CLINICIAN'S CAPSULE
What is known about the topic?
Emergency department (ED) physicians have been previously identified outside of Canada as a high-risk specialty for burnout.
What did this study ask?
What is the burnout rate among ED physicians in Canada just before COVID-19?
What did this study find?
Canadian physicians experience high rates of burn-out, with 86.1% meeting at least one of the criteria for burnout in Canada just before COVID-19.
Why does this study matter to clinicians?
Front-line staff will be adversely affected by COVID-19 both during and after the pandemic. Baseline data are needed.
INTRODUCTION
International data indicates that emergency medicine (EM) is one of the most unwell professions with a high risk for burnout.1–Reference Kane4 (Additional references available in the online Supplemental Appendix.) Consequences of burnout in medicine are severe and impact patient care, the health care system, and physician health.Reference Wallace, Lemaire and Ghali5 Burnout results in lower quality care, increased medical errors, lower patient satisfaction, increased physician turnover, increased cost, and lower productivity.Reference Wallace, Lemaire and Ghali5 Physician health effects include increased substance abuse, depression, and suicidal ideation.Reference Wallace, Lemaire and Ghali5 COVID-19 has fundamentally disrupted the world and EM physicians are at extensive risk of further health-related and psychological injury.Reference Wu, Styra and Gold6 Studies have indicated a risk of depression, anxiety, and mental health complaints in the frontlines in China during the early days of COVID-19.Reference Lai, Ma and Wang7 A baseline on the current rate of burnout, depression, and suicidality of EM physicians in Canada would be of great importance to monitor their health during and post-COVID pandemic and the effect of any wellness interventions to support them.
METHODS
Survey design
The survey tool available in English included demographic information, the Maslach Burnout Inventory – Health Services Tool (MBI-HSS), Patient Health Questionnaire (PHQ-9), and a question regarding if the physician had ever or in the past 12 months contemplated suicide. The survey was pilot tested and reviewed for accuracy among ED doctors from lead authors home institution.
The MBI-HSS is a standardized validated 22-item tool that scores questions on a 7-point Likert scale, across three dimensions: emotional exhaustion, depersonalization, and personal achievement.Reference Maslach, Jackson and Leiter8 The PHQ-9 is a standardized validated instrument for screening and measuring the severity of depression in five categories. This study was approved by Western University's Health Science Research Ethics Board.
Survey distribution
The survey was distributed using a modified snowball method. An invitation to join a roster (February to May 2019) was sent by means of the Canadian Association of Emergency Physicians (CAEP) survey distribution network, posted on social media (Facebook, Twitter, CAEP website), and physical posters at the 2019 CAEP Annual Conference. Rostered physicians were then asked to forward the invitation to any EM physician in Canada. The survey was distributed in June 2019 with reminders sent at week 2 and 4 post invitation. The total sample size was not captured. All data were collected anonymously using the REDCap platform housed at the host institution, and responses were reported in aggregates.
Outcome measures
The primary outcome was the percentage of EM physicians who met the criteria for burnout. The MBI-HSS was used to assess burnout on three dimensions (defined as emotional exhaustion ≥27, depersonalization ≥10, or personal accomplishment <34).Reference Doulougeri, Georganta and Montgomery9 Secondary outcomes were burnout rates by gender and years of practice. Percentage of respondents by severity of depression on the PHQ-9 scale, as well as percentage positive to suicidal ideation in career/past year, were obtained. A violin plot was created displaying the distribution of total score for each MBI domain to visualize the proportion above the MBI threshold.
Data analysis
Data were analyzed using SPSS version 23 (IBM Corp, Seattle, WA). Demographic information was analyzed descriptively. Categorical data were presented using proportions with percentages, and continuous data were tested for normality and presented as a median with interquartile range. Differences between groups were calculated using chi-square analyses.
As a secondary outcome, a logistic regression analysis was performed to assess which variables were associated with burnout. Variables were first analyzed in a univariate manner, and variables found to be associated (p < 0.1) with burnout were included as initial input in a multivariable model to determine which factors were independently associated with physician burnout.
