Introduction
Thirteen to nineteen percent of new mothers experience postpartum depression and one out of 10 women with a child under age 18 experience at least one episode of major depression (Ertel et al., Reference Ertel, Rich-Edwards and Koenen2011; O’Hara & McCabe, Reference O’Hara and McCabe2013; O’Hara & Swain, Reference O’Hara and Swain1996). Elevated maternal depressive symptoms (MDS) may increase health risks for both mothers and their children (Goodman et al., Reference Goodman, Rouse, Connell, Broth, Hall and Heyward2011; O’Hara & McCabe, Reference O’Hara and McCabe2013). Women with heightened depressive symptoms often face challenges in their daily functioning within the personal and social contexts. MDS are associated with increased negative emotionality and cognitive biases towards others, and impairment in the ability to recognize affective cues (Dietz et al., Reference Dietz, Jennings, Kelley and Marshal2009; Flanagan et al., Reference Flanagan, White and Carter2011; Stein et al., Reference Stein, Arteche, Lehtonen, Craske, Harvey, Counsell and Murray2010). In the family context, even at subclinical levels, MDS are associated with negative parenting behaviors, including decreased sensitivity or increased hostility during mother-child interactions (Dietz et al., Reference Dietz, Jennings, Kelley and Marshal2009; Feldman et al., Reference Feldman, Granat, Pariente, Kanety, Kuint and Gilboa-Schechtman2009; Ku & Feng, Reference Ku and Feng2023; Lovejoy et al., Reference Lovejoy, Graczyk, O’Hare and Neuma2000; Wu et al., Reference Wu, Feng, Hooper and Ku2017). In general, MDS typically decrease as children age (Ku & Feng, Reference Ku and Feng2023; Wu et al., Reference Wu, Selig, Roberts and Steele2011). There is emerging evidence for heterogeneity in both the severity and stability of long-term MDS (e.g., Ahmed et al., Reference Ahmed, Bowen, Feng and Muhajarine2019; Chow et al., Reference Chow, Dharma, Chen, Mandhane, Turvey, Elliott, Becker, Subbarao, Sears and Kozyrskyj2019; Denckla et al., Reference Denckla, Mancini, Consedine, Milanovic, Basu, Seedat, Spies, Henderson, Bonanno and Koenen2018; Putnick et al., Reference Putnick, Sundaram, Bell, Ghassabian, Goldstein, Robinson, Vafai, Gilman and Yeung2020). Yet, there is limited understanding of MDS trajectories among underserved populations, such as mothers living in poverty in rural areas (Wikman et al., Reference Wikman, Axfors, Iliadis, Cox, Fransson and Skalkidou2020), who may be vulnerable to experiencing elevated postpartum MDS (Goyal et al., Reference Goyal, Gay and Lee2010; Halbreich & Karkun, Reference Halbreich and Karkun2006). Therefore, the current study aimed to identify distinct trajectories of MDS over the first five years using a sample of low-income mothers living in rural areas in the U.S. Importantly, we also examined the roles of various early social contexts in developing MDS trajectories with a focus on socioeconomic status (SES; both objective and subjective measures), perceived neighborhood safety, and interpersonal contexts (i.e., social support and intimate partner violence [IPV]).
Heterogeneity in longitudinal trajectories of depressive symptoms among rural, low-income mothers
Empirical studies have identified distinct trajectories of MDS from as early as the second trimester of pregnancy through early childhood, using both community samples (e.g., Choe et al., Reference Choe, McDonough, Sameroff and Lawrence2020) and population-based samples in Western, industrialized countries, among mothers with diverse socioeconomic backgrounds (e.g., Ahmed et al., Reference Ahmed, Bowen, Feng and Muhajarine2019; Campbell et al., Reference Campbell, Matestic, von Stauffenberg, Mohan and Kirchner2007; Denckla et al., Reference Denckla, Mancini, Consedine, Milanovic, Basu, Seedat, Spies, Henderson, Bonanno and Koenen2018; Kiviruusu et al., Reference Kiviruusu, Pietikäinen, Kylliäinen, Pölkki, Saarenpää-Heikkilä, Marttunen, Paunio and Paavonen2020; Putnick et al., 2018; Wikman et al., Reference Wikman, Axfors, Iliadis, Cox, Fransson and Skalkidou2020). Across studies, the most commonly observed trajectories of MDS from infancy through early childhood include the following trajectories: (a) minimal symptoms over time, with the majority of mothers typically classified in this trajectory; (b) increasing over time; (c) decreasing over time; and (d) chronically high. For example, using a population-based sample of 4,866 mothers from New York State, Putnick et al. (Reference Putnick, Sundaram, Bell, Ghassabian, Goldstein, Robinson, Vafai, Gilman and Yeung2020) identified four trajectories of MDS from 4 to 36 months, including low-stable, low-increasing, medium-decreasing, and high-persistent trajectories. Moreover, using 615 high-SES mothers in Canada, Ahmed et al. (Reference Ahmed, Bowen, Feng and Muhajarine2019) identified four trajectories of MDS from mid-pregnancy through 5 years, including low-stable, moderate-stable, moderate-increasing, and high-decreasing. In contrast to other work (e.g., Campbell et al., Reference Campbell, Matestic, von Stauffenberg, Mohan and Kirchner2007; Putnick et al., Reference Putnick, Sundaram, Bell, Ghassabian, Goldstein, Robinson, Vafai, Gilman and Yeung2020), a chronically high trajectory was not identified among higher SES mothers in this sample, suggesting that additional risk factors associated with low-SES may influence trajectories of MDS.
