Research investigating the duration of untreated psychosis (DUP) has invariably reported long average delays from the onset of psychosis to the beginning of treatment (variously defined), usually of 1–2 years (Reference Norman and MallaNorman & Malla, 2001). The distributions of periods of untreated psychosis in these studies have been heavily skewed, the majority of patients accessing treatment within 3–6 months of onset and the minority experiencing delays in excess of a year. Interest in DUP is driven by the apparent association between a long period of untreated psychosis and poor outcomes (Reference Drake, Haley and AkhtarDrake et al, 2000; Reference Addington, Van Mastrigt and AddingtonAddington et al, 2004). A recent meta-analysis of the more methodologically robust studies of DUP and outcomes by Marshall et al (Reference Marshall, Lewis and Lockwood2005) suggests there is a modest association between DUP and outcomes and that this holds independently of premorbid adjustment. However, Verdoux & Cougnard (Reference Verdoux and Cougnard2003) have commented that most studies investigating DUP and outcome have failed to control adequately for potential confounding factors – notably mode of onset – a limitation also acknowledged by Marshall et al (Reference Marshall, Lewis and Lockwood2005). Other methodological inconsistencies limit the comparability of studies, including diagnostically diverse samples and different definitions and measures of DUP (Reference Norman and MallaNorman & Malla, 2001; Reference WarnerWarner, 2005). Conversely, there is a dearth of population-based studies charting DUP, and we still know surprisingly little about the determinants of DUP.
Using data collected as part of a large epidemiological study of first-onset psychosis, we sought to investigate the relationship between DUP and both clinical and social variables. Specifically, we sought to test the hypotheses that a long DUP prior to first contact with services would be independently associated with an insidious mode of onset; socio-demographic factors indicative of social isolation or reduced social functioning (unemployment, living alone, being single); and absence of family involvement in help-seeking.
METHOD
This research forms part of the Aetiology and Ethnicity in Schizophrenia and Other Psychoses (ÆSOP) study. This is a three-centre epidemiological study, conducted over a 2-year period, of all patients with a first episode of psychosis (conforming to ICD–10 codes F20–F29 and F30–F33; World Health Organization, 1992a ) who presented to statutory services within defined catchment areas in south-east London, Nottingham and Bristol, UK; here our data relate only to the first two cities. Potential patients were screened for inclusion using the Screening Schedule for Psychosis (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992). Each patient who screened positive was approached to take part in the study and permission was sought to interview a relative who had had recent contact with the patient. After complete description of the study, written informed consent was obtained from the participants. Exclusion criteria were age under 16 years or over 65 years; evidence of psychotic symptoms precipitated by an organic cause; previous treatment for psychosis; and transient psychotic symptoms resulting from acute intoxication as defined by ICD–10.
Data collection
Duration of untreated psychosis
Data relating to date of onset of psychosis were collated from interviews with the patient and a close relative of the patient, and from clinical notes using the World Health Organization (WHO) Personal and Psychiatric History Schedule (PPHS; World Health Organization, 1996). Duration of untreated psychosis was defined as the period in weeks from the onset of psychosis to first contact with statutory mental health services. In line with previous studies (Reference Craig, Bromet and FennigCraig et al, 2000), onset of psychosis was defined as the presence for 1 week or more of one of the following psychotic symptoms: delusions; hallucinations; marked thought disorder; marked psychomotor disorder; and bizarre, grossly inappropriate and/or disorganised behaviour with a marked deterioration in function. A rating of onset was made only when there was a clear, unequivocal description from any source of symptoms meeting these criteria. Previous studies have used a number of different end-points in defining DUP, including first admission (Reference Craig, Bromet and FennigCraig et al, 2000) and start of antipsychotic medication (Reference Norman and MallaNorman & Malla, 2001). For our study, patients were included whether they were admitted to hospital or treated in the community, and not all were prescribed anti-psychotic medication within the time frame of the study. Our end-point, therefore, was contact with mental health services. Interrater reliability was assessed for the authors who rated DUP (C.M., R.A., J.M.L.) by each independently rating DUP on a random subset of 50 participants. Reliability was satisfactory: intraclass correlation (two-way mixed) r=0.903.
Clinical data
Mode of onset and diagnostic data were collected using the Schedules for Clinical Assessment in Neuropsychiatry (SCAN; World Health Organization, 1992b ) and the PPHS. Mode of onset was operationalised and rated according to the three main categories in the PPHS:
-
(a) sudden (psychotic symptoms appeared within days of first noticeable behavioural change);
-
(b) acute (psychotic symptoms appeared within 1 month of first noticeable behavioural change);
-
(c) insidious (psychotic symptoms appeared incrementally over a period of more than 1 month since first noticeable behavioural change).