Backward, stepwise multivariable logistic regression (Wald removal criterion 0.1) was used to determine predictor variables independently associated with burnout. Likelihood ratio tests were used to determine appropriate inclusion of variables in the multivariable model.
RESULTS
A total of 384 respondent surveys were included in the final analysis after exclusion of 43 surveys where only the demographic information was completed. Respondents were primarily male (213/383, 55.6%) and married (327/384, 85.2%) with a median [IQR] of 17.5 [7.25–26.0] years of experience since residency.
Respondent MBI mean domain scores were emotional exhaustion 34.07 [23–43.25], depersonalization 16.35 [11–21.25], personal accomplishment 45.64 [41–51]. A total of 86.1% (329/382) met at least one of the criteria for burnout. Plots for mean domain score and thresholds can be seen in Figure 1.
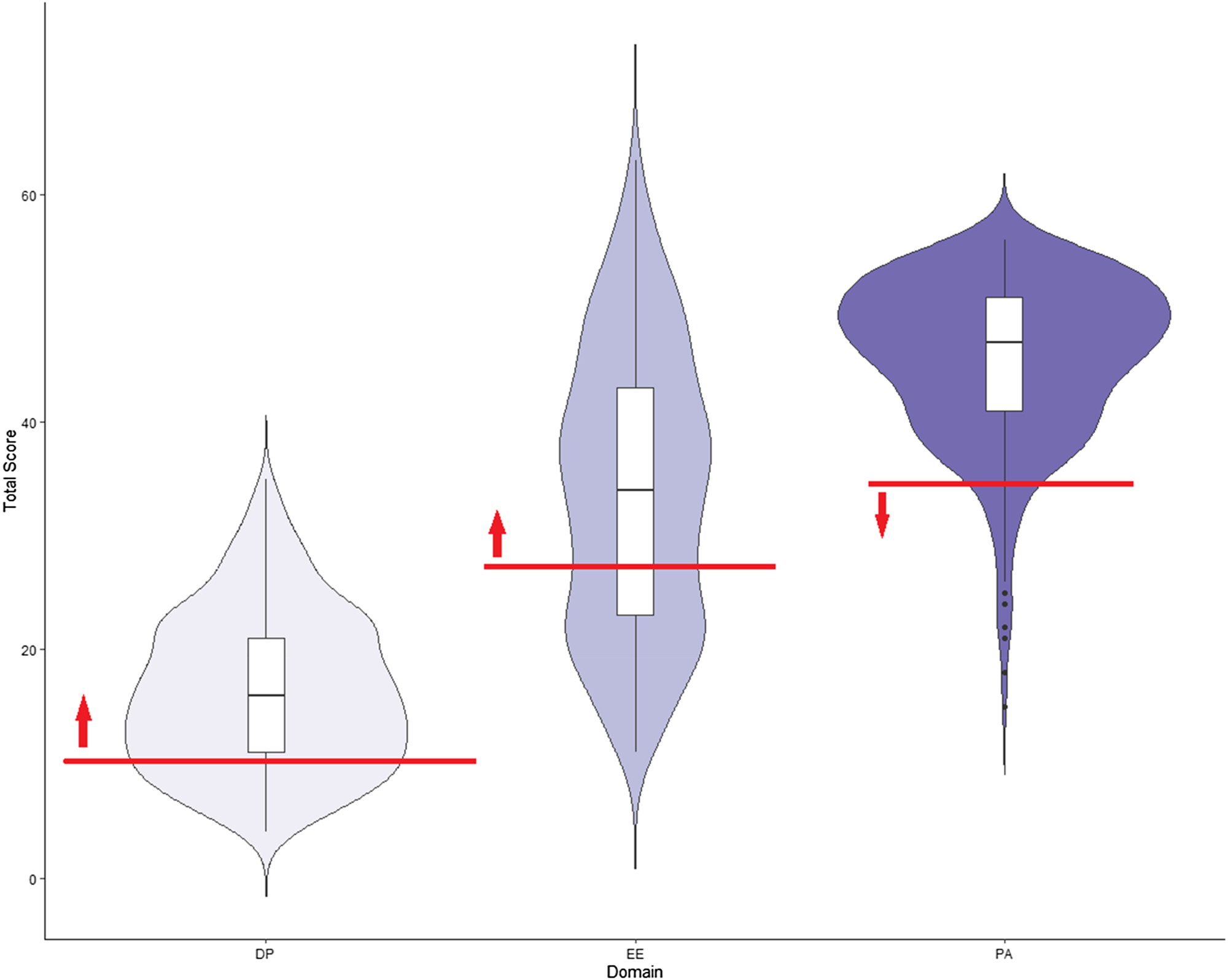
Figure 1. Violin plot showing threshold and distribution for burnout. Red lines indicate burnout threshold with respect to each domain. Arrows indicate all participants who met or exceeded the threshold for burnout. DP, depersonalization; EE, emotional exhaustion; PA, personal achievement.
