Cyproheptadine, or glutodine, is a first-generation anti-histaminic, that has been on market since the 1960s. It has a unique pharmacologic portfolio that speaks to the idea of a pluripotent molecule beyond an anti-allergic agent which can expand its therapeutic potential to address a multitude of psychiatric indications (Table 1). That said, it should be borne in mind that the level of evidence supporting the use of cyproheptadine in these off-label indications is highly variable, and, hence, sound clinical judgement is necessary for its proper use and placement in real-life psychiatric practice and psychopharmacotherapy algorithms. Here, we briefly touch on some of these indications with helpful some clinical tips and caveats.
Table 1. Cyproheptadine Uses
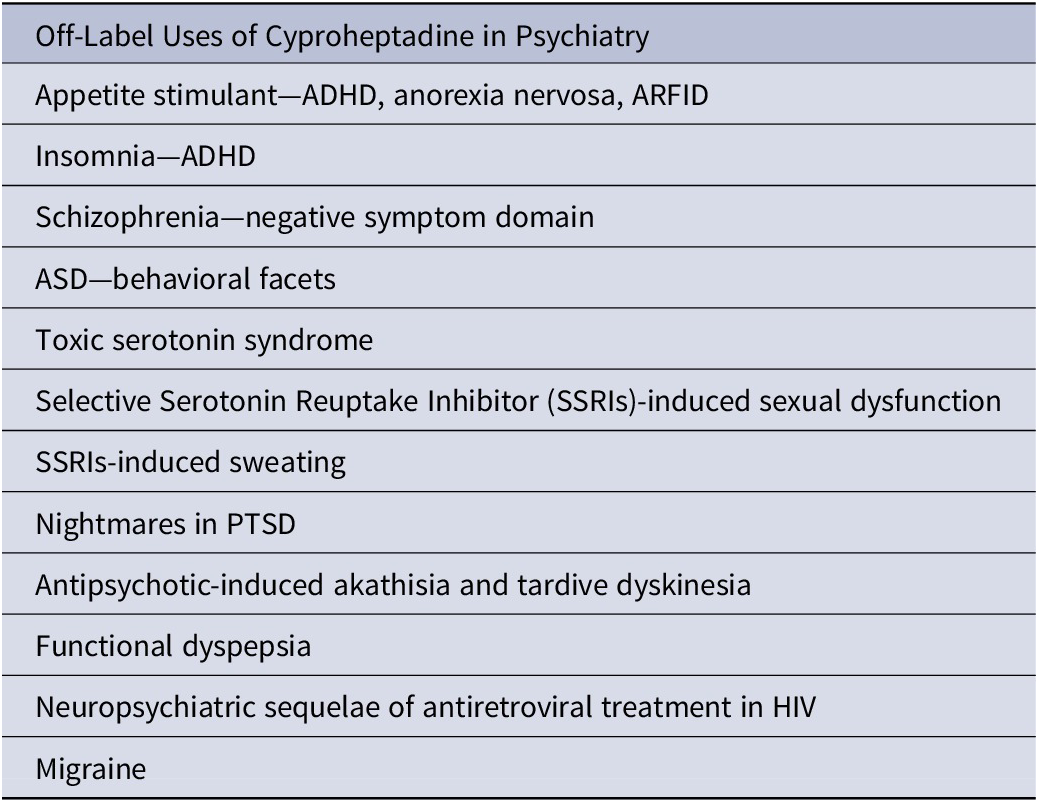
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; ARFID, avoidant/restrictive food intake disorder; ASD, autism spectrum disorder; PTSD, posttraumatic stress disorder.
Cyproheptadine is H1 histaminergic, M1 muscarinic, 5HT2A serotonergic, and reportedly calcium channel blocker. No significant kinetic interactions are expected. Dosing depends on indication for appetite stimulation: 2 mg × 4 increased to a target of 8 mg × 4 over 3 weeks; serotonin syndrome: 12 mg × 1, then 2 mg q 2 hours till response with a max. 32 mg/day; nightmares: 4 mg qhs but can go up to 24 mg qhs; female anorgasmia: 4–12 mg PRN 1–2 hours before coitus.
Appetite Stimulant
Due to H1 blockade, cyproheptadine can increase the appetite, hence the alternate name glutodine. Anticholinergic actions might be contributory too. Cyproheptadine has been used to address stimulant-related appetite suppression in children with attention-deficit/hyperactivity disorder (ADHD),Reference Naguy 1 although anticholinergic actions sound counterintuitive as it might negatively impact cognition. Paradoxical aggression has been reported in a 5-year-old boy treated with cyproheptadine given the causal link between serotonin and aggression (serotonin inhibits aggression).Reference Strayhorn 2 Due to anti-serotonergic properties, cyproheptadine was also reported to induce obsessive–compulsive symptoms of religious and sexual themes (with a fundamental 5HT dysregulation) in a preschool girl.Reference Kaya, Suleyman and Coskun 3 Moreover, cyproheptadine has been successfully trialled for weight gain in restrictive anorexia nervosa,Reference Miniati, Mauri and Ciberti 4 although olanzapine has sounder evidence-base. Similarly, cyproheptadine can be a viable option in avoidant/restrictive food intake disorder (ARFID).Reference Naguy, Roshdy and Al-Mutairi 5
Insomnia
Cyproheptadine has been used to tackle stimulant-induced insomnia in ADHD.Reference Naguy 6 Clonidine or melatonin can be used in lieu without impairing cognitive functions. Use of antihistaminics for insomnia is generally discouraged as tachyphylaxis tends to develop soon (as early as day 3).