This is in line with how mode of onset was defined in the WHO studies of the incidence and outcome of schizophrenia (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992) and, as in previous studies (Reference Harrison, Croudace and MasonHarrison et al, 1996), for the purposes of the analysis patients were grouped into two categories: acute (comprising the sudden and acute modes) and insidious.
The ICD–10 diagnoses were determined using data from the SCAN (which incorporates the Present State Examination version 10) on the basis of consensus meetings involving one of the ÆSOP study's senior psychiatrists (J.L. or R.M. in London and P.J. in Nottingham) and other members of the research team. Full details are provided in the report by Kirkbride et al (Reference Kirkbride, Fearon and Morgan2006). For the analysis, patients were grouped into two categories of diagnosis: schizophrenia and non-affective psychoses (ICD–10 codes F20–29) and affective psychoses (ICD–10 codes F30–33).
Social data
Data on ethnicity, gender, educational level achieved, employment status, living circumstances and relationship status at contact with services were collected using the Medical Research Council Socio-Demographic Schedule (available from the authors upon request). Data on the pathway to care and family involvement in seeking help were collected using the PPHS.
Analysis
Comparisons between groups in the sample were conducted using χ2 and t-tests, as appropriate. Our approach to analysing the relationship between DUP and other variables was informed by the facts that the distribution of periods of untreated psychosis in our sample was heavily skewed, making the use of non-parametric statistics appropriate, and that DUP is time-to-event data. We began by describing the median DUP for each group within each variable of interest and conducting preliminary analyses of differences between groups using Wilcoxon rank-sum tests. Univariable associations between DUP and other variables were further analysed using survival analysis, with onset of psychosis as the entry point and contact with services as the end-point. We constructed Kaplan–Meier survival curves and, following Pocock et al (Reference Pocock, Clayton and Altman2002), present these going upwards to represent the cumulative probability of contact with services over time in different groups. To aid interpretation of these plots, 95% confidence intervals are displayed at regularly spaced intervals, and the x-axis is halted at the point at which the number of remaining participants became unduly small, in this case at 18 months. Log-rank tests were performed to assess whether the probability of contact over time differed between groups. Initially, univariable analyses were conducted with the data stratified by study centre to assess whether the same variables were correlated with DUP in both centres. We found this to be the case (data not shown) and consequently all univariable analyses are presented with data from both centres combined. Cox regression was used to confirm and quantify univariable associations in terms of the hazard ratio, and to investigate whether observed associations were independent of potential confounders. For these multivariable analyses, a variable for study centre was always included to adjust for any confounding effects of study setting. All analyses were conducted using Stata version 8 for Windows.
RESULTS
During the study period we identified 511 patients: 308 in south-east London and 203 in Nottingham. Of these, sufficient information was available to rate DUP for 495 (96.9%). There was no evidence of any significant difference between those for whom information was available to rate DUP and those for whom it was not (data not shown). The small number of patients for which other data were missing were included and the missing values are noted in the relevant tables. There was no evidence that the proportion of missing values varied systematically between key groups in the sample.
Of the 495 patients included in the analysis, key informant data were available for 328 (66.3%). Case notes were scrutinised for all patients. There was no evidence of any significant difference in socio-demographic or clinical characteristics or in DUP between those for whom information from a key informant was available and those for whom it was not (Table 1).
Table 1 Social and clinical variables by informant interview

| Informant interview | ||||
|---|---|---|---|---|
| Yes (n=328) | No (n=167) | Statistical test | P | |
| DUP, weeks: median (IQR) | 8 (2-37) | 12 (3-49) | z=1.70 | 0.09 |
