Introduction
Granular myringitis is characterised by de-epithelialisation of the tympanic membrane. It can be missed when clinicians use only a general otoscopic examination, and general practitioners frequently misdiagnose the condition as otitis externa or suppurative otitis media.Reference Khalifa MC, Bassiouny and Kamel1 The most common presentation of granular myringitis is intermittent otorrhoea.Reference Makino, Amatsu, Kinishi and Mohri2 Tympanic membrane perforation can also be found concurrently in granular myringitis.Reference Wolf, Primov-Fever, Barshack, Polack-Charcon and Kronenberg3
Granular myringitis can be classified into two forms: primary, which is idiopathic, and secondary, which results from trauma or infection.Reference Bansal4 Previous studies have shown positive bacterial cultures from aural discharge, such as staphylococcus, corynebacterium and Pseudomonas aeruginosa. Granular myringitis could result in ear canal stenosis from fibrotic formation because of improper or inadequate treatment.
Currently, there are no standardised, specific treatments for granular myringitis.Reference Suvarnsit, Prakairungthong, Limviriyakul, Atipas and Pitathawatchai5,Reference Devaraja6 A variety of treatment choices are available, such as antibiotic ear drops, diluted vinegar solution, diluted hydrogen peroxide, Castellani solution and carbon dioxide laser. These treatments have demonstrated inconsistent success rates. Moreover, the timelines used by studies to evaluate their success have also been variable,Reference Atef, Hamouda, Mohamed and Fattah7–Reference Jung, Cho, Yoo, Lim and Chae10 ranging from several weeks to months.
Prolonged granular myringitis treatment may cause collateral effects, such as high treatment costs or reduced compliance with drug therapy. Furthermore, an extended period of using an antibiotic or an antibiotic in conjunction with steroid ear drops may induce adverse effects, drug resistance or an opportunistic fungal infection.
Diluted vinegar (an antiseptic solution) is an interesting option for treating granular myringitis. Topical acetic acid has been employed as an acidic astringent for a century.Reference Dohar11 It was frequently used to treat mild to moderate otitis externa until the antibiotic era. There is in vitro and in vivo evidence of the antimicrobial effects of acetic acid.Reference Agrawal, Sarda, Shrotriya, Bachhav, Puri and Nataraj12–Reference Thorp, Kruger, Oliver, Nilssen and Prescott14 Nevertheless, the proper concentration of diluted vinegar for granular myringitis treatment is still in question. At a higher concentration with a lower pH, the antimicrobial effect of the solution might be increased, but local irritation might also be worse.
TanejaReference Taneja15 carried out a prospective study on treating patients with ear discharge, ear pain or ear itching with various formulas of otic drops. One of those otic drops was 2 per cent acetic acid in saline solution. Taneja reported that this formula had a success rate of 81 per cent at 2 weeks.
A randomised, controlled trialReference Prakairungthong, Ungchoomchoke, Limviriyakul, Suvarnsit, Atipas and Thongyai16 on granular myringitis treatment was conducted in 2020. The researchers compared a 1 per cent acetic acid solution and chloramphenicol eardrops, measuring their outcomes at 8 weeks. The success rates of the diluted vinegar and chloramphenicol groups were 91.7 per cent and 66.7 per cent, respectively, with no statistically significant difference. However, the diluted vinegar group participants tended to completely heal earlier. When looking at the success rate at 2 weeks, the diluted vinegar group had a recovery rate of approximately 40 per cent.
The present work aimed to assess the effectiveness of a high concentration of an acetic acid solution while monitoring the local irritative effects on patients. The effectiveness of treating granular myringitis with 1 and 2 per cent acetic acid solutions for 2 weeks was compared, and the respective recurrence rates of the condition was determined.
