1. Introduction
Healthcare systems all over the world are facing many challenges because of changes in demand (ageing population, increased prevalence of chronic diseases and emergence of new, often treatment-resistant pathogens) as well as concerns with the adequacy and safety of the care provided and its equal access for all. These challenges are compounded by the rising cost of new medical innovations and pressures to contain the expansion of healthcare budgets.
Some of these problems require new technologies, new treatment strategies or new therapeutics. However, many of these challenges also require rethinking the way healthcare is delivered. There is great potential for design to contribute to this endeavour (Clarkson Reference Clarkson2018). In general, the contribution of design in health has tended to focus on medical products and devices, or medical IT. Its contribution towards designing healthcare services is relatively young, witnessing the small number of papers in key journals like Design Studies, the Journal of Engineering Design or Research in Engineering Design.
We make the argument that when applying design to healthcare services, designers may wish to learn from the experience of design’s sister discipline, operational research (OR), which has a longer history of trying to improve healthcare organisation and services. Since its inception just before World War II, OR has developed methods and approaches aimed at improving the performance of complex systems and processes (which health services certainly are), often relying on quantitative modelling, but including also more qualitative but still disciplined methods that facilitate stakeholder engagement and participation. The desirability of better integration between OR and design has been noted over the years (Holzman Reference Holzman1979; Levary Reference Levary1994; O’Keefe Reference O’Keefe1995, Reference O’Keefe2014; Royston Reference Royston2013). What remains to be seen is how these complementarities can best be operationalised in a healthcare context. In what follows, we propose a partnership and consider how the two disciplines might complement each other in contributing to (re)designing healthcare services. First, we provide some background about the involvement of OR and design in healthcare. We then describe some of the similarities and complementarities of design and OR as we begin to set out how they might join forces in tackling challenges in healthcare.
2. Design and healthcare
In this paper, we use the term design in the broadest sense, as envisioned by the Design Science Journal (Papalambros et al. Reference Papalambros, Ahmed-Kristensen, Badke-Schaub, Bauerly, Boujut, Cagan, Cantamessa, Chakrabarti, Chen, Chen, Clarkson, Duffy, Goel, Hanna, Jin, Kim, Knight, Lindemann, Louviere, McMahon, Nagai, Reich, Seifert, Smith, Tseng, Vermaas, Wood, Yannou and Gero2015). This, therefore, covers aspects of design from cognitive design through to service design and parts of human factors/ergonomics and systems engineering. For this reason, it is impossible to be exhaustive in describing design and healthcare in this short section. It is also important to point out that industrial designers and design engineers are not the only professional designers (Simon Reference Simon1996): arguably, all professionals design (although some may be more conscious of this fact than others). At the heart of design is the desire to realise functional products and systems and the belief that ‘systems [or products] that work do not just happen – they have to be planned, designed and built’ (Elliott & Deasley Reference Elliott and Deasley2007).
Design researchers have tackled issues in health services, for example, to better integrate users in product development (Weightman et al. Reference Weightman, Preston, Holt, Allsop, Levesley and Bhakta2010), to reduce errors and increase patient safety (Roesler et al. Reference Roesler, Grigg, Martin, Ross, Feil, Rampersad, Haberkern and Martin2019) or to use design as a problem-solving strategy to effectively manage indeterminate problem situations (Van Stralen Reference van Stralen2008). No comprehensive review of the application of design in healthcare has been published to date, but the literature shows that a range of design methods have been applied to various areas of healthcare (Box 1).
Box 1. Examples of applications of design approaches in healthcare.
