensitivity to the different risk domains; however, class 1 tended to be insensitive to all risks.
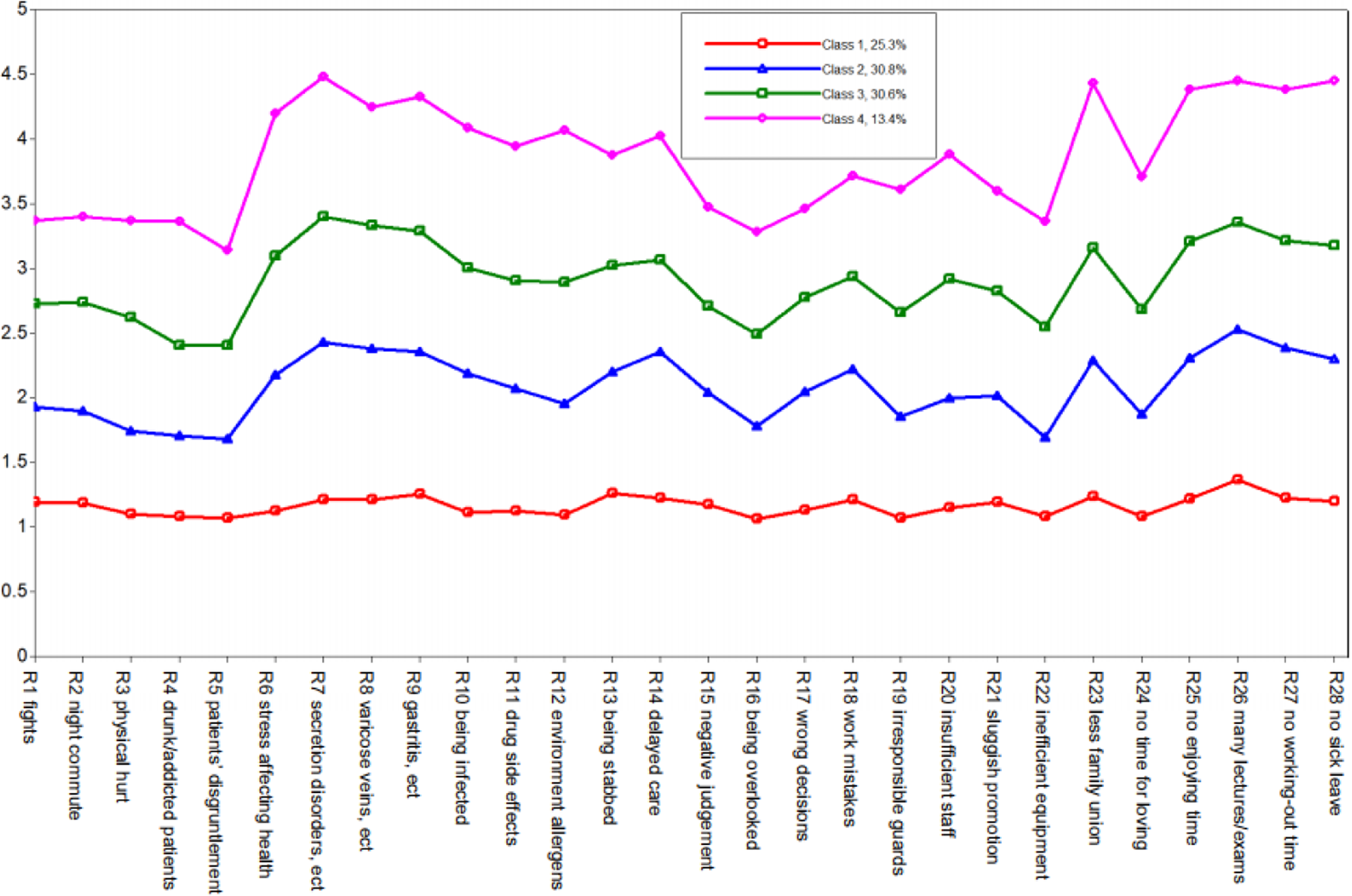
Fig. 1. Estimated means of risk perceptions and percentiles for the four-class solution.