Materials and methods
Study design
Before this research began, its protocol was approved by the institutional review boards of Siriraj Hospital (Si208/2021), Chulalongkorn Memorial Hospital (449/2021), Lerdsin Hospital (LH641019) and Somdejprapinklao Hospital (NMD-REC 020/64). This double-blind, randomised, controlled trial was conducted from October 2021 to June 2022 and included patients with granular myringitis grades I and II (Fig. 1), as per the study by Wolf et al.Reference Wolf, Primov-Fever, Barshack, Polack-Charcon and Kronenberg3
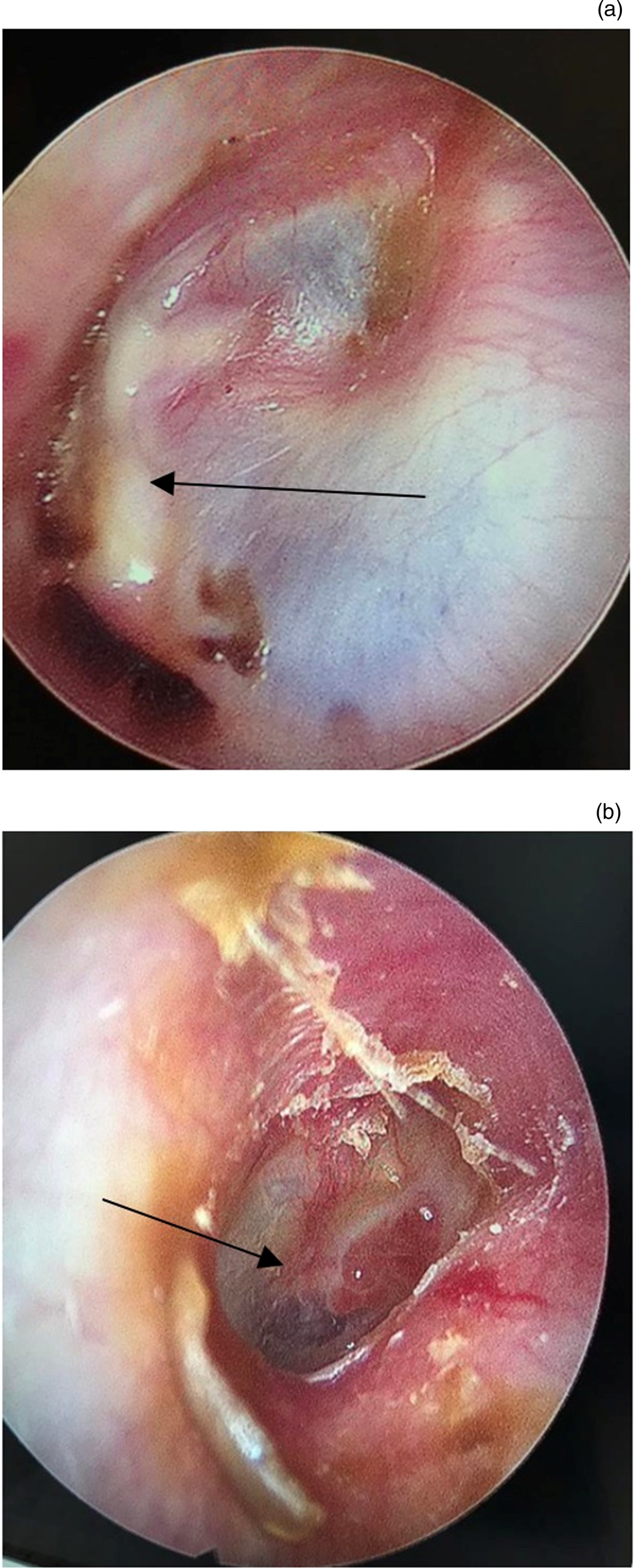
Figure 1. (a) Grade I myringitis shows non-epithelial surface with crusting on tympanic membrane surface (arrow). (b) Grade II myringitis shows focal raised polypoid formations or granulation tissue develop on tympanic membrane surface (arrow).
Study population
This study enrolled patients visiting Lerdsin Hospital, Somdejprapinklao Hospital and Siriraj Hospital. The inclusion criteria were granular myringitis (grades I and II) and adult patients (18 years and over). The exclusion criteria were: (1) a tympanic membrane perforation of more than 3 mm, (2) a history of intolerance to acetic acid, (3) a prior ear operation on the lesion side within the preceding 3 months, and (4) concomitant middle-ear disease.
Study protocol
Diagnoses of granular myringitis were confirmed by either microscopic or endoscopic examination. Clinicians then cleaned the ear canals meticulously with proper instruments and suctioning. Chemical cauterisation with 85 per cent trichloroacetic acid and astringent products (such as 2 per cent merbromin solution) were applied if needed at each patient visit.
Forty-eight bottles of the study's otic drops were prepared. Twenty-four bottles contained 1 per cent diluted vinegar (1 cc of acetic acid combined with 99 cc of sterile water), and the other 24 bottles had 2 per cent diluted vinegar (2 cc of acetic acid combined with 98 cc of sterile water). The bottles were randomly numbered from 1 to 48 and randomly allocated to patients. The pharmacists who prepared the medications managed this process, drawing upon the website www.randomization.com. Except for the individually assigned numbers, all characteristics of the 48 bottles were identical (Fig. 2). Only the pharmacists knew which study drug had been given to each patient; the authors were blinded to this information.

