Mental disorders are common and cause a huge social burden in most countries (World Bank, 1993; Reference UstunUstun, 1999). However, few psychiatric household surveys from Latin America have been published in peer-reviewed journals (Reference Canino, Bird and ShroutCanino et al, 1987; Reference Almeida-Filho, Mari and CoutinhoAlmeida-Filho et al, 1997). Chile appears to have one of the highest prevalence rates of psychiatric morbidity in primary care (Reference Araya, Wynn and LeonardAraya et al, 1994; Reference Ustun and SartoriusUstun & Sartorius, 1995; Reference ArayaAraya, 2000). There have been no previous studies that have attempted to estimate the prevalence of common mental disorder in a representative sample of residents of private households in a defined geographical area of Chile.
Research from developed and developing countries has shown that mental disorders are more common among the more socially disadvantaged, people who have previously been married and women (Reference Canino, Bird and ShroutCanino et al, 1987; Reference ChengCheng, 1988; Reference Chen, Wong and LeeChen et al, 1993; Reference Kessler, McGonagle and ZhaoKessler et al, 1994; Reference Almeida-Filho, Mari and CoutinhoAlmeida-Filho et al, 1997; Reference Jenkins, Lewis and BebbingtonJenkins et al, 1997).
This study used similar methodology to the National Psychiatric Morbidity survey of Great Britain (Reference Jenkins, Lewis and BebbingtonJenkins et al, 1997) and aimed:
-
(a) to estimate the prevalence of common neurotic symptoms and common psychiatric diagnoses among adults (aged 15 to 64 years) living in the capital of Chile, Santiago;
-
(b) to study the association between socio-demographic factors and the prevalence of common mental disorders (CMD).
METHOD
Sampling
The sampling frame used was the adult population (aged 16 to 64 years) living in private households in Greater Santiago, with a population of 3 237 286. The sampling design was carried out by the Chilean Institute of National Statistics. Greater Santiago is divided into 35 boroughs, each containing a variable number of sectors of about 200 households. The sampling strategy involved a three-stage design, which included all 35 boroughs, 252 sectors and 4693 households randomly selected with a probability proportional to the size of the sampling units. Sectors within the most affluent boroughs were oversampled to assist with comparisons between people from different socio-economic groups. Finally, one adult person for every household was chosen at random using the Kish method (Reference KishKish, 1965).
Interviewers were instructed to make at least four visits before declaring an address as lost. The only criterion for exclusion, apart from age, was that the person selected was unable to answer questions because of physical impediments or other personal reasons such as being away for a long period. Household size was defined as the number of people aged 16-64 years residing in that property who were eligible for interview. The selected households were not visited before initiation of the fieldwork, so it was not possible to ascertain a priori if any of the residents did not meet the criteria for inclusion in the study. (Further details of the sampling design or procedures are available from R.A. upon request.)
Several pilot studies were carried out to study the validity, reliability and feasibility of the questionnaires and the procedures to be used (Reference Lewis, Pelosi and ArayaLewis et al, 1992; Reference Araya, Wynn and LeonardAraya et al, 1994). One hundred and ninety-seven interviewers took part in the fieldwork. Each interviewer had to complete successfully a 3-day training course that included a reliability exercise marking three mock videotape interviews. Lay interviewers who did not achieve satisfactory agreement with most of the ratings on the video interviews were excluded from the fieldwork. Interviewers were closely supervised, with systematic revisiting of randomly chosen addresses to check the reliability of information. Data collection took place between October 1996 and April 1998.
Assessment
A detailed structured questionnaire covering socio-demographic factors, general health, use of health services, social support, psychiatric morbidity, and tobacco, alcohol and drug use was administered to each interviewee.
