In general, monochorionic twins are monozygotic, meaning that their gene characteristics, such as karyotype, gender and blood group type, are the same. However, several reports have revealed that monochorionic dizygotic twins exist, and genetic information different from their own was detected in them (Peters et al., Reference Peters, Koning, Verhoeven, Schats, Mijatovic, Ket and Lambalk2017; Souter et al. Reference Souter, Kapur, Nyholt, Skogerboe, Myerson, Ton, Opheim, Easterling, Shields, Montgomery and Glass2003). In other words, the paired twins were a chimera. A chimera is defined as an organism that contains different cells derived from two or more distinct zygotes; the chimerism of monochorionic dizygotic twins was shown only through blood. Most of these twins were conceived through fertilization mediated by treatment, particularly artificial reproductive techniques; it is possible that infertility treatment affects the development of monochorionic dizygotic twins (Aoki et al., Reference Aoki, Honma, Yada, Momoi and Iwamoto2006; Miura & Niikawa, Reference Miura and Niikawa2005). Here, we report a rare case of monochorionic dizygotic twins from a spontaneous pregnancy with chimerism of blood identified through karyotyping and ABO blood grouping.
Case
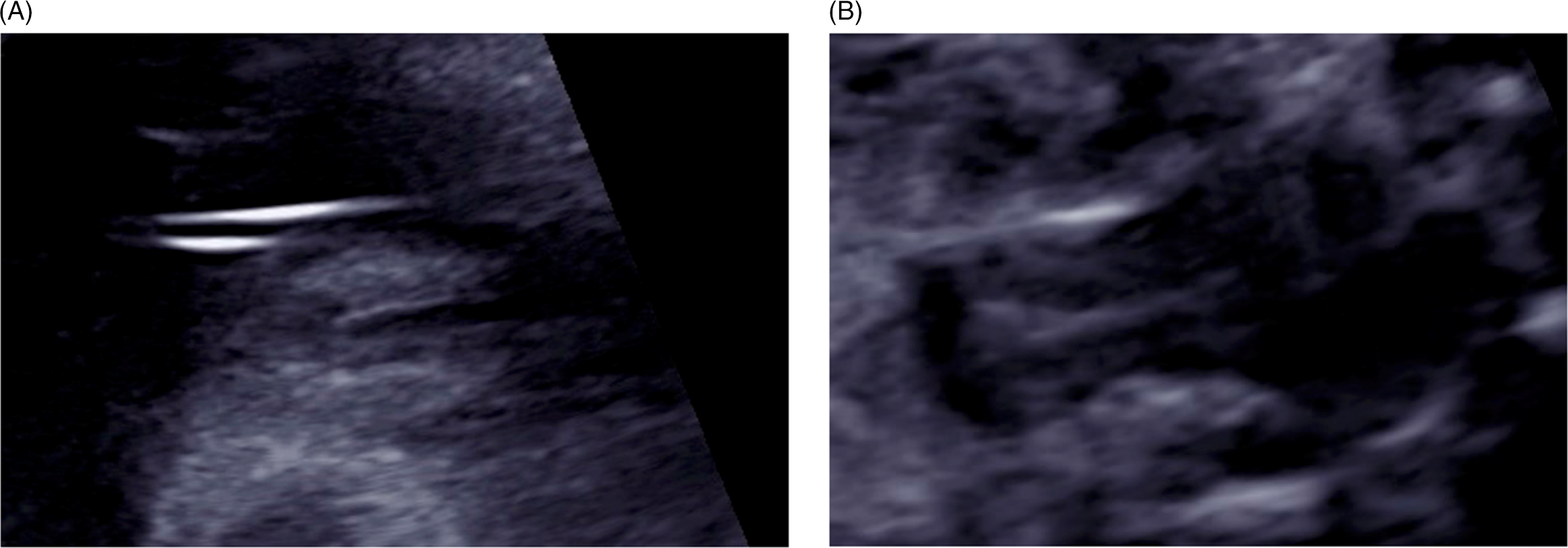
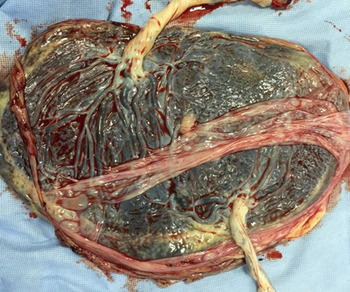
A 30-year-old primipara who conceived spontaneously was diagnosed with a monochorionic (MC) diamniotic twin pregnancy through ultrasonographic findings at 9 weeks’ gestation because there were two fetuses. They were in a common gestational sac, and each had its own amniotic cavity. The primipara was referred to us at 12 weeks’ gestation for