While individuals in poverty are more likely to experience depression than those who are not in poverty (Pratt & Brody, Reference Pratt and Brody2008), a line of research with low-income mothers suggests that heterogenous patters of changes in MDS may also exist among high-risk populations (Christensen et al., Reference Christensen, Stuart, Perry and Le2011; Guyon-Harris et al., Reference Guyon-Harris, Huth-Bocks, Lauterbach and Janisse2016; Mora et al., Reference Mora, Bennett, Elo, Mathew, Coyne and Culhane2009). Using a community sample of 121 low-income, racially diverse mothers, Guyon-Harris et al. (Reference Guyon-Harris, Huth-Bocks, Lauterbach and Janisse2016) identified four trajectories across the third trimester of pregnancy, 3 months, 1-year, and 2-year postpartum, including the low-decreasing (47.5 %), stable-low (22.5 %), stable-moderate (21.7 %), and increasing (8.3%). Using a large sample of low-income mothers (n = 1,735) from urban areas of the U.S. Mora and colleagues (2009) identified five MDS trajectories from 15 weeks before giving birth through 25-month postpartum (i.e., never [71%], late [7%], antepartum [6%], postpartum [9%], chronic [7%] trajectories). It appears that a large percentage of low-income mothers exhibit minimal to low symptoms over the postpartum period and early childhood of their child’s life.
In addition, poverty in rural areas presents unique challenges to mothers with young children. Rural low-income mothers often encounter challenges related to unsafe neighborhoods, food insecurity, inadequate housing, and limited access to childcare (Bauer & Dolan, Reference Bauer and Dolan2011). There have been mixed findings regarding rural mothers’ experience vs. urban. It has been documented that compared to urban low-income mothers living in the U.S., rural low-income mothers are greater risk of experiencing elevated depressive symptoms in early childhood (Mollard et al., Reference Mollard, Hudson, Ford and Pullen2016). In contrast, more recent evidence suggests that rural low-income mothers are not necessarily at high risk of experiencing elevated/clinical levels of depressive symptoms. Instead, they tend to show differences in the patterns of depressive symptoms (e.g., Gueron-Sala et al., Reference Gueron-Sela, Camerota, Willoughby, Vernon-Feagans and Cox2018). Using the dataset used in the current study, Gueron-Sale et al. (Reference Gueron-Sela, Camerota, Willoughby, Vernon-Feagans and Cox2018) reported that only six to nine percentage of the mothers exhibited clinical depression between 6 and 15-month postpartum. However, to our understanding, only a few studies appear to have investigated rural mothers’ depression using a group-based approach (Familiar et al., Reference Familiar, Sikorskii, Murray, Ruisenor-Escudero, Nakasujja, Korneffel, Boivin and Bass2019; Lee & Park, Reference Lee and Park2020). Familiar et al. (Reference Familiar, Sikorskii, Murray, Ruisenor-Escudero, Nakasujja, Korneffel, Boivin and Bass2019) found three trajectories among rural Uganda mothers with HIV (i.e., stable-low [53%], moderate-subclinical [39%], and chronic-high [8%]). Using a community sample, Sano et al. (Reference Sano, Bolkan and Mammen2020) found two trajectories, the constantly depressed (n = 11) and constantly improved (n = 21) trajectories, over three years among rural, low-income mothers who had a child at the age of 13 or below. As such, examining distinct trajectories of MDS among rural lower-SES mothers is needed, which may expand our understanding of risk and resilience factors in those most vulnerable to experiencing adverse health outcomes.
The conditions in which people are born, grow, live, work, and age and the fundamental drivers of these conditions are defined as the social determinants of health (SDH; Braveman & Gottlieb, Reference Braveman and Gottlieb2014). Decades of research on the SDH have documented that contextual factors related to socioeconomic SES may influence individuals’ health outcomes, either directly or indirectly (Adler & Stewart, Reference Adler and Stewart2010). The potential determinants include not only individuals’ education and income, but also individuals’ perception on their SES, neighborhood environments, and social support. In supportive of the SDH framework, empirical work on MDS also suggests that MDS may be affected by various factors at the interpersonal, family, and neighborhood levels (e.g., Goodman et al., Reference Goodman, Huang, Schafer-Kalkhoff and Adler2007). In this way, each of the predictors included in the current analysis represent mothers’ meaningful experiences that can affect their depressive symptoms.