Common mental disorders
Common mental disorders (CMDs) were assessed using the Revised Clinical Interview Schedule (CIS—R) (Reference Lewis, Pelosi and ArayaLewis et al, 1992). This is a structured interview that has been fully standardised so that it can be administered by social survey interviewers. The English and Spanish versions of the CIS—R have been used extensively in primary care, occupational and community studies with good reliability and validity (Reference Lewis, Pelosi and ArayaLewis et al, 1992). Although the CIS—R enquires about 14 common neurotic symptoms present during the preceding week, it includes questions to identify the onset and duration of each episode, so allowing categorisation according to ICD—10 (World Health Organization, 1992) criteria for the most common disorders. Each one of the 14 symptoms is rated with an individual score. The total sum of these 14 scores can be used as a good indicator of the severity of a CMD. People scoring 12 or above on the CIS—R were regarded as suffering from a CMD (Reference Lewis, Pelosi and ArayaLewis et al, 1992). The following ICD—10 diagnoses were included: depressive episodes (F32.00, 32.01, 32.10, 32.11, 32.2); phobias (F40.00, 40.01, 40.01, F40.2); panic disorder (F41.1); generalised anxiety disorder (F41.1); and obsessive—compulsive disorder (F42). The diagnostic group of mixed anxiety and depressive disorder (F42.1) was not included because the ICD—10 does not provide an operational definition for research purposes. All those subjects who were above the threshold on the CIS—R, but failed to meet explicit ICD—10 criteria for a psychiatric diagnosis were grouped under a category denominated non-specific neurotic disorder, our equivalent of the mixed anxiety and depressive disorder. The prevalence rates of specific diagnoses cannot be added up because no attempt was made to establish a hierarchy of specific diagnoses. ICD—10 diagnoses were reached using computer-assisted algorithms developed by Meltzer et al (Reference Meltzer, Gill and Petticrew1995).
The CIS—R was chosen for several reasons. First, because it provides a measurement of the severity of symptoms including those with a sub-threshold intensity. Second, because it allows establishing ICD—10 diagnoses of the most common disorders. Third, because the period of time enquired about is reasonably short, diminishing the possibility of memory distortions about conditions experienced many years ago. Fourth, because the time taken to administer this interview is brief in comparison with other similar instruments. The administration of the CIS—R took an average of 30 minutes in this study. This is important because the length of an interview influences the reliability of the answers, the refusal rates, and the costs of the fieldwork. Lastly, because the validity and reliability of the CIS—R are comparable to the other commonly used structured interview, Composite International Diagnostic Interview (CIDI) (Reference Lewis, Pelosi and ArayaLewis et al, 1992; Reference Andrews and PetersAndrews & Peters, 1998; Reference Brugha, Bebbington and JenkinsBrugha et al, 2000).
Most of the questions used to measure other variables included in this study were derived from the National Psychiatric Morbidity Survey of Great Britain (NPMSGB; Reference Meltzer, Gill and PetticrewMeltzer et al, 1995). The Spanish questionnaires were translated and back-translated using a standard procedure recommended by the World Health Organization. These questionnaires are available upon request from R.A.
Family type
This variable is divided in the same five categories as in the NPMSGB. Couples were divided into two groups: those with or without children. The other three groups included were lone parents, ‘one-person families’, and respondents living with parents. Lone parents and couples with children could include children older than 16 years provided they were not married or they did not have children of their own in the same household. The ‘one-person family’ does not necessarily mean a person living alone because this person may be sharing premises with another family unit.
Social class
This variable was based on the household's main earner's occupation. We used the Chilean National Institute of Statistics scale to classify occupations according to: “prestige, power, economic income, and stability of occupation”. Four categories were included: (a) low-status and unstable occupation — involving manual non-specialised working freelance; (b) low-status but stable occupation — involving manual nonspecialised employees; (c) middle-status occupation — involving non-manual workers, with no professional qualifications; (d) high-status occupation — involving nonmanual professional or business people with prestigious posts. For those households where no one was currently employed, coding was based on the last occupation of the main earner.
Employment status
This was divided in four groups. The ‘employed’, including those people doing unpaid work for a family business. The ‘unemployed’ category, including those who were looking for a job and those individuals who were temporarily unemployed because of sickness or injury. The ‘economically inactive’ group, including housewives, students, the retired and those permanently unable to work because of illness or disability.
Analysis
This was approached in two different ways. Prevalence estimates for the adult population of Greater Santiago, Chile, were calculated adjusting for differential sampling and household size by using weights in the analysis. The interviewed sample was compared by age and gender with population projections based on the 1992 National Census results for Greater Santiago, and differences were used to further modify the weights. In view of the multi-stage random sampling design, 95% confidence intervals (95% CIs) were calculated from standard errors estimated using the survey commands of the computer program STATA (STATA, 1999), which takes into account the effect of the sampling strategy (stratification and clustering) and sampling weights.
