Introduction
Disasters are events that kill, maim, and create needs that exceed available health care capacities. Natural disasters such as typhoon and flooding cause a significant burden of minor injuries requiring surgical wound care.1–Reference Centurion, Van Den Bergh and Gray3 This requires surgical instruments that must be decontaminated to avoid transmission of pathogens.Reference Leaper and Edmiston4,Reference Rutala and Weber5 There are different degrees of decontamination: clean, disinfected, and sterile.Reference Rutala and Weber5,6 Disinfected means that microorganisms have been destroyed or removed but does not necessarily include destruction of bacterial spores. Sterilization is the process used to render an object free from viable microorganisms, including viruses and bacterial spores, but not prions.6,7 The Spaulding classification is a widely accepted classification for decontamination of medical devices.Reference Rutala and Weber5 Surgical instruments and other reusable medical devices are classified into Critical, Semi-Critical, and Non-Critical devices based on their risk to spread infections.Reference Rutala and Weber5,7 Sterilized instruments (critical devices) are mandatory for surgery on intact skin while high-level disinfected instruments (semi-critical devices) are considered sufficient for non-intact skin, such as open wounds.Reference Leaper and Edmiston4,7 Common microbes found in open wounds are eradicated when instruments are disinfected.7,Reference Bessa, Fazii and Di Giulio8 However, spores from a few spore-forming bacteria may survive disinfection and potentially cause infections. However, it remains unclear to what extent this has clinical value in the disaster setting where wounds already are contaminated.
Following the chaos of unregulated international health care assistance after the 2010 Haiti earthquake, the World Health Organization (WHO; Geneva, Switzerland) and partners developed standards and classification for Emergency Medical Teams (EMTs) deployed to natural disasters.9 In these, EMT Type 1 provides fixed or mobile out-patient care including basic wound care.9 The EMT standards stipulate that wound care should only be done with disposable or autoclaved instruments using high pressure and steam.9 However, EMT Type 1 mobile experiences from the 2015 earthquake in Nepal, as well as the 2019 Mozambique typhoon, have highlighted significant logistical problems (ie, weight, size, and lack of electricity) with bringing an autoclave or sufficient disposable instruments to remotely affected areas to manage a significant number of minor wounds. To ensure rapid and mobile health response to disasters, there is need for decontamination techniques that are safe but also easy to both deploy and use in a resource-scarce field setting. This article aims to assess portable and non-electricity-dependent alternative techniques for safe decontamination of surgical material for minor wound surgery in disaster settings.
Materials and Methods
This scoping review followed established scoping review methodology defined by Arksey and O’Malley.Reference Arksey and O’Malley10 The Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) protocolReference Tricco, Lillie and Zarin11 was used. Three databases were searched (PubMed [National Center for Biotechnology Information, National Institutes of Health; Bethesda, Maryland USA], Web of Science [Thomson Reuters; New York, New York USA], and Global Health [EBSCO Information Services; Ipswich, Massachusetts USA]); grey literature via additional databases (Global Index Medicus [WHO; Geneva, Switzerland], Popline [Johns Hopkins Bloomberg School of Public Health; Baltimore, Maryland USA], Grey Matters [CADTH; Ottawa, Ontario, Canada], BASE, WHO HQ, JBI [Ovid Technologies; New York, New York USA], and INAHTA [Institute of Health Economics; Edmonton, Alberta, Canada]); data from relevant organizations (WHO, Médecins Sans Frontières [MSF; Geneva, Switzerland], and the International Committee of the Red Cross [ICRC; Geneva, Switzerland]); and various journals.