In line with the SDH, studies examining trajectories of MDS in early childhood have collectively indicated that low objective SES (e.g., education, income) and inadequate interpersonal relationships (e.g., lack of social support, high levels of IPV) are reliably associated with high-risk trajectories, such as increasing and chronically high trajectories (e.g., Campbell et al., Reference Campbell, Matestic, von Stauffenberg, Mohan and Kirchner2007; Choe et al., Reference Choe, McDonough, Sameroff and Lawrence2020; Denckla et al., Reference Denckla, Mancini, Consedine, Milanovic, Basu, Seedat, Spies, Henderson, Bonanno and Koenen2018; Giallo et al., Reference Giallo, Pilkington, McDonald, Gartland, Woolhouse and Brown2017). However, recent evidence suggests that subjective measures of SES, which refers individuals’ evaluation of their own social status and/or financial and economic power are also an important factor predicting individuals’ psychological symptoms, including depression (Assari et al., Reference Assari, Smith, Mistry, Farokhnia and Bazargan2019; Baker et al., Reference Baker, Huang, Liu and Battista2021; Kim & Radoias, Reference Kim and Radoias2021). In addition, while broader contexts (e.g., neighborhood environments) may affect MDS (Huang et al., Reference Huang, King and McAtee2018), little is known about how these contexts are associated with longitudinal trajectories of MDS. Given the importance of proximal and distal social determinants of MDS, the current study sought to extend prior research to examine the unique roles of objective and subjective SES, neighborhood environment, social support, and IPV in predicting trajectories of MDS in the first five years of their child’s life among rural, low-income mothers.
Objective versus subjective measures of socioeconomic contexts predicting trajectory membership of maternal depressive symptoms
As noted above, objective measures of SES are considered important predictors of individuals’ health disparities overall (Adler & Stewart, 2010), and longitudinal change in MDS, in particular (e.g., Kingsbury et al., Reference Kingsbury, Hayatbakhsh, Mamun, Clavarino, Williams and Najman2015; Wikman et al., Reference Wikman, Axfors, Iliadis, Cox, Fransson and Skalkidou2020). A systematic review of heterogeneity of individuals’ depression conducted by Musliner et al. (Reference Musliner, Munk-Olsen, Eaton and Zandi2016) reported that women with low-income/education and of non-White racial/ethnic backgrounds tend to display greater symptoms over time. Indeed, empirical studies with new mothers also show that lower household income or more exposure to financial adversity predicted a greater likelihood of being in risk trajectories of MDS, such as moderate-increasing and chronically high trajectories (e.g., Campbell et al., Reference Campbell, Matestic, von Stauffenberg, Mohan and Kirchner2007; Denckla et al., Reference Denckla, Mancini, Consedine, Milanovic, Basu, Seedat, Spies, Henderson, Bonanno and Koenen2018). For example, Choe et al. (Reference Choe, McDonough, Sameroff and Lawrence2020) identified three trajectories of MDS, low-decreasing, moderate, and increasing (a trajectory starting with elevated MDS with an increase over time) from 7 to 33 months and found lower paternal/maternal SES (a composite of income, education, and occupational prestige) predicted an increased likelihood of being in the moderate or increasing trajectories, compared to the low-decreasing trajectory.
In addition, emerging evidence suggests that subjective measures of SES (e.g., perceived financial strain, perceived social standing) may affect overall mental health outcomes over and beyond the influence of objective SES (Franzini & Fernandez-Esquer, Reference Franzini and Fernandez-Esquer2006; Goodman et al., Reference Goodman, Huang, Schafer-Kalkhoff and Adler2007; Kim & Radoias, Reference Kim and Radoias2021). Notably, some studies report even stronger effects of subjective SES on health outcomes than objective SES (Adler et al., Reference Adler, Epel, Castellazzo and Ickovics2000). For example, Franzini and Fernandez-Esquer (Reference Franzini and Fernandez-Esquer2006) found that among low-income Mexican-American adults (75% women), both lower perceived social status and higher perceived financial strain (e.g., not having enough money to buy clothing and pay the rent) predicted poor mental health, independent of the contribution of education and income. In addition, using data from the Family Life Project (FLP), Newland et al. (Reference Newland, Crnic, Cox and Mills-Koonce2013) found that higher levels of subjective SES, measured by perceived financial strain, predicted MDS at early childhood, while objective SES measured by income-to-needs ratio did not. Theoretically, individuals’ feelings related to social status or financial strain may be fundamental to health outcomes, given that negative feelings and subjective experiences related to lower SES (e.g., stress, disrespect, inferiority, distrust, and lower social cohesion) may interfere with neuroendocrine functioning and in turn, affect mental health symptoms and behavior (Wilkinson, Reference Wilkinson1999). Thus, subjective SES may be a key factor influencing longitudinal trajectories of MDS in early childhood, particularly among lower-income mothers.
