T wave inversions were defined as a negative T-wave ≥ 1 mm in depth in two or more contiguous leads, with exclusion of leads aVR, III, and V1. Reference Sharma, Drezner and Baggish1 The current literature reports a T wave inversion prevalence of 2% in young general population (16–35 years) Reference Malhotra, Dhutia and Gati,2 about 3% in young athletes Reference Wilson, Sharma and Carré3 and 5–16% in younger children. Reference Migliore, Zorzi and Michieli4,Reference D’Ascenzi, Anselmi and Berti5
Since the presence of T wave inversions can represent one of the criteria for the diagnosis of arrhythmogenic right ventricular cardiomyopathy and other cardiomyopathies, Reference Corrado, Zorzi and Cipriani6 this finding is subject to scrupulous attention by cardiologists. A comparison was made in the application of diagnostic criteria for arrhythmogenic right ventricular cardiomyopathy in young athletes with and without T wave inversions and in subjects affected by arrhythmogenic right ventricular cardiomyopathy. Reference Zaidi, Sheikh and Jongman7 The results showed that isolated anterior T wave inversions do not discriminate between patients with arrhythmogenic right ventricular cardiomyopathy and healthy athletes. So T wave inversions could be a diagnostic criterion for arrhythmogenic right ventricular cardiomyopathy but it is also a common feature of the so-called “athlete’s heart.” We know from literature that the morphological characteristics of the athlete’s heart may overlap with some structural and electrical cardiac diseases Reference Palermi, Cavarretta and D’Ascenzi8 and that adding second and third-level exams can help to differentiate the two conditions. T wave inversions may also represent an early sign of hypertrophic cardiomyopathy Reference Elliott, Anastasakis and Borger9 but diagnosis is often associated with other electrocardiographic signs and echocardiographic evidences. The latest research carried out on the paediatric population reveals that T wave inversions are found more frequently in the anterior precordial leads (V1-V3) than in the inferior-lateral leads; in particular, those in the anterior leads are considered a normal finding in children, which disappear with growth in most cases. Reference Wilson, Sharma and Carré3–Reference D’Ascenzi, Anselmi and Berti5 On the other hand, inferior-lateral T wave inversions are not so frequent, they tend to persist and may represent an early sign of cardiomyopathy. Reference Wilson, Sharma and Carré3–Reference D’Ascenzi, Anselmi and Berti5,Reference D’Ascenzi, Anselmi, Adami and Pelliccia10,Reference McClean, Riding and Ardern11
The aim of this study was to evaluate the prevalence of T wave inversions in a population of young competitive athletes and determine whether T wave inversions can be associated with the occurrence of cardiomyopathies in the absence of familiarity for cardiomyopathy, symptoms, and other anomalies in electrocardiogram.
Materials and methods
Study design
A prospective cross-sectional study was carried out over 18 months, at Bambino Gesù Children’s Hospital in Rome, Italy. Athletes were enrolled in the study during pre-participation screening for competitive sport performed in our institution. The study conforms to the ethical principles of the Good Clinical Practice, was conducted according to the Helsinki Declaration and its later amendments, and was approved by the Ethics Committee of Bambino Gesù Children’s Hospital (protocol code 2799_OPBG_2022), following the current Italian regulations. Moreover, all subjects and their parents were verbally informed about the aim and the procedures of the study and signed a written informed consent. All participants were assured about the anonymity of data and that the data would have been processed for scientific purposes and in an aggregate manner.
Subjects
Patients were enrolled in the study if they met the following inclusion criteria:
-
8–18 years old
-
≥5 hours per week of competitive sport
-
Asymptomatic
-
Absence of familiarity with cardiomyopathy
-
T wave inversions > 1 mm in two or more leads at baseline electrocardiogram and/or after 3-minute step test effort electrocardiogram
Exclusion criteria were:
-
T wave inversions only in V1–V2 leads
-
History of CHD
-
Known coronary artery anomalies
-
Bronchial asthma diagnosis
-
Children with infectious disease in the previous 2 months
Study protocol
The study population underwent pre-participation evaluation. That included a thorough history taking, physical examination, spirometry, and a 12-lead electrocardiogram both at rest and after a step test (submaximal effort test in which the athlete goes up and down a step for a continuous duration of 3 minutes).