Associations between CMD and socio-demographic factors of the respondents were examined using odd ratios. These ratios and their 95% CIs were calculated using logistic regression, both before and after adjustment for various socio-demographic factors. The analysis was performed using STATA survey commands adjusting for sampling design effects as well as differential sampling weights.
RESULTS
Sampling
Four thousand six hundred and ninety-three addresses were sampled, 393 of which were declared unusable because they were non-residential or contained only residents over the age of 65 years. So effectively 4300 private households were approached. Three thousand eight hundred and seventy subjects were interviewed, a response rate of exactly 90%. Reasons for refusals were varied but the most frequently mentioned were being ‘too busy’, ‘did not believe in surveys’ or ‘would not answer questions from strangers’. No one refused claiming ‘personal problems’. No other information was available from households that refused to participate.
Prevalence of common neurotic symptoms
The most common symptom was ‘worries’, with a prevalence of 43%. Other non-specific symptoms were also common, such as fatigue, irritability and sleep problems. Specific psychiatric symptoms such as depression, anxiety or phobias were less common. All symptoms were more common in women than in men. The prevalence by gender of the 14 neurotic symptoms included in the CIS-R is presented in Fig. 1.
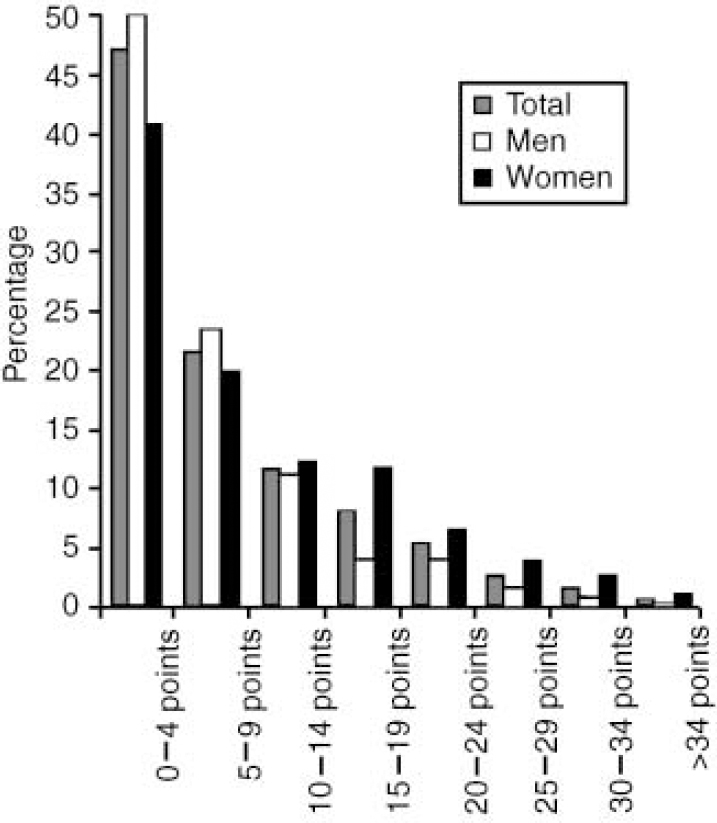
Fig. 1 Distribution of the Clinical Interview Schedule-Revised (CIS-R; Reference Lewis, Pelosi and ArayaLewis et al, 1992) scores by gender in Santiago, Chile.
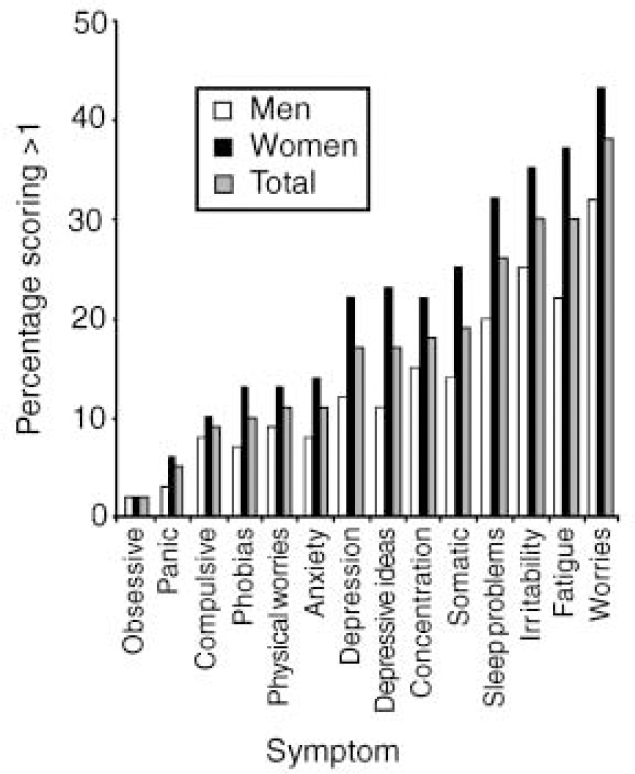
Fig. 2 Prevalence of psychiatric symptoms by gender in Santiago, Chile.