Application of specific design methods in healthcare:
-
(i) Design thinking (Altman, Huang, & Breland Reference Altman, Huang and Breland2018; Oliveira, Zancul, & Fleury Reference Oliveira, Zancul and Fleury2021; Ku & Lupton Reference Ku and Lupton2022)
-
(ii) Systems approaches (Clarkson et al. Reference Clarkson, Bogle, Dean, Tooley, Trewby, Vaughan and Shelton2017; Komashie et al. Reference Komashie, Ward, Bashford, Dickerson, Kaya, Liu, Kuhn, Günay, Kohler, Boddy, O’Kelly, Masters, Dean, Meads and Clarkson2021)
-
(iii) Service design (Pfannstiel & Rasche Reference Pfannstiel and Rasche2019)
-
(iv) Systems engineering (Rouse & Cortese Reference Rouse and Cortese2010; Griffin et al. Reference Griffin, Nembhard, DeFlitch, Bastian, Kang and Muñoz2016)
-
(v) Experience-based co-design (Donetto et al. Reference Donetto, Pierri, Tsianakas and Robert2015; Green et al. Reference Green, Bonner, Teleni, Bradford, Purtell, Douglas, Yates, MacAndrew, Dao and Chan2020)
-
(vi) Human factors and ergonomics (Catchpole Reference Catchpole2013)
-
(vii) Human-centred design (Melles, Albayrak, & Goossens Reference Melles, Albayrak and Goossens2020)
-
(viii) Healthcare environment design (Ulrich et al. Reference Ulrich, Zimring, Zhu, DuBose, Seo and Choi2008; Cama Reference Cama2009)
Applications of design to specific areas of healthcare:
-
(i) P4 (Predictive, Preventive, Personalised and Participative) healthcare (Patou et al. Reference Patou, Ciccone, Thorpe and Maier2020)
-
(ii) Medical technology innovation (Zenios et al. Reference Zenios, Makower, Yock, Denend, Brinton, Kumar and Krummel2010)
-
(iii) Global health (Bazzano et al. Reference Bazzano, Martin, Hicks, Faughnan and Murphy2017)
-
(iv) Medical education (McLaughlin et al. Reference McLaughlin, Wolcott, Hubbard, Umstead and Rider2019)
-
(v) Medical simulation (Petrosoniak et al. Reference Petrosoniak, Hicks, Barratt, Gascon, Kokoski, Campbell, White, Bandiera, Lum-Kwong, Nemoy and Brydges2020)
-
(vi) Patient safety (Xie & Carayon Reference Xie and Carayon2015)
-
(vii) Person-centred care (Bhattacharyya et al. Reference Bhattacharyya, Blumenthal, Stoddard, Mansell, Mossman and Schneider2019)
-
(viii) Patient work (Werner et al. Reference Werner, Ponnala, Doutcheva and Holden2020)
However, design in healthcare remains a relatively recent academic discipline, and a simple bibliometric analysis reveals that it has only a limited presence in healthcare (Table 1). Between 2001 and 2020, less than 2.1% of articles published in key design journals focused on healthcare. In absolute terms, this amounted to less than 150 articles. In practice, national institutions have recommended a better use of engineering and design skills in solving healthcare problems (Reid et al. Reference Reid, Compton, Grossman and Fanjiang2005; Clarkson et al. Reference Clarkson, Bogle, Dean, Tooley, Trewby, Vaughan and Shelton2017). Yet, health services have repeatedly been found to be out-of-step with contemporary design thinking. Key characteristics of the design mindset, for example, user-centredness, openness in problem exploration, learning through iteration, creativity in solution generation, robust testing or risk assessment (Dieter & Schmidt Reference Dieter and Schmidt2013; Clarkson Reference Clarkson2018), are often missing in practical service development projects (Clarkson et al. Reference Clarkson, Buckle, Coleman, Stubbs, Ward, Jarrett, Lane and Bound2004; Jun, Morrison, & Clarkson Reference Jun, Morrison and Clarkson2014).
Table 1. Articles published on healthcare in OR and design journals between 2001 and 2020