Articles were scanned for safe and feasible decontamination techniques. A technique was considered feasible if it was portable or did not require a power grid. Portability in this study is defined using the International Air Transport Association (IATA; Montreal, Quebec, Canada) recommended weight limit, stating that the maximum weight of any single piece should not exceed 23kgs.12 Minor wound surgery was defined as surgical management of already open and contaminated minor wounds that can be managed at a primary health service level such as EMT Type 1. A technique was considered safe if it achieved semi-critical decontamination level by either sterilization or high-level disinfection. A thematic analysis of the findings was performed and a numerical summary of the searches outlined using a PRISMA flowchart.Reference Tricco, Lillie and Zarin11,Reference Moher, Liberati and Tetzlaff13 The results were compiled in two tables.
Table 1. An Introduction to the Techniques
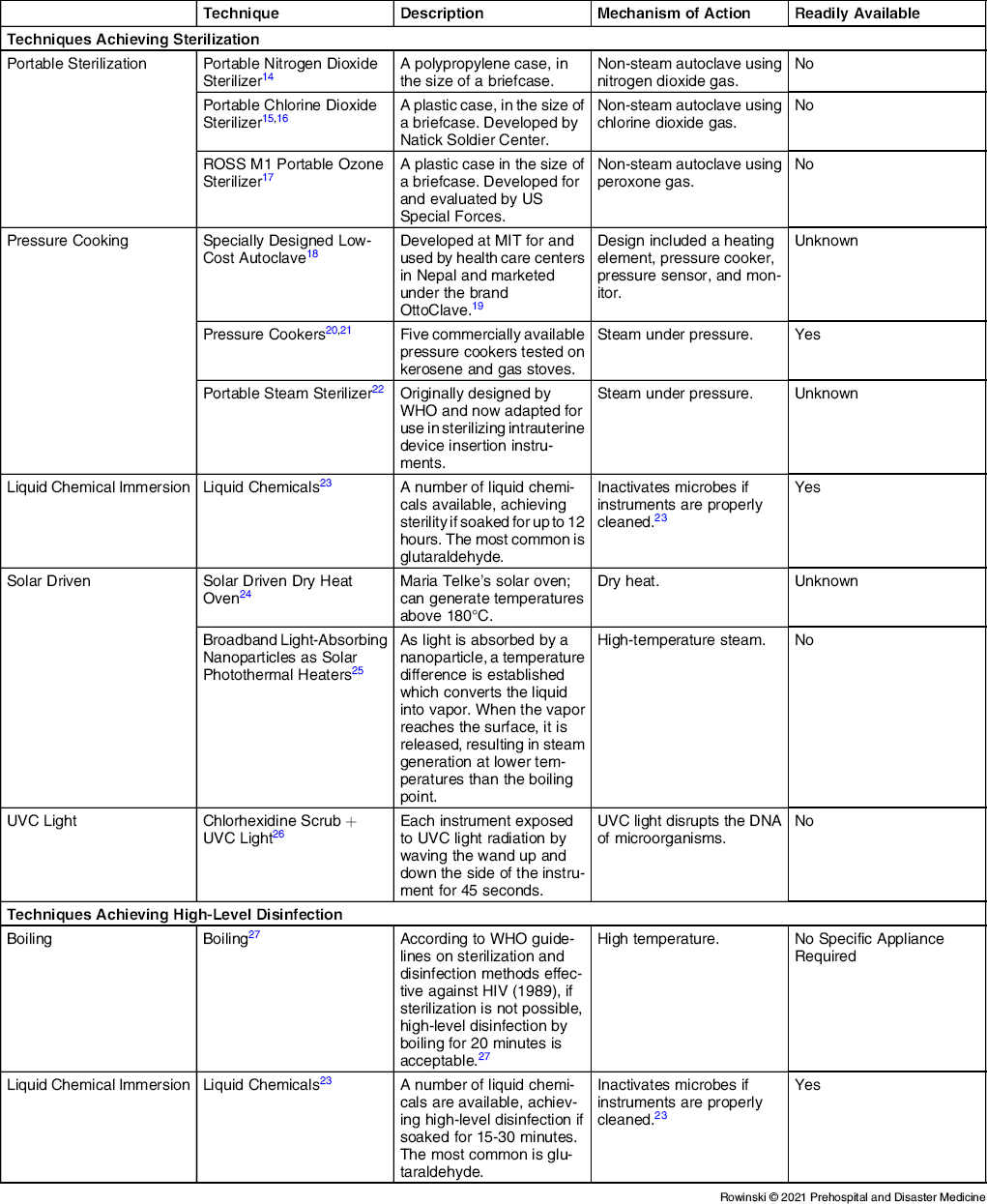
Abbreviation: UVC light, ultraviolet C light
Table 2. Techniques that are Portable and do not Require a Power Grid
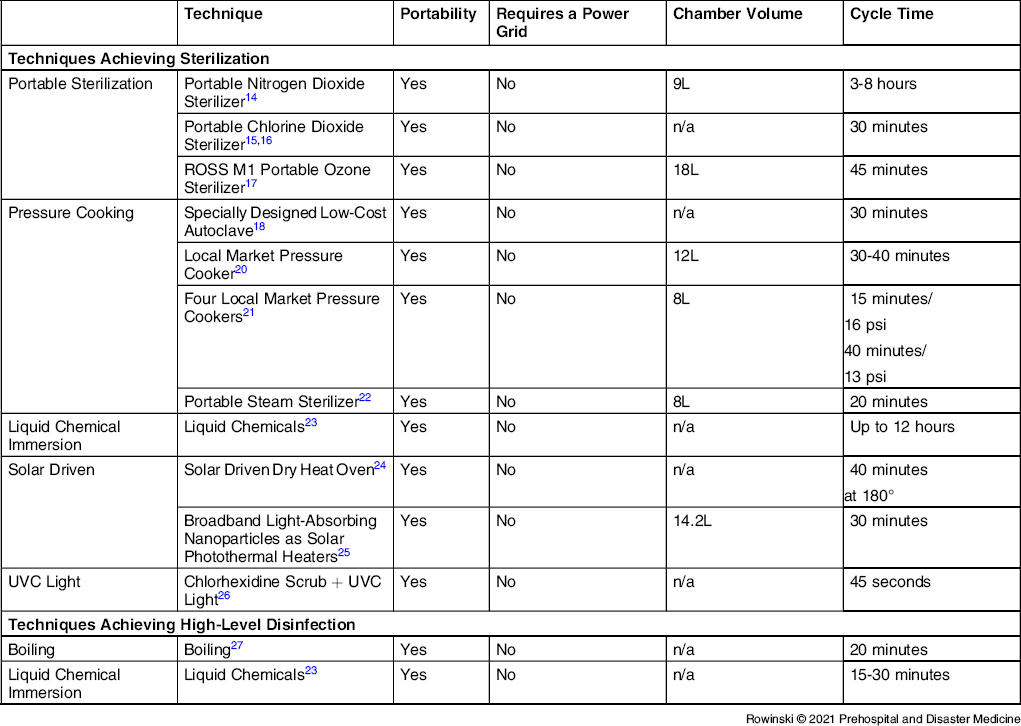
Note: Not applicable (n/a) - the information could not be found.
Abbreviations: PSI, pound-force per square inch (unit of pressure); UVC light, ultraviolet C light.
Results
The search rendered 401 articles that were screened for eligibility (Figure 1). Following screening, a total of 13 records matched the inclusion criteria. The 13 studies described six techniques, out of which three were easily available for use or purchase. The identified techniques achieving either sterilized or high-level disinfected instruments were pressure cooking, boiling, and liquid chemical immersion. They are all portable techniques and do not require a power grid.