Prevalence of common mental disorders
The mean CIS-R total score was 7.78 (95% CI 7.45-8.30). The distribution of total CIS-R scores for each gender for the surveyed household sample can be seen in Fig. 1. Women were overrepresented compared with men in the high-score bands of the CIS-R.
The overall prevalence of CMD in Greater Santiago was 26.7% (95% CI 24.5-29.0), including both CIS-R cases and ICD-10 diagnoses. Approximately half of these individuals met ICD-10 criteria for at least one of the five diagnoses studied and the remaining half were cases of ‘non-specific neurosis’ (being a CIS-R case but not meeting criteria for any of the ICD-10 diagnoses included) (see Table 1). The 1-week prevalence of individuals scoring more than 12 points in the CIS-R was 25% (95% CI 22.8-27.3). The 1-week prevalence of individual ICD-10 psychiatric diagnoses is shown in Table 1. Depressive and generalised anxiety disorders were the most common ICD-10 diagnoses found in this study. Taken as a whole 9.5% (95% CI 8.1-10.9) of the people met criteria for either a diagnosis of ICD-10 depression or anxiety in the preceding week. Women had higher prevalence rates than men in all diagnostic categories with the exception of the least prevalent diagnosis of obsessive-compulsive disorder. Women had nearly twice the prevalence of ‘non-specific neurotic disorders’ and overall ICD-10 diagnoses.
Table 1 Percentage prevalence (95% CI1) of common mental conditions and diagnoses (ICD-10) in men and women of Greater Santiago, Chile2
| Women % (95% CI) | Men % (95% CI) | Total % (95% CI) | |
|---|---|---|---|
| Generalised anxiety disorder | 6.9 (5.6-8.5) | 3.2 (2.1-4.7) | 5.1 (4.2-6.2) |
| Depressive episode | 8.0 (6.5-9.8) | 2.7 (1.4-5.1) | 5.5 (4.5-6.7) |
| All phobias | 5.6 (4.4-7.0) | 2.9 (2.0-4.2) | 4.3 (3.5-5.3) |
| Obsessive—compulsive disorder | 1.1 (0.6-1.9) | 1.4 (1.0-1.9) | 1.3 (0.8-2.0) |
| Panic disorder | 1.5 (1.0-2.1) | 1.1 (0.5-2.3) | 1.3 (0.9-1.9) |
| Any of above ICD-10 diagnoses | 17.2 (15.2-19.4) | 8.2 (6.2-10.8) | 12.9 (11.6-14.5) |
| Non-specific neurotic disorder | 18.0 (15.9-20.3) | 9.1 (7.2-11.3) | 13.8 (12.1-15.5) |
| Any ICD-10 or non-specific disorder | 35.2 (32.3-38.2) | 17.3 (14.9-20.1) | 26.7 (24.5-29.0) |
Common mental disorders and socio-demographic correlates
Many socio-demographic factors were associated with a higher prevalence of CMD (see Tables 2 and 3). CMDs were significantly more prevalent among women than men and the strength of this association changed little after adjusting for other variables. Age was associated with the prevalence of CMD: the highest prevalence was found among those individuals aged 25-39 years and the lowest in the oldest group. These differences remained significant in the multivariate analysis (adjusted Wald test F=7.1, P=0.0001), after adjusting for other confounding variables.