Neighborhood adversity predicting trajectory membership of maternal depressive symptoms
Broader environmental contexts, such as community/neighborhood characteristics, have also been identified as a significant social determinant of maternal depression, independent of the predictive role of family SES (e.g., Huang et al., Reference Huang, King and McAtee2018; Shaw et al., Reference Shaw, Sitnick, Reuben, Dishion and Wilson2016). Living in impoverished, dangerous, and noisy neighborhoods appear to undermine individuals’ health and well-being and potentially increases depressive symptoms across the life span (Cammack et al., Reference Cammack, Lambert and Ialongo2011; Cutrona et al., Reference Cutrona, Wallace and Wesner2006; Kim, Reference Kim2008; Kohen et al., Reference Kohen, Leventhal, Dahinten and McIntosh2008). For example, Huang et al. (Reference Huang, King and McAtee2018) reported that greater exposure to community violence predicted increased depressive symptoms among low-income mothers, after controlling for family SES. Similarly, work by Cammack et al. (Reference Cammack, Lambert and Ialongo2011) demonstrates that perceived neighborhood violence is longitudinally associated with increased depressive symptoms in adolescents. Importantly, the authors also found that perceived neighborhood violence, compared to objective exposure to neighborhood violence, was more strongly associated with adolescents’ depressive symptoms.
Early social support as a resilience factor for maternal depressive symptoms across early childhood
Social partners (e.g., a caregiver, an intimate partner) can reduce physiological stress responses among altricial species, including human and nonhuman primates, throughout the lifespan (Gunnar & Hostinar, Reference Gunnar and Hostinar2015; Kikusui et al., Reference Kikusui, Winslow and Mori2006). In line with this notion, social support from a partner, extended family and friends, and the community are key resilience factors in the prevention and recovery from MDS in new mothers (Manuel et al., Reference Manuel, Martinson, Bledsoe-Mansori and Bellamy2012; Nagy et al., Reference Nagy, Moore, Silveira, Meaney, Levitan and Dubé2022; Vliegen et al., Reference Vliegen, Casalin and Luyten2014). In addition, Beck's (Reference Beck2001) meta-analysis informs that the effect of social support on maternal depression is even stronger than the effect of objective SES. Work using 414 Black rural, low-income mothers from the FLP data showed that mothers reporting high satisfaction with the quality of church-based social support in infancy reported fewer MDS at 24 months (Odom & Vernon-Feagans, Reference Odom and Vernon-Feagans2010). In regard to longitudinal MDS, inadequate social support, such as low quality of interpersonal relationships, greater needs for social support, and increased loneliness, predicted chronically high or increasing trajectories, compared to mothers in low-stable/decreasing trajectories (Choe et al., Reference Choe, McDonough, Sameroff and Lawrence2020; Denckla et al., Reference Denckla, Mancini, Consedine, Milanovic, Basu, Seedat, Spies, Henderson, Bonanno and Koenen2018; McCall-Hosenfeld et al., Reference McCall-Hosenfeld, Phiri, Schaefer, Zhu and Kjerulff2016). Thus, the examination of how social support predicts trajectory membership may provide meaningful implications in terms of early resilience factors for MDS among rural, low-income mothers.
Intimate partner violence predicting trajectory membership of maternal depressive symptoms
Intimate partner violence (IPV) is also relevant in considering MDS in diverse contexts (Conway et al., Reference Conway, Cook, Cahir, Mensah, Reilly, Brown, Gartland and Giallo2021), including low-income rural mothers in the U.S. (Gustafsson & Cox, Reference Gustafsson and Cox2012), Brazil (Ludermir et al., Reference Ludermir, Lewis, Valongueiro, de Araújo and Araya2010), and South Africa (Tsai et al., Reference Tsai, Tomlinson, Comulada and Rotheram-Borus2016). Across both high- and low-income countries, mothers’ exposure to physical and/or psychological (e.g., verbal aggression) violence by their intimate partner in pregnancy or early childhood has been consistently associated with elevated MDS. However, there is limited work examining the role of IPV on longitudinal trajectories of MDS. A few studies have reported that mothers’ negative feelings and experiences with the partner (e.g., fear of the partner) are associated with high-risk trajectories of MDS in early childhood (Denckla et al., Reference Denckla, Mancini, Consedine, Milanovic, Basu, Seedat, Spies, Henderson, Bonanno and Koenen2018; Giallo et al., Reference Giallo, Pilkington, McDonald, Gartland, Woolhouse and Brown2017; Wikman et al., Reference Wikman, Axfors, Iliadis, Cox, Fransson and Skalkidou2020). For example, Giallo and colleagues (2017) identified three trajectories of MDS from early pregnancy (< 24 weeks) through the first 4 years of the child’s life, using a sample of 1,102 mothers in Australia who had relatively high SES (i.e., obtaining at least a college degree, married/living with a partner) and were in paid employment during pregnancy. They found that, compared to the minimal symptoms trajectory over time, mothers reporting greater relationship problems with their partner during pregnancy were more likely to fall into the elevated MDS trajectory, and those experiencing higher levels of fear of the partner at 6 months postpartum were more likely to fall into the persistently high MDS trajectory. Despite this evidence, there is less research using direct maternal-report measures of IPV (including both physical and psychological violence), rather than proximal experiences relevant to IPV (e.g., fear of partner), in predicting MDS.
