Introduction
The primary purpose of foodborne illness outbreak investigations is to identify the source of illness in order to implement control and prevention measures. Investigators collate evidence from three streams of investigation: microbiological, food safety and epidemiological. The epidemiological investigation involves collecting information to generate, refine and ultimately test hypotheses regarding the source of illness. The hypothesis generation process is a critical step, as the findings inform further investigative activities and the ability to take action [Reference Gregg1, 2]. Despite the importance of hypothesis generation, it is often not well described in published outbreak investigation reports, limiting the ability of investigators to learn from other experiences [Reference Ickert3]. In some investigations, a hypothesis is easily identified, but in other investigations, particularly those involving novel or unusual food products, the hypothesis generation phase can be challenging and complex. Hypothesis generation methods vary by investigation and typically iterative and overlapping. Hypothesis generation methods that may be used in foodborne illness outbreaks include case interviewing techniques (e.g. close-ended hypothesis-generating questionnaires), food history supplementation (e.g. loyalty card data), food item investigation (e.g. sampling of food from case homes), expert consultations (e.g. discussions with commodity experts) and review of additional data sources (e.g. literature reviews).
Shiga-toxigenic E. coli (STEC) is an important pathogen that causes foodborne disease. In Canada, the number of reported cases of E. coli non-O157 infections has increased over the last several years with an incidence rate from 0.41/100 000 in 2012 to 0.99/100 000 in 2017, whereas the number of E. coli O157 infections has remained relatively constant [4]. The increase in E. coli non-O157 infections has been attributed to changes in testing and reporting practices [Reference Chui5]. Despite this change, the true burden of illness is likely underestimated as E. coli non-O157 strains are not routinely screened for by private laboratories in some provincial jurisdictions. Historically, E. coli non-O157 outbreaks have been associated with a wide range of products including leafy greens and beef, as well as a 2016 outbreak in the United States linked to wheat flour [Reference Kinnula6–Reference Crowe9].
In December 2016, a cluster of six E. coli O121 cases were identified in Canada with matching pulsed-field gel electrophoresis (PFGE) pattern combinations. Cases were geographically dispersed and had symptom onset dates within 5 weeks of each other. This was the first national outbreak associated with a non-O157 strain of E. coli identified and the first outbreak linked to wheat flour. This paper describes the outbreak investigation, highlighting the various methods used for hypothesis generation during the investigation.
Methods
Case identification
A confirmed case was defined as a resident or visitor to Canada with E. coli non-O157 that had one of the outbreak PFGE pattern combinations or was closely related by whole-genome sequencing (WGS) with symptom onset on or after 1 November 2016. Closely related was defined as within 0–10 whole genome multi-locus sequencing typing (wgMLST) allele differences.
Laboratory investigation
To aid with case identification, PFGE was completed by provincial laboratories on all E. coli non-O157 isolates reported in Canada since 1 November 2016. WGS analysis was also completed by PulseNet Canada using wgMLST within Bionumerics v.7.6 (Applied Maths) [Reference Rumore10]. Clinical and non-clinical isolates were considered related by WGS if they were within 0–10 wgMLST allele differences. PulseNet Canada compared the Canadian isolates to the 2016 US flour outbreak based on WGS data. In-silico prediction of virulence factors was done for Canadian isolates using the genotyping plug-in within BioNumerics v7.6 [Reference Lindsey11].