Table 2 One-week prevalence of Clinical Interview Schedule—Revised (CIS-R) ‘cases’ by gender, age, marital status and family type

| Sample size | % Prevalence (95% CI)1 | Crude odds ratio (95% CI) | Adjusted odds ratio (95% CI)1,2 | |
|---|---|---|---|---|
| Gender | ||||
| Female | 1538 | 15.7 (15.6-15.7) | 1.00 | 1.00 |
| Male | 2332 | 33.6 (33.5-33.7) | 2.72 (2.19-3.38) | 2.37 (1.84-3.07) |
| Age (years) | ||||
| 16-24 | 884 | 22.4 (22.2-22.5) | 1.00 | 1.00 |
| 25-39 | 1416 | 29.5 (29.4-29.6) | 1.45 (1.10-1.92) | 1.41 (0.87-2.27) |
| 40-54 | 1038 | 23.1 (23.0-23.2) | 1.04 (0.79-1.38) | 0.82 (0.52-1.29) |
| 55-64 | 532 | 23.6 (23.4-23.9) | 1.07 (0.73-1.56) | 0.61 (0.37-1.01) |
| Marital status3 | ||||
| Never married | 1249 | 21.9 (21.8-22.0) | 1.00 | 1.00 |
| Married | 2059 | 24.3 (24.2-24.4) | 1.14 (0.85-1.54) | 1.08 (0.72-1.62) |
| Separated | 289 | 36.6 (36.1-37.1) | 2.06 (1.33-3.17) | 1.83 (1.14-2.92) |
| Widowed | 143 | 37.3 (36.4-38.3) | 2.12 (1.23-3.65) | 1.65 (0.88-3.11) |
| Cohabiting3 | 130 | 39.2 (38.3-40.1) | 2.30 (1.41-3.75) | 1.76 (1.00-3.09) |
| Family type | ||||
| Couple with children | 1597 | 24.8 (24.7-24.9) | 1.00 | 1.00 |
| Couple without children | 592 | 26.8 (26.7-27.0) | 1.11 (0.84-1.47) | 1.26 (0.94-1.68) |
| Young single | 888 | 20.7 (20.6-20.9) | 0.79 (0.56-1.12) | 0.93 (0.55-1.56) |
| Adult single | 425 | 23.6 (23.3-23.8) | 0.93 (0.65-1.35) | 1.06 (0.73-1.54) |
| Lone parent | 368 | 39.4 (39.1-39.7) | 1.97 (1.44-2.70) | 1.61 (1.12-2.32) |
Table 3 One-week prevalence of Clinical Interview Schedule—Revised (CIS—R) ‘cases’ by education, social class and employment status
| Sample size | % Prevalence (95% CI)1 | Crude odds ratio (95% CI) | Adjusted odds ratio (95% CI)1,2 | |
|---|---|---|---|---|
| Educational level3 | ||||
| Higher | 1314 | 14.6 (14.5-14.6) | 1.00 | 1.00 |
| Secondary | 1881 | 24.3 (24.2-24.3) | 1.88 (1.47-2.40) | 1.34 (1.01-1.78) |
| Primary | 669 | 37.0 (36.8-37.2) | 3.44 (2.51-4.71) | 2.56 (1.71-3.84) |
| Social class4 | ||||
| Highest | 975 | 12.6 (12.5-12.7) | 1.00 | 1.00 |
| Middle | 1403 | 23.4 (23.3-23.5) | 2.12 (1.54-2.91) | 1.48 (1.05-2.09) |
| Low | 1180 | 28.6 (28.5-28.7) | 2.77 (2.02-3.79) | 1.65 (1.11-2.44) |
| Unstable | 297 | 34.7 (34.3-35.1) | 3.67 (2.47-5.46) | 1.80 (1.15-2.83) |
| Employment status4 | ||||
| Full-time employed | 1822 | 19.5 (19.4-19.5) | 1.00 | 1.00 |
| Economically inactive | 1602 | 29.2 (29.1-29.2) | 1.70 (1.35-2.15) | 1.30 (0.95-1.78) |
| Self-employed | 286 | 31.9 (31.4-32.9) | 1.94 (1.20-3.13) | 1.46 (0.87-2.44) |
| Unemployed | 121 | 37.7 (36.6-38.8) | 2.50 (1.46-4.28) | 2.29 (1.27-4.11) |
Respondents who had been separated or widowed were more likely to be a case of CMD than single individuals. However, only those individuals who were separated showed a statistically significant (P < 0.05) association with a higher prevalence of CMD, after adjustment for other variables. Lone parents with children had increased rates of psychiatric morbidity, an association that persisted after adjusting for other potential confounding variables.
