Prevalence of mental illness is notable in people with intellectual disabilities. Reference Dosen1–Reference Cooper, Smiley, Morrison, Williamson and Allan4 Mental health problems have a negative impact on the lives of many people with such disabilities, Reference Brown, Brown and Dibiasio5 and evidence-based interventions tailored to the needs of this vulnerable population are called for. Over past years some reviews have summarised the evidence for a wide range of interventions including psychotherapy and biological and system-level interventions for people with intellectual disabilities and comorbid mental illness. Drawing upon uncontrolled studies or case reports, reviews showed that behavioural interventions – especially cognitive–behavioural therapy (CBT) – are effective in reducing depression, anxiety, anger and challenging behaviour in people with intellectual disabilities. Reference Hatton6,Reference Didden, Korzilius, van Oorsouw and Sturmey7 Furthermore, challenging behaviour has been found to be hardly affected by massage therapy. Reference Chan and Tse8 There is also limited evidence for the use of antipsychotic medication such as risperidone to reduce behaviour problems in people with intellectual disabilities, which also bear a high risk of serious adverse effects. Reference Ulzen and Powers9–Reference Duggan and Brylewski11
Available evidence from controlled studies is scarce when investigating specific interventions or combinations of interventions. For example, a meta-analysis showed rather large effect sizes for anger management in people with intellectual disabilities, albeit based upon only two randomised controlled trials (RCTs) and six non-randomised controlled trials. Reference Hamelin, Travis and Sturmey12 Based on six RCTs, a Cochrane review showed that system-level interventions did not produce significant effects on functioning or quality of life of people with intellectual disabilities and mental health problems. Reference Balogh, Ouellette-Kuntz, Bourne, Lunsky and Colantonio13 However, some meta-analyses using a broader approach including the investigation of a wider range of interventions have been put forth. For example, Heyvaert et al, on the basis of 30 controlled studies, reported an overall large effect (d = 0.671) for interventions targeting challenging behaviour in people with intellectual disabilities, Reference Heyvaert, Maes and Onghena14 which varied by type of intervention (psychotherapy d = 0.752, biological d = 0.646, system-level d = 0.624). Reference Heyvaert, Maes and Onghena14 Furthermore, on the basis of 14 trials, Vereenooghe & Langdon also found a large effect (g = 0.682) for psychotherapy in people with intellectual disabilities, with subgroup analyses showing somewhat higher effect sizes for CBT. Reference Vereenooghe and Langdon15
Taken together, the majority of reviews summarising the evidence on interventions targeting mental health problems in people with intellectual disabilities did not employ a systematic search strategy, did not rely on controlled trials, or included studies with children and adolescents, making questionable the transfer of results to adults. The few meta-analyses reported overall moderate to large effect sizes. Thus, findings should be interpreted with caution as the number of rigorously controlled studies in the field is low, as are sample sizes of included studies, and outcome measures are heterogeneous. Furthermore, there is solid evidence that the manifestations of mental illness and their appropriate treatment options, especially in the case of interventions requiring a fair amount of language skills such as psychotherapy, differ substantially by level of severity of intellectual disabilities. Reference Hatton6,Reference Coelho, Kelley and Deatsman-Kelly16 So far, none of the systematic reviews, except for one, Reference Didden, Korzilius, van Oorsouw and Sturmey7 was tailored to identify evidence for people with a defined severity level of intellectual disabilities (mild, moderate, severe or profound). Findings from the existing reviews, which were not specifically based on studies examining adults with mild to moderate intellectual disabilities, may not be valid for this subgroup. We therefore systematically reviewed the evidence from controlled studies examining the effectiveness of diverse interventions (psychotherapy, biological and system-level approaches) for people with mild to moderate intellectual disabilities and comorbid mental health problems.
Method
The systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist. Reference Moher, Liberati, Tetzlaff and Altman17
Inclusion and exclusion criteria
We included English-language articles published after 1980 reporting the results of randomised controlled trials or controlled studies using parallel group designs to test any type of intervention focusing on the treatment of mental health problems for adults with intellectual disability and comorbid mental illness or behavioural problems. Study participants had to be identified as intellectually disabled with any comorbid mental illness or any behaviour problems. At least 75% of the sample had to be aged 18–64 years and had to function in the range of mild to moderate intellectual disabilities defined by an IQ score of 35–69 or author classification.
We did not include studies in which the intellectual disability levels of participants were not reported, or only an average IQ score was presented without information on the range of IQ scores or the distribution of participants over severity levels of intellectual disability. Studies reporting only scores on the British Picture Vocabulary Scale were excluded as this is a measure of receptive language abilities and thus limited to the verbal component of intelligence. Reference Dunn, Dunn, Whetton and Pintilie18,Reference Beech and Keys19 Studies in which more than 25% of the study participants were outside the designated age range were also excluded. Furthermore, studies testing interventions that aimed at the primary prevention of mental illness or behavioural problems were excluded.