Hypothesis generation
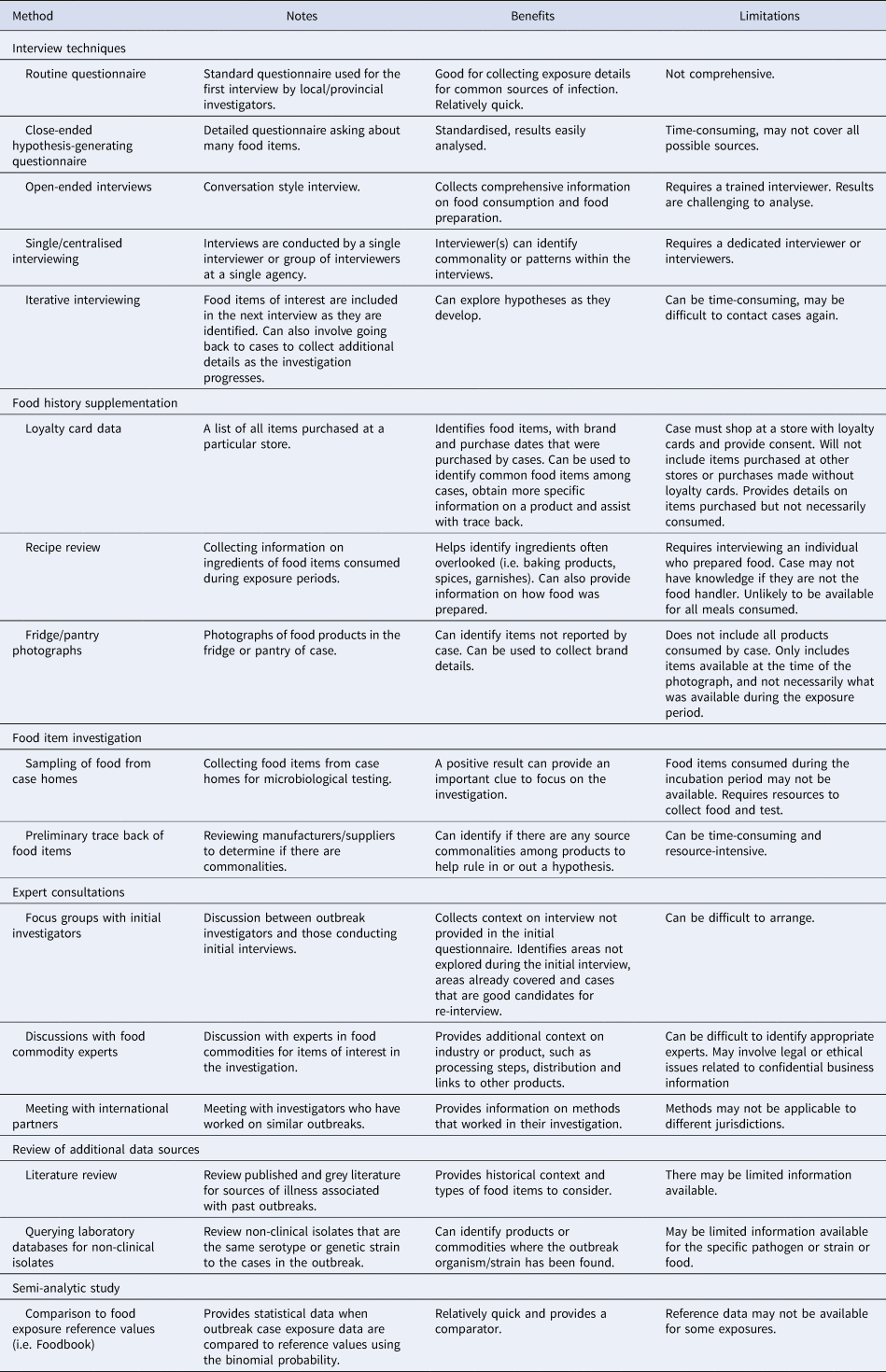
A variety of hypothesis-generating methods were used during this outbreak investigation. The most successful methods are described in detail below, with additional methods listed in Table 1.
Table 1. Summary of hypothesis generation techniques used in the investigation of E. coli O121 infections, Canada, 2016–2017
Interview techniques
Initial case interviews were conducted by local public health investigators using routine provincial case questionnaires or the national E. coli hypothesis-generating questionnaire. Routine case questionnaires differ by the province in regard to the specific exposures included and the level of details collected on these exposures. This initial interview is often conducted before typing information is available to indicate the case is part of an outbreak investigation.