| Gender, n (%) | ||||
| Male | 184 (56.1) | 102 (61.1) | χ2=1.13, d.f.=1 | 0.29 |
| Female | 144 (43.9) | 65 (38.9) | ||
| Age at onset, n (%) | ||||
| 16-29 years | 187 (57.0) | 100 (60.2) | χ2=0.47, d.f.=1 | 0.49 |
| 30-65 years | 141 (43.0) | 66 (39.8) | ||
| Age at contact, n (%) | ||||
| 16-29 years | 174 (53.1) | 90 (53.9) | χ2=0.03, d.f.=1 | 0.86 |
| 30-65 years | 154 (46.9) | 77 (46.1) | ||
| Ethnicity, n (%) | ||||
| White British | 155 (47.3) | 62 (37.1) | χ2=9.18, d.f.=5 | 0.10 |
| Other White | 22 (6.7) | 17 (10.2) | ||
| African—Caribbean | 84 (25.6) | 45 (27.0) | ||
| Black African | 39 (11.9) | 29 (17.4) | ||
| Asian (all) | 19 (5.8) | 6 (3.6) | ||
| Other | 9 (2.7) | 8 (4.8) | ||
| Living circumstances, n (%)1 | ||||
| Lives alone | 147 (45.0) | 73 (44.0) | χ2=0.04, d.f.=1 | 0.84 |
| Lives with others | 180 (55.0) | 93 (56.0) | ||
| Relationship status, n (%)2 | ||||
| Single | 234 (71.8) | 112 (74.2) | χ2=0.30, d.f.=1 | 0.59 |
| In stable relationship | 92 (28.2) | 39 (25.8) | ||
| Education, n (%)3 | ||||
| Up to age 16 years | 206 (62.8) | 87 (56.1) | χ2=2.20, d.f.=1 | 0.33 |
| Age 16-18 years | 83 (25.3) | 44 (28.4) | ||
| Over age 18 years | 39 (11.9) | 24 (15.5) | ||
| Employment status, n (%)4 | ||||
| Unemployed | 203 (61.9) | 106 (65.0) | χ2=0.46, d.f.=1 | 0.50 |
| Other | 125 (38.1) | 57 (35.0) | ||
| Mode of onset, n (%)5 | ||||
| Sudden (< 1 week) | 69 (22.2) | 28 (17.6) | χ2=1.70, d.f.=2 | 0.43 |
| Acute (< 1 month) | 83 (26.7) | 41 (25.8) | ||
| Insidious (> 1 month) | 159 (51.1) | 90 (56.6) | ||
| Diagnosis, n (%) | ||||
| Non-affective psychosis | 228 (69.5) | 127 (76.0) | χ2=2.33, d.f.=1 | 0.13 |
| Affective psychosis | 100 (30.5) | 40 (24.0) | ||
Sample characteristics
Across the whole sample the median DUP was 9 weeks (interquartile range (IQR) 2–40) and the mean was 58 weeks (s.d.=148). As in all previous research the distribution of DUP was heavily skewed, with a majority of patients making contact with services within 10 weeks of onset and a small number accessing services only after a very long delay, in several cases in excess of 2 years. The average age at onset in the full sample was 30 years (s.d.=10); this was significantly lower for men (mean 29 years; s.d.=10) than for women (mean 32 years; s.d.=10); t=–3.45, P<0.001. Table 2 shows the social and clinical characteristics of the sample.
Table 2 Social and clinical characteristics of full sample

| Total sample (n = 495) | |
|---|---|
| DUP, weeks | |
| Median (IQR) | 9 (2-40) |
| Mean (s.d.) | 58 (148) |
| Gender, n (%) | |
| Male | 286 (57.8) |
| Female | 209 (42.2) |
| Age at onset, n (%) | |
| 16-29 years | 288 (58.2) |
| 30-65 years | 207 (41.8) |
| Age at contact, n (%) | |
| 16-29 years | 264 (53.3) |
| 30-65 years | 231 (46.7) |
| Ethnicity, n (%) | |
| White British | 217 (43.8) |
| Other White | 39 (7.9) |
| African—Caribbean | 129 (26.1) |
| Black African | 68 (13.7) |
| Asian (all) | 25 (5.1) |
| Other | 17 (3.4) |
| Living circumstances, n (%)1 | |
| Lives alone | 220 (44.6) |
| Lives with others | 273 (55.4) |
| Relationship status, n (%)2 | |
| Single | 346 (72.5) |
| In stable relationship | 131 (27.5) |
| Education, n (%)3 | |
| Up to age 16 years | 293 (60.7) |
| Age 16-18 years | 127 (26.3) |
| Over age 18 years | 63 (13.0) |
| Employment status, n (%)4 | |
| Unemployed5 | 309 (62.9) |
| Other6 | 182 (37.1) |
| Family involvement in help-seeking, n (%)7 | |
| No | 265 (57.1) |
| Yes8 | 199 (42.9) |
| Mode of onset, n (%)9 | |
| Sudden (< 1 week) | 97 (20.6) |
| Acute (< 1 month) | 124 (26.4) |
| Insidious (> 1 month) | 249 (53.0) |
| Diagnosis, n (%) | |
| Non-affective psychosis | 355 (71.7) |
| Affective psychosis | 140 (28.3) |
Patients in London were more likely to live alone, more likely to live in rented accommodation and less likely to have any family involved in seeking help. The London sample was also more ethnically diverse than the Nottingham sample (data not shown). There was some evidence that DUP was generally longer for London patients than for Nottingham patients when data were analysed using the Wilcoxon rank-sum test (z=1.94, P=0.053); however, the association was weaker when assessed using survival analysis and the log-rank test (survival curve not shown; log-rank test χ2=2.34, d.f.=1, P=0.126). As noted above, initially univariable analyses were conducted with the data stratified by study centre; as there was no evidence that the effect of any variable on DUP varied by study site, all analyses are presented below with data from both centres combined.
