No CrossRef data available.
Article contents
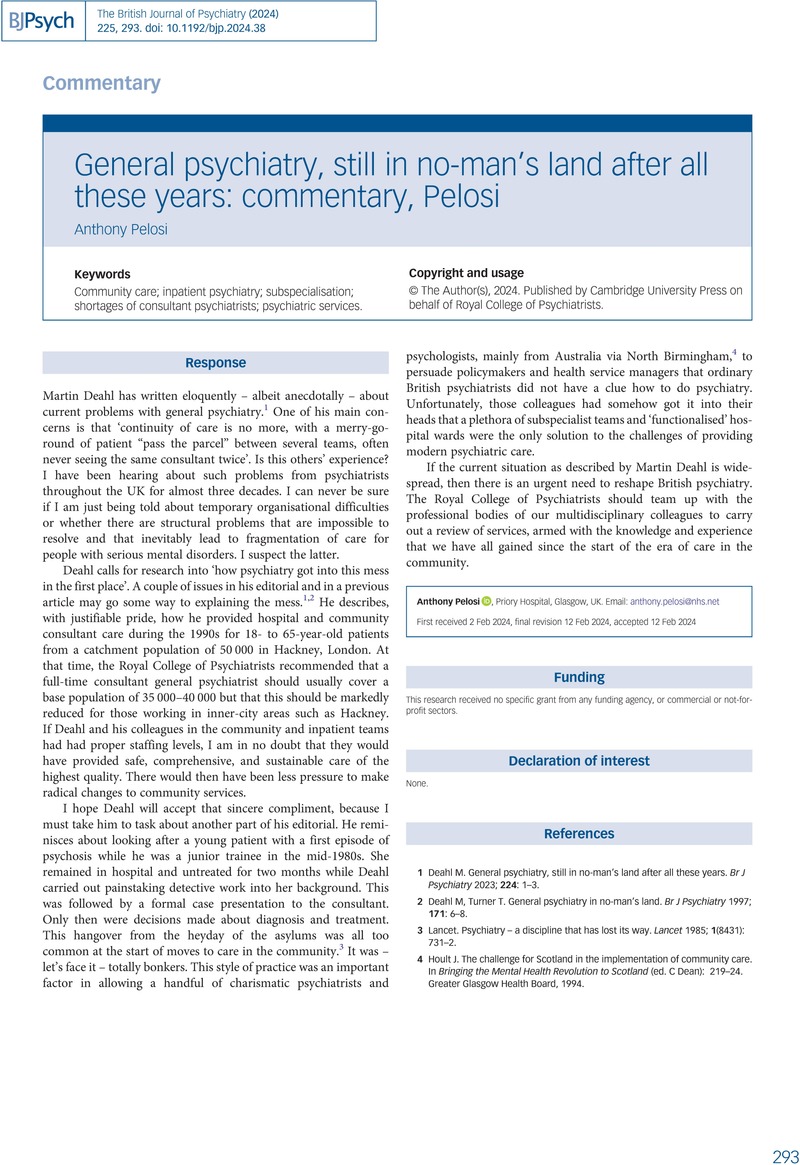
General psychiatry, still in no-man's land after all these years: commentary, Pelosi
Published online by Cambridge University Press: 02 September 2024
Abstract
An abstract is not available for this content so a preview has been provided. Please use the Get access link above for information on how to access this content.
Keywords
- Type
- Commentary
- Information
- Copyright
- Copyright © The Author(s), 2024. Published by Cambridge University Press on behalf of Royal College of Psychiatrists
References
Deahl, M. General psychiatry, still in no-man's land after all these years. Br J Psychiatry 2023; 224: 1–3.Google Scholar
Deahl, M, Turner, T. General psychiatry in no-man's land. Br J Psychiatry 1997; 171: 6–8.10.1192/bjp.171.1.6CrossRefGoogle ScholarPubMed
Hoult, J. The challenge for Scotland in the implementation of community care. In Bringing the Mental Health Revolution to Scotland (ed. C, Dean): 219–24. Greater Glasgow Health Board, 1994.Google Scholar



eLetters
No eLetters have been published for this article.