Introduction
A critical focus of the US response to coronavirus disease (COVID-19) is to protect nearly 18 million health care personnel (HCP). 1 Without proven, effective treatments, use of personal protective equipment (PPE) remains key to HCP safety. To date, the Centers of Disease Control and Prevention (CDC) has provided PPE recommendations in the United States to facilitate a safer work environment. 2,3 Through an online, anonymous survey, we collected data on adherence to CDC PPE guidelines among HCP in different US states.
Methods
By referencing guidelines from the CDC, 2,3 we defined the standard of optimal PPE use in 5 different clinical scenarios (Table 1). Following approval from the review board at Brigham and Women’s Hospital, an online questionnaire was designed, using REDCap (Vanderbilt University, Tennessee), and distributed among statewide health care institutions and to HCP through the snowball sampling technique. Adherence was determined by calculating the proportion of respondents who met the optimum PPE standard. Data were processed and analyzed using Microsoft Excel 365 (Microsoft, WA) and RStudio 1.2.5033 (RStudio, MA).
Table 1. Clinical scenarios and optimal personal protective equipment combinations
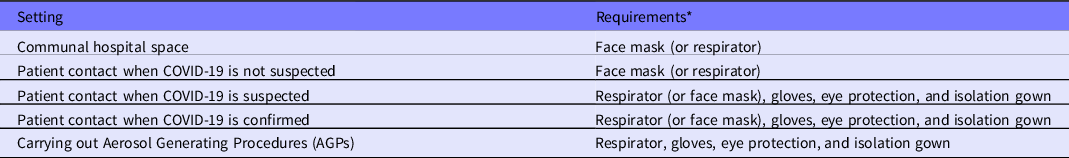
Note:
* To accommodate for PPE shortages, the CDC guidelines state that surgical masks are an acceptable alternative for patient contact when COVID-19 is suspected or confirmed when there is a shortage of respirator masks. We accommodate this as adherent to the guidelines.
Results
From June 15 to July 17, 2020, 2245 responses from 44 US states were collected; 436 responses from 8 states – Washington (n = 61); Texas (n = 64); South Carolina (n = 30); Oregon (n = 25); Louisiana (n = 100); Colorado (n = 41); California (n = 62); Arizona (n = 53) – are included in the quantitative analysis. Only the first 100 of 1760 responses received from Louisiana were analyzed to control for sampling bias. Respondents included nurses (57.8%), doctors (26.8%), midwives (11.5%), paramedics (1.9%), medical technicians (1.2%), and unknown/unstated (0.7%). Among different professions, doctors demonstrated greatest adherence in all scenarios except for “patient contact when COVID-19 suspected,” for which nurses demonstrated the highest adherence. The rate of adherence to optimum PPE guidelines in the 8 states included is shown in Figure 1.
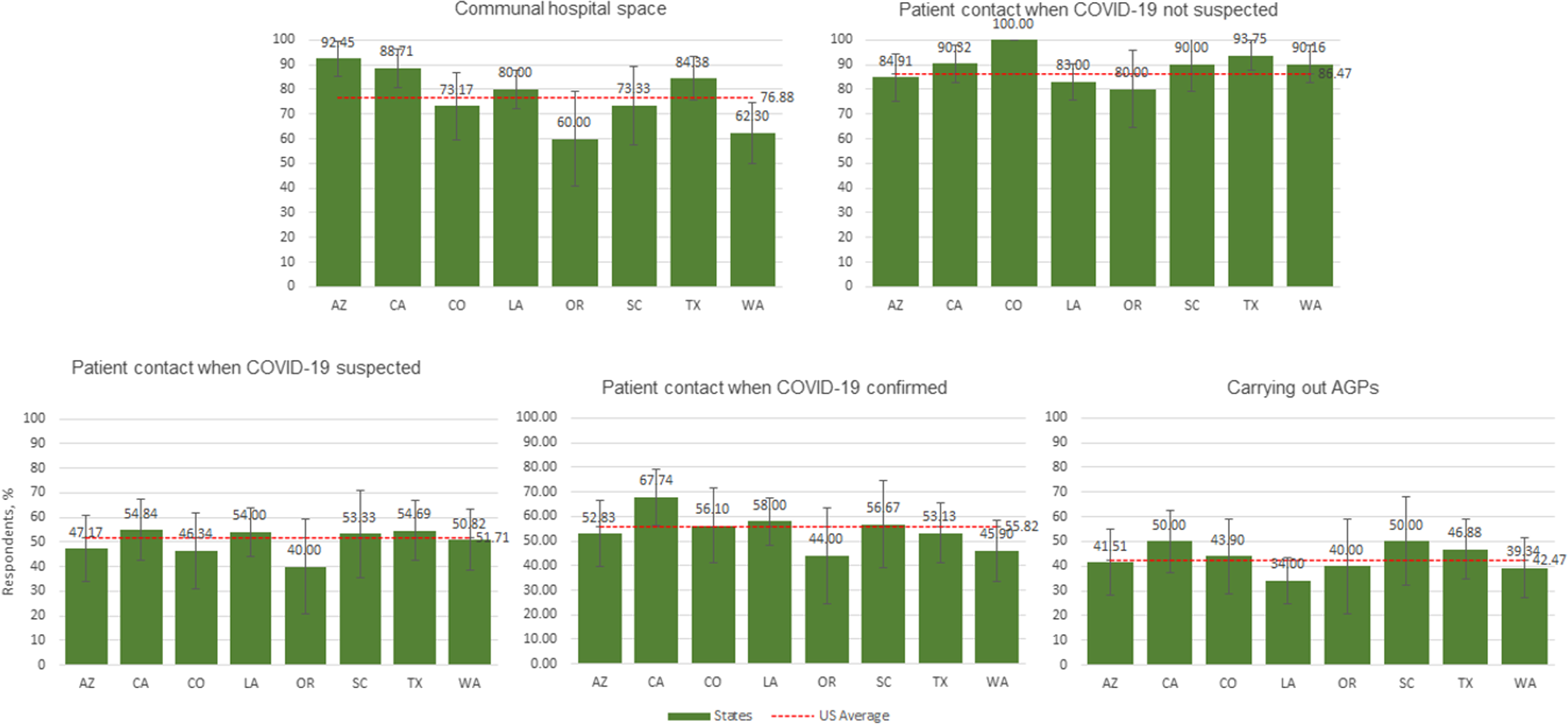
Figure 1. Percent adherence to optimum personal protective equipment (PPE) guidelines in 5 clinical scenarios in different states: WA, Washington; TX, Texas; SC, South Carolina; OR, Oregon; LA, Louisiana; CO, Colorado; CA, California; AZ, Arizona.
Discussion
HCP adherence to PPE guidelines has remained a key concern throughout the ongoing COVID-19 crisis, particularly because effective prophylaxis and treatments have yet to become available. Based on a prior global survey study conducted by Panayi et. al. Reference Panayi, Flores-Huidobro and Wu4 regarding HCP adherence to the World Health Organization PPE recommendations, we investigated nationwide adherence to CDC PPE recommendations among HCP, during a time when the COVID-19 crisis has been rapidly evolving.