Table 1. Goodness-of-fit statistics for 1–6 class solutions
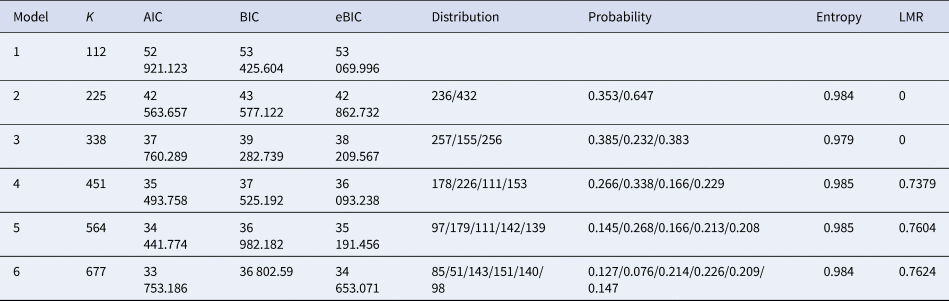
K, free parameter; AIC, Akaike information criterion; BIC, Bayesian information criterion; e-BIC, sample size-adjusted Bayesian information criterion; LMR, Lo–Mendell–Rubin.
Differences between LPA classes
Participant characteristics, COVID-19 related experiences, and mean psychological outcome scores for each of the LPA classes were also presented in Table 2. The χ 2 analysis demonstrated no significant differences between classes in terms of marriages, department, positions, contact history, age, years of being working. However, gender was significantly disparate between classes as women tended to be more worried than men. Notably, a series of one-way ANOVAs indicated that the psychological outcomes were related to the risk perceptions. Post hoc tests showed between-class differences were all significant (p < 0.001). In class 4, the average score of IES, ISI, PHQ, and GAD were the highest, while in class 1, they were the lowest, thus indicating the high class scored significantly higher than the lower on each sub-scale.
Table 2. Participants characteristics and psychological outcomes one year after COVID-19