Clinical and social correlates of DUP
Clinical variables
There was strong evidence of an association between DUP and mode of onset. In the full sample, the median DUP for those with an insidious onset of psychosis was 32 weeks (IQR 11–99) compared with a median of 3 weeks (IQR 1–8) for those with an acute onset (z=–13.00, P<0.001). This difference was equally evident using survival analysis. The Kaplan–Meier survival curves (Fig. 1) reveal a clear divergence in the cumulative probability of contact following onset of psychosis according to mode of onset (log-rank test χ2=211.41, d.f.=1, P<0.001). There is a clear pattern for the majority of those with an acute onset to present within 10 weeks of onset, with a small number taking much longer, in contrast to those with an insidious onset, whose time to presentation is more evenly distributed.
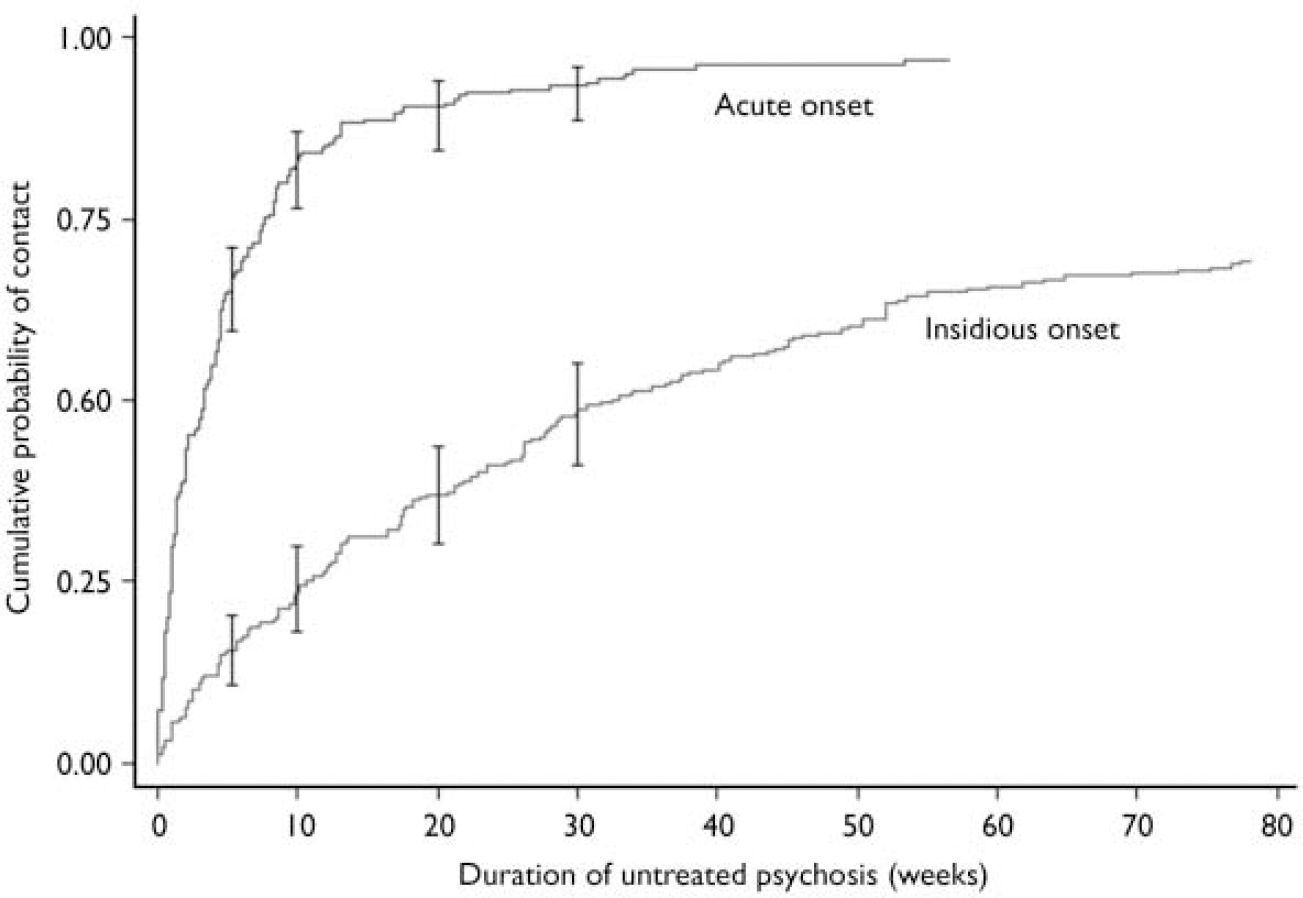
Fig. 1 Survival curves for mode of onset (with 95% CI bars).