Search strategy
The electronic databases Medline, EMBASE, PsycINFO and EBM Reviews were searched combining key terms describing indications, interventions and study types (see online Table DS1). The electronic search was run in April 2013 and updated in September 2014. References of included studies and related reviews were cross-checked for further relevant literature. We performed a hand search for further relevant literature in the American Journal of Mental Retardation, Journal of Applied Research in Intellectual Disabilities and Journal of Mental Health Research in Intellectual Disabilities. In cases of missing or unclear data we contacted the authors for further information.
Study selection
Each study was independently inspected by two of three reviewers (K.K., K.A. and N.K.). Any disagreements between the reviewers were resolved by discussion.
Data extraction and quality assessment
Variables extracted from primary data were sample size and patient characteristics (gender, age and diagnosis), type of intervention, length of follow-up, design and outcome measures. We extracted any clinical outcomes related to mental health (e.g. symptom severity, psychopathology) and any social outcomes (e.g. quality of life, social functioning) reported in the primary studies. Outcomes were summarised in the following domains: behavioural problems, depressive symptoms, anxiety symptoms, quality of life and functioning. We assessed the quality of the included studies by means of the Cochrane risk of bias tool which consists of seven domains: sequence generation, allocation concealment, masking (blinding) of participants and personnel, masking of outcome assessment, incomplete outcome data, selective outcome reporting and ‘other issues’. Reference Higgins and Green20 Each domain and overall risk of bias was assessed and categorised as low, high or unclear.
Data aggregation
Data synthesis implied both a qualitative analysis to provide a narrative overview and quantitative analyses (meta-analyses) for the five outcome domains which were carried out separately for all trials with sufficient data (mean, standard deviation, number of participants). If studies reported more than one measure in each domain, we calculated a single mean effect for each study. Outcome domains included the following measures:
-
(a) behavioural problems: Checklist of Challenging Behaviour, Stereotypic Self-Stimulating Behavior, the Behavior Checklist, the Aberrant Behavior Checklist, the Modified Overt Aggression Scale, the Provocation Index and the Anger Inventory;
-
(b) depressive symptoms: Beck Depression Inventory and the Automatic Thoughts Questionnaire – Revised;
-
(c) anxiety symptoms: Beck Anxiety Inventory and the Glasgow Anxiety Scale;
-
(d) quality of life: Quality of Life Questionnaire, Manchester Short Assessment of Quality of Life, World Health Organization Quality of Life-Bref and the Comprehensive Quality of Life Scale – Intellectual Disability;
-
(e) functioning: Global Assessment of Functioning, and the American Association for Mental Deficiency Adaptive Behavior Scale.
The direction of effect was standardised with positive values indicating a better outcome in the intervention group. As studies were expected to differ in duration of follow-up, we selected the end-point of the intervention for meta-analysis. Effect sizes and their 95% confidence intervals were calculated as standardised mean differences (SMDs). In case of missing standard deviations, these were calculated (e.g. from standard error) or imputed (from pre-intervention scores) if possible. Effect sizes were interpreted according Cohen's rule of thumb (small 0.20–0.49, medium 0.50–0.79, large 0.8 and higher). Reference Cohen21 The meta-analysis was performed using a random effects model. We calculated I 2 scores to examine heterogeneity between studies. Reference Higgins and Green20 The results of the meta-analysis were presented as forest plots.
Results
The electronic search identified 4602 publications (Fig. 1). Two hand-search runs yielded another 110 potentially relevant articles. After removal of duplicates 3072 studies remained. The initial title and abstract screening identified 146 potentially relevant studies which were screened in full text. Of these, 12 trials fulfilled the inclusion criteria. The main reasons for exclusion were that studies were not controlled or did not report information about the participants' severity of intellectual disability.