In order to collect more information on exposures, two initial cases were centrally re-interviewed by a single interviewer at the Public Health Agency of Canada (PHAC) using the E. coli national hypothesis-generating questionnaire, which is a close-ended questionnaire including an extensive list of possible sources of illness. When a suspect source was not identified, the interview strategy moved to open-ended interviewing by a single, centralised interviewer from PHAC. Open-ended interviews did not follow a questionnaire or script; these interviews were designed to elicit free-form responses. Cases were asked about food consumed the week prior to symptom onset as well as general food preferences, purchasing habits and cooking practices. Knowledge of the 2016 E. coli O121 flour-associated outbreak in the U.S. prompted interviewers to ask about baking when open-ended interviewing was initiated [Reference Crowe9]. As new exposures were identified through case interviews, these exposures were included in subsequent open-ended case interviews as part of an iterative hypothesis generation process. Following a hypothesis generation session with the U.S. Centers for Disease Control and Prevention colleagues, who had investigated an outbreak of E. coli O121 that was associated with contaminated flour earlier in 2016, exposure to raw flour or dough was also asked during case re-interviews [Reference Crowe9].
Food history supplementation
Cases were asked about the availability of grocery store loyalty card records to provide detailed information on grocery store purchases. In the early stages of the investigation, loyalty card information for purchase histories of 2 months prior to onset was requested. As the investigation progressed and lengthened in time, a longer period, up to a year, was used for loyalty card information. Information from loyalty card records was categorised, collated and analysed to identify common food products.
Food item investigation
Cases were asked if any leftover food items that were consumed in the week prior to their illness were available for sampling. The food items were tested for verotoxigenic E. coli (VTEC) if they were items of interest at that point in the investigation and were biologically plausible.
Food safety investigation
Once a positive finding of E. coli O121 was identified in an open sample of Brand X flour from a case home, two intact bags from the same production lot were collected and tested from a retail establishment. To determine if other flour lot codes could be affected, a range of flour products of different sizes and production dates manufactured at the originating mill between 1 September and 30 November 2016 were sampled and tested. An environmental investigation was conducted at the originating mill. Trace-back activities included reviewing raw grain input, production records and processing information to identify possible common inputs to the affected flour. Trace forward was done by following-up with food companies that had received recalled flour to determine if additional products had been made from the recalled flour that was for sale in a raw state (e.g. raw dough, uncooked pie crusts, etc.).
Results
Case identification
A total of 30 confirmed cases of E. coli O121 were identified in this outbreak investigation with symptom onset dates between 13 November 2016 and 3 April 2017. Cases ranged in age from 2 to 79 years (median 23.5 years) and 15 (50%) were female. Eight cases were hospitalised, one case developed haemolytic uremic syndrome and no deaths were reported.
Laboratory investigation
Twenty-nine clinical outbreak isolates in this cluster had the same PFGE or highly similar PFGE pattern combination, all of which were new to the PulseNet Canada database. The one remaining clinical isolate had only the primary PFGE enzyme pattern available, but it was related to the other cases based on WGS. All clinical outbreak isolates were serotyped as E. coli O121. Of these, 28 were further typed as O121:H19 and two were unable to be typed further. All clinical and food isolates grouped together with 0–6 wgMLST allele differences and were considered related by WGS. None of the Canadian isolates were considered related by WGS to the 2016 US outbreak associated with flour or related to any other isolates in Canada. Based on in-silico testing, the Canadian clinical isolates carried the stx2 gene.
Hypothesis generation
A timeline illustrating when key hypothesis generation methods were implemented and significant events in the outbreak investigation occurred can be seen in Figure 1.