Among the 8 states included in this report, the highest and lowest complete adherence to 4 of 5 clinical scenarios were seen in California and Oregon, respectively. While adherence to the PPE guidelines in different clinical scenarios varied widely, our results showed average adherence in each scenario is poor (ranging from 42.47% to 86.47%). As a general trend, HCP adherence to PPE in “Patient contact when COVID-19 is not suspected” was highest, and in “Carrying out AGPs” was lowest compared with the other clinical scenarios.
Although this study provides new insights on the use of PPE among HCP, its limitations cannot be ignored. Data were included from only 8 states, which limits the generalizability of the results. Further, individual institutional guidelines can influence HCP understanding of optimum standard PPE-use in different scenarios. PPE availability is changing rapidly as state and local decision makers adapt to their situations. These data represent only 1 time frame during the course of a longer public health crisis and should be considered in this context.
Conclusions
Factors driving low adherence rates may be PPE shortages, insufficient training, and/or a low level of awareness among HCP, as well as the inability to remain informed on rapidly evolving recommendations by the CDC or individual institutional administrations. Although our survey does not reflect possible reasons for such variability, it highlights the need to address disparities in PPE use among different HCPs and to urgently investigate the factors that may be contributing to disparities among the states. Providing effective training programs, an adequate supply of PPE, and in-training evaluation are top strategies that can be enforced by policy-makers and safety managers of health care institutions. Further research is warranted to identify which strategies may be most useful.
Acknowledgments
We thank those who helped disseminate the survey on various platforms: Karen C. Lyon, PhD, MBA, APRN-CNS, NEA; Medical Societies of Washoe County, NV, Philadelphia County, PA, Baltimore County, MD, Harford County, MD, TriCounty, TX, Pueblo County, NM, Metropolitan Portland, OR; South Carolina Medical Association; Maryland Dermatologic Society; South Carolina Nurses Association; North Dakota Nurses Association; North Dakota Center for Nursing; Virginia Midwives Alliance; VA Affiliate of the American College of Nurse-Midwives; and Wisconsin EMS Association.
Author contributions
OAD and AA contributed equally as co-first authors.
Funding Statement
This manuscript, in part, was funded by an NIH 5 T35 HL110843 fellowship position to OAD.
Conflict(s) of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this paper.