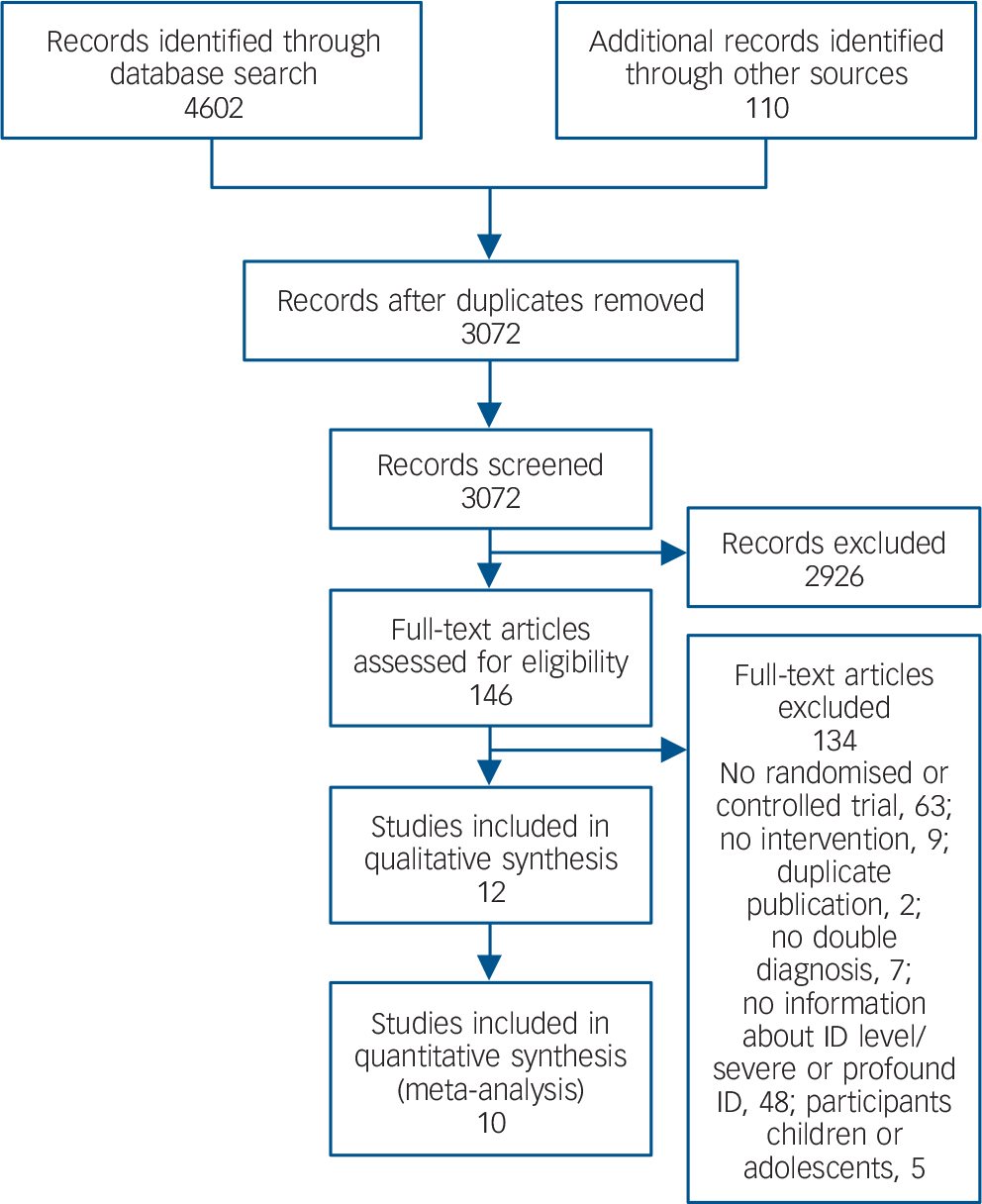
Fig. 1 Selection of studies.
Characteristics of included studies
The included studies were published between 1980 and 2014. Eleven were RCTs, Reference Coelho, Kelley and Deatsman-Kelly16,Reference Chan, Fung, Tong and Thompson22–Reference Willner, Jones, Tams and Green31 and one was a non-randomised study. Reference Benson, Rice and Miranti32 Study characteristics are summarised online in Table DS2. Ten of the twelve included studies were conducted in a single country: USA, Reference Coelho, Kelley and Deatsman-Kelly16,Reference Benson, Rice and Miranti32 UK, Reference Hassiotis, Serfaty, Azam, Strydom, Blizard and Romeo24,Reference Martin, Costello, Leese, Slade, Bouras and Higgins25,Reference Oliver, Piachaud, Tyrer, Regan, Dack and Alexander28,Reference Willner, Rose, Jahoda, Stenfert Kroese, Felce and Cohen30,Reference Willner, Jones, Tams and Green31 Australia, Reference McCabe, McGillivray and Newton26,Reference McGillivray, McCabe and Kershaw27 and China. Reference Chan, Fung, Tong and Thompson22 Six studies were multicentre trials, Reference Gagiano, Read, Thorpe, Eerdekens and van Hove23–Reference Martin, Costello, Leese, Slade, Bouras and Higgins25,Reference Oliver, Piachaud, Tyrer, Regan, Dack and Alexander28–Reference Willner, Rose, Jahoda, Stenfert Kroese, Felce and Cohen30 two of which were multinational – one conducted in South Africa, UK, Canada and Belgium, Reference Gagiano, Read, Thorpe, Eerdekens and van Hove23 and the other in the UK and Australia. Reference Tyrer, Oliver-Africano, Ahmed, Bouras, Cooray and Deb29 Studies were implemented in community, Reference Oliver, Piachaud, Tyrer, Regan, Dack and Alexander28,Reference Tyrer, Oliver-Africano, Ahmed, Bouras, Cooray and Deb29 supported employment, Reference McCabe, McGillivray and Newton26,Reference McGillivray, McCabe and Kershaw27,Reference Benson, Rice and Miranti32 or special service settings. Reference Coelho, Kelley and Deatsman-Kelly16,Reference Chan, Fung, Tong and Thompson22,Reference Hassiotis, Serfaty, Azam, Strydom, Blizard and Romeo24,Reference Martin, Costello, Leese, Slade, Bouras and Higgins25,Reference Willner, Rose, Jahoda, Stenfert Kroese, Felce and Cohen30,Reference Willner, Jones, Tams and Green31 One study did not report the setting. Reference Gagiano, Read, Thorpe, Eerdekens and van Hove23