Note: Search run on 7 February 2022 on ISI Web of Knowledge. Sample of design journals: Journal of Engineering Design, Research in Engineering Design, International Journal of Design, Design Studies, Design Issues, Design Science, Artificial Intelligence for Engineering Design, Analysis and Manufacturing (AI EDAM), ASME Journal of Mechanical Design. Sample of OR journals: European Journal of Operational Research, Journal of the Operational Research Society, Management Science, Operations Research, Omega, Computers & OR, International Transactions in Operational Research, Annals of Operations Research, IISE Transactions. ISI Web of Knowledge’s ‘topic’ field combines title, abstract and keywords.
The amount and share of published healthcare-related research are substantially larger in OR than in design research (Table 1). The first OR papers in healthcare date back to the 1950s (Bailey Reference Bailey1952), and the literature has developed steadily since then (Figure 1). This suggests that the findings, expertise and experience accumulated in the OR community in relation to healthcare are greater than in design.
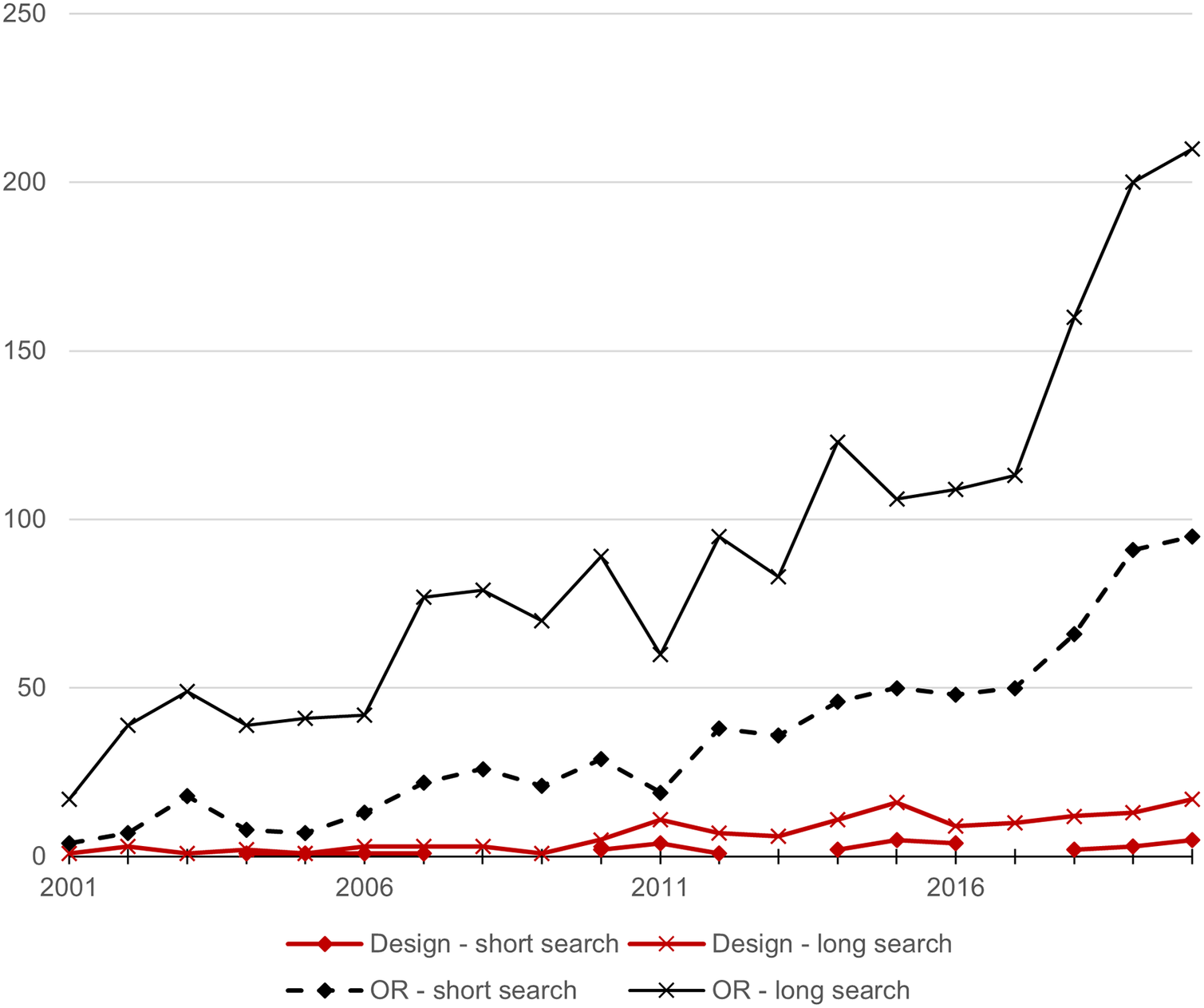
Figure 1. Number of healthcare-related publications per year, in design and OR, in the same selection of journals as Table 1. Short search: ‘healthcare or health care’ in topic. Long search: ‘health or healthcare or health care or medic* or pharma* or nurs* or hospital or doctor or physician or patient’ in topic.
3. OR and healthcare
The Operational Research Society describes OR as ‘a scientific approach to the solution of problems in the management of complex systems that enables decision makers to make better decisions’ [The OR Society (n.d.)]. A complementary description might be that OR is a discipline focused on supporting people to organise and manage processes and services more effectively and efficiently so as to improve system performance – OR, like medicine or engineering, is an improvement science. Traditional applications of OR draw on quantitative methods such as optimisation, queueing models and simulation (Winston Reference Winston1993). A typical example would be seeking to improve the efficiency and effectiveness of an organisation by optimising the use of a given amount of resources invested (time, money, facilities, staff).
However, many organisational challenges do not lend themselves to reductionist modelling approaches as they are particularly complex, unstructured or have multiple and potentially contested versions of ‘what better looks like’. To assist in such cases, so-called ‘soft’ OR has been developed. This draws largely on qualitative approaches such as soft systems methodology, cognitive mapping, and strategic options and decision analysis and can be used to help improve collective understanding of the aims of a system, to ask questions of it and to facilitate agreement on how to proceed (Mingers & Rosenhead Reference Mingers, Rosenhead, Rosenhead and Mingers2001).
OR has a long history of working on healthcare issues, with an acceleration of research and applications in this field over recent decades (Pitt et al. Reference Pitt, Monks, Crowe and Vasilakis2016). OR has been applied at different decision levels (strategic planning, tactical planning, advance operational decision-making and real-time reactive operational decision-making) and in a variety of services: ambulatory care services; emergency care services; surgical care services; inpatient care services; home care services and residential care services (Hulshof et al. Reference Hulshof, Kortbeek, Boucherie, Hans and Bakker2012). Multiple literature reviews have summarised how different OR techniques have been applied in healthcare and/or summarise OR applications published in specific areas of healthcare (Box 2).
Box 2. Examples of applications of OR in healthcare.