Current study
Given the importance of proximal and broader social determinants in predicting MDS, the current study aimed to examine the unique roles of objective and subjective SES, neighborhood environment, social support, and maternal-reported exposure to IPV in predicting trajectories of MDS in the first five years of their child’s life among low-income, rural mothers. We considered changes across the first five years because maternal mental health greatly impacts the well-being of both mothers and their young children during the early childhood years (Dietz et al., Reference Dietz, Jennings, Kelley and Marshal2009; Goodman et al., Reference Goodman, Huang, Schafer-Kalkhoff and Adler2007 Flanagan et al., Reference Flanagan, White and Carter2011; Stein et al., Reference Stein, Arteche, Lehtonen, Craske, Harvey, Counsell and Murray2010). Moreover, recent empirical evidence demonstrates that mothers consistently show changes in their depressive symptoms over time and exhibit individual differences in these longitudinal changes over the course of early childhood (e.g., Ahmed et al., Reference Ahmed, Bowen, Feng and Muhajarine2019; Denckla et al., Reference Denckla, Mancini, Consedine, Milanovic, Basu, Seedat, Spies, Henderson, Bonanno and Koenen2018). Therefore, identifying factors associated with risk and resilience in MDS trajectories may have implications for practice and policy interventions aimed at promoting the well-being of their mothers and their children’s development. Importantly, a better understanding of the early predictors of low-income mothers’ depressive symptoms may also contribute to identifying mothers at greater risk of developing elevated MDS/clinical depression at distinct time points, and may increase our knowledge about the factors promoting resilience to maladaptive outcomes.
Method
Participants
The Family Life Project (FLP) is a prospective longitudinal study of families residing in six predominantly low-income and rural counties in Pennsylvania (PA) and North Carolina (NC). These regions were selected to be representative of the Black South and Appalachia, respectively (Dill & Myers, Reference Dill, Myers and Blau2004). Adopting a developmental epidemiological design, a representative sample of 1,292 families who resided in one of the six counties at the time of the child’s birth were recruited. Participants were oversampled for low-income in both states and for African American race in NC. Information about participants’ ethnicity was not collected. A comprehensive description of the sampling procedure is provided by Vernon-Feagans et al. (Reference Vernon-Feagans and Cox2013). Among 1,292 families (51% boys), 59% of mothers were White and 41% were African American.
Procedure
For this study, families were seen in home visits at child age of 2, 6, 15, 24, and 58 months. At all times, demographic information was collected and primary caregivers completed questionnaires asking about their mental health symptoms. In the current study, MDS assessed with the Brief Symptoms Inventory-18 at 6, 15, 24, and 58 months were included. Data used in the current study also included primary caregivers’ demographic information (i.e., race, state) at 2 months, and multiple aspects of family and neighborhood environments, health information, and social relationships at 6 months.
Measures
Maternal depressive symptoms
At 6, 15, 24, and 58 months primary caregivers completed the Brief Symptoms Inventory-18 (BSI-18; Derogatis, Reference Derogatis2000), a validated, widely used self-report questionnaire adapted from the Symptom Checklist-90-Revised (SCL-90-R; Derogatis, Reference Derogatis1977) and BSI-53 (Zabora et al., Reference Zabora, Brintzenhofeszoc, Jacobsen, Curbow, Piantadosi and Hooker2001). The BSI-18 consists of the three subscales of depression, anxiety, and somatization with each subscale including 6 items (Govindasamy et al., Reference Govindasamy, Green and Olmos2020). The items of the depression subscale asked about mothers’ depressive symptoms in the preceding seven days and each was scored on a Likert-type scale, 0 = not at all to 4 = extremely, (αs = 0.81–.86 across 6 and 58 months). The BSI-18 has been widely used in studies with diverse populations, including both in community samples and large-national level samples (e.g., Houghton et al., Reference Houghton, Keane, Lewis, Murphy, Houghton and Dunne2013; Newland et al., Reference Newland, Crnic, Cox and Mills-Koonce2013) and postpartum mothers, in particular (e.g., Gueron-Sela et al., Reference Gueron-Sela, Camerota, Willoughby, Vernon-Feagans and Cox2018; Kotchick et al., Reference Kotchick, Dorsey and Heller2005; Lega et al., Reference Lega, Bramante, Lauria, Grussu, Dubini, Falcieri, Ghiani, Giordano, Guidomei, Mignuoli, Paris, Bettinelli, Proietti, Andreozzi, Brenna, Bucciarelli, Martelli, Ferraro, Torrisi, Carrozzino and Donati2022; Padrutt et al., Reference Padrutt, DeJoseph, Wilson, Mills-Koonce and Berry2023). Prior work has shown high internal consistency of the depression subscale in diverse populations (e.g., Derogatis, Reference Derogatis and Maruish2017; Houghton et al., Reference Houghton, Keane, Lewis, Murphy, Houghton and Dunne2013; Prinz et al., Reference Prinz, Nutzinger, Schulz, Petermann, Braukhaus and Andreas2013), including rural low-income mothers from their postpartum period through the early childhood of their child (Aisenberg, Reference Aisenberg2001; Gueron-Sela et al., Reference Gueron-Sela, Camerota, Willoughby, Vernon-Feagans and Cox2018; Ku & Blair, Reference Ku and Blair2023). The internal consistent of the current measure was high, ranging from 0.81 to .86 across 6 and 58 months. The depression subscale has good convergent, discriminant, and construct validity in assessing depressive symptoms of individuals across the United States and countries in Europe (e.g., Hamidia et al., Reference Hamidia, Kheirkhah, Chehrazi, Basirat, Ghadimi, Barat, Cuijpers, O’Connor, Mirtabar and Faramarzi2022; Kim et al., Reference Kim, Michalopoulos and Voisin2021; Li et al., Reference Li, Wang, Shou, Zhong, Ren, Zhang and Yang2018; Prinz et al., Reference Prinz, Nutzinger, Schulz, Petermann, Braukhaus and Andreas2013; Spitzer et al., Reference Spitzer, Hammer, Löwe, Grabe, Barnow, Rose, Wingenfeld, Freyberger and Franke2011). For the current analysis, outliers (i.e., scores ± 3SD from the mean at each time point) were replaced with the second highest or lowest values (n = 2, n = 3, n = 3, n = 6 across 6 and 58 months, respectively). The mean score was square-root transformed to correct skewness. In our sample, the percentage of mothers showing MDS scores at or above clinical cutoff (T-scores at or above 63; Derogatis, Reference Derogatis2000) at each time point were: 7% at 6 months, 9% at 15 months, 7% at 24 months, and 7% at 58 months.