The mean sample size was 60.3 (s.d. = 44.6; median 48, range 14–179), with larger sample sizes in biological studies. On average 44% (s.d. = 12; median 40) of study participants were female. The majority of study participants were adults. In two studies some participants were less than 18 years old, Reference Chan, Fung, Tong and Thompson22,Reference Benson, Rice and Miranti32, and in four studies a few participants were over 65 years old (maximum 70 years). Reference Coelho, Kelley and Deatsman-Kelly16,Reference Chan, Fung, Tong and Thompson22,Reference Hassiotis, Serfaty, Azam, Strydom, Blizard and Romeo24,Reference Oliver, Piachaud, Tyrer, Regan, Dack and Alexander28 Participants' mental health problems were described as mental disorders or behavioural problems diagnosed according to DSM or ICD-10 criteria in four studies, Reference Coelho, Kelley and Deatsman-Kelly16,Reference Gagiano, Read, Thorpe, Eerdekens and van Hove23–Reference Martin, Costello, Leese, Slade, Bouras and Higgins25 as depressive symptoms in three studies, Reference McCabe, McGillivray and Newton26–Reference Oliver, Piachaud, Tyrer, Regan, Dack and Alexander28 and as behaviour problems including aggressive or inappropriate behaviour or problems handling anger in five studies. Reference Chan, Fung, Tong and Thompson22,Reference Tyrer, Oliver-Africano, Ahmed, Bouras, Cooray and Deb29–Reference Benson, Rice and Miranti32 Interventions delivered were classified as biological (risperidone, risperidone and haloperidol, and multisensory therapy) in three studies, Reference Chan, Fung, Tong and Thompson22,Reference Gagiano, Read, Thorpe, Eerdekens and van Hove23,Reference Tyrer, Oliver-Africano, Ahmed, Bouras, Cooray and Deb29 system-level (assertive community treatment and case management) in three studies, Reference Coelho, Kelley and Deatsman-Kelly16,Reference Martin, Costello, Leese, Slade, Bouras and Higgins25,Reference Oliver, Piachaud, Tyrer, Regan, Dack and Alexander28 and as psychotherapy (CBT) in six studies. Reference Hassiotis, Serfaty, Azam, Strydom, Blizard and Romeo24,Reference McCabe, McGillivray and Newton26,Reference McGillivray, McCabe and Kershaw27,Reference Willner, Rose, Jahoda, Stenfert Kroese, Felce and Cohen30–Reference Benson, Rice and Miranti32 Treatment outcome domains examined were behavioural problems, Reference Coelho, Kelley and Deatsman-Kelly16,Reference Chan, Fung, Tong and Thompson22,Reference Gagiano, Read, Thorpe, Eerdekens and van Hove23,Reference Martin, Costello, Leese, Slade, Bouras and Higgins25,Reference Tyrer, Oliver-Africano, Ahmed, Bouras, Cooray and Deb29–Reference Benson, Rice and Miranti32 depressive symptoms, Reference Hassiotis, Serfaty, Azam, Strydom, Blizard and Romeo24,Reference McCabe, McGillivray and Newton26,Reference McGillivray, McCabe and Kershaw27,Reference