There were also notable differences in DUP by diagnostic group. The median DUP for those with a diagnosis of schizophrenia or other non-affective psychosis was 13 weeks (IQR 3–53) compared with a median of 5 weeks (IQR 1–17) for those with an affective psychosis (z=4.84; P<0.001). Survival analysis confirmed this difference (survival curve not shown; log-rank test χ2=26.20, d.f.=1; P<0.001). Not surprisingly, mode of onset and diagnosis were also strongly correlated with each other, with those with a diagnosis of schizophrenia or other non-affective psychosis being more likely to experience an insidious onset (χ2=14.39, d.f.=1, P<0.001).
Pathway and social variables
Of the social variables considered, employment status and family involvement in help-seeking were associated with DUP. The median DUP for those who were unemployed was 13 weeks (IQR 4–52) compared with 5 weeks (IQR 1–19) for those who were employed or students (z=4.64, P<0.001). Once again, this association was evident in the Kaplan–Meier survival curves for employment status (Fig. 2), which show a clear divergence in the cumulative probability of contact between the two groups over time (log-rank test χ2=24.91, d.f.=1, P<0.001).
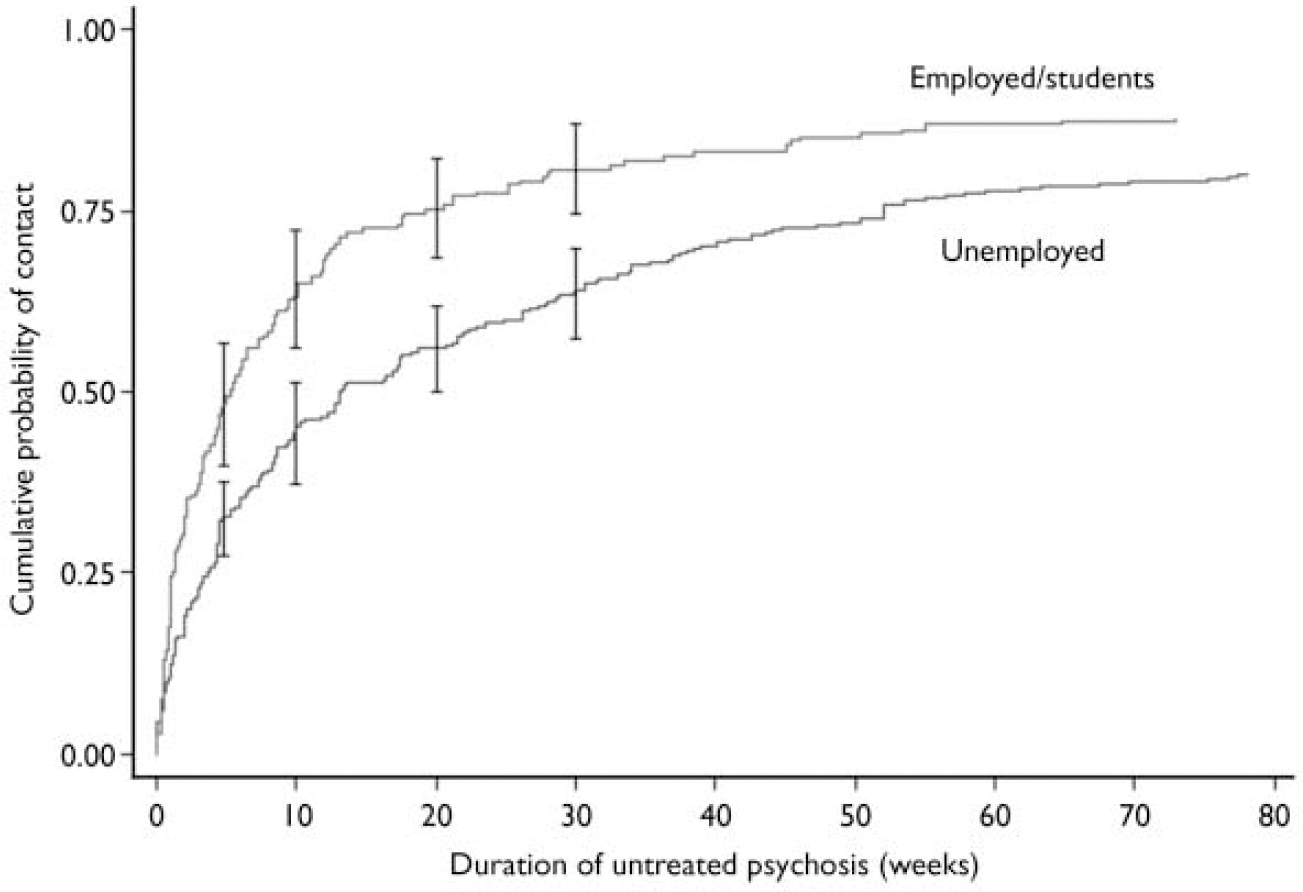
Fig. 2 Survival curves for employment status (with 95% CI bars).