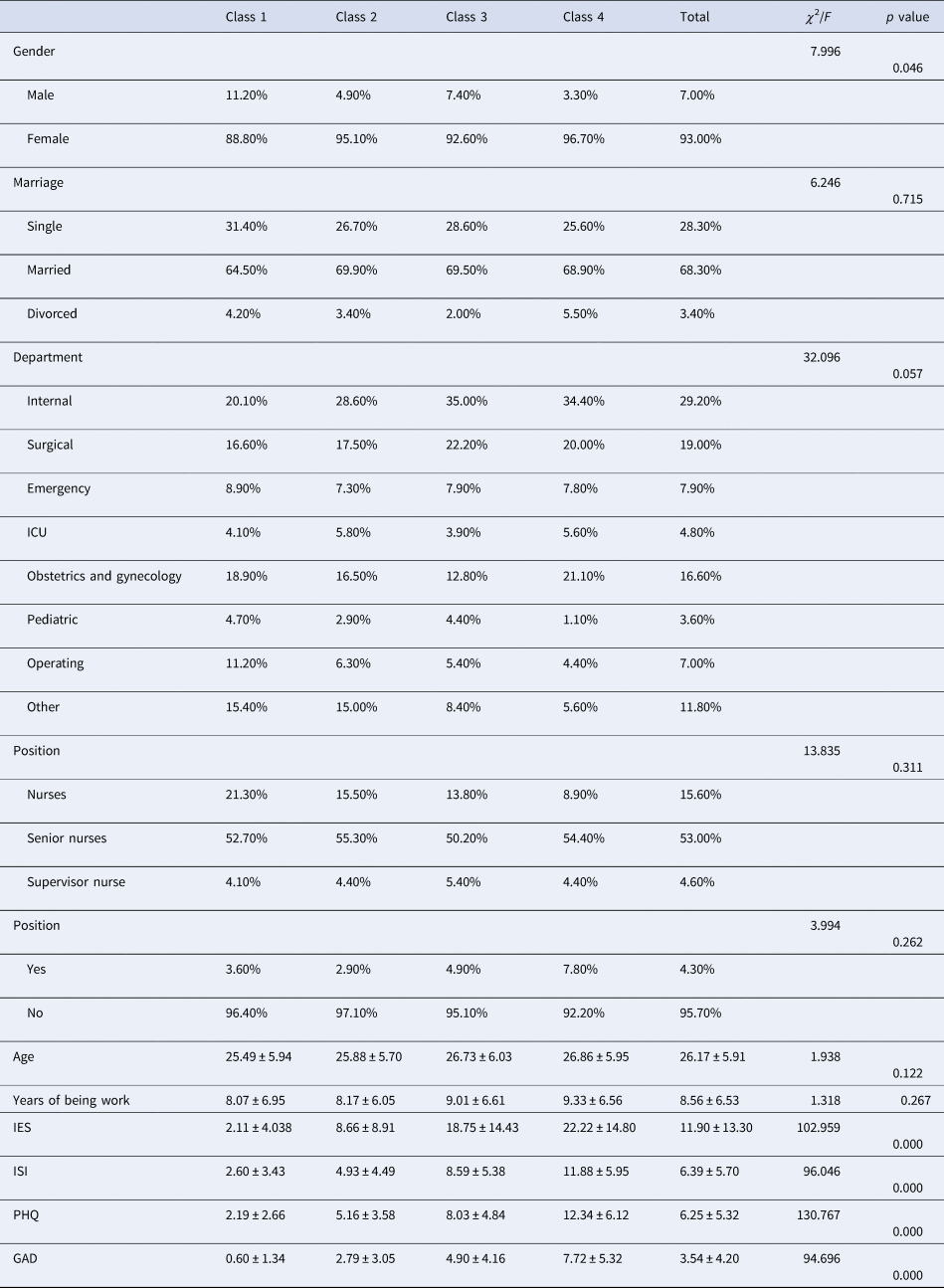
IES, The impact of Event Scale-revised; ISI, Insomnia Severity Index; PHQ, Patient Health Questionnaire items; GAD, The Generalized Anxiety Disorder Questionnaire.
The predictive effects of psychological variables
To examine the long-term effect of COVID-19 on nurses' risk perceptions, a multinominal logistic regression and a probability regression were respectively conducted by using the total score of IES, ISI, GAD, or PHQ as predictors. Due to the near-significant result for gender between classes, we also included this variable as a co-variable in the multinominal logistic regression model with class 1 as the reference class. As Table 3 showed, gender differences were only slightly significant in the comparison between class 4 and class 1; however, psychological outcomes strongly predicted the class of risk perceptions with between-level disparities.
Table 3. Multinomial logistic regression predicting class membership using class 1 as reference
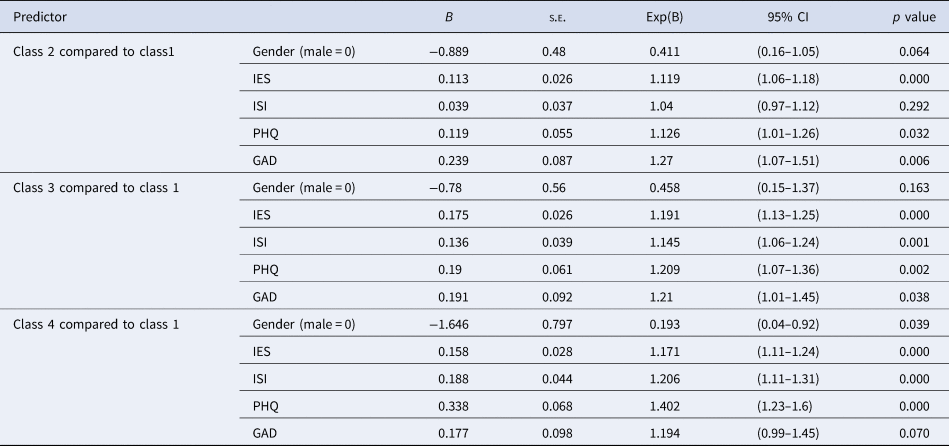
IES, The impact of Event Scale-revised; ISI, Insomnia Severity Index; PHQ, Patient Health Questionnaire items; GAD, The Generalized Anxiety Disorder Questionnaire; s.e., standard error; CI, confidence interval.