Figure 2. Medication bottle with assigned number.
Patients numbered 1 to 8 were enrolled at Lerdsin Hospital, those numbered 9 to 32 were enrolled at Siriraj Hospital, and patients 33 to 48 were enrolled at Somdejprapinklao Hospital. All were requested to use their assigned ear drops at a rate of 4 to 6 drops over 5 minutes, 3 times a day. Appointments for 1 to 2 weeks were scheduled. Outcomes were measured between 14 and 20 days from the initial consultation.
After the two-week treatment period, unhealed granular myringitis participants were treated continuously until recovered tympanic membranes were identified. Patients declared to be completely healed of the disease were scheduled for a follow-up visit to check if there was a recurrence.
Data collection process
Patient data were recorded on a case record form, and strict data confidentiality was maintained. The information recorded included: demographic data (age and sex), clinical data at presentation (history of ear surgery, duration of onset, presenting symptoms, perforation size and myringitis grading) and follow-up data (individual treatment and side effects).
Outcome measurement
A ‘recovered’ status was documented when otologists identified complete epithelialisation of the tympanic membrane either with endoscopy or microscopy. All patients were asked to report any side effects of using their assigned study drug.
Sample size calculation
The sample size was calculated using reference proportions from studies by TanejaReference Taneja15 and Prakairungthong et al.Reference Prakairungthong, Ungchoomchoke, Limviriyakul, Suvarnsit, Atipas and Thongyai16 The reference success rates for the 1 and 2 per cent acetic acid solutions at 2 weeks were 40 per cent and 81 per cent, respectively. The significance level was set at 0.05 with a test power of 80 per cent. The study required a sample size of 44 participants with an equal allocation ratio between the 2 groups. An anticipated drop-out rate of 10 per cent was included. Therefore, the study required 48 participants: 24 for the 1 per cent acetic acid solution group and 24 for the 2 per cent acetic acid solution group.
Statistical analysis
The data were analysed with an intention-to-treat protocol. However, the data were analysed in a per protocol fashion concomitantly for the overall aspects. Descriptive analysis of the baseline characteristics was performed, with results presented as a percentage, mean and standard deviation, or median with interquartile range, as appropriate. Comparisons of the 1 and 2 per cent acetic acid solution results at 2 weeks and the categorical data (sex, history of ear surgery, grading and disease size) were conducted with the chi-squared or Mann–Whitney tests. Probability values of less than 0.05 were considered statistically significant. All data were analysed using SPSS® (version 26.0) statistical analysis software.
Results
Fifty-eight patients from 3 hospitals were invited to participate in this study. Two patients were excluded because their age and disease severity did not meet the inclusion criteria. One patient was diagnosed with a co-morbid coronavirus disease 2019 infection, and seven patients declined to participate.
The remaining 48 patients were enrolled in the study. After enrolment, however, one patient had active middle-ear disease confirmed and was excluded; tympanomastoidectomy was later performed on this patient. The 47 remaining participants were randomised into 2 groups. Twenty-four patients were assigned to the 1 per cent acetic acid solution group, and 23 patients were placed in the 2 per cent acetic acid solution group (Fig. 3). In the case of four participants with bilateral myringitis, we chose only one side sequentially from right to left.

Figure 3. Study flow diagram. Covid = coronavirus disease 2019
The demographic data of the two groups are presented in Table 1. There were no significant differences in sex, sides, tympanic membrane perforation, duration and size of myringitis except for a prior history of ear surgery. The common presenting symptoms were otorrhoea (36 out of 47; 76.6 per cent), itching (29 out of 47; 61.7 per cent), aural fullness (13 out of 47; 27.7 per cent) and otalgia (7 out of 47; 14.9 per cent).
Table 1. Demographic and clinical data at presentation

*n = 24; †n = 23; ‡n = 47; **p < 0.05 = statistical significance. TM = tympanic membrane
At the end of the 2-week treatment period, 5 participants were lost to follow up. Three participants (13 per cent) were in the 2 per cent acetic acid group, and the other 2 participants (8 per cent) were in the 1 per cent acetic acid group. During the 2-week treatment period, 125 patient visits were recorded. In 64 of the 125 visits (51.2 per cent), patients received 85 per cent trichloroacetic acid cauterisation. In the other 66 of 125 visits (52.8 per cent), a 2 per cent merbromin solution was administered to patients.