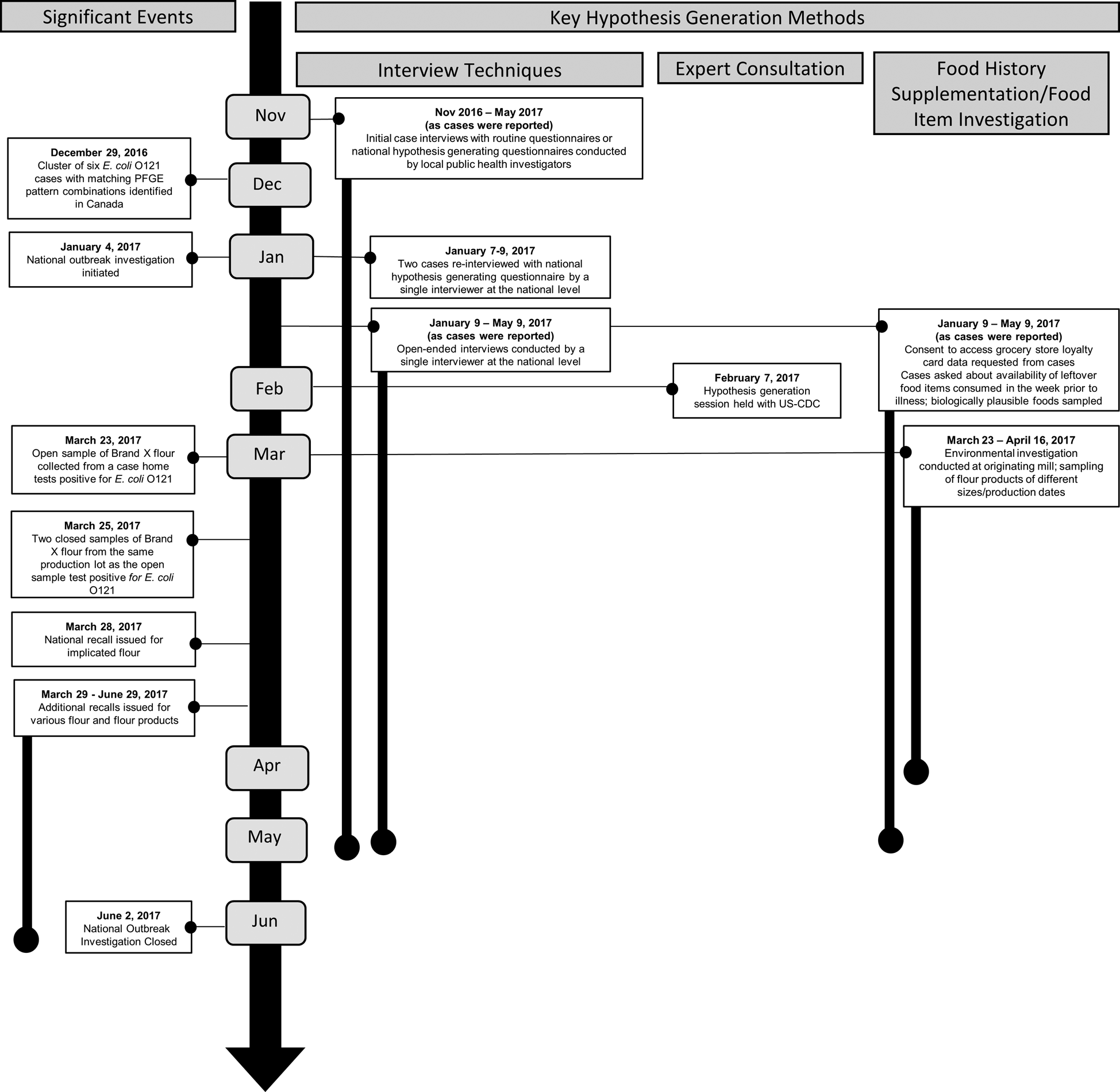
Fig. 1. Timeline of significant events and key hypothesis generation methods used in the investigation of E. coli O121 infections, Canada, 2016–2017.
Interview techniques
All 30 cases were interviewed by local public health investigators, 21 with routine provincial case questionnaires and nine with the national E. coli hypothesis-generating questionnaire. Two cases were re-interviewed by PHAC using the national E. coli hypothesis-generating questionnaire before the interview strategy moved to open-ended interviewing. Initial case interviews identified ground beef as a possible source of infections, as all six initial cases reported this exposure.
Three of these cases had consumed hamburgers at two different restaurant chains in the same province. Local public health investigators in that province determined that these restaurants obtained hamburgers from the same supplier. These initial cases were predominantly younger males and convenience foods and restaurant exposures were commonly reported by these cases.