Both education level (χ2=14.07, d.f.=3, P<0.0001) and social class according to occupation (χ2=27.68, d.f.=3, P<0.0001) had linear dose-response associations with the prevalence of CMD. Those in the most disadvantaged groups with less education and in lower social class had a higher prevalence of CMD. Although these gradients were reduced after adjustment, they remained statistically significant. Although all employment status groups had higher prevalence rates than the full-time employed, these associations were not statistically significant after adjustment, with the exception of being unemployed.
DISCUSSION
This large and comprehensive study provides an estimate of the prevalence of CMDs for the private household population of Greater Santiago, Chile, based on a methodology similar to that used in the Office of Population Censuses and Surveys National Psychiatric Morbidity Survey (Reference Jenkins, Lewis and BebbingtonJenkins et al, 1997) thus allowing comparisons with urban locations in Great Britain.
A quarter of the adult residents of Greater Santiago could be considered to be suffering from a common neurotic disorder, half of whom met criteria for an ICD-10 psychiatric diagnosis. Of the neurotic disorders considered, the two most common ICD-10 diagnoses were depressive and generalised anxiety disorders. Women and the most socially disadvantaged groups had a higher prevalence of CMD.
Strengths and weaknesses of this study
This study used a structured psychiatric interview (CIS-R) administered to a representative sample of the adult population residing in private households in Santiago, capital of Chile. Experienced lay interviewers underwent an intensive training, including several tests of reliability, and were closely supervised during the fieldwork. Studies of this design and scale are difficult to conduct outside Western market economies. Despite these strengths, this was a cross-sectional study involving only one city, thus it would be unwise to generalise our results to the rest of the country or to reach conclusions about aetiological relationships. However, it is still possible to identify groups with poor health and identify strong associations that might inform future research on causal relationships.
The validity of information collected using clinical interviews administered by lay people has been questioned (Reference Brugha, Bebbington and JenkinsBrugha et al, 1999), but we agree with other researchers (Reference Wittchen, Ustun and KesslerWittchen et al, 1999) in thinking that on balance this method represents the most cost-efficient way of undertaking community surveys of this size. From a practical perspective, it is difficult to conceive of a study over a large geographical area involving several thousand interviews that could be administered by psychiatrists in settings with a shortage of these specialists. We are not aware of any survey of the house-hold population that has achieved more than 1000 structured interviews administered by psychiatrists.
In the absence of gold standards one can only assess the reliability of measurement. Structured interviews administered by lay people are as reliable, if not more reliable, than interviews administered by psychiatrists (Reference Lewis, Pelosi and ArayaLewis et al, 1992; Reference Andrews and PetersAndrews & Peters, 1998; Reference Wittchen, Ustun and KesslerWittchen et al, 1999). By using this methodology we can be confident that everyone in the study was asked the same questions and this aids comparison within and between studies.
Prevalence of common mental symptoms
Non-specific symptoms such as worries, irritability, fatigue and sleep problems were by far the most frequent both in the Chilean and the British urban samples. Specific psychological symptoms such as depressed or anxious mood, essentials for reaching ICD-10 diagnoses, were much less common in both countries. In the Chilean survey the most common reported symptom was ‘worries’ (Chile, 38%; GB urban, 21%) whereas ‘fatigue’ was the most common symptom in Great Britain (GB urban, 28%; Chile, 30%). The high prevalence of these non-specific symptoms might help to explain the large proportion of people with high scores in the CIS-R who did not meet criteria for an ICD-10 diagnosis.
All symptoms were more frequent in the Chilean than in the British sample. In both countries all symptoms were more prevalent in women than men. In addition, this study contributed to the growing body of research showing that people from many non-Western countries do report psychological symptoms when asked specifically about them. Notwithstanding this, somatic complaints and worries about physical health were more common in Chile than in urban areas of Great Britain: 19% v. 8% and 11% v. 5%, respectively.
Prevalence of CMDs
Prevalence rates of common neurotic disorders among adult residents from the Greater Santiago area (27%) were higher than those found in urban areas of Great Britain (18%). However, approximately the same proportion of ICD-10 diagnosable conditions and non-specific neurotic disorders were present in both samples. It can be argued that non-specific neurotic disorders do not represent ‘clinically meaningful’ morbidity. However, previous studies have demonstrated the public health importance of sub-threshold and mild psychiatric disorders (Reference Broadhead, Blazer and GeorgeBroadhead et al, 1990). As far as diagnoses are concerned, higher prevalence rates were found for the diagnoses of depressive disorders and phobias in the Chilean compared with the UK sample: 5.5% v. 2.6% and 4.3% v. 2.1%, respectively.