For those whose family was involved in seeking help, the median DUP was 5 weeks (IQR 1–27) compared with a median of 12 weeks (IQR 3–54) for those who did not have any family involved (z=–3.80, P<0.001). Survival analysis confirmed this (survival curve not shown; log-rank test χ2=15.22, d.f.=1, P<0.001). There was no evidence in either centre of an association between DUP and any of the other variables considered: age at onset, gender, living alone, level of education, ethnicity and source of referral (including by a general practitioner).
Independent predictors of DUP
The next stage in the analysis sought to probe these associations further using Cox regression to quantify associations in terms of the hazard ratio, and to adjust for potential confounders. As the end-point for the analyses was contact with services, a hazard ratio less than 1 indicates a longer DUP on average (i.e. a lower ‘risk’ of contact with services) and a hazard ratio greater than 1 indicates a shorter DUP on average (i.e. a higher ‘risk’ of contact with services). Table 3 shows the unadjusted and adjusted hazard ratios for each variable crudely associated with DUP and for study centre. The adjusted hazard ratios are adjusted for age at onset, gender, ethnicity and all other variables listed in the table.
Table 3 Unadjusted and adjusted hazard ratios for contact with services over time following onset of psychosis

| Unadjusted hazard ratio (95% CI) | P | Adjusted hazard ratio1,2 (95% CI) | P | |
|---|---|---|---|---|
| Nottingham (v. south-east London) | 1.15 (0.96-1.38) | 0.129 | 1.22 (0.96-1.54) | 0.097 |
| Unemployed (v. other) | 0.63 (0.52-0.75) | < 0.001 | 0.78 (0.64-0.96) | 0.021 |
| Family involvement (v. none) | 1.44 (1.20-1.74) | < 0.001 | 1.24 (1.01-1.51) | 0.038 |
| Insidious (v. acute) mode of onset | 0.24 (0.19-0.29) | < 0.001 | 0.27 (0.22-0.34) | < 0.001 |
| Affective (v. non-affective) psychosis | 1.67 (1.37-2.04) | < 0.001 | 1.25 (0.99-1.57) | 0.056 |
The unadjusted hazard ratios confirm the strong crude associations between DUP and mode of onset, diagnosis, employment status and family involvement, and the weak association between DUP and study centre. After adjusting for other variables, mode of onset, employment status and family involvement retained strong independent effects on DUP. An insidious mode of onset, for example, was associated with a substantially longer DUP on average compared with an acute onset, independent of other factors (adjusted HR=0.27, 95% CI 0.22–0.34). There was no evidence that the relationship between DUP and mode of onset varied by diagnosis. Unemployment had a similar, if less strong, effect (adjusted HR=0.78, 95% CI 0.64–0.96). Conversely, if family members were involved in seeking help, the time from onset to contact was on average shorter, independent of other variables in the model (adjusted HR=1.24, 95% CI 1.01–1.51). The evidence was less clear regarding diagnosis. After adjusting, affective psychosis was only marginally associated with an increased likelihood of contact over time (i.e. with a shorter DUP on average) compared with non-affective psychosis (adjusted HR=1.25, 95% CI 0.99–1.57). Finally, the adjusted hazard ratio for study centre was slightly greater than the unadjusted hazard ratio (adjusted HR=1.22, 95% CI 0.96–1.54).
DISCUSSION
This study is the largest population-based investigation of first-episode psychosis to report on DUP and associated variables. It is also the first such study conducted simultaneously in two distinct settings within a single country using an identical methodology.
Conceptual and methodological issues
The development and early course of psychosis have generally been divided into three phases: the premorbid period, the prodromal period and the first psychotic episode. Mode of onset relates to the prodromal period; it categorises the period of the development of psychotic symptoms according to the speed at which they emerge. However, in cases where psychosis emerges insidiously, it is more difficult to draw a clear line between the prodrome and psychotic episode; the two phases blur into each other, making the potential for measurement error greater. It is possible, for example, that the presence of unusual perceptual experiences or odd beliefs during the prodromal period can lead to onset being dated too early in such cases (i.e. before the criteria for onset of psychosis, set out above, are fully met). If true, this would overstate the strength of any association between an insidious mode of onset and a long DUP. We were careful to distinguish mode of onset from the date of onset and subsequent DUP when making ratings, and examination of the data suggests we were able to do this. For example, although the association between DUP and mode of onset was strong, it was far from perfect: Fig. 1 clearly shows that many people with an acute mode of onset experienced long periods of untreated psychosis and, conversely, that a number of people with an insidious onset had a relatively short DUP. The possibility of measurement error none the less remains and this adds an important note of caution regarding the strength of the association we observed between mode of onset and DUP. Indeed, it remains an important methodological point for future research, given that our approach to rating the onset of psychosis is consistent with that employed in other studies in this field. Further, the difficulties encountered in some cases in drawing a line between mode of onset or prodrome and the beginning of a psychotic episode inevitably poses challenging questions about how the early course of psychosis is currently being conceptualised.