As more cases were reported, cases continued to report ground beef consumption, but other hypotheses also emerged, including sausage style deli-meats (e.g. pepperoni, salami, bologna and sausage), bacon, pizza, pork pieces or parts and oats (e.g. raw oats, oatmeal and/or granola bars). As additional cases were reported, ground beef and sausage-style deli meats were no longer frequently reported and further data collected about these exposures did not converge on any specific products.
In total, 25 cases were re-interviewed centrally by PHAC using an open-ended approach. Just over half of these cases (13/25; 52%) were re-interviewed by PHAC on two separate occasions to ask additional questions and gather more specific information; two cases were re-interviewed three and four times, respectively.
During open-ended interviewing, the exploration of cooking and baking behaviours in the home revealed exposures to raw flour and consumption of raw batter/dough. Further questioning on brand names uncovered Brand X flour as a commonly used ingredient in baking and cooking.
Once flour was identified as the likely source, this information was strengthened by re-interviewing cases that had not been specifically asked about flour exposure earlier in the investigation to ask about their flour exposure. At the conclusion of the outbreak, 12 cases had reported using or probably using Brand X flour during the exposure period and 16 cases reported that Brand X flour was used or was probably used in the home during their exposure period (Table 2). Twelve cases had both direct and indirect exposure to Brand X flour in the home and four cases had only indirect exposure to Brand X flour though baking done by others in the home. Information on brand was obtained for 7/12 (58%) cases that had direct exposure and 12/16 (75%) cases that had indirect exposure to Brand X flour only after flour was identified as the source of the outbreak. Of cases that did not report exposure to Brand X flour, one case reported exposure to pizza made at a restaurant that used flour produced by the implicated mill. An additional three cases may have had occupational exposure: one case was a baker in a restaurant (brand of flour used at work was unknown) and two cases were grocery store cashiers who may have had contact with flour through their work.
Table 2. Proportion of cases reporting flour exposures in the investigation of E. coli O121, Canada, 2016–2017
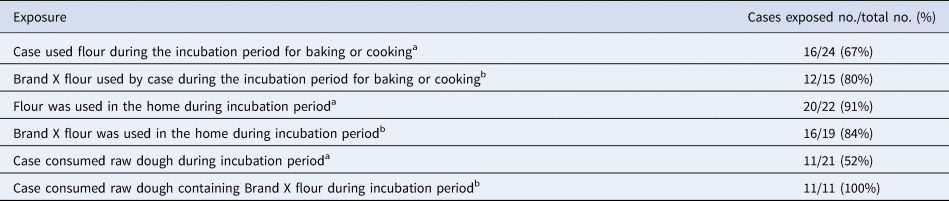
a Denominator includes the number of cases reporting yes, probably, or no to specific exposures, cases were excluded if they were not asked or did not know.
b Denominator excludes cases that did not report direct or indirect flour exposure and those that did not recall the brand name of flour used.
Food history supplementation
Loyalty card purchase records were available for 12 cases and 28 stores. Analysis of these records did not identify potential hypotheses outside of those identified through case interviews. Purchase records of four cases verified the purchase of Brand X flour and purchase date. Three additional cases had purchased other brands of flour and the remaining five cases had no record of flour purchases.