Autism Spectrum Disorder (ASD)
Hyperserotonaemia has been reported in 40% of ASD population.Reference Naguy, Ali and Elsori 7 A positive 8-week randomized controlled trial (RCT) has attested to the superiority of combined anti-serotonergic cyproheptadine with haloperidol over haloperidol alone for behavioral dyscontrol in ASD with no difference in extrapyramidal syndromes (EPS) or side effects.Reference Akhondzadeh, Erfani and Mohammadi 8
Nightmares in PTSD
Cyproheptadine can improve sleep architecture and REM (rapid eye movement) sleep pattern. It has been used to address distressing nightmares in patients with posttraumatic stress disorder (PTSD) in a dose range of 4 to 24 mg/day.Reference Hammer, Robert and Frueh 9 Prazosin and possibly gabapentin remain better alternatives.
SSRIs-Related Sexual Dysfunction
Given 5HT2A antagonistic actions, cyproheptadine has been used as an antidote to the commonly encountered SSRIs-induced sexual dysfunction including female anorgasmia.Reference Stimmel and Gutierrez 10 Add-on bupropion, mirtazapine, gingko biloba, or phosphodiesterase PD-5 inhibitors (eg, sildenafil) are better options. It behooves clinicians to be vigilant and mindful to the fact that cyproheptadine, by virtue of anti-serotonergic actions, can nullify antidepressant actions with a resultant dynamic failure and treatment “pseudo-resistance.”
SSRIs-Related Sweating
Diaphoresis (hyperhiderosis), which can be socially embarrassing, has been reported to affect 1 in 5 persons on antidepressants. Via central antiserotonergic actions, cyproheptadine has been reported to help with diaphoresis.Reference Marcy and Britton 11 Other options include benzotropine, mirtazapine or aripiprazole.
Akathisia
Neurobiological underpinnings of akathisia include D2 blockade, 5HT2A overstimulation, GABA deficiency, M1 Cholinergic overactivity, and, noradrenergic overactivity.Reference Naguy 12 Cyproheptadine, by blocking 5HT2A and M1 receptors can be an attractive option for antipsychotic-induced akathisia.Reference Lohr, Eidt and Alfaraj 13 Antidepressants, mirtazapine and mianserin, have been used similarly. β blockers and benzodiazepines remain first-line options, though. Of related interest, cyproheptadine was reported as a treatment option for tardive dyskinesia.Reference Kurata, Hosokawa and Koshino 14
Serotonin Syndrome
Cyproheptadine has been deployed as antidote in toxic serotonin syndrome. Case reports abound in literature.Reference Huska, Catalano and Catalano 15 Medetomidine, benzodiazepines, or chlorpromazine are alternative symptomatic options besides stopping the offending agent. Similarly, cyproheptadine has been successfully used in serotonin-producing carcinoid tumor.
Schizophrenia
Add-on cyproheptadine to haloperidol has been demonstrated in one RCT to outperform haloperidol with placebo in treatment of negative symptom domain.Reference Akhondzadeh, Mohammadi and Amini-Nooshabadi 16 Alleviation of EPS could be contributory as shown in another 6-week RCT.Reference Lee, Song and Kim 17 A case report of a 66-year-old female patient, who developed clozapine-induced agranulocytosis after 10 weeks of clozapine treatment was subsequently successfully treated with a combination of loxapine and cyproheptadine. This combination is thought to mimic the pharmacological profile of clozapine, rendering it as a possible alternative to traditional clozapine treatment.Reference Aboueid and McCarthy 18
Abdominal Migraine and Cyclic Vomiting in Children
As serotonin is highly expressed in gut, cyproheptadine has been successfully reported to mitigate functional dyspepsia and irritable bowel syndrome. Use of cyproheptadine in migraineReference Silberstein 19 is akin to the use of pizotifen, another antihistaminic commonly prescribed for migraine prophylaxis (and appetite stimulation as well).
Neuropsychiatric Sequelae of Efavirenz in Patients with AIDS
A positive RCT has attested to efficacy of cyproheptadine to mitigate neuropsychiatric sequelae of the antiretroviral agent, efavirenz in HIV-positive patients, which is pretty common in 50% of cases.Reference Dabaghzadeh, Ghaeli and Khalili 20 Use of cyproheptadine can be advantageous here to help with cachexia as well.
This list is by no means all-inclusive. As data accrues, therapeutic potential of cyproheptadine expands. Definitely, large, well-conducted trials are sorely needed to define the real place of cyproheptadine in psychiatric pharmacopeia.
Disclosures
The authors have no competing interests or financial affiliations.