For further analysis of the predicted value, a regression on the post probability of categorized risk perceptions with psychological outcomes was conducted, results from which were presented in Table 4. This prediction analysis revealed that the score of IES-R significantly increased the possibility of being classified from class 1 to class 2 by 12.3%, from class 1 to class 3 by 19.8%, and from class 1 to class 4 by 6.6%. Similarly, increased scores in ISI and depression significantly elevated the possibility of being classified into the higher risk perceptions. Especially, in comparison, GAD scaling for anxiety only significantly accounted for the increase from low-risk perception to mild (p = 0.012), but no significance for further elevation. Referred to class 3, increases in PHQ scaling for depression added the possibility of being classified to class 4 by 16.5%. Anxiety existed in all classes and significantly augmented nurses' risk perception into a mild class instead of a moderate one; however, the PTSD after COVID-19, insomnia, and depression would render moderate and high-risk perception in nurses. As a whole, in our samples, we attained that psychological status affected risk perceptions.
Table 4. Alternative parameterizations for the categorical latent regression using class 1 as reference
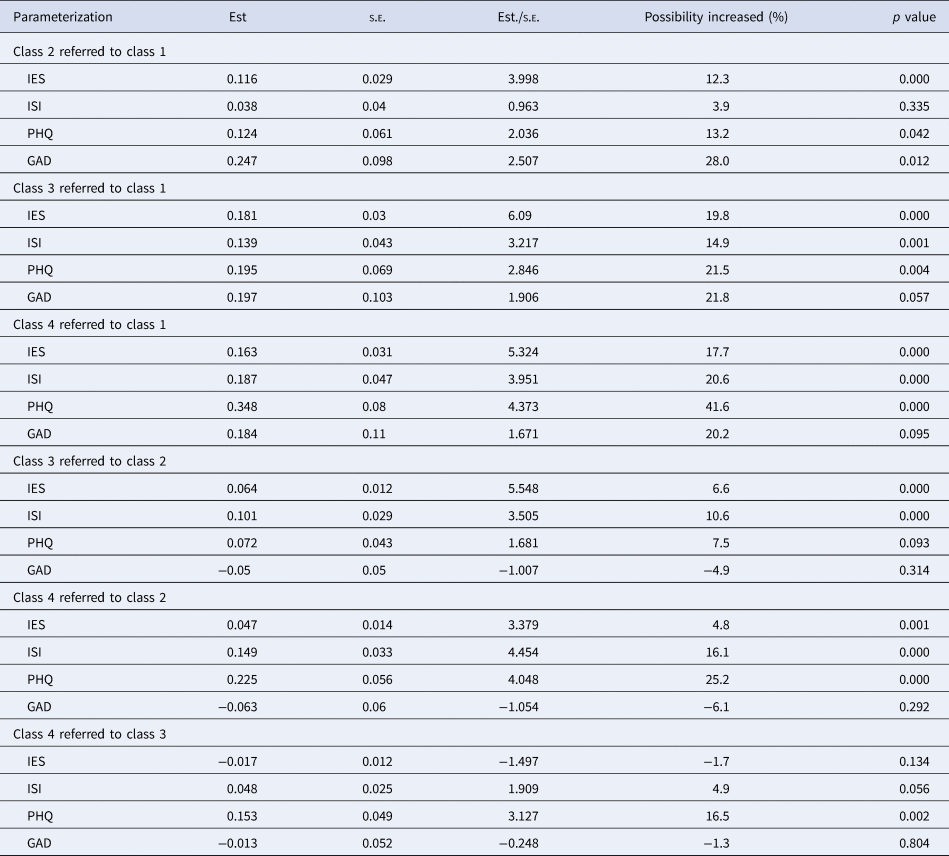
IES, The impact of Event Scale-revised; ISI, Insomnia Severity Index; PHQ, Patient Health Questionnaire items; GAD, The Generalized Anxiety Disorder Questionnaire; Est, estimation; s.e., standard error.
Discussion
This study examined the extent to which psychological outcomes of a pandemic were associated with risk perceptions in a sample of nurses working against COVID-19 using an LPA approach. We identified four subgroups of nurses: a low-level class, a mild-level class, a moderate-level class, and a high-level class for all risk perceptions. Anxiety elevated nurses' risk perception to a mild level, while the PTSD after COVID-19, insomnia, and depression would accelerate the process, reaching a moderate and high level of risk perceptions. Overall, a poor psychological status confirmed by the clinic questionnaires could predict a high level of risk perceptions to nursing works.