Patients meeting the inclusion criteria underwent further evaluation:
-
Second level: Trans-thoracic echocardiogram, exercise stress test on treadmill or cycle-ergometer (reaching at least 85% of age-predicted maximal heart rate), and 24h Holter electrocardiogram monitoring (including 1-hour training session).
-
Third level: Cardio-MRI and/or Cardio-CT
At the end of this evaluation, a board of expert cardiologists and sport physicians decided about the eligibility for competitive sport.
Statistical analysis
Data analysis was performed using the SPSS ver.21 statistical programme International Business Machine Corporation. The normal distribution of continuous variables was verified by Kolmogorov-Smirnov test. For continuous variables, mean ± standard deviation was reported, while categorical data were expressed as absolute numbers and percentages. Mean differences were investigated by analysis of variance in case the normal distribution of the data occurred, or through Wilcoxon Signed Rank test for data not normally distributed. The results were considered statistically significant with p < 0.05
Results
During the recruitment period, 581 consecutive athletes were screened for competitive sport eligibility. All subjects came from the European geographical area. Fifty-three patients met the inclusion criteria (9,1%) and were selected for this study. The mean age was 15.3 ± 2.75 years old and 79.2% of them were male. The majority of the study population was normal weight (mean body mass index 20,7 ± 4,2 kg/m2).
Pre-participation screening
Thirty-nine athletes showed T wave inversions at baseline electrocardiogram. T wave inversions persisted during the step test in 16 cases and disappeared or regressed (T waves looked less negative) in 23. Fourteen athletes had T wave inversions after 3-minute step test.
All patients showed a normal corrected QT interval both at rest and during the recovery stage of exercise. T wave inversion localization is reported in Table 1.
Table 1. TWIs localization on ECG

TWIs = T wave inversion; ECG = electrocardiogram; VR = ventricular repolarization.
Second-level evaluation
All 53 subjects underwent second-level evaluation.
T wave inversions disappeared during maximal exercise test in 23 cases, persisted in 15, and worsened in the remaining 15 (T waves became deeply negative).
Twenty-four-hour Holter electrocardiogram monitoring did not show significant arrhythmias.
Thirty-two athletes showed a normal trans-thoracic echocardiogram. Twenty-one athletes showed structural abnormalities: bicuspid aorta (1), atrial septal defect (1), ventricular septal defect (1), hypertrophied localised area of left ventricle (16), and enlarged left atrium and/or left ventricle (3).
Fourty-seven athletes (88,7%) underwent the third-level evaluation and the remaining six were eligible for competitive sport.
Third-level evaluation
Thirty-nine athletes underwent cardio-MRI, 21 athletes underwent cardio-CT, and 11 underwent both instrumental tests.
Cardiac-Magnetic Resonance Imaging showed myocarditis in two cases (based on Lake Louise Criteria 2018), Reference Ferreira, Schulz-Menger and Holmvang12 a suspected cardiomyopathy in seven (moderate-severe ventricular dilatation with ventricular systolic function reduction, increase in mid-apical lateral trabeculation and associated parietal thinning, and myocardial mass at the upper limits with thickening of the ventricular walls), mild anomalies in 18 (mild harmonic ventricular dilatation with preserved ventricular systolic function, mild apical hypertrabeculation of the left ventricle, and dispersed appearance of the papillary muscles insertion), and it was normal in the remaining 12 athletes.
Cardio-CT showed anomalies of right coronary arteries origin in two, a left anterior descending coronary myocardial bridge in five, and normal origin and course of coronary arteries in the remaining 14 athletes.