The majority of respondents of the PHQ-9 (217/374; 58.0%) scored as “minimal-none” for depression while those scoring as mild, moderate, moderately severe, and severe were 24.3%, 11.5%, 4.0%, and 2.1%, respectively. Of respondents, 14.3% (53/371) contemplated suicide during their EM career, and of those, 22/371 (5.9%) had considered suicide in the past year.
The logistic regression model correctly classified 86.5% of cases and explained 33.0% of the variance in burnout. Physicians aged 30–39 (compared with those 40–49 years) were almost four times more likely (95% confidence interval [CI], 1.03–15.1) to suffer from burnout. Physicians who were CCFP-EM trained were 2.7 (95% CI, 1.27–5.8) times more likely to suffer from burnout compared with FRCPC trained physicians. Finally, physicians with any indication of depression on the PHQ-9 were 43.7 times (95% CI, 5.9–321.8) more likely to suffer from burnout compared with those who score in the lowest “minimal” category.
DISCUSSION
In this national survey of Canadian EM physicians in the immediate period before COVID-19, an alarming number met the criteria of burnout by the MBI-HSS. Beyond simply meeting the dichotomous outcome, respondents unfortunately far exceeded the predefined thresholds (Figure 1). Additionally, EM physicians screened for moderate/severe depression 3× higher than the general population.Reference Kocalevent, Hinz and Brähler10 and had alarming rates of reported suicidal ideation. These results are consistent with the EM literature from the United States showing rates of burnout ranging from 65 to 80%,Reference Arora, Asha, Chinnappa and Diwan3 and the Canadian Medical Association study showing 19% of respondents contemplated suicide within their lifetime.1–Reference Kane4 (Additional references available in the online Supplemental Appendix.)
The strengths of this study involve the methods to increase the reach out to EM physicians using snowball techniques, social media, and posters at a national conference. Scales of measure were chosen with validity evidence, and rigorous statistical methods were used. Limitations for this study include the potential for selection bias. As a result of trying to reach a wide audience by means of a snowball methodology, we were unable to calculate a response rate, because the denominator is unknown. This cannot be considered population-based data due it being a convenience sample.
The long-term health effects for frontline workers due to COVID-19 should be a significant concern to government, hospitals, and doctors both during and after the pandemic. Current and future health systems and the patients they serve rely on healthy EM teams. Departments need to move toward making wellness interventions a priority now more than ever, and results of this survey can serve as a baseline for measurement to monitor and evaluate success of interventions and supports. The Canadian Medical Association has called for a national mental health support service,11 which would be a good first step, as comprehensive and centralized supports for EM physicians are needed. CAEP may be an important forum to provide support or advocate for services to this high-risk group.
CONCLUSION
In this survey of Canadian EM physicians just before the COVID-19 pandemic, the majority of physicians met the threshold for burnout and a concerning number of physicians have contemplated suicide. This baseline measurement will be useful as the COVID-19 pandemic will have serious and important healthcare implications during and after the pandemic.
Supplemental material
The supplemental material for this article can be found at https://doi.org/10.1017/cem.2020.431.
Financial support
The authors have no financial relationships relevant to this article to disclose.
Competing interests
The authors have no conflicts of interest relevant to this article to disclose.
Authors’ Contributions
RL conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. KVA designed the data collection instruments, collected data, carried out the initial analyses, helped draft and revised the manuscript. LR, SG, LF, and JF critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.