After the 2-week treatment period, the success rates of the 1 and 2 per cent acetic acid solutions were 70.8 per cent and 52.2 per cent, respectively. The difference was not significant (Table 2). The 1 per cent acetic acid protocol subsequently achieved a 79 per cent success rate at 4 weeks and an 83.3 per cent rate at 6 weeks. In comparison, the 2 per cent acetic acid protocol continued to achieve relatively low rates: 56.5 per cent at 4 weeks and 73.9 per cent at 6 weeks.
Table 2. Results of success rate of 1 and 2 per cent acetic acid ear drops at 2 weeks

*n = 18; †n = 29; ‡n = 13; **n = 29
Looking at factors that may affect success rate, there was no statistical significance between cured and not-cured groups in terms of previous history of surgery, grading of myringitis, size of myringitis and tympanic membrane perforation (Table 3).
Table 3. Factors that may affect healing process

* n = 47
Discussion
Prakairungthong et al.Reference Prakairungthong, Ungchoomchoke, Limviriyakul, Suvarnsit, Atipas and Thongyai16 found that a 1 per cent acetic acid solution effectively treated granular myringitis compared with antibiotic eardrops. Nevertheless, we wondered if any regimen could reduce the treatment duration. Because granular myringitis might be affected by infection,Reference Makino, Amatsu, Kinishi and Mohri2 a higher concentration of diluted vinegar, with its more potent antibacterial property,Reference Agrawal, Sarda, Shrotriya, Bachhav, Puri and Nataraj12,Reference Thorp, Kruger, Oliver, Nilssen and Prescott14 may prove clinically more effective.
There were no significant differences between the demographic data of the two groups. Regarding the clinical data at presentation, the groups had a significant difference in their history of prior ear surgery (p = 0.04). The 2 per cent group had a 3-fold higher rate of previous ear surgery than the 1 per cent group (34.8 per cent and 12.5 per cent, respectively; Table 1).
The present investigation found no statistically significant difference between the 1 and 2 per cent acetic acid solution treatments for granular myringitis. Looking at the raw data, the success rate of the 1 per cent acetic acid group was superior to that of the 2 per cent acetic acid group. The participants in both groups reported using the medication as prescribed. We subsequently removed the data relating to the 5 patients lost to follow-up and re-performed our calculations using only the available follow-up data on a per-protocol basis. The success rates of the 1 and 2 per cent acetic acid solution groups changed to 77.3 per cent and 60 per cent, respectively. However, the difference in the two groups’ success rates was non-significant in both the intention-to-treat and the per-protocol calculations. The number of cured patients in the 1 per cent acetic acid solution group was slightly higher than that in the 2 per cent acetic acid solution group (Table 2).
Twenty-nine participants from the 1 and 2 per cent acetic acid groups were cured within the 2-week treatment period. However, 3 of these 29 cured participants (10.3 per cent) later showed evidence of disease recurrence within the 8-week follow up. In contrast, in the per-protocol analysis, 13 patients (5 from the 1 per cent group and 8 from the 2 per cent group) failed the treatment at 2 weeks. These patients were given standard ear care and eardrops for home application. Some were prescribed the remaining medication, and others were prescribed alternative medications (for example, clotrimazole eardrops). Lastly, although patients from the 1 per cent acetic acid group were completely healed of myringitis by the 16th week, patients from the 2 per cent acetic acid group needed more prolonged treatment (Fig. 4).

Figure 4. Graph showing healing time for good epithelialisation between the 1 and 2 per cent acetic acid groups.
In the case of the 2 per cent acetic acid group, the higher acid concentration improved the solution's ability to lower the pH in the ear canal. The participants in that group were therefore expected to have more irritation symptoms. Nevertheless, they still reported good compliance.
The two groups used the same protocol to manage granular myringitis. The first step was aural toileting, which facilitated diagnosis and enhanced disease resolution. The next step was either chemical cauterisation or the application of an astringent product; the choice depended on the characteristics and severity of the granular myringitis. The differences between the two groups were the abilities of their respective medications to affect the pH in an ear canal and to control antimicrobial activity. The comparable results achieved by this study's 1 and 2 per cent acetic acid solutions suggest that eardrops might only be a complementary therapy for granular myringitis treatment.