Norman & Malla (Reference Norman and Malla2001) highlighted a number of differences between studies of DUP that limit their comparability, most notably in relation to how DUP has been defined. Unlike many researchers, we used service contact as the end-point because our sample included patients treated in the community and patients who were not prescribed antipsychotic medication within the time frame of the study. None the less, all patients were assessed by, and received input from, mental health services (i.e. treatment, broadly defined), and although our definition of the end-point may limit direct comparisons with some other studies, it has the advantage that ours is one of the few studies to include non-hospitalised patients, which reduces selection bias related to treatment decisions and illness severity. Further, it is unlikely that many patients were treated in a primary care setting prior to referral to mental health services. Only 160 (34%) of the patients in our sample were referred to services through primary care (Reference Morgan, Mallett and HutchinsonMorgan et al, 2005), and prior to beginning any treatment for first-episode psychosis, referral for assessment to secondary services is recommended (Reference LesterLester, 2001). Further, as far as we could ascertain, in only 4 (2.5%) of 160 patients referred by a general practitioner, was the patient prescribed antipsychotic medication prior to contact with services. In all 4 patients the general practitioner started antipsychotic medication pending referral to services, and in no patient did contact with services occur more than 2 weeks after antipsychotic medication was prescribed. Consequently, although some patients did receive anti-psychotic medication for a short period prior to contact with secondary mental health services, this number was small and would not affect our results. In general, given the varying definitions, absolute estimates of DUP have to be considered cautiously. However, this should not undermine comparisons of DUP between groups within individual studies, if the definitions have been applied reliably. Our interrater reliability exercise showed very good reliability between those rating DUP.
To rate DUP we used all available information from interviews with patients and relatives and from case records; for a proportion of patients the only available information was from case records. We made a series of comparisons between patients for whom we had key informant data and those for whom we did not, to assess whether there was any notable difference between them and to assess whether there was any evidence of systematic information bias. There was no evidence of any difference between the groups; importantly, there was no evidence of a systematic difference in estimates of DUP (see Table 1). Furthermore, we were not able to investigate the role of substance use (or indeed other possible factors such as stigma and beliefs about mental illness and mental health services) in determining DUP, as these data were not appropriately recorded for this study. This is a limitation that needs to be considered in future research.
Comparisons with previous research
We found some evidence that DUP varied by study setting: in general, periods of untreated psychosis were shorter in Nottingham than in south-east London. Although our findings in relation to this were not strong, they raise the important possibility that DUP may (and perhaps should be expected to) vary across different settings. However, the same variables were associated with DUP in the two samples; some factors, it seems, increase DUP independently of the overall social and service context.
Clinical correlates
We found strong evidence to support our first hypothesis that an insidious mode of onset would be associated with a long DUP; this held when other variables, including diagnosis, were adjusted for. This replicates findings from smaller studies (Reference Larsen, McGlashan and MoeLarsen et al, 1996) and is not surprising. Research from the social sciences shows that a common response to the development of psychosis within families is an attempt to normalise and adjust to the associated behaviours. Where the development of psychosis is characterised more by negative symptoms and is spread over a long period, and the subsequent transition less dramatic, the potential for families and others to adjust and consequently delay involving external agencies is no doubt greater. Individuals with psychosis may also be able to adjust their own lifestyles to minimise the disruption and visibility of their disorder. The reverse holds where the onset is acute and involves a rapid transformation in behaviour.
In relation to diagnosis, there was a tendency for DUP to be longer in those with a diagnosis of a non-affective psychosis compared with those with an affective psychosis. Only a limited number of previous studies have reported on DUP and diagnosis, and all have reported similar findings to ours. Craig et al (Reference Craig, Bromet and Fennig2000), for example, in a population-based study of 429 first-admission patients reported a significantly longer median DUP for patients with schizophrenia spectrum disorders (14 weeks) than for those with a manic psychosis (1 week) or with a depressive psychosis (3 weeks), findings notably similar to ours. In our study we were able to take the next step in adjusting for potential confounders of the association between DUP and diagnosis, notably mode of onset. When we did this, the hazard ratio was markedly reduced, suggesting that much of the difference in DUP between non-affective and affective psychosis can be accounted for by related differences in, for instance, mode of onset.