Willner, Rose, Jahoda, Stenfert Kroese, Felce and Cohen30 anxiety symptoms, Reference Hassiotis, Serfaty, Azam, Strydom, Blizard and Romeo24,Reference Willner, Rose, Jahoda, Stenfert Kroese, Felce and Cohen30 quality of life, Reference Martin, Costello, Leese, Slade, Bouras and Higgins25,Reference Oliver, Piachaud, Tyrer, Regan, Dack and Alexander28–Reference Willner, Rose, Jahoda, Stenfert Kroese, Felce and Cohen30 and functioning. Reference Coelho, Kelley and Deatsman-Kelly16,Reference Martin, Costello, Leese, Slade, Bouras and Higgins25,Reference Oliver, Piachaud, Tyrer, Regan, Dack and Alexander28 Control conditions were active treatment, Reference Coelho, Kelley and Deatsman-Kelly16,Reference Chan, Fung, Tong and Thompson22,Reference Martin, Costello, Leese, Slade, Bouras and Higgins25,Reference Oliver, Piachaud, Tyrer, Regan, Dack and Alexander28 waiting list, Reference McCabe, McGillivray and Newton26,Reference McGillivray, McCabe and Kershaw27,Reference Willner, Rose, Jahoda, Stenfert Kroese, Felce and Cohen30,Reference Willner, Jones, Tams and Green31 or treatment as usual. Reference Gagiano, Read, Thorpe, Eerdekens and van Hove23,Reference Hassiotis, Serfaty, Azam, Strydom, Blizard and Romeo24,Reference McCabe, McGillivray and Newton26,Reference McGillivray, McCabe and Kershaw27,Reference Willner, Rose, Jahoda, Stenfert Kroese, Felce and Cohen30,Reference Willner, Jones, Tams and Green31 Furthermore, one study compared anger management with three control conditions, Reference Benson, Rice and Miranti32 one placebo-controlled study compared risperidone and haloperidol, Reference Tyrer, Oliver-Africano, Ahmed, Bouras, Cooray and Deb29 and one study compared risperidone with placebo. Reference Gagiano, Read, Thorpe, Eerdekens and van Hove23 Most of the included studies measured the impact of the intervention at the end of treatment or within 3 weeks thereafter. One study assessed the impact of the intervention 6 months after initiation of treatment. Reference Martin, Costello, Leese, Slade, Bouras and Higgins25 All included studies, except for three, Reference Gagiano, Read, Thorpe, Eerdekens and van Hove23,Reference Martin, Costello, Leese, Slade, Bouras and Higgins25,Reference Oliver, Piachaud, Tyrer, Regan, Dack and Alexander28 evaluated long-term effects. Length of follow-up ranged between 5 weeks Reference Chan, Fung, Tong and Thompson22,Reference Benson, Rice and Miranti32 and 2 years. Reference Coelho, Kelley and Deatsman-Kelly16
Risk of bias