These findings are consistent with previous studies that found a link between negative emotions, sleep problems, PTSD, and risk perceptions (Frings, Reference Frings2012; Spada and Reisse, Reference Spada and Reisse2012; Palgi et al., Reference Palgi, Avidor, Shrira, Bodner, Ben-Ezra, Zaslavsky and Hoffman2018; Chew et al., Reference Chew, Lee, Tan, Jing, Goh, Ngiam, Yeo, Ahmad, Khan and Shanmugam2020). As a consensus, a high level of perceived risk could have a side-effect on the mental health of people during public health crises (Ding et al., Reference Ding, Xu, Huang, Li, Lu and Xie2020). However, these studies did not report recurrences of mental problems caused by the crisis without a follow-up study in the back-to-normal process. In particular, our study was the first to explore the post-acute sequelae of COVID-19 in the mental health of nurses and the risk perception for their work. Although without a clinical diagnosis and based on the participants' self-reported possibilities and severities of mental problems, our results still proved that psychological outcomes of COVID-19 elevated the level of nurses' risk perceptions, supported by the fact that the members in class 4 (showing a high level of risk perceptions) have a high prevalence of PTSD, sleep, and emotional disorders.
Additionally, in our cohort, PTSD, insomnia, depression, and anxiety were not as severe as previous studies reported immediately after the outbreak of COVID-19 given their total scores on the subscales (Magnavita et al., Reference Magnavita, Tripepi and Prinzio2020; Tan et al., Reference Tan, Chew, Lee, Jing and Sharma2020; Yin et al., Reference Yin, Sun, Liu, Ni, Deng, Jia, Shang, Zhou and Liu2020), while a series of studies conducted at different stages of COVID-19 in Central Italy showed that the psychological problems of health care workers were not significantly improved and that various problems and worries were perceived in their work and life (Magnavita et al., Reference Magnavita, Soave and Antonelli2021a, Reference Magnavita, Soave and Antonelli2021b). Moreover, a recent review also reported that mental health issues, such as anxiety, depression, PTSD, and sleep disorders, had great impacts on health care workers, especially on their contacts with the public (Giorgi et al., Reference Giorgi, Lecca, Alessio, Finstad, Bondanini, Lulli, Arcangeli and Mucci2020). Therefore, we cautiously interpreted our findings with studies after COVID-19. Most nurses stimulated their worries about their physical health risk and time pressures from their works signaled by anxiety, which could be an adaptive self-protective reaction to the crisis. However, depression, insomnia, and PTSD, as worse by-products of COVID-19, could continue to deteriorate and elevate nurses' risk perceptions of fears, avoidance, and discouragement. The persistent debate over COVID-19 would discombobulate nurses when they encounter risk. Worse, these nurses would not seek the help of a mental health professional as they lack the energy and inclination to do so. Therefore, there could be no positive changes in the prevalence of depression, insomnia, and PTSD. Miserably, suicide and substance use disorders could be further problems (Valente, Reference Valente2011).
To prevent tragedies, we must acknowledge that this pandemic has created enormous stress and heartache in our health care professionals, especially nurse clinicians, despite their attempts to mask it. Without the lessons taught by the COVID-19 pandemic, few could have imagined or anticipated a situation such as this. Hence, special attention should be given to nurses, especially those who avoid clinical practices. Psychological programs to relieve anxiety and fear such as mental exercises and gradual desensitization should be designed to intervene in psychological reactions and risk perceptions. Furthermore, although nurses are praised for their heroic actions during the COVID-19 pandemic to shoulder their responsibilities and spare no efforts to guard public health, which are undoubtedly appreciated, we must be cautious that heroic actions – voluntary prosocial actions – associated with an acknowledged degree of personal risk, transcend the duty of nurses, and aggregate their psychosocial risks (MacDonald et al., Reference MacDonald, De Zylva, McAllister and Brien2018). After the outbreak of COVID-19, more discussions centered around the risk and obligation of ‘duty of care’, or ‘duty to treat’, weighing the risks against their duties (WHO, 2020b). Consequently, the prevalence of psychosis has been emphasized by many studies. However, fragments of psychological help are not timely and lack follow-up; therefore, at the latter stage of the pandemic, the psychological outcomes were predominantly reflected in risk perceptions for work and life (Kontoangelos et al., Reference Kontoangelos, Economou and Papageorgiou2020; Saladino et al., Reference Saladino, Algeri and Auriemma2020). Nurses’ feelings of devoting less time to physical activity or meditation and intellectual activities reduce resilience and hinder the application of individual psychological support treatments. Perceived heavy workload could be alleviated by increasing staff, but adequately trained clinic personnel are not available given that fewer nurses are willing to practice in the clinics. Therefore, interventions on nurses' risk perceptions through ameliorating the psychological impact of the COVID-19 pandemic are imperative. It should be a network to ease all factors for overly elevated risk perceptions to motivate nurses. Clinicians who provide care for moral injury and associated mental illness should also be aware of opportunities to speak about the worries of their jobs and focus on their psychological status during therapy. Supervisors should ensure that time is allotted to reflect on and learn from extraordinarily difficult experiences and encourage therapeutic intervention. Additionally, nurses themselves should increase their knowledge about their work and not be shameful about their worries and fears; instead, nurses should discuss their concerns with peers who are experiencing similar concerns.