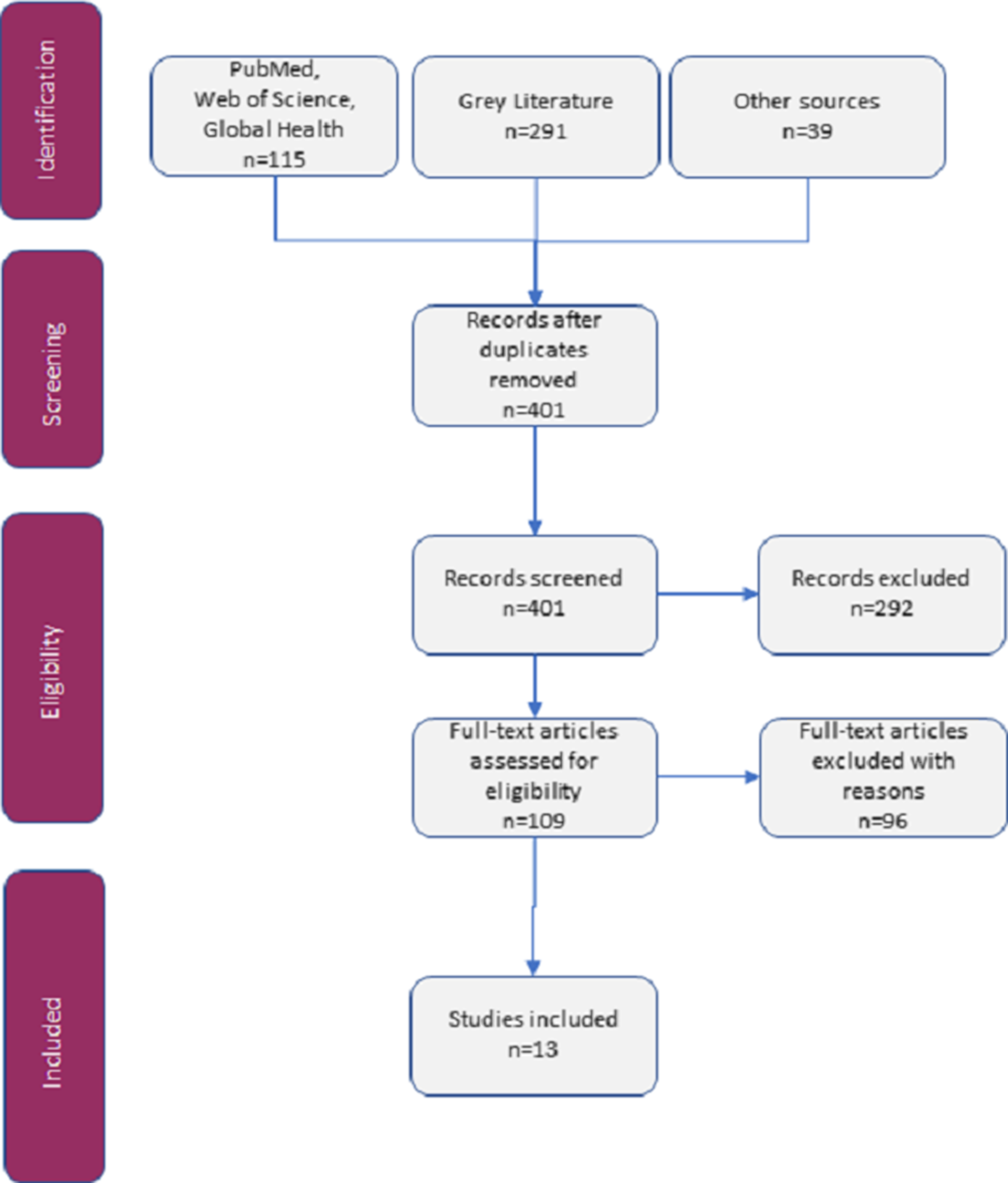
Figure 1. PRISMA-ScR Flowchart: Search Results.
Abbreviation: PRISMA-ScR, Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews.