The overall methodological quality of the included studies was modest (Fig. 2). With one exception, Reference Tyrer, Oliver-Africano, Ahmed, Bouras, Cooray and Deb29 studies had unclear risk in at least one domain. Furthermore, we judged four studies as having high risk in at least one domain (see online Table DS3). Reference Chan, Fung, Tong and Thompson22,Reference Martin, Costello, Leese, Slade, Bouras and Higgins25,Reference McCabe, McGillivray and Newton26,Reference Benson, Rice and Miranti32
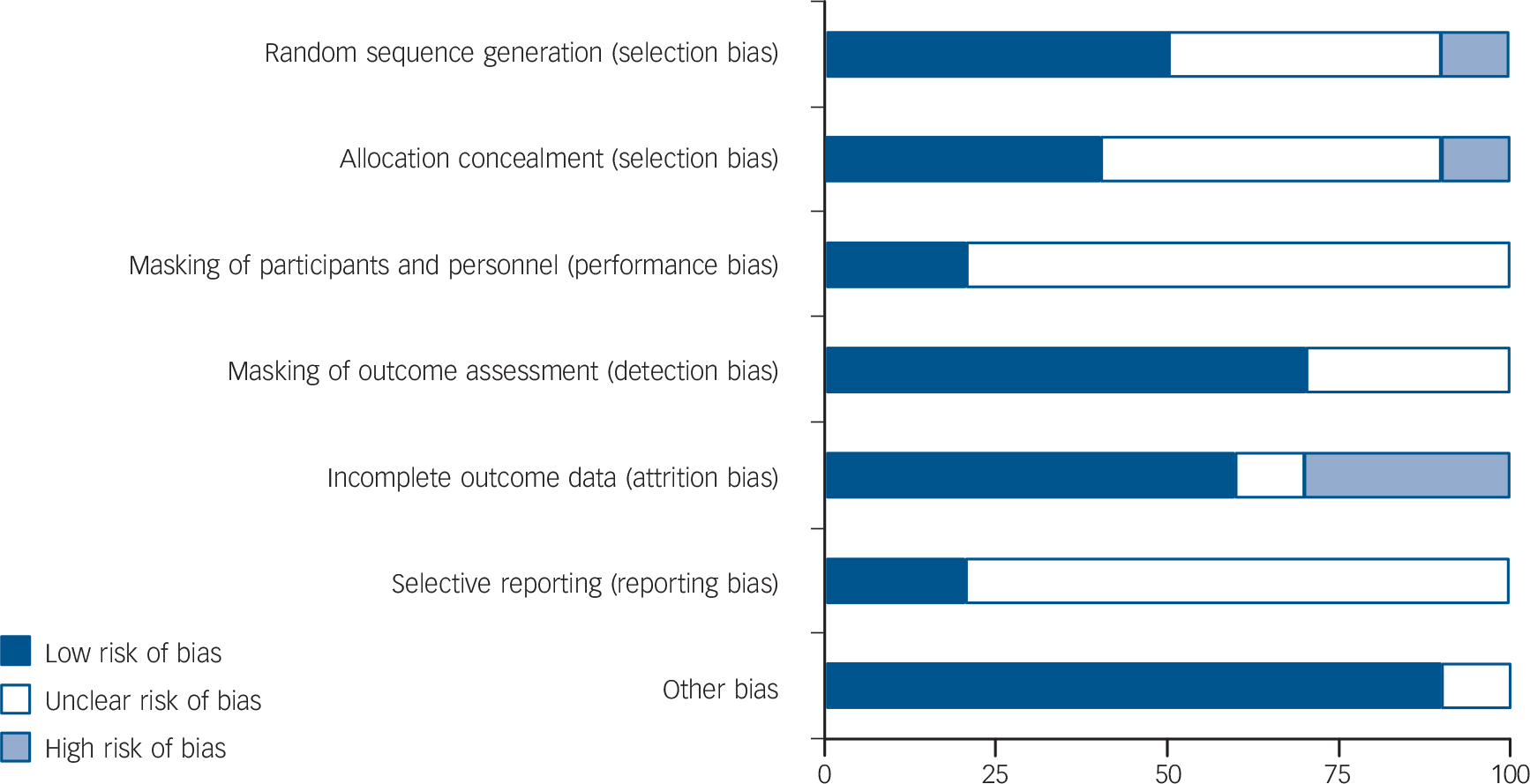
Fig. 2 Risk of bias.
Effects on outcome domains
Of the twelve included studies, two were excluded from quantitative synthesis because of insufficient data or data being markedly skewed, Reference Benson, Rice and Miranti32,Reference Tyrer, Oliver-Africano, Ahmed, Bouras, Cooray and Deb29 resulting in ten studies subjected to meta-analysis.
Behavioural problems
Six studies (total n = 402) showed no overall effect (d = 0.03, 95% CI −0.77 to 0.84; P = 0.94) (Fig. 3). Reference Coelho, Kelley and Deatsman-Kelly16,Reference Chan, Fung, Tong and Thompson22,Reference Gagiano, Read, Thorpe, Eerdekens and van Hove23,Reference Martin, Costello, Leese, Slade, Bouras and Higgins25,Reference Willner, Rose, Jahoda, Stenfert Kroese, Felce and Cohen30,Reference Willner, Jones, Tams and Green31 Interventions delivered were psychotherapy, Reference Willner, Rose, Jahoda, Stenfert Kroese, Felce and Cohen30,Reference Willner, Jones, Tams and Green31 biological treatment, Reference Chan, Fung, Tong and Thompson22,Reference Gagiano, Read, Thorpe, Eerdekens and van Hove23 and system-level approaches, Reference Coelho, Kelley and Deatsman-Kelly16,Reference Martin, Costello, Leese, Slade, Bouras and Higgins25 in two studies each. Heterogeneity was high (I 2 = 92%). A large and statistically significant effect in favour of the control condition was found in one study. Reference Chan, Fung, Tong and Thompson22 All other studies included showed positive effect sizes, although only one study showed a statistically significant effect. Reference Chan, Fung, Tong and Thompson22

Fig. 3 Forest plot of behavioural problems, depressive and anxiety symptoms. SMD, standardised mean difference; SE, standard error.
Depressive symptoms
Four studies, all of which tested psychotherapy (total n = 283), showed a moderate effect size which was non-significant (d = 0.49, 95% CI −0.05 to 1.03; P = 0.08). Reference Hassiotis, Serfaty, Azam, Strydom, Blizard and Romeo24,Reference McCabe, McGillivray and Newton26,Reference McGillivray, McCabe and Kershaw27,Reference Willner, Rose, Jahoda, Stenfert Kroese, Felce and Cohen30 Heterogeneity between studies was high (I 2 = 74%; P = 0.009) (Fig. 3).