Maternal education
Primary caregivers reported their highest levels of completed education in years, ranging from 6 to 22(doctoral degree). This approach has been used in a large number of studies using the FLP dataset (e.g., Ku & Blair, Reference Ku and Blair2023; Newland et al., Reference Newland, Crnic, Cox and Mills-Koonce2013).
Income-to-needs ratio (INR)
INR were calculated by dividing the total household income by the federal poverty threshold for the number of people residing in the household for that year. An INR below 1 thus indicates households with incomes that fall below the federal poverty level. INR has been used in various studies using the FLP dataset (e.g., Gustafsson & Cox, Reference Gustafsson and Cox2012; Gueron-Sela et al., Reference Gueron-Sela, Camerota, Willoughby, Vernon-Feagans and Cox2018; Newland et al., Reference Newland, Crnic, Cox and Mills-Koonce2013).
Financial strain
Primary caregivers completed the Economic Strain Questionnaire, adapted from Conger and Elder’s (Reference Conger and Elder1994). The original measure has been used to assess financial strain or financial stress experienced by individuals or families. The current measure consisted of six items assessing financial pressure/difficulty, the degree to which the family had difficulty paying bills and ran out of money each month (1 = great deal of difficulty to 5 = no difficulty at all). This measure has been widely used to assess financial hardship families experienced among families with diverse backgrounds (e.g., rural low-income families; Kainz et al., Reference Kainz, Willoughby, Vernon-Feagans and Burchinal2012; Ku & Blair, Reference Ku and Blair2023; Newland et al., Reference Newland, Crnic, Cox and Mills-Koonce2013; Odom & Vernon-Feagans, Reference Odom and Vernon-Feagans2010). Prior work has shown the high reliability of the current measure (e.g., Newland et al., Reference Newland, Crnic, Cox and Mills-Koonce2013; Odom & Vernon-Feagans, Reference Odom and Vernon-Feagans2010). Perception of financial strain assessed by the current measure has been found to be associated with other measures of SES, such as negative correlations with education attainment, income-to-needs ratio, and occupational prestige and positive associations with maternal health outcomes, such as depression and anxiety (e.g., Ku & Blair, Reference Ku and Blair2023; Odom & Vernon-Feagans, Reference Odom and Vernon-Feagans2010). Scores of positively worded items were reverse-scored, and scores of all items were averaged (α = .81).
Neighborhood safety/quietness
Mothers completed the Windshield Survey consisting of 12 items drawn from the Post-Visit Reaction Inventory in the FAST Track project (Conduct Problems Prevention Research Group, 1992). The current study included three items asking about the safety and quietness of the neighborhood around the dwelling on a Likert type scale (1 = obviously dangerous/noisy to 4 = above average safety/quietness). This measure has been widely used in studies, showing high internal consistency in prior work (e.g., Burchinal et al., Reference Burchinal, Vernon-Feagans and Cox2008; De Marco & Vernon-Feagans, Reference De Marco and Vernon-Feagans2013). The average scores across the items have shown positive associations with maternal education attainment, income-to-needs ratio, and occupational prestige, and a negative association with MDS (e.g., Ku & Blair, Reference Ku and Blair2023). For the current study, scores of all items were averaged and higher scores represent safer and quieter neighborhood environment (α = .76).