Applications of specific OR techniques in healthcare:
-
(i) Modelling and simulation (Wilson Reference Wilson1981; Fone et al. Reference Fone, Hollinghurst, Temple, Round, Lester, Weightman, Roberts, Coyle, Bevan and Palmer2003; Brailsford et al. Reference Brailsford, Harper, Patel and Pitt2009; Jahangirian et al. Reference Jahangirian, Naseer, Stergioulas, Young, Eldabi, Brailsford, Patel and Harper2012; van Lent, VanBerkel, & van Harten Reference van Lent, VanBerkel and van Harten2012; Mohiuddin et al. Reference Mohiuddin, Busby, Savović, Richards, Northstone, Hollingworth, Donovan and Vasilakis2017; Long & Meadows Reference Long and Meadows2018)
-
(ii) Multi-criteria decision analysis (Marsh et al. Reference Marsh, Lanitis, Neasham, Orfanos and Caro2014)
-
(iii) Scheduling (Samudra et al. Reference Samudra, Van Riet, Demeulemeester, Cardoen, Vansteenkiste and Rademakers2016; Marynissen & Demeulemeester Reference Marynissen and Demeulemeester2019)
-
(iv) Optimisation (Ahmadi-Javid, Jalali, & Klassen Reference Ahmadi-Javid, Jalali and Klassen2017)
-
(v) Soft systems methodology (Augustsson, Churruca, & Braithwaite Reference Augustsson, Churruca and Braithwaite2020)
-
(vi) Behavioural OR (Kunc, Harper, & Katsikopoulos Reference Kunc, Harper and Katsikopoulos2018)
Applications of OR to specific areas of healthcare:
-
(i) Emergency departments (Mohiuddin et al. Reference Mohiuddin, Busby, Savović, Richards, Northstone, Hollingworth, Donovan and Vasilakis2017)
-
(ii) Outpatient clinics (Lamé, Jouini, & Stal-Le Cardinal Reference Lamé, Jouini and Stal-Le Cardinal2016; Ahmadi-Javid et al. Reference Ahmadi-Javid, Jalali and Klassen2017)
-
(iii) Operating rooms (Cardoen, Demeulemeester, & Beliën Reference Cardoen, Demeulemeester and Beliën2010; Samudra et al. Reference Samudra, Van Riet, Demeulemeester, Cardoen, Vansteenkiste and Rademakers2016)
-
(iv) Staff rostering and scheduling (Ernst et al. Reference Ernst, Jiang, Krishnamoorthy and Sier2004; Van den Bergh et al. Reference Van den Bergh, Beliën, De Bruecker, Demeulemeester and De Boeck2013)
-
(v) Community care (Palmer, Fulop, & Utley Reference Palmer, Fulop and Utley2018)
-
(vi) Mental health (Long & Meadows Reference Long and Meadows2018)
-
(vii) Cancer care (Saville, Smith, & Bijak Reference Saville, Smith and Bijak2019)
-
(viii) Home healthcare (Cissé et al. Reference Cissé, Yalçındağ, Kergosien, Şahin, Lenté and Matta2017; Fikar & Hirsch Reference Fikar and Hirsch2017; Grieco, Utley, & Crowe Reference Grieco, Utley and Crowe2020)
-
(ix) Global health (Royston Reference Royston2011; Bradley et al. Reference Bradley, Jung, Tandon-Verma, Khoury, Chan and Cheng2017)
In terms of methods, a comprehensive review of the healthcare OR literature by Brailsford et al. (Reference Brailsford, Harper, Patel and Pitt2009) shows that the majority of publications in healthcare OR have been found to employ statistical analysis (e.g., regression analysis), statistical modelling (e.g., Markov models, structural equation modelling), simulation (discrete event, system dynamics, Monte Carlo) or qualitative modelling (e.g., process mapping, cognitive modelling). They also find that the rate of healthcare OR publications is steadily increasing, with a particularly prominent rise in simulation and qualitative (soft) methods.
When it comes to areas of application, Brailsford & Vissers (Reference Brailsford and Vissers2011) review papers presented at the meetings of the Operational Research Applied to Health Services European Working Group from 1975 to 2009 and categorise them according to the nine stages of the product life cycle, that is, stages of developing and managing a service. By far the most common categories for OR applications were ‘managing the performance of service delivery’ (39% of papers), ‘developing programs and plans for using resources’ (24%) and ‘evaluating the performance of service delivery’ (18%). Hardly any papers were categorised as ‘identifying customer requirements’ or ‘developing a new service’, which are both key areas where one might expect design to make major contributions.
Increasing attention is also paid to the best ways of engaging and working with healthcare organisations and stakeholders in healthcare OR projects (Brailsford et al. Reference Brailsford, Bolt, Bucci, Chaussalet, Connell, Harper, Klein, Pitt and Taylor2013; Pearson et al. Reference Pearson, Monks, Gibson, Allen, Komashie, Fordyce, Harris-Golesworthy, Pitt, Brailsford and Stein2013). However, there are still very few published examples of successful implementations of OR (Brailsford et al. Reference Brailsford, Harper, Patel and Pitt2009; Brailsford & Vissers Reference Brailsford and Vissers2011), and few published empirical evaluations of the impact of OR on health services (Lamé, Crowe, & Barclay Reference Lamé, Crowe and Barclay2022). This shows that despite a steady growth in academic healthcare OR over a number of years, its overall influence over healthcare in practice remains uncertain. There is more indication of influence where teams of OR analysts have been embedded in healthcare organisations (e.g., Royston et al. Reference Royston, Dost, Townshend and Turner1999; Royston et al. Reference Royston, Halsall, Halsall and Braithwaite2003; Marshall et al. Reference Marshall, Pagel, French, Utley, Allwood, Fulop, Pope, Banks and Goldmann2014; Crowe et al. Reference Crowe, Grieco, Vindrola-Padros, Elkhodair, Walton, Fulop and Utley2019; Harper Reference Harper2020), but there is still a long way to go, and we suggest that combining design’s strengths with OR’s expertise and experience in healthcare could be particularly fruitful.