Anxiety symptoms
Two studies testing psychotherapy (total n = 185) yielded no significant effect (d = 0.15, 95% CI −0.20 to 0.49; P = 0.41); heterogeneity was low (I 2 = 16%; P = 0.28) (Fig. 3). Reference Hassiotis, Serfaty, Azam, Strydom, Blizard and Romeo24,Reference Willner, Rose, Jahoda, Stenfert Kroese, Felce and Cohen30
Quality of life
Three studies (total n = 179) yielded no significant overall effect (d = −0.33; 95% CI −0.82 to 0.16; P = 0.18). Reference Martin, Costello, Leese, Slade, Bouras and Higgins25,Reference Oliver, Piachaud, Tyrer, Regan, Dack and Alexander28,Reference Willner, Rose, Jahoda, Stenfert Kroese, Felce and Cohen30 Heterogeneity was moderate (I 2 = 44%; P = 0.17) (Fig. 4). One study excluded from meta-analysis did not report a significant effect on quality of life. Reference Tyrer, Oliver-Africano, Ahmed, Bouras, Cooray and Deb29 One intervention was psychotherapy, Reference Willner, Rose, Jahoda, Stenfert Kroese, Felce and Cohen30 and two interventions were system-level. Reference Martin, Costello, Leese, Slade, Bouras and Higgins25,Reference Oliver, Piachaud, Tyrer, Regan, Dack and Alexander28
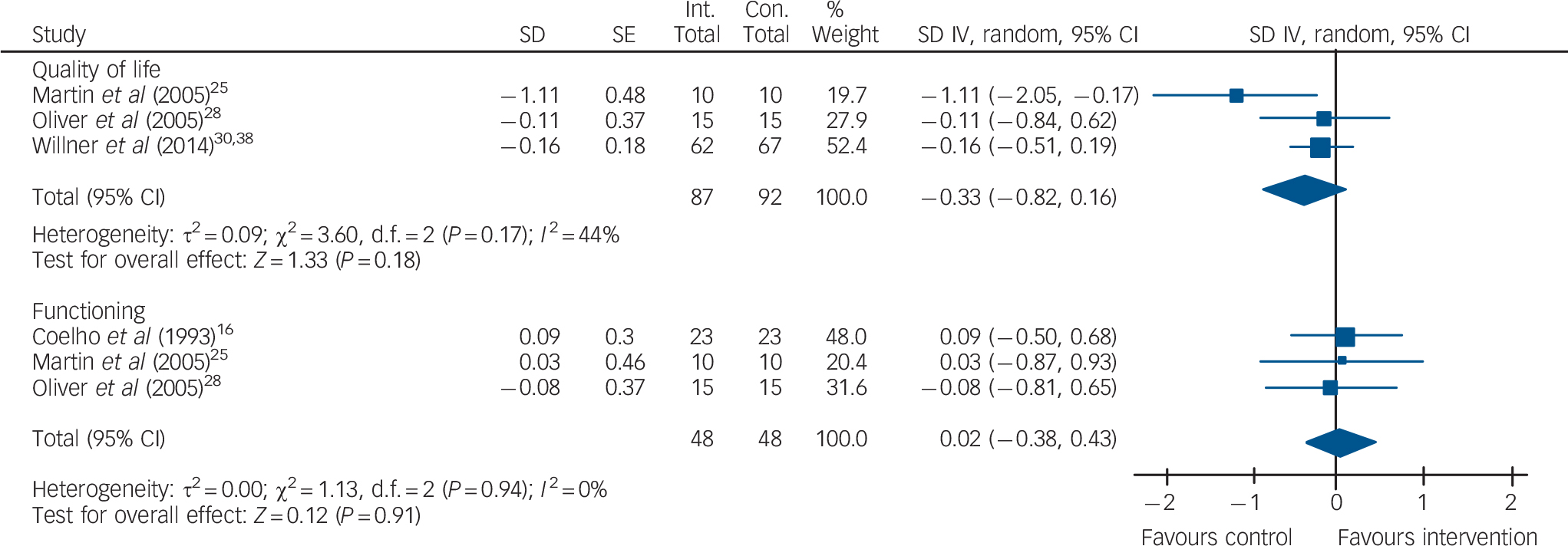
Fig. 4 Forest plot of quality of life and functioning. SMD, standardised mean difference; SE, standard error.
Functioning
Three studies delivering system-level interventions (total n = 96) yielded no effect (d = 0.02, 95% CI −0.38 to 0.43; P = 0.91). Reference Coelho, Kelley and Deatsman-Kelly16,Reference Martin, Costello, Leese, Slade, Bouras and Higgins25,Reference Oliver, Piachaud, Tyrer, Regan, Dack and Alexander28 Heterogeneity between studies was very low (I 2 = 0%; P = 0.94) (Fig. 4).
Discussion
This systematic review identified 12 controlled studies (total n = 724) which investigated the effectiveness of interventions targeting mental health problems in adults with mild to moderate intellectual disability. Meta-analysis showed that none of a wide range of interventions grouped into psychotherapy, biological and system-level approaches was effective in the sense of yielding statistically significant effect sizes for a number of vital outcome domains including behavioural problems, depression, anxiety, quality of life and functioning.