The feasible and safe techniques identified in this study are presented in two tables and are shown as either achieving sterilized or high-level disinfected instruments. Table 1Reference Shomali, Opie and Avasthi14-27 contains a brief introduction of the techniques. The attributes of the techniques are presented in Table 2: portability, chamber volume, cycle time, and whether it requires a power grid or not.
Discussion
This scoping study found 13 articles presenting six techniques that can sufficiently decontaminate instruments for safe minor wound surgery and seem feasible to use in disaster settings. The identified techniques are easier to use and transport to remotely affected disaster areas compared to heavy and electricity-dependent autoclaves. It was found that safe alternatives to more resource-demanding autoclaves that are currently defined as minimum standards for EMT Type 1 are available.9 Pressure cooking, liquid chemicals, and boiling are the techniques that can easily be available for purchase or use today. Pressure cooking or boiling are the most favorable techniques, considering the potential toxicity and residue of liquid chemicals.Reference Rutala and Weber5,6 In addition, the WHO does not recommend liquid chemicals for sterilization. It is difficult to control the process and there is a risk of contamination during the rinse of residual chemicals before patient use.Reference Leaper and Edmiston4,6 Pressure cooking for 15-40 minutes achieves a higher level of decontamination than boiling for 20 minutes. A pressure cooker can be purchased on local markets while boiling is even easier to achieve with limited resources. In addition, pressure cooking and boiling are more sustainable than disposables and do not require transportation of large quantities of disposables in order to perform the number of wound surgeries often needed after a disaster.
According to Spaulding, high-level disinfected instruments are acceptable for instruments in contact with non-intact skin,Reference Leaper and Edmiston4,Reference Rutala and Weber5,7 but what are the safety implications of using high-level disinfected instead of sterilized instruments in a disaster setting? A systematic review focusing on the nature of wounds in disaster situations studied the most common organisms of infected wounds.Reference Wuthisuthimethawee, Lindquist and Sandler28 All of those pathogens are removed with high-level disinfection.Reference Rutala and Weber5 However, it remains undocumented to what extent high-level disinfected instruments could pose risks in the disaster setting as spores are not fully eliminated. Spores of concern in the disaster setting are Clostridium perfringens and tetani. Tetanus cases have been reported following natural disasters in areas with low tetanus vaccination coverage.Reference Pascapurnama, Murakami and Chagan-Yasutan29 While non-sterile instruments theoretically could spread tetanus, this has not been documented in practice. Poor early wound care is often complicated by more extensive infection and tissue necrosis, gangrene, sepsis, and mortality.30 Wound infections and complications including tetanus may develop if surgical cleaning and debridement is not adequately carried out. Spore transmission and infection could besides debridement be avoided (but not replaced) by preventive antibiotic regimes.Reference Wuthisuthimethawee, Lindquist and Sandler28 With this in mind, one should aim to autoclave instruments, but when this is not feasible, pressure cooking is an acceptable alternative if combined with tetanus prophylaxis.
Methodological Considerations/Limitations
The scoping review methodology enables searching both published and unpublished material, suitable in this area where important evidence might not yet have been published. Nonetheless, using such a broad search scope makes is challenging to establish boundaries. Therefore, a well-defined search strategy was developed. For this project, other methods could have been relevant to use, for example, a qualitative interview-based method. However, this would impose the risk of only increasing knowledge about current processes, not finding research on new developments. Another example is a systematic review which might have yielded a larger number of articles, yet carrying the risk of missing important evidence from unpublished sources. It would also have been interesting to compare these results with similar research, but no previous research in a similar area was found. In summary, a scoping study is particularly relevant to disciplines with emerging evidence such as this study.
Conclusion
This study found alternative safe, easily deployable, and feasible techniques to decontaminate surgical instruments for wound management in disaster settings, such as pressure cookers, boiling, and liquid chemicals. The study result suggests that current EMT Type 1 decontamination standards for minor wound surgery instruments could be adapted.
Conflicts of interest
The authors declare that they have no conflicting interests.