Pathway and social correlates
Our second hypothesis, that indicators of social isolation or poor social functioning would be associated with a long DUP, was only partially supported. Of the social variables considered, employment status had the strongest relationship with DUP, a finding that has been reported in previous studies (Reference Barnes, Hutton and ChapmanBarnes et al, 2000). It is not clear, however, whether being unemployed leads to a long DUP, perhaps through reducing the visibility of psychosis and its socially disruptive effects, or whether a long DUP contributes to increasing social withdrawal and reduced function, one consequence of which is unemployment. Our final hypothesis, that a long DUP would be associated with absence of family involvement in the pathway to care, was supported – a finding that ties in with research showing social networks to be particularly important in facilitating access to care (Reference Morgan, Mallett and HutchinsonMorgan et al, 2005). That said, in contrast to some previous studies (Reference Drake, Haley and AkhtarDrake et al, 2000; Reference Skeate, Jackson and BirchwoodSkeate et al, 2002), we found no association between living alone and other possible indicators of social isolation and a long DUP, or between source of referral and a long DUP.
Determinants, implications and confounders
Our findings suggest that the length of time between the onset of psychosis and contact is influenced by features of both the illness (mode of onset, initial diagnosis) and the person's social context (family involvement, employment, local setting). Understanding what influences the time between onset and contact with services is important in informing services about the types of strategies that are likely to help reduce delays. Our findings suggest that DUP is at least partly shaped by malleable social factors, and as such should be amenable to socially oriented interventions.
The more challenging issue is whether DUP has an independent effect on outcomes. This is an important question, given that the assumption underpinning the development of early intervention services in the UK and elsewhere is that DUP does have an impact on outcomes and that reducing it not only alleviates unnecessary suffering but also contributes to improving outcomes. Our data suggest that a long DUP is correlated with an early illness course characterised by an insidious onset, a non-affective diagnosis, and reduced social networks and social function. Each of these has been linked to poorer outcomes, particularly insidious onset (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992; Reference Harrison, Croudace and MasonHarrison et al, 1996). Although the conceptual questions regarding mode of onset noted above necessarily temper any conclusions drawn from our data, one interpretation is that these features of early illness course are reflections of a more severe and chronic underlying illness, hence the strong associations with poor outcomes, particularly continuous illness course and negative symptoms. As yet there is only limited research that has adjusted for potential confounders, mainly premorbid functioning (Reference Harrigan, McGorry and KrstevHarrigan et al, 2003; Reference Addington, Van Mastrigt and AddingtonAddington et al, 2004; Reference Perkins, Lieberman and GuPerkins et al, 2004; Reference Marshall, Lewis and LockwoodMarshall et al, 2005), and the effects of mode of onset and length of prodrome have been explored in only a small number of studies (Reference Verdoux, Liraud and BergeyVerdoux et al, 2001; Reference Harrigan, McGorry and KrstevHarrigan et al, 2003). It consequently remains possible that the association between DUP and outcomes is confounded, and while this remains the case greater caution is needed before basing wholesale service reforms on the reported association between DUP and outcomes.
Acknowledgements
We wish to thank the ÆSOP researchers who helped with data collection. We are grateful to mental health services and patients in Bristol, Nottingham and south-east London for their cooperation and support with this study, and to the UK Medical Research Council and the Stanley Medical Research Institute for funding.
Members of the ÆSOP Study Group are as follows: Glynn Harrison, John Holloway, Florence Muga (Bristol); Peter Jones, Rudwan Abdul-Al, Maureen Ashby, Alan Fung, Hazel Hayhurst, James Kirkbride, Jouko Mietunen (Cambridge); Robin Murray, Julian Leff, Stefan Auer, Jane Boydell, Rachel Burnett, Ben Chapple, Tom Craig, Paola Dazzan, Kimberlie Dean, Arsime Demjaha, Rina Dutta, Paul Fearon, Francena Fonseca, Marta Di Forti, Helen Fisher, Ayana Gibbs, Kathy Greenwood, Edwin Gwenzi, Tirril Harris, Gerard Hutchinson, Samantha Jones, Maria Lambri, Julia Lappin, Noel Kennedy, James McCabe, Laura McIntosh, Rosemarie Mallett, Ana Martinez, Ana Miorelli, Craig Morgan, Kevin Morgan, Kris Naudts, Kenneth Orr, Per Rohebak, Jeza Salvo, Chiara Samele, Mandy Sharpley, Simon Vearnals, Jolanta Zanelli (London); Peter Jones, Hemant Bagalkote, Daphne Boot, John Brewin, Gill Doody, Becci Dow, Annette Farrant, Steve Jones, Tuhina Lloyd, Ian Medley, Ramona Moanette, Shilpa Nairi, Mark Ruddell, Jayne Simpson, Sirip Suranim, Jane Tarrant, Philip Whitehead, Pat Williams, Sue Window (Nottingham).








eLetters
No eLetters have been published for this article.