Social support
Social support was assessed using the nine items from the modified version of the Questionnaire on Social Support (Crnic et al., Reference Crnic, Greenberg, Ragzin, Robinson and Basham1983). The measure has been widely used to assess social support among populations from diverse backgrounds (e.g., Barnett & The Family Life Project Key Investigators, Reference Barnett2008), and this has shown high internal consistency in other studies as well as the current study (α = .80). Mothers rated their satisfaction with the quality of relationships with their intimate partner, extended family, and friends on a 4-point Likert-type scale (1 = very dissatisfied to 4 = very satisfied). Previous studies have identified social support as a predictor of positive maternal outcomes, such as positive maternal behavior with their child and lower postpartum depressive symptoms (Crnic et al., Reference Crnic, Greenberg, Ragzin, Robinson and Basham1983; Crockenberg, Reference Crockenberg1981, Reference Crockenberg1987; Taraban et al., Reference Taraban, Shaw, Leve, Wilson, Dishion, Natsuaki, Neiderhiser and Reiss2017; Unger & Powell, Reference Unger and Powell1980; Weinraub & Wolf, Reference Weinraub and Wolf1983). The nine items were selected by the FLP Investigators based on factor analyses and were averaged to generate a social support composite.
Intimate partner violence (IPV)
Mothers rated their partners’ use of verbal and physical violence during the past 12 months on the Conflict Tactics Scale (CTS– Couple Form R [CTS-R]; Straus et al., Reference Straus, Hamby, Boney-McCoy and Sugarman1996), a widely used measure of IPV. Scores from the CTS across the three subscales (i.e., verbal aggression, physical violence, and reasoning) have demonstrated good internal consistency for mothers in the postpartum and early childhood of their child (Gustafsson & Cox, Reference Gustafsson and Cox2012). For the present study, the means of the verbal aggression (six items) and physical violence (nine items) subscales were averaged to create an IPV composite. The scores from the items showed acceptable internal consistency (α = .68). Previous work has demonstrated that higher IPV, as measured by the physical violence at 6 months, predicted higher MDS at 15 months (Gustafsson & Cox, Reference Gustafsson and Cox2012). For the present study, among the 1,006 mothers who participated in the 6-month demographic interviews, 84.69% reported having a spouse/partner, either residential or nonresidential. However, the current relationship status was not used as the eligibility criterion for mothers to complete the survey because mothers were asked to reflect on their experiences in the past 12 months with any romantic partner.
Covariates
Maternal race (0 = White; 1 = Black), age, whether the mother lived with a spouse/partner (0 = no; 1 = yes), state (0 = PA; 1 = NC), and maternal anxiety (measured by the anxiety symptomology subscale of BSI-18) were included as covariates in analytic models. Maternal depression and anxiety symptoms are common sources of distress for new mothers and the most prevalent psychological symptoms new mothers experience. Although the two types of psychological symptoms may be comorbid, recent evidence shows distinct trajectories of two symptoms (Ahmed et al., Reference Ahmed, Bowen, Feng and Muhajarine2019) and each has unique effects on maternal behavior (Feldman et al., Reference Feldman, Granat, Pariente, Kanety, Kuint and Gilboa-Schechtman2009; Hakanen et al., Reference Hakanen, Flykt, Sinervä, Nolvi, Kataja, Pelto, Karlsson, Karlsson and Korja2019). The inclusion of maternal anxiety as a covariate allows us to examine the impact of other factors on membership of MDS trajectories, while accounting for the influence of anxiety.
Missing data
Among 1,292 families enrolled at the 2-month assessments, 6.97% of the families were not seen at the 6-month assessment, 10.06% at 15 months, 14.78% at 24 months, and 17.80% at 58 months. Families who did not participate at 6, 15, 24, or 58 months did not differ from those who participated on most study variables but differed on some sociodemographic variables (ps < .05). Specifically, families residing in PA were more likely to have assessments at 6 and 24 months, compared to those in NC. Families with higher maternal education tended to have the 15-month assessments, and those with higher INR tended to have the 24-month assessments. Full information likelihood estimation (FIML) was used to account for missing data, as FIML produces unbiased parameter estimates under the condition of missing at random (Enders & Bandalos, Reference Enders and Bandalos2001).
Analytic plan
Analyses proceeded in two steps using Mplus 8.4 (Muthén & Muthén, Reference Muthén and Muthén1998–2017). First, we identified different trajectories of MDS between 6 and 58 months of the child age using latent class growth analysis (LCGA; Jung & Wickrama, Reference Jung and Wickrama2008). LCGA is a special type of latent growth mixture modeling that allows one to identify multiple trajectories of certain characteristics among individuals and this approach does not estimate the variances of growth factors within classes (i.e., intercept and slope of maternal depressive symptoms). A series of LCGA models, from 1- to 6-trajectory models, were estimated with varying sets of starting values so that we ensured global maximum in each model (Masyn, Reference Masyn and Little2013). We initially estimated both linear and quadratic growth of MDS in each profile across 1–7-trajectory models. All LPA models were unconditional models, which of each was estimated without any covariates. A set of criteria was used to determine the best fitting model, including Bayesian information criterion (BIC; Schwarz, Reference Schwarz1978), Vuong-Lo-Mendell-Rubin likelihood ratio test (VLMR-LRT; Vuong, Reference Vuong1989), Lo-Mendell-Rubin likelihood ratio test (LMR-LRT; Lo et al., Reference Lo, Mendell and Rubin2001), entropy (Jedidi et al., Reference Jedidi, Ramaswamy and Desarbo1993), conceptual clarity and interpretability of the trajectory membership (Muthén, Reference Muthén2003), and a reasonable proportion of mothers assigned to each trajectory group, which is no less than 1% of the whole sample size (Jung & Wickrama, Reference Jung and Wickrama2008). After the best fitting model was selected, we removed non-significant higher-order terms (i.e., a quadratic slope) to improve the precision of the model estimation. Next, multinomial logistic regression was estimated to examine whether indicators of early experiences predict membership in a particular depression trajectory after controlling for covariate, using the manual three-step approach with Bayesian estimation (Asparouhov & Muthén, Reference Asparouhov and Muthén2014; Reference Asparouhov and Muthén2021). For a full description of the three-step approach, see the Supplemental Materials at the end of the manuscript.