Finally, among the 47 subjects who underwent the third-level evaluation, cardiac pathologies were excluded in 24 athletes who were readmitted to competitive activity with regular follow-up. The other athletes were temporarily excluded from sports activities due to suspected cardiac anomalies related to the T wave inversions.
After third-level exams, a total of 23 athletes were referred to cardiomyopathy specialists because they showed suspected anomalies at Cardiac-Magnetic Resonance Imaging or mild anomalies of non-univocal interpretation. At the end of the specialist evaluation, based on the second and third-level exams, cardiomyopathy was excluded in eight athletes, eight were diagnosed with either dilated or hypertrophic cardiomyopathy, and in seven athletes, cardiomyopathy diagnosis remained dubious (Fig. 1).

Figure 1. Flow-chart to identify cardiomyopathies.
We observed that the greater the abnormalities at the cardio-MRI, the greater the possibility that they represented a sign of cardiomyopathy (see Table 2).
Table 2. Outcomes after third-level evaluation (23 athletes)
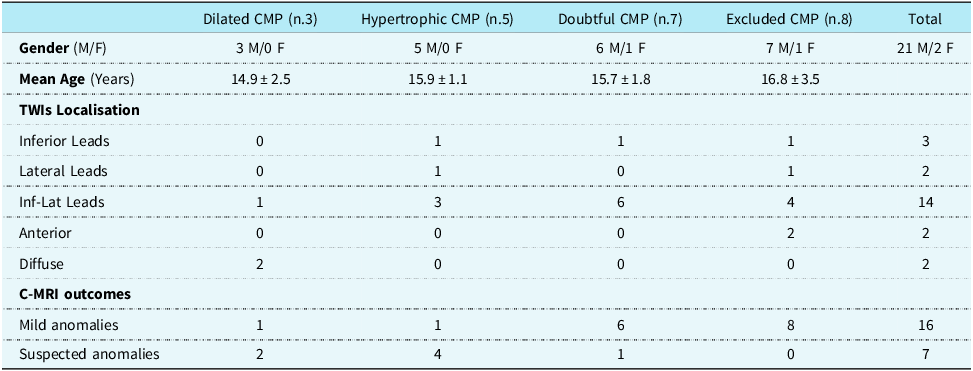
M = male; F = female; CMP = cardiomyopathies; C-MRI = Cardio-MRI; Inf-Lat = Inferior-lateral.
Cardiomyopathy cases have been definitively suspended from competitive sport activity. The other athletes continued their sporting activity albeit with close follow-up over time. Among the cases of cardiomyopathy, three dilated Cardiomyopathy and five hypertrophic Cardiomyopathy were reported. In seven of eight cases, echocardiogram showed in advance signs of pathology.
We analysed the localization of T wave inversions of athletes evaluated by cardiomyopathy specialists. The T wave inversions in cardiomyopathy or suspicious cases were both located in the inferior-lateral leads.
Of the 53 subjects enrolled in the study, 17 (32.1%) had an identified cause of T wave inversions and needed to suspend competitive activity (two due to myocarditis; two because of anomalous origin of the coronary arteries; five because of myocardial bridge and eight with cardiomyopathies). So, in 32,1% of cases, we have identified the cause of T wave inversions (see Fig. 2). In 36 athletes, we were not able to identify a clear cause for the T wave inversions, and they were therefore allowed to continue competitive activities with appropriate follow-up with different timing: 6 months in subjects with mild anomalies at echocardiogram and/or Cardiac-Magnetic Resonance Imaging, and 12 months in those athletes who showed a normal echocardiogram and/or Cardiac-Magnetic Resonance Imaging.

Figure 2. Causes of suspension from competitive activity in athletes with T wave inversions.