Our finding for interventions targeting problem behaviours is inconsistent with previous reviews where medium to large effect sizes have been reported for psychosocial therapies, especially CBT, Reference Vereenooghe and Langdon15 anger management, Reference Hamelin, Travis and Sturmey12 and behavioural interventions. Reference Didden, Korzilius, van Oorsouw and Sturmey7 This might be due to considerable differences in sampling and methods. Vereenooghe & Langdon included people with all levels of severity of intellectual disabilities, whereas strictly behavioural interventions (e.g. behavioural relaxation), non-traditional and other psychotherapeutic interventions such as life skills training were excluded. Reference Vereenooghe and Langdon15 Also, differences from the positive results of a review of 30 controlled studies which also examined the effects of psychological, biological and system or contextual interventions might be due to differences in selection criteria, resulting in fewer studies being analysed. Reference Heyvaert, Maes and Onghena14 The review of Hamelin et al was restricted to testing one specific intervention, Reference Hamelin, Travis and Sturmey12 and the work of Didden et al was based upon case reports only. Reference Didden, Korzilius, van Oorsouw and Sturmey7 Moreover, only two included studies tested biological interventions, substantiating reservations about using antipsychotics such as risperidone in the treatment of behavioural problems. Reference Gagiano, Read, Thorpe, Eerdekens and van Hove23 Another trial tested ‘multisensory therapy’, yielding a large negative effect which was a significant outlier. Reference Chan, Fung, Tong and Thompson22
For the domain of depressive symptoms, the four included trials testing CBT showed a moderate effect size barely below the threshold of statistical significance. This might be a problem of power, i.e. it is possible that only one or two studies more might produce a significant effect. However, it has to be considered that one of the studies showing only a small effect on depression tested CBT focusing on anger rather than on depression. This said, our findings add to the existing evidence for CBT in the treatment of depression in people with mild to moderate intellectual disabilities. Reference Hatton6,Reference Heyvaert, Maes and Onghena14,Reference Vereenooghe and Langdon15 On the other hand, non-significant negative effects were found for the few interventions targeting quality of life, which were mostly system-level approaches. This finding is in line with another comparable review. Reference Balogh, Ouellette-Kuntz, Bourne, Lunsky and Colantonio13 This does not necessarily indicate a general ineffectiveness of system-level interventions, but might point to a lack of distinction between intervention and control conditions where, for example, assertive community treatment might have not added enough to an already strong routine community care. Reference Burns33 In addition, the amount of available evidence and sample sizes in the included studies were low. Similarly, interventions targeting the outcome domains anxiety and functioning showed no overall effect.
The methodological quality of the included primary studies varied. Randomisation and masking of participants often were not adequately described, and in ten of the twelve included studies it was not clear whether only selected data had been reported. Moreover, this review showed that the majority of included trials focused on global mental health problems deemed specific to people with intellectual disabilities, such as ‘behavioural problems’ including poorly defined conditions such as ‘aggression’ or ‘challenging behaviour’, rather than focusing on clearly diagnosable mental illnesses such as depression or anxiety, or on outcome domains such as quality of life and functioning for which established standardised measures are available. Also, ‘behaviour problems’ have usually been assessed using crude, non-standardised staff ratings. Although some behavioural problems may be a manifestation of an underlying mental illness or appear as a comorbid condition to mental illness, Reference Allen and Davies34,Reference Deb, Chaplin, Sohanpal, Unwin, Soni and Lenotre35 it remains a challenge to research to distinguish clearly between mental illness and behavioural problems in people with intellectual disabilities.
Limitations
Only a small number of studies fulfilled the inclusion criteria, limiting representativeness. Second, heterogeneity of the included studies was substantial, which was especially due to considerable differences in patient characteristics and treatment duration. Third, quite a few of the included studies used waiting lists as a control condition, which might contribute to a ‘door-handle’ effect, i.e. early and possibly lasting improvement due to the expectation that treatment will start soon. Reference Gillespie36 Fourth, our categorisations of both outcome domains and interventions are open to debate. This was especially obvious for the outcome domain of behavioural problems, which consisted of a mix of poorly defined and measured outcomes. There was also considerable variation in the category of biological interventions.
Implications and outlook
For the first time the effectiveness of interventions for people with mild to moderate severity of intellectual disabilities and comorbid mental health problems has been systematically reviewed without any restrictions on the type of intervention or outcome domain. These trials represent an important foundation on which further, larger and more rigorous trials can now be designed. At first glance, the main result – there is no compelling evidence supporting interventions aimed at improving mental health problems in people with mild to moderate intellectual disabilities – is rather sobering. Nonetheless, some single interventions showed impressive effects on a number of outcome domains. Future research efforts should focus on the domains of ‘genuine’ comorbid mental illnesses such as depression and anxiety. Especially CBT seems to be a promising intervention for the treatment of depression, warranting further scrutiny. Finally, efforts should be made toward disentangling the commonly used and nevertheless questionable outcome ‘behavioural problems’, primarily aiming at the development of a sound definition and adequate measurement.
Funding
This work is part of the study Mental Health Care Provision for Adults with Mental Retardation and a Psychiatric Diagnosis (MEMENTA) which has been funded by the German Federal Ministry for Education and Research (grant number 01GY1134).
Acknowledgements
We are grateful to Professor Thomas Becker, Department of Psychiatry II, Ulm University, Germany, for useful comments on an earlier manuscript version.







eLetters
No eLetters have been published for this article.