4. Joining forces
Although they have grown separately, OR and design have much in common. ‘Everyone designs who devises courses of action aimed at changing existing situations into preferred ones’, wrote Herbert Simon, a leading figure in both OR and design (Simon Reference Simon1996). Churchman, one of the early pioneers of OR, defined OR as ‘the securing of improvement in social systems by means of scientific method’ (Churchman Reference Churchman1970). One of the other key figures in the postwar development of OR, Russel Ackoff, argued (albeit without much success) that the discipline needed to focus much more on design issues and later wrote a book about design for management (Ackoff, Magidson, & Addison Reference Ackoff, Magidson and Addison2006). With these definitions, design and OR belong to a broader ensemble of design disciplines that aim to improve the world rather than explain it, much like medicine or architecture in their respective domains (Royston & Komashie Reference Royston and Komashie2016).
Previous publications have discussed how OR and design could complement each other. In the OR community, in a brief letter to the editor, Holzman (Reference Holzman1979) acknowledged the rift between engineering design and OR and highlighted common denominators (the formulation of objectives, a systems perspective, the choice between alternatives and optimisation) between them. A decade later, Levary (Reference Levary1988, Reference Levary1994) reviewed the potential for OR contributions to engineering, mentioning computer communications engineering, structural engineering or chemical engineering. O’Keefe (Reference O’Keefe1995) discussed how systems design could improve OR’s impact by focusing on designing better systems rather than improving existing ones. In a series of articles, Evans (Reference Evans1991, Reference Evans1992, Reference Evans1993, Reference Evans1997a,Reference Evans b) argued for the key role of creativity in OR, soon followed by Keys (Reference Keys2000) with a framework for examining the role of creativity and design in OR practice. Fifteen years later, O’Keefe (Reference O’Keefe2014) extended his argument by proposing a design science approach to OR projects, in order to better embed OR solutions into organisational and information systems. Around the same time, Royston (Reference Royston2013) argued that OR was often involved in designing systems, for example, through scenario analysis or simulation, as well as in the complementary task of assisting decisions. This, in his view, meant that OR needed to pay better attention to design thinking.
In parallel, in the design research community, Cross (Reference Cross2001) noted how OR impacted the origins of design methods. Indeed, design engineering courses included OR modules (Fenves & Grossmann Reference Fenves and Grossmann1992), and optimal design developed as a strong stream of engineering design research (Cagan, Grossmann, & Hooker Reference Cagan, Grossmann and Hooker1997; Papalambros & Wilde Reference Papalambros and Wilde2000). Examples of combining human factors engineering and OR have also appeared (Ryan et al. Reference Ryan, Qu, Schock and Parry2011) but have remained limited. In the systems engineering community, some authors go as far as considering OR as a subset of the methods available to systems engineers (Rouse & Cortese Reference Rouse and Cortese2010).
Many complementarities between OR and design could be harnessed in responding to the numerous complex challenges facing modern healthcare delivery systems, but practical steps are needed (Box 3).
Box 3: Complementarities between OR and design, and the steps needed to capitalise on them in the context of improving healthcare
Complementarities:
-
(i) Technology (a key focus of design) and organisation (a key focus of OR) are increasingly entangled and convergent, requiring a holistic approach that considers them together
-
(ii) Design’s distinct strengths include a wide-ranging and creative search for potential solutions and a pragmatic concern for workable solutions through frequent prototyping
-
(iii) OR’s unique contribution lies in its unparalleled developments for quantitative and qualitative analysis and modelling for improving organisational decision-making and system performance
-
(iv) OR and design have developed different approaches to stakeholder engagement, which could benefit from cross-learning
-
(v) OR and design share a common challenge in evidencing their impact in healthcare
-
(vi) OR and design could both learn from other research communities who have successfully engaged with healthcare systems
Steps needed to bring design and OR together to improve healthcare:
-
(i) Strategic reflection on how to collaborate better, with joint initiatives between learned societies and professional bodies to launch common projects
-
(ii) Promoting the emergence of healthcare specialists in design research and practice, who are devoted to the application and development of design in this sector
-
(iii) Identifying common (grand) challenges in health that OR and design could tackle together
-
(iv) Breaking down perceived differences and preconceptions about the disciplines
-
(v) Training cross-disciplinary researchers and practitioners, apt in both OR and design methods
-
(vi) Learning from the experience of other disciplines that have collaborated effectively across boundaries, such as health economics, social sciences or human factors and ergonomics
-
(vii) Generating empirical evidence for the impact of OR and design in healthcare
4.1. Complementarities
Because of a shared ethos of improving the world around us, methods and techniques are both a major research output and a core element of practice in OR and design (Ackoff Reference Ackoff1956; Gericke et al. Reference Gericke, Eckert, Campean, Clarkson, Flening, Isaksson, Kipouros, Kokkolaras, Köhler, Panarotto and Wilmsen2020). By providing practitioners with methods, tools and techniques, OR and design both seek to achieve improvement – but traditionally on different objects and through different routes. OR works at supporting better organisational decision-making and performance, while design aims at improving design processes and products or technologies.