A factor that may affect the healing rate is the severity of the disease. In this study, we graded our participants per the recommendations of Wolf et al.Reference Wolf, Primov-Fever, Barshack, Polack-Charcon and Kronenberg3 Our patients had been graded into grades I and II at the first diagnosis of myringitis. Grade II is considered more severe because focal raised polypoid formations develop. We found that grade II tended to heal incompletely and needed more prolonged treatment than grade I (Fig. 5). There was no statistical significance of success rate between grade I and grade II groups at two weeks (p = 0.53).

Figure 5. Graph showing healing time for good epithelialisation between the grade 1 and 2 groups.
Although there was a significant difference in previous history of ear surgery (Table 1), the cure rate at two-week follow up between patients with and without prior ear surgery saw no difference in percentage of cure rate (p = 0.49) (Table 3).
We wondered whether tympanic membrane perforation as a presenting finding is a poor prognostic factor. We considered perforation size up to 3 mm as the safety point for eardrops; at this perforation size, eardrops do not get into the middle-ear space. Although acetic acid solution might leak into the middle ear and irritate middle-ear mucosa, it will drain through the Eustachian tube and discharge, or tissue fluid in the middle ear dilutes the acetic acid.Reference Yamano, Higuchi, Nakagawa and Morizono17 There is no issue regarding its ototoxicity at the present time.Reference Thorp, Kruger, Oliver, Nilssen and Prescott14,Reference Yamano, Higuchi, Nakagawa and Morizono17 There was no difference in the success rate at two weeks between patients with and without perforation (p = 1.00) (Table 3). There were more unhealed cases among patients with tympanic membrane perforation in the longer follow-up period (Fig. 6).

Figure 6. Graph showing healing time with and without tympanic membrane perforation.
Another point of concern is the recurrence of the disease. Three out of 29 cases (approximately 10 per cent) from the cured group had recurrence within 8 weeks. The three patients had one common factor: they did not frequently use ear picking to remove wax from their ears. Two of them had never used a cotton bud, and the third patient sometimes used a cotton bud. This common factor implies that the aetiologies of their granular myringitis were unclear and unlikely to result from trauma.
It is generally recognised that there are no effective modalities for treating granular myringitis. Our systematic literature search for treatments showed options such as carbon dioxide lasers, surgery and various otic drops (e.g. antibiotic drops, antibiotic plus steroid drops and diluted vinegar). The purpose of the prescribed eardrops depends on the physician's judgment of the cause of granular myringitis. Physicians who suspect an underlying infection may prescribe drops designed to counter antimicrobial activity. On the other hand, physicians who suspect an inflammatory process may prescribe steroid drops because of their anti-inflammatory properties.
• The success rate of 1 per cent diluted vinegar shows no statistically significant difference from 2 per cent diluted vinegar at 2-week treatment period
• The number of cured patients in the 1 per cent acetic acid solution group was slightly higher than that in the 2 per cent acetic acid solution group
• There were no side effects from either 1 per cent or 2 per cent acetic acid solution groups
• Wound care is necessary, including aural toileting to clean the ear canal
The primary treatment procedure for granular myringitis should be local wound care. Affected ears must be meticulously cleaned of discharge and debris because any remaining debris or sticky discharge can cause further epithelial maceration. In addition, chemical cauterisation and astringent products enhance the period of dryness and stimulate the epithelial migration needed to heal myringitis. Attending physicians can also prescribe eardrops for ear care during the follow-up period, which should not exceed one week. Patients who fail non-invasive management should be switched to surgical management.
Conclusion
There are no differences in the effectiveness of 1 and 2 per cent acetic acid solutions in treating granular myringitis over two weeks. Both concentrations satisfactorily promote the healing of granular myringitis. Wound care is necessary and comprises aural toileting to clean the ear canal and chemical cauterisation or the application of an astringent product to dry the canal. All patients should be followed up within a period not exceeding one week. They should also be informed about the possibility of disease recurrence.
Acknowledgements
The authors acknowledge Ms Pataravadee Chukaewrungroj, a pharmacist at Siriraj Hospital, for preparation of the acetic acid solutions used in this study, and Ms Jeerapa Kerdnoppakhun (a research assistant) for her help managing documents. The authors are also indebted to Mr David Park for the English-language editing of this paper. This study was funded by a grant from the Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, Thailand (R016431067).
Competing interests
None declared.