Discussion
A prospective cross-sectional study was conducted in a group of 581 very young competitive athletes who showed T wave inversions during pre-participation screening. These athletes were asymptomatic and were always found eligible at previous evaluations. A 53-subject sample was investigated through second and third-level instrumental exams with the aim of excluding an early onset of cardiomyopathy, which might contraindicate the practice of competitive sport.
Our results showed T wave inversions in 53 athletes equal to 9,1% of the study population similar to current literature. Reference Malhotra, Dhutia and Gati2–Reference Migliore, Zorzi and Michieli4,Reference McClean, Riding and Ardern11 Eight athletes presenting with T wave inversions were diagnosed with an early onset of cardiomyopathy.
We also noticed that T wave inversions were mainly located in the infero-lateral leads (58,5%). Other distributions included: inferior leads (11,3%), lateral leads (7,5%), anterior leads (11,3%), or diffuse (11,3%). These findings differ from what has been described in current literature, Reference Malhotra, Dhutia and Gati2,Reference Migliore, Zorzi and Michieli4,Reference D’Ascenzi, Anselmi, Adami and Pelliccia10 likely due to our decision to exclude from the instrumental investigations those athletes who showed T wave inversions in V1–V2 leads only. Previous studies Reference D’Ascenzi, Anselmi and Berti5,Reference D’Ascenzi, Anselmi, Adami and Pelliccia10,Reference Anselmi, Cangiano and Fusi13 have infact shown that these alterations are often found in very young athletes and they rarely hide an underlying cardiomyopathy. We also included those subjects in which the “anterior” localization was extended up to V1–V4. Most of the T wave inversions (73,6%) were evident at baseline electrocardiogram; however, a small percentage of cases were elicited by physical effort (step test). This finding suggests how a simple tool like the step test can be useful in detecting additional cases of T wave inversions.
The majority of athletes with T wave inversions at pre-participation screening showed normal echocardiogram and/or cardio-MRI. We suspended from competitive activity all those athletes in whom we found a cause of T wave inversions that could represent a risk factor for sudden cardiac death. In particular, we suspended two athletes with anomalous origin of the coronary arteries (right coronary artery originating above the commissural junction between the left and right aortic sinuses, with a slit-like ostium and intramural course and hypoplasia of the first section); five athletes showed a left anterior descending artery myocardial bridge (>1 cm in length and ≥ 3 mm in depth). None of these athletes required surgery but they were excluded from competitive sports practice in accordance with the Italian guidelines for sport eligibility. 14 Two athletes showed signs of myocarditis, so they were temporarily suspended from competitive sport and their eligibility will be reviewed over time, based on recovery from the acute inflammatory phenomenon and the presence of any sequelae of disease. Lastly, eight athletes showed an early onset of cardiomyopathy, and the rest of the study population was admitted to competitive sport with a 6–12 months follow-up.
None of the athletes with T wave inversions showed significant arrhythmic events on 24h Ambulatory electrocardiogram. Malignant arrhythmias were not observed even during step tests or ergometric tests.
At the end of evaluations, eight athletes (15% of subjects with T wave inversions) were suspended from competitive sport due to cardiomyopathy. This percentage seems high compared to what is currently reported in literature; Reference Lee, Hsu and Kantor15,Reference Lipshultz, Law and Asante-Korang16 however, these results are in line with what was demonstrated by Sheik Reference Sheikh, Papadakis and Wilson17 who observed cardiomyopathy in 21% of young athletes with T wave inversions. The study population in that case was not as young as ours, showing a mean age of 25.1 ± 7.1 years old. The high percentage of suspicious cases we found is probably due to the easy access to advanced exams and assessments in our high-level centre, which facilitates us to reach early diagnoses before the disease fully develops.