However, these domains are not independent. Technology and organisation both have a key role to play in the future sustainability of healthcare, and they are intertwined: changes in technology often demand changes in the organisation of processes and services, and conversely, organisational changes could often benefit from technological innovations. For instance, to make the most of developments in medical technologies (including data-driven artificial intelligence) requires a refined understanding of human behaviour with technology and product-service development (both of which design has a long history of dealing with), the implications for demand and workforce planning (a core expertise in OR) and a robust model of value flows throughout the service (where both design and OR have elements to contribute).
More generally, it can be argued that design takes a more holistic approach to solving problems than OR, which often focuses on improving the efficiency of a particular process or aspect of a system. That said, problem structuring methods in OR support a wider system view of a problematic situation (Ackermann Reference Ackermann2012). These ‘soft’ methods also help operational researchers to incorporate the views of different stakeholders, but nonetheless much could be learnt in this regard from the more explicit detailing of user requirements that is standard practice in design. Similarly, greater attention could be given in OR to the more explicit, traceable and systematic process for making decisions that design adopts, for example, about priorities between requirements and solution characteristics.
Another strength of design that complements OR is in the way it tackles risk analysis. While ‘what does good, or better, look like?’ and ‘what could go wrong?’ (Clarkson Reference Clarkson2018) are important aspects in both disciplines, design covers so-called ‘human factors’ (Karsh et al. Reference Karsh, Holden, Alper and Or2006; Mumma et al. Reference Mumma, Durso, Ferguson, Gipson, Casanova, Erukunuakpor, Kraft, Walsh, Zimring, DuBose and Jacob2018) which tend to be overlooked in OR [despite recent but growing interest in Behavioural OR (Kunc, Malpass, & White Reference Kunc, Malpass and White2016; Kunc et al. Reference Kunc, Harper and Katsikopoulos2018)], while OR tends to focus on quantitative risk modelling.
Although both disciplines have a background of engaging with stakeholders in order to elicit their needs and collaborate towards solutions, the methods differ. OR has developed a tradition of model-supported participative workshops. In addition to workshops, design has adopted a broader range of methods, for example, design ethnography (Hughes et al. Reference Hughes, King, Rodden and Andersen1994) and living labs. These methods have evolved and been refined in line with the objectives and interests of each discipline. Their combination could enrich interactions with stakeholders.
Related to this, design could offer rich insights to OR practitioners in relation to prototyping. While OR modelling is iterative and models typically progress through several stages in collaboration with users, there is rarely the early and rapid testing that would generate a wider range of ideas to be trialled and more creative adaptation to meet user needs. Indeed, although design thinking and creativity, key elements of design, also play a role in OR practice, this is often downplayed, naïve or even unconscious (Evans Reference Evans1997a,Reference Evans b; Keys Reference Keys2000; Royston Reference Royston2013, Reference Royston, Kunc, Malpass and White2016), and better links with design could support this key process.
At the same time, OR can support many areas of design with its optimisation and decision-making techniques (Barish Reference Barish1963; Levary Reference Levary1994). OR is well recognised for its numerous approaches to finding quantitative solutions to sometimes fairly complex real-world problems. It also has a rigorous approach to understanding variability or stochasticity and hence can make a good contribution to designing resilient systems. For similar reasons, through its use of models and forecasts it plays a key role in understanding the immediate future in complex chaotic situations such as a pandemic where it may be desired to explore a wide range of scenarios of capacity requirement or disease progression (Currie et al. Reference Currie, Fowler, Kotiadis, Monks, Onggo, Robertson and Tako2020; Kaplan Reference Kaplan2020).
Soft OR could also prove complementary to standard stakeholder engagement in design (which focuses on a good understanding of user needs), because techniques such as Rich Pictures (Checkland & Scholes Reference Checkland and Scholes1990; Crowe et al. Reference Crowe, Brown, Tregay, Wray, Knowles, Ridout and Utley2017) help the OR practitioner to go deeper than expressed needs to understand worldviews, concerns and values that are relevant to the complex situation and not just the system. Through years of engagement with issues in health services, OR has also developed specific insights on how best to engage with its stakeholders (Pearson et al. Reference Pearson, Monks, Gibson, Allen, Komashie, Fordyce, Harris-Golesworthy, Pitt, Brailsford and Stein2013; Jahangirian et al. Reference Jahangirian, Taylor, Eatock, Stergioulas and Taylor2015), which design could learn from.