the management of her twin pregnancy. At 26 weeks, serial scans showed that the fetuses had a different sex. No abnormalities were found in their anatomy, including the genital organs. The twins were delivered via cesarean section at 38 weeks’ gestation. Apgar scores and pH values were normal. Twin A was a phenotypically normal female, with a birth weight of 2612 g, and Twin B was a phenotypically normal male, weighing 2458 g. Histological examination of the placenta confirmed MC diamniotic twinning (see Figures 1 and 2). Karyotyping was performed on each umbilical cord blood and revealed the chimeric karyotypes 46,XX[15]/46,XY[15] and 46,XY[21]/46,XX[9] for Twin A and Twin B, respectively. Ultrasonography determined normal female and male internal genitalia concordant with their phenotypes (see Figures 3 and 4). Karyotyping was performed again from blood samples at 7 months of age. The results confirmed that the twins had similar chimericg karyotypes: 46,XY[7]/46,XX[13] in Twin A and 46,XX[9]/46,XY[11] in Twin B.

Fig. 1. Macroscopic imaging of the placenta revealed that the twins were monochorionic–diamniotic.
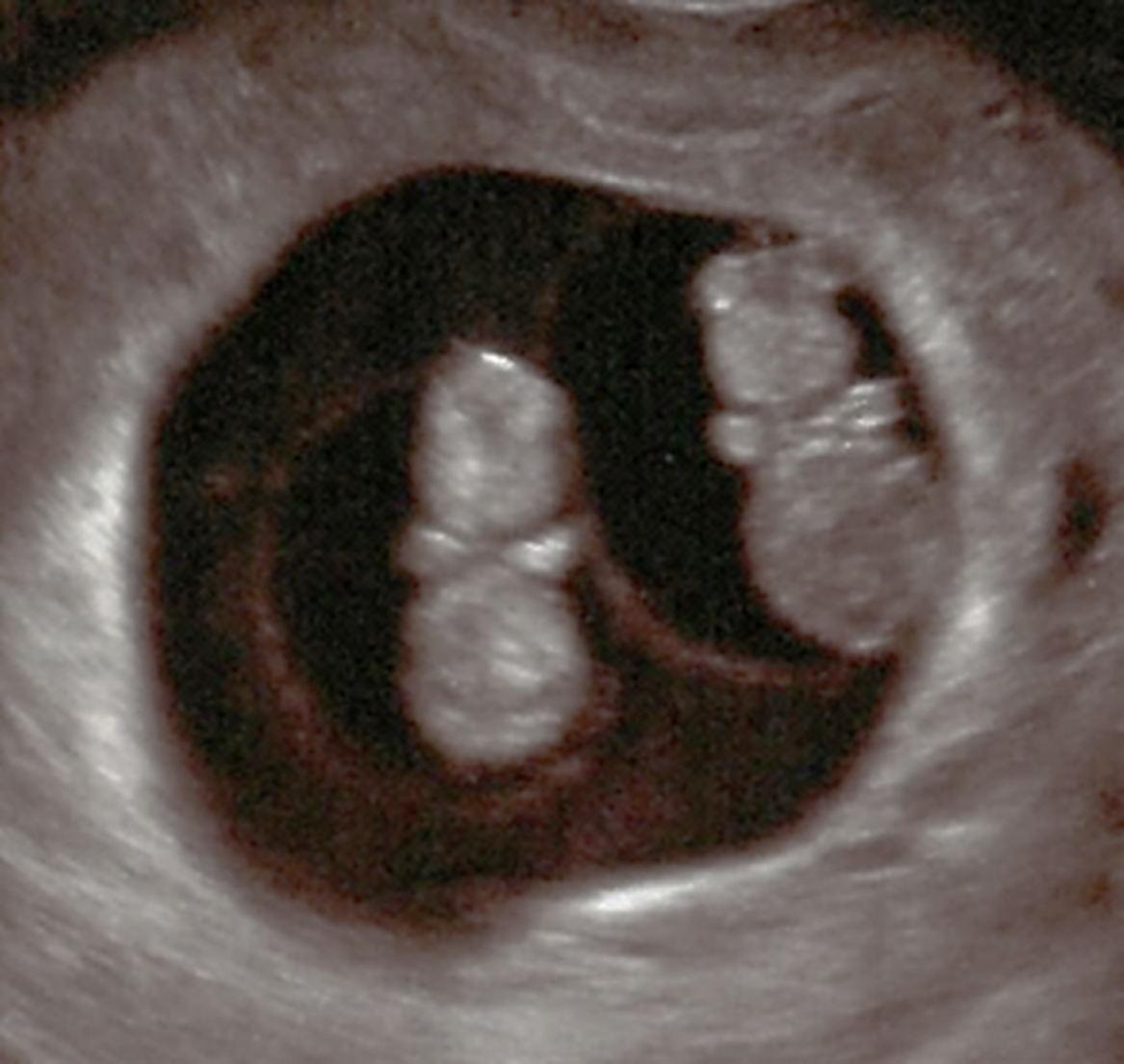
Fig. 2. Monochorionic–diamniotic twin pregnancy in the ninth gestational week.

Fig. 4. Ultrasound findings for Twin B. A normal penis (male reproductive organ) could be seen indicating that Twin B is a boy.
To determine whether this chimerism was temporarily due to vascular communication via placenta between twins or permanently due to the chimera of hematopoietic stem cells, karyotype analysis was repeated. At 1-year-old, we evaluated their buccal swab cells. The results were normal female and normal male karyotypes, respectively — 46,XX[98]/46,XY[2] in Twin A and 46,XY[98]/46,XX[2] in Twin B. Furthermore, ultrasonography revealed normal female and male internal genitalia. These results showed that they were MC dizygotic (DZ) twins (MC-DZ twins). Two years later, the twins underwent blood typing tests. ABO blood grouping was carried out using the manual tile method using anti-A, -B and -AB antisera, along with the micro-column agglutination technique. In addition, because of the possibility of chimerism in the blood group type, the blood sample was analyzed using the transferase method as well as flow cytometry. These revealed a very subtle blood group chimerism that would be overlooked without chromosomal information (Table 1). At first glance, the blood of Twin A was B type, but ABO glycosyltransferase examination revealed that the blood was in fact O type. It was inferred that this was the reason flow cytometry revealed the blood of Twin A to be a type B/O chimera.
Table 1. Blood group typing for the twins. Basic blood groups were the same for both twins. Glycosyltransferase examination showed type B and type O blood types. Flow cytometry showed subtle blood group chimerism

We have been able to observe the twins for up to 5 years of age and have not found any abnormalities in their genitals or development so far. We plan to examine their blood types through HLA typing and DNA polymorphism analysis in the future. At least until puberty, we will continue to observe their mental and physical growth, as well as their reproductive functions.
Discussion
We encountered a very rare case of sex-discordant MC-DZ twins conceived through spontaneous pregnancy who showed chimeric blood group types (Table 1).