Food item investigation
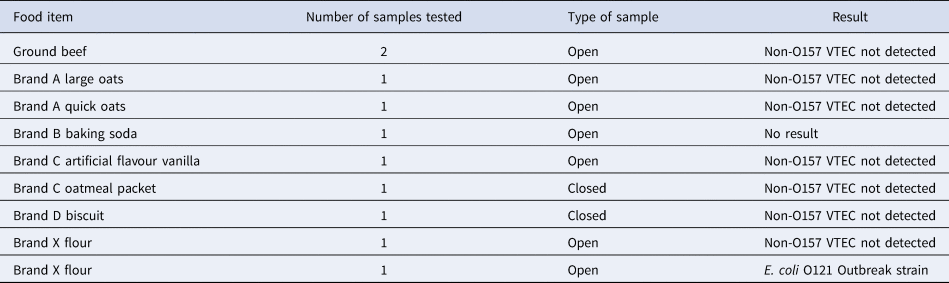
Ten foods were collected from case homes during the investigation to aid hypothesis generation, including samples of flour (N = 2), oats/oatmeal (N = 3), ground beef (N = 2), baking soda (N = 1), vanilla (N = 1) and biscuits (N = 1) (Table 3). On 23 March 2017, one of the open samples of Brand X flour collected from a case home tested positive for E. coli O121 with PFGE and WGS that matched the outbreak strain. This sample had complete lot code information available and the case had not used or handled the flour after illness onset. Results for all other samples were not detected for VTEC.
Table 3. List of food items tested from confirmed case homes as part of hypothesis generation activities during the investigation of E. coli O121, Canada, 2016–2017
Food safety investigation
Both flour samples collected from a retail establishment tested positive for E. coli O121 and matched the clinical cases by PFGE and WGS. A national recall for the implicated lot of flour was conducted on 28 March 2017. A total of 109 samples from 257 bags of Brand X flour were sampled and tested (226 bags from retail establishments and 31 bags from consumer complaints). A total of 12% of samples tested positive for VTEC. The outbreak strain of E. coli O121 was isolated in several Brand X flour products of different sizes and production dates between 1 September and 30 November 2016. In addition to E. coli O121:H19, a number of different E. coli serotypes, including O8:H19, O8:H28, O15:H4, O88:H25 and O187:H52, were identified during testing of closed and open samples of flour, but no clinical cases were a match to these serotypes. Additional recalls for flour and flour-containing products were conducted between 28 March and 29 June 2017. No deviations were noted at the originating mill where the recalled product was manufactured. There was no kill step in flour processing and no testing for pathogens done at the mill. Investigation at the mill did not identify a specific source of E. coli contamination in the respective flour products.
Discussion
This investigation utilised several hypothesis generation methods in order to identify Brand X flour as the source of the outbreak (Table 1). Open-ended interviewing and product sampling from case homes proved to be successful hypothesis generation methods in this investigation. Other hypothesis-generating methods were not as useful in this investigation, included loyalty card data, recipe and pantry photo comparisons and food exposure reference values. However, outbreak investigations are unique and methods that may not have contributed information in this outbreak may prove to be more beneficial in other outbreak investigations. This outbreak also demonstrated the importance of triangulation of information from multiple hypothesis generation techniques to identify the source of infection.
The open-ended interview approach allowed the flexibility to explore sources of illness that were not initially considered and were not included in the hypothesis-generating questionnaires. The open-ended interviews were completed by two interviewers within one agency. However, the majority of interviews were completed by a single interviewer. Centralised re-interviewing cases from geographically dispersed jurisdictions enabled the interviewers to identify themes and food products in common among the cases. Although this method proved successful in this investigation, centralised open-ended interviewing can be resource-intensive and requires the availability of a highly trained professional. Also, the largely qualitative data obtained from these interviews can be challenging to analyse, there is not a consistent list of food items covered in each interview, and the data obtained may reflect food preferences or typical foods consumed rather than definitively consumed products. Open-ended interviewing with a single or central interviewer should be considered when investigating outbreaks where no source emerges through interviews with routine or hypothesis-generating questionnaires or when an ingredient, like flour, is suspected.
In this outbreak, the collection of food samples from case homes was conducted as part of hypothesis-generating activities. These items were collected if they represented products consumed by cases during the incubation period. As these were mostly open samples, the presence of bacteria would not automatically confirm the product as the source of the outbreak, but rather provide additional evidence to be considered in the investigation. In this investigation, the finding of the outbreak strain of E. coli O121 in an open sample resulted in a hypothesis that was tested by re-interviewing cases to ask specifically about flour as well as a food sampling plan. The open sample provided lot code and brand details which were necessary to inform the food safety investigation and take public health action (i.e. product recall).