Here, both disciplines might benefit from the more in-depth qualitative research methods developed in the social sciences such as ethnography, which can help to establish a far richer and contextually nuanced understanding of a socially constructed system and situation. More generally, OR and design could learn from the broader health services research community which has, for example, developed a strong track record in evaluation of interventions in healthcare. In 1993, Pope and Mays (Reference Pope and Mays1993) discussed the integration of qualitative research in health services research. Thirty years later, quantitative methods remain the norm, but qualitative research has made definite progress. Similarly, human factors and ergonomics researchers have long wondered about the best way to make an impact in healthcare and generated useful insights about the need to tailor the discipline to the requirements of healthcare (Catchpole Reference Catchpole2013).
OR and design could also partner with emerging sub-disciplines in health services research that have shown successful integration with other health disciplines. For example, the growing field of ‘improvement science’ in healthcare has made a large impact in healthcare by transferring industrial engineering and quality engineering principles (Berwick Reference Berwick1989). Although OR and design are not absent in this field (Clarkson et al. Reference Clarkson, Bogle, Dean, Tooley, Trewby, Vaughan and Shelton2017, Reference Clarkson, Dean, Ward, Komashie and Bashford2018; Crowe et al. Reference Crowe, Brown, Tregay, Wray, Knowles, Ridout and Utley2017), they still have much to contribute. Another area where OR and design could make a contribution is implementation science, ‘the scientific study of methods to promote the systematic uptake of research findings and other evidence-based practices into routine practice, and, hence, to improve the quality and effectiveness of health services’ (Eccles & Mittman Reference Eccles and Mittman2006). Through modelling and human-centred design of existing and new services, OR and design could help bridge translation gaps between scientific evidence and clinical practice (Cooksey Reference Cooksey2006; Morris, Wooding, & Grant Reference Morris, Wooding and Grant2011).
Finally, design and OR share a common challenge in relating to the evaluation-driven tradition of medical disciplines. Published evaluations of OR and design methods remain very rare (Frey & Dym Reference Frey and Dym2006; Gericke et al. Reference Gericke, Eckert, Campean, Clarkson, Flening, Isaksson, Kipouros, Kokkolaras, Köhler, Panarotto and Wilmsen2020; Lamé et al. Reference Lamé, Crowe and Barclay2022): a recent systematic review and meta-analysis of evaluations of systems approaches to improving healthcare delivery did not find any suitable study to include from either a design or OR journal (Komashie et al. Reference Komashie, Ward, Bashford, Dickerson, Kaya, Liu, Kuhn, Günay, Kohler, Boddy, O’Kelly, Masters, Dean, Meads and Clarkson2021). This attests to the dearth of rigorous evaluation of the impact of our approaches in improving healthcare delivery. Yet, being ‘evidence-based’ is a growing concern and key expectation in healthcare (Lamé Reference Lamé2018). Design and OR could benefit from a shared conversation on how to overcome this challenge and to draw on each other’s strengths.
To summarise the complementarities of design and OR, we draw on Royston’s adaptation of the Johari window to OR (Royston Reference Royston, Kunc, Malpass and White2016). The Johari window was first proposed by Joseph Luft and Harrington Ingham in 1955 to describe how people perceive themselves and how they are in turn perceived by others. Table 2 shows the Johari window adapted to OR and design in healthcare, showing areas that are recognised by one or both disciplines, as well as ‘blind spots’, that is, areas under-recognised by both.
Table 2. ‘Johari window’ of OR and design in healthcare

4.2. Practical steps to bridge the gap
Taking advantage of the complementarities between design and OR in tackling problems in healthcare systems is no straightforward task. The disciplines have grown separately and have formed distinct research communities, with almost no interface. Bringing them together requires broadening the vision of their respective perimeters and roles in improving healthcare (Royston Reference Royston2013). We suggest practical steps to make this happen (Figure 2).

Figure 2. Practical steps to tackling healthcare challenges through OR and design.
Increasing engagement
This move will require strategic thinking on the part of both communities. Effort has begun in this direction, with a number of initiatives to bring together OR and design researchers, such as between the OR Society and Design Society (Royston Reference Royston2014) or through other interdisciplinary encounters (Komashie et al. Reference Komashie, Lamé, Patou, Ciccone, Maier and Clarkson2019; Ciccone et al. Reference Ciccone, Patou, Komashie, Lame, Clarkson and Maier2020). Further engagement between the two research communities is required to build on this early momentum and make things happen. One possible outcome of such engagement could be to identify common grand challenges that could be tackled jointly. The recent creation of a Special Interest Group on Health Systems Design at the Design Society is an encouraging sign and could be a vehicle for identifying common challenges.
Increasing health research in design
To enable greater collaboration, design needs to strengthen its healthcare research stream. OR has a strong sub-community of healthcare specialists, with dedicated conferences and journals. In contrast, design’s involvement remains limited and healthcare is often a supplement to work in other sectors for many design researchers. We argue that the specificities of healthcare and its importance as an industrial sector also justify the emergence of specialists in design.