After a literature search covering the period from 1985 up to the present, only two Latin American household surveys of psychiatric morbidity that had used a structured interview and a probabilistic sampling design were found in English peer-reviewed journals (Reference Canino, Bird and ShroutCanino et al, 1987; Reference Almeida-Filho, Mari and CoutinhoAlmeida-Filho et al, 1997). Other household surveys have been carried out but do not meet the criteria previously outlined.
Comparing our results with these two surveys is difficult because of methodological differences. The Puerto Rican study (Reference Canino, Bird and ShroutCanino et al, 1987) utilised the Diagnostic Interview Schedule (DIS) with an island-wide probability sample and calculated 6-month prevalence estimates of DSM-III (American Psychiatric Association, 1980) diagnoses. The overall prevalence found in Puerto Rico is not comparable with our study because it includes psychotic disorders and substance misuse. However, rates of DSM-III major depression (3%) and anxiety disorders (7.5%) were similar to our study. However, it needs to be borne in mind that our study involved a much shorter prevalence period.
The Brazilian study (Reference Almeida-Filho, Mari and CoutinhoAlmeida-Filho et al, 1997) was a two-stage design of population samples from three major cities. A subsample of individuals had diagnostic interviews using the Brazilian version of the DSM-III Symptom Check-List administered by psychiatrists. Comparisons with this study are even more cumbersome because their 1-year prevalence estimates were adjusted according to the ‘potential need-for-treatment’ judged by the interviewing psychiatrist. The most common diagnoses were anxiety and phobic disorders, with 1-year prevalence estimates varying between 7% to 12%.
CMD and socio-demographic correlates
Most of the published research from the developing, as well as developed, countries has found that women, people who had been previously married and people belonging to the most socially disadvantaged groups (education, income, and social class) have a much higher prevalence of CMD. This study replicated these findings, showing a similar profile of associations between socio-economic variables and CMD as in Great Britain (Reference Jenkins, Lewis and BebbingtonJenkins et al, 1997) and Puerto Rico (Reference Canino, Bird and ShroutCanino et al, 1987). Women, divorced or separated individuals, lone parents, those people with less education or belonging to lower social class groups and the unemployed all showed higher prevalence rates of common neurotic disorders in both countries.
The mild but significant association between young adulthood (age 25-39 years) and the presence of a CMD found in the Chilean study persisted after adjusting for other variables. This association was not found in the British study, which showed a trend for the prevalence of mental disorders to decrease with greater age - this is similar to the trends found in the Chilean study for other age bands. In keeping with our results, some studies have found an increased prevalence of CMD in younger cohorts, with a decrease with age in other groups (Reference Kessler, McGonagle and ZhaoKessler et al, 1994). However, other studies have found a rise in the prevalence of CMD with increasing age (Reference Canino, Bird and ShroutCanino et al, 1987). The higher prevalence of CMD among young adults in Chile and other countries deserves further investigation because this age group plays a vital role in any productive economy and these individuals could be experiencing more distress as a result of all the pressures of living in emerging economies.
On the basis of our study we estimate that about 390 134 people met criteria for an ICD-10 psychiatric diagnosis in Santiago, Chile. If only half of this group needed treatment at an average annual cost of US$150, this would total US$74 million per annum. Bearing in mind that the entire Chilean health budget was about US$1500 million in 1997 and that approximately 10% of this sum went into mental health, half of the mental health budget would have to be spent on the treatment of these common neurotic disorders. Based on this example it is clear that establishing priorities becomes an essential first step in dealing with this important disease burden. Unfortunately, local data on the cost and benefits of treating common psychiatric disorders are scarce. Information derived from community surveys should help decision makers know how best to allocate scarce resources.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ High levels of clinically meaningful morbidity were found in this Latin American city.
-
▪ Psychological symptoms were more common in Santiago than in urban settings in Great Britain.
-
▪ The most socially disadvantaged groups had the highest prevalence of common mental disorders.
LIMITATIONS
-
▪ It is a cross-sectional design, so it is difficult to draw causal implications.
-
▪ This study is restricted to urban locations.
-
▪ Psychotic morbidity was not assessed.
ACKNOWLEDGEMENT
We thank all the interviewers who participated in this study.








eLetters
No eLetters have been published for this article.