The Italian pre-participation screening is confirmed as a simple, inexpensive, and valid tool for the early detection of cardiomyopathy. It has allowed identification of subjects who could be at risk of sport-induced sudden cardiac death. Our results reiterate, as sustained by previous studies, that electrocardiogram anticipates the diagnosis of cardiomyopathy before it fully manifests on cardiovascular image tools. Reference Calò, Martino and Tranchita18,Reference Silvetti, Lanza and Romeo19
Second-level diagnostic investigations were suggested for cases with evident electrocardiogram abnormalities (T wave inversions) while third-level diagnostic investigations were reserved for an even smaller number of subjects who showed persistence or worsening of T wave inversions during effort or ST segment alterations on electrocardiogram that led to the suspicion of an ischaemic cause of T wave inversions. By following this pathway, it is possible to optimise resources and focus our attention on those few cases that warrant further investigations in order to rule out risk factors for sudden cardiac death. Our management of athletes with T wave inversions is completely comparable to what Wilson suggested in his work. Reference Wilson, Sharma and Carré3
Clinical implications derived from our study are that apparently healthy athletes who showed T wave inversions during pre-participation evaluation for competitive sport need further investigation before they are deemed eligible. Particular attention must be paid to those athletes who show T wave inversions in the infero-lateral leads and significant abnormalities on the echocardiogram. They warrant a third-level diagnostic investigation and a multidisciplinary evaluation. The question is whether or not to permit competitive activity in athletes with T wave inversions. Our opinion is that we must first exclude any risk factors for sudden cardiac death and then it is possible to give eligibility with close follow-up. It is important to re-evaluate athletes with T wave inversions and structurally normal hearts over time, to verify their conditions remain stable and safe. If any change occurs, then it would be appropriate to modify the decision on their eligibility in order to prevent adverse events.
The strength of this study is that, for the first time, a network of specialists was created for the diagnosis, follow-up, and management of these patients with T wave inversions in order to continue practicing sports in total safety. Further long-term follow-up is needed to evaluate over time any disease progression or new diagnoses in those patients who currently only show T wave inversions on the electrocardiogram. Longitudinal studies could help us make the right decisions in regard to the eligibility of these athletes for competitive sport.
Study limitation is that it involved only White athletes and we were therefore not able to make a comparison with Black athletes who have electrocardiographic variants of ventricular repolarization. Reference Davis, Semsarian and Orchard20 It would be very useful in the future to be able to compare these two populations and understand whether they show overlapping electrocardiographic patterns in the initial forms of cardiomyopathies. A larger study population is needed to confirm the prevalence of T wave inversions in competitive younger athletes and how often these are the first signs of a cardiomyopathy in asymptomatic subjects.
Conclusion
In rare cases, T wave inversions can represent early onset of cardiomyopathy. Pre-participation screening represents an opportunity to highlight early-stage cardiomyopathies. Prevalence of T wave inversions in our population of young competitive athletes was 9,1%. Our study highlights that the T wave inversions in inferior-lateral leads need to be explored in greater detail in young athletes. In particular, we observed that 15% of athletes who showed T wave inversions presented cardiomyopathies. These athletes were suspended from competitive sport in order to reduce the risk of sudden cardiac death. The remaining athletes with T wave inversions and apparently healthy hearts will be subjected to close instrumental follow-up to see if their conditions will change over time. The need has emerged to create a network of specialists who can properly manage patients with T wave inversions over time, allowing them to practice physical activity safely and carrying out the appropriate re-evaluation at the right time. Future studies should examine larger and heterogeneous population of athletes with T wave inversions with a longer follow-up to better assess outcomes.
Acknowledgements
None.
Financial support
This work was supported by the Italian Ministry of Health with Current Research national funds for the three-year period 2022–2024 (Directorial Decree of December 22, 2022) and by Bambino Gesù Children’s Hospital Foundation 5x1000 Funds for health and scientific research n. 20225_MULTI_CAFI1.9 for the two-year period 2022–2023.
Competing interests
None.
Ethical standard
The authors declare that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by Ethics Committee of Bambino Gesù Children’s Hospital (protocol code 2799_OPBG_2022).