Limitations
There are limitations to the conclusions that can be drawn from this study. As mentioned, LPA is a data-determined statistical approach. The analysis described in this paper was undertaken using a sample of five hospital nurses, in Jiangsu, China. A strength of our sample is that it was collected from a place where there were no other emergencies except COVID-19. However, there was no significant disparity of exposures in our cohort; therefore, findings generalized to other samples await further investigation. Additionally, the analysis was cross-sectional, and it was not possible to determine a cause-effect relationship. Finally, a limitation inherent in LPA is that it classifies individuals into distinct subclasses based on the dichotomization of constructs. However, an advantage of the approach is that it enables researchers to sort individuals into relatively homogeneous subgroups that are more similar to each other than other subgroups within a sample (Borsboom et al., Reference Borsboom, Rhemtulla, Cramer, Van der Maas, Scheffer and Dolan2016). A similar application was also seen in the study of public people with various levels of risk perceptions (Wang et al., Reference Wang, Chen, Chang, Wu, Lu and Yen2021). In our study, the technique helps evaluate the characteristics of nurses' risk perceptions through the application of varied statistical approaches.
Certainly, further insights can be gained from the ongoing analysis of the factors that promote nurses' willingness to work. For example, risk communication, referring to exchanging information, advice, and opinions, enables at-risk people to make judgements of uncertainty and to protect themselves. The frequency of risk communications between nurses and patients, doctors, and supervisors creates the foundation for social support systems, which directly affects the individual psychological state and perceptions (Ell, Reference Ell1984). Another study of our cohort also found a buffer effect of perceived social support on anxiety 1 year after the COVID-19 (Hou et al., Reference Hou, Yin, Xu, Gao, Bin, Li, Cai, Liu, Dong, Deng and Ni2021). However, it is unknown about how nurses' risk perceptions coevolve with social connections. The role of risk communication in various classes of risk perceptions and psychological outcomes after the COVID-19 pandemic warrants further study. Hence, it is necessary to examine the roles of the individual, psychosocial, and other structural variables in various classes of risk perceptions and psychological outcomes. Notably, longitudinal studies with proper intervention may contribute to confirming previous findings and inspiring future research.
Conclusion
There are extraordinary times during the COVID-19 pandemic. Now, there is an urgent need to ensure that the tasks ahead do not cause long-lasting damage to health care staff. The results of this study, consistent with theoretical conceptions, highlight the important impacts of psychological outcomes after the outbreak of COVID-19 on risk perceptions among nurses. As an appropriate job-related risk perception is closely related to nurses working motivation, it is imperative to intervene in nurses' psychological outcomes, such as PTSD, insomnia, depression, and other server outcomes, while simultaneously focusing on work-related worries.
Data
The data that support the findings of this study are available upon reasonable request.
Acknowledgements
We thank all the participated nurses and the dedicated leaders for their assistance in implementing this study.
Author contributions
YQ, HT, and LW participated in manuscript writing and literature review; GJ performed the literature review and participated in data analysis; NC performed the literature review, data collection; ZW collected the data and reviewed the manuscript; LB and LH contributed to data analysis, interpretation of the results, and critically revised the manuscript; DW, DG, and JY led the whole study.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.