Blood chimerism in MC twins occurs via the exchange of blood stem cells between fetuses through vascular anastomoses in the placenta during early pregnancy. To date, 21 cases of sex-discordant MC-DZ twin chimerism with normal phenotypes have been described (Peters et al., Reference Peters, Koning, Verhoeven, Schats, Mijatovic, Ket and Lambalk2017). Most of these cases were fertility-treated pregnancies; there were only two spontaneous pregnancies, which suggests that assisted reproductive technology may be involved in MC-DZ twin development. The occurrence of MC-DZ twins is mainly considered in this manner: the two fertilized eggs are fused before implantation at their outer cell mass; two inner cell masses (ICMs) are formed, leading to a monochorionic–diamniotic placenta (Ogita et al., Reference Ogita, Kajii, Matsuda and Yamamura1991). Such fusion seldom occurs in spontaneous pregnancies because the (spontaneous) fertilization of one egg usually occurs far from the other egg. However, it is quite possible that a similar phenomenon will occur spontaneously as well.
Currently, there are many concerns with the MC-DZ twins because of their dizygocity, as well as the blood traffic between the two infants. First, as a chimera effect, the possibility of freemartinism cannot be completely ruled out. Peters reported that the rate of genital anomalies in sex-discordant twins was 15.4% (Peters et al., Reference Peters, Koning, Verhoeven, Schats, Mijatovic, Ket and Lambalk2017). Furthermore, one girl of the sex-discordant twins had aplasia of Müllerian derivatives, like freemartinism in animals (Bogdanova et al., Reference Bogdanova, Siebers, Kelsch, Markoff, Ropke, Exeler and Wieacker2010). Fortunately, there have been no other reports of freemartinism in human MC-DZ twins; however, long-term, careful observation of genital development and fertility is needed. The effects of chimerism can also affect organs other than the genitals. For example, Brix et al. (Reference Brix, Hansen, Kyvik and Hegedus2009) claim that microchimerism may be involved in the development of thyroid autoantibodies because both female and male twins from opposite-sex pairs have an increased frequency of thyroid autoantibodies, as opposed to monozygotic pairs. More detailed research is needed on the relationship between chimerism in MC-DZ twins and health complications.
In addition, because their genetic information is different, the blood type of each twin may also be different. In fact, there is a report of MC-DZ twins found with blood group type chimeras (Aoki et al., Reference Aoki, Honma, Yada, Momoi and Iwamoto2006). Here, the blood types of the twins showed chimerism, revealing that the twins have different blood types. They likely would not have been identified as blood group chimeras without prior information, due to the extremely biased ratios of their chimerism. Blood group chimeras and combinations thereof can cause confusion and adverse events in blood transfusions or transplantation. Blood group typing in monochorionic diamniotic (MD) twins should thus be performed more carefully because their blood types may be chimeric.
A previous study reported the case of a girl with a sex-discordant chimeric karyotype (because of the tendency of MC-DZ twins) who was misidentified as a boy with gonadal hypoplasia. Her bilateral ovaries had been resected, despite being normal (Johannsen et al., Reference Johannsen, Lundsteen, Visfeldt, Schwartz, Petersen, Byskov and Müller2003). If it had been known then that dizygotic MD twins could exist, the possibility of the patient being a normal girl could have been considered during the evaluation of her karyotype and sex; however, MC-DZ twins are not widely known. Moreover, it is extremely difficult to diagnose MC-DZ twins if there is no difference in phenotypes between the twins, such as heterosexuality or one-sided chromosomal abnormalities. However, these issues also suggest that the presence of MC-DZ twins is far greater than currently reported. MC-DZ twins have multiple and unknown problems. We reported this case with the hope that the pathogenesis, pathophysiology and problems encountered in MC-DZ twins will be further elucidated.
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None.
Ethical standards
Not applicable.