Training a new cohort of improvers
This last point begs the question of appropriate training. A way to bridge the gap between OR and design in healthcare could be to train graduates in design and OR tools and approaches applied to healthcare, thus promoting the emergence of a cohort of cross-disciplinary healthcare improvement specialists. Currently, ‘quality improvement’ in healthcare is often based on principles derived from industrial engineering and quality management by the Institute for Healthcare Improvement, such as Plan-Do-Study-Act cycles or statistical process control. Yet, this single perspective can be limiting, and improvement specialists could benefit from a broader toolkit, as proposed and studied in the emerging multidisciplinary field of improvement science/research (Marshall, Pronovost, & Dixon-Woods Reference Marshall, Pronovost and Dixon-Woods2013). Embedding these specialists close to practice, in healthcare organisations, would be one way to understand better the effective ways to make an impact through design or OR methods (Marshall et al. Reference Marshall, Pagel, French, Utley, Allwood, Fulop, Pope, Banks and Goldmann2014; Perry et al. Reference Perry, Catchpole, Rivera, Henrickson Parker and Gosbee2021). Healthcare professionals are also increasingly encouraged to train in quality improvement (Worsley, Webb, & Vaux Reference Worsley, Webb and Vaux2016). This training could be an opportunity to expose them to elements of systems analysis, modelling and design based on design and OR principles and concepts.
Combining curricula
OR and design curricula are often separate and even hosted in different schools (mathematics, business and management or computer science for OR, engineering for engineering design, arts or technology for industrial design), but combining them in a training programme seems feasible. Recent interdisciplinary workshops with both design and OR participants (as well as human factors and ergonomics specialists, social scientists and clinicians) revealed that much of the gap between disciplines, including that between OR and design, is often due to preconceptions about other disciplines, miscommunication and perceived differences that do not stand up to careful analysis of what gets done in actual projects (Komashie et al. Reference Komashie, Lamé, Patou, Ciccone, Maier and Clarkson2019). Despite using different vocabulary and mastering different tools, methods and techniques, participants shared a strong common purpose of making a positive impact on the way healthcare is delivered and a sense that the problems warranted collaboration. It quickly emerged that the methods were complementary. A systems-oriented perspective, highlighting the complex interactions between elements of health services, proved to be a fruitful angle to generate common discussions (Komashie et al. Reference Komashie, Lamé, Patou, Ciccone, Maier and Clarkson2019; Ciccone et al. Reference Ciccone, Patou, Komashie, Lame, Clarkson and Maier2020).
Looking beyond OR and design
Finally, it is important to remain conscious that the simple alliance of OR and design is unlikely to transform healthcare on its own. The way issues are defined and presented (Martin et al. Reference Martin, Ozieranski, Leslie and Dixon-Woods2019), leadership or organisational culture are strong factors in the success or failure of improvement projects (Dixon-Woods, McNicol, & Martin Reference Dixon-Woods, McNicol and Martin2012). At an individual level, successful healthcare improvers rely on varied habits of mind, including influencing, communication and resilience (Lucas Reference Lucas2016), which are distinct from the methods, tools and disciplinary frameworks that define design and OR. More generally, innovation requires entrepreneurship as well as good design and science to happen (Luo Reference Luo2015). Therefore, a broader understanding of business, economics and organisations will be required, if OR and design are to affect healthcare delivery. Learning from other disciplines that have engaged with healthcare research (e.g., social sciences, economics) may also help better adapt our approaches to the context of healthcare and complement them, for example, in evaluating the impact of our interventions.
5. Conclusion
This paper explores some of the potential benefits and opportunities for design and OR to join forces in addressing the increasingly complex challenges facing modern day healthcare delivery systems. OR has a long history of engaging with healthcare systems and has developed a strong sub-community around this topic. Design would benefit from learning from this experience and could in return complement OR’s approach with its own methods and perspectives on how to improve healthcare systems.
We suggest that a systems perspective, problem solving and stakeholder engagement are all common to design and OR, while design has unique strengths in approaches to creativity, iterative experimentation and prototyping, and OR brings expertise in quantitative and qualitative analytical and modelling techniques for improving organisational decision-making and system performance.
Both disciplines, however, have a challenge in common with regard to generating the empirical evidence of their impact on healthcare delivery. This presents an opportunity for collaborative research into better ways of evaluating systems-informed interventions in healthcare.
Nonetheless, it is recognised that, bringing these two communities together is no simple task and requires a coordinated effort. There would be a practical interest in combining the approaches of OR and design but also a research interest in analysing if and how such collaborations work, and what makes them more or less feasible and effective.
Acknowledgments
The authors thank Professor John Clarkson for his comments on earlier drafts.
Financial support
A.K. was funded through a Postdoctoral Interdisciplinary Fellowship by The Healthcare Improvement Studies Institute (THIS Institute), University of Cambridge. THIS Institute is supported by the Health Foundation, an independent charity committed to bringing about better health and healthcare for people in the UK.