Flour is a challenging food item to identify as it is a raw ingredient used both in cooking and baking and is not an easily recalled exposure by cases. Previous outbreaks have identified contaminated flour used in a specific product (i.e. cookie dough) as a risk factor or baking as a risk activity [Reference Crowe9, Reference Neil12, Reference McCallum13]. In this outbreak, flour was a possible exposure considered from the start because of the recent US outbreak. However, the majority of initial cases did not report baking or cooking and had other food exposures in common (i.e. ground beef and convenience foods). As additional cases were reported, no clear profile emerged: cases were varied in their age, gender, food preferences and baking or cooking behaviours. It was only after probing specifically about exposure to flour and licking the spoon while baking that flour became an item of interest. Many cases had to be contacted multiple times and asked multiple questions about flour, baking or cooking activities and consumption of raw dough or licking the spoon when there was baking in the home in order to get details on flour and Brand X exposure. There were also four cases who were exposed to Brand X flour though baking was done by others in the home, suggesting that cases should be asked about baking in the home as part of flour investigation.
Twenty-six per cent (6/23) of outbreak cases who were asked about flour exposure reported that they were not exposed to Brand X flour prior to their illness onset. This is not unusual in an outbreak investigation, as there are many reasons why a case may not recall exposure to a specific product (e.g. poor recall, ingredient in a food made by others, occupational exposure, cross-contamination). It is also possible that cases had exposure to the implicated flour through other products that were not identified during the food safety investigation or were not asked about during the re-interview (e.g. pizza made with Brand X flour).
This outbreak was the first national outbreak of non-O157 E. coli in Canada. Testing for non-O157 E. coli varies by province and territory. In some provinces, stool samples are tested for the Shiga-toxin-producing gene but in other provinces, this is not routine and only done by request. This may lead to under-diagnosis of non-O157 cases. In addition to these testing limitations, at the time of this outbreak, typing of E. coli non-O157 isolates using PFGE was not routinely done on all isolates. However, advancements in next-generation sequencing technologies as well as significant decreases in the cost of processing samples, coupled with the higher discriminatory power of WGS compared to traditional methods such as PFGE prompted Canada to transition to using WGS as the primary subtyping method for all non-O157 E. coli isolates in June 2018. This outbreak was the first in Canada to implicate flour as the source of illnesses and the second flour related outbreak in North America since 2015. Genetic analysis of E. coli O121 strains implicated in the Canadian and American outbreaks concluded that they were not related. In both these outbreaks, the root cause of contamination was not identified [Reference Crowe9]. Flour is a raw agricultural product and is manufactured without the application of a kill step for pathogenic bacteria. Wheat is exposed to possible sources of contamination during growing and harvesting that can carry over to the end product. These recent E. coli O121 flour outbreaks, combined with the finding of other E. coli non-O157 serotypes in closed flour samples, suggest that flour is an emerging vehicle for non-O157 STEC infections and should be considered as a potential source in non-O157 STEC outbreak investigations.
Acknowledgements
The authors thank the following organisations for their contribution to the outbreak investigation: local public health colleagues and public health laboratories in British Columbia, Alberta, Newfoundland and Labrador, Saskatchewan, Ontario, Quebec and Washington State; British Columbia Centre for Disease Control; British Columbia Centre for Disease Control Public Health Laboratory; Alberta Health; Alberta Health Services; Public Health Laboratories; Newfoundland and Labrador Department of Health and Community Service; Saskatchewan Ministry of Health; Newfoundland & Labrador Public Health Laboratory; Roy Romanow Provincial Laboratory; Public Health Ontario; Public Health Ontario Laboratory; Ontario Ministry of Health and Long-Term Care; Ministère de la Santé et des Services sociaux du Québec; Laboratoire de santé publique du Québec; Canadian Food Inspection Agency; Health Canada; Public Health Agency of Canada and the Centres for Disease Control and Prevention.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None.
Data
The data from this paper are not publicly available due to privacy concerns and legislative requirements. Please contact the corresponding author (VM) for additional information on data.