Results
Preliminary analyses
Means, standard deviations, and ranges for all study variables are presented in Table 1. MDS scores across 6 and 58 months had moderate, positive correlations with financial strain and IPV, and small to moderate, negative correlations with maternal education, INR, neighborhood safety/quietness, and social support.
Table 1. Descriptive statistics and bivariate correlations

Note. Correlations in bold are p < 0.001; IPV = intimate partner violence; MDS = maternal depressive symptoms; scores of MDS are square−root transformed to correct skewness; m = months.
Latent profiles of maternal depressive symptoms trajectories
Given model comparison and fit criteria (see Analytic plan), the four-profile model was selected (Table 2). The four-profile showed a smaller BIC value and higher entropy relative to the other solutions, and also showed significant VLMR and LMR tests. The five- and six-profile models showed smaller BIC values than the four-profile model. However, the VLMR and LMR tests in the five-profile model were not significant, indicating that this model was not significantly better than the four-profile model. In addition, the six-profile model had one subgroup including only 4% of the participants, and two profiles in the six-profile model also displayed very similar patterns of MDS, both of which had moderate initial levels of MDS and showed a slight increase over time. Finally, the four-profile solution showed reasonably high posterior probabilities (range = .80–.92), and the identified trajectories aligned with the theoretical framework and empirical research. Then, the initial four-trajectory model was refined by removing nonsignificant quadratic growth terms and the refined, final model showed good model fit with posterior probabilities ranging from .81 to .91 (Table 2).
Table 2. Comparisons of fit among latent class growth analysis solutions with 1–6-trajectory models of maternal depressive symptoms
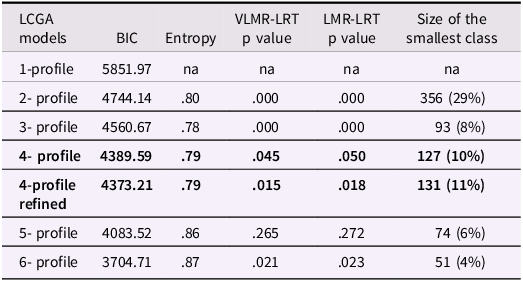
Note. LCGA = Latent class growth analysis; BIC = Bayesian Information Criteria; VLMR = Vuong-Lo-Mendell-Rubin; LMR = Lo-Mendell-Rubin; lower values of BIC indicate better fitting models and entropy values at or above 0.70 indicate good classification; a significant p-value of VLMR and LMR suggests that an estimated model with K trajectories was a better fit compared to a model with K-1 trajectories; the row with bold text is the best solution based on overall fit indices, parsimony, and interpretability; the 4-profile refined model was estimated after nonsignificant quadratic terms were removed from each profile.
As presented in Figure 1, the final LCGA model identified four trajectories of MDS: Low-decreasing (50%; n = 622), Low-increasing (26%; n = 324), Moderate-decreasing (13%; n = 156), and Moderate-increasing (11%; n = 131) trajectories. The Low-decreasing trajectory (50%) consisted of half of the mothers, who showed consistently low levels of MDS, specifically low with a slight linear decrease, through early childhood. (M Int = 0.22, SE = 0.02, p < .001; M LinearSlope = −0.03, SE = 0.01, p = .001). T-scores of MDS on average demonstrated that those mothers’ symptoms fell below clinical cutoff scores (T-scores at or above 63) at all time points (T-score Ms = 42.92, 43.00, 42.42, 40.62 at 6, 15, 24, 58 months). Next, in the Low-increasing trajectory (26%), mothers had moderate levels of MDS at 6 months, equivalent to the average of MDS among the whole sample at 6 months, and showed a slight linear increase over time (M Int = 0.42; SE = 0.05, p < .001; M LinearSlope = 0.06, SE = 0.01, p < .001). For this group, the means of T-scores fell below clinical cutoff scores across all time points (T-score Ms = 46.35, 48.48, 48.31, 51.74 across 6 and 58 months). The third trajectory, Moderate-decreasing (13%), consisted of mothers with high levels of MDS at 6 months, and they showed a large linear decrease from 6 through 58 months (M Int = 0.98; SE = 0.05, p < .001; M LinearSlope = −0.14, SE = 0.01, p < .001). This trajectory group had MDS T-scores on average below the clinical cutoff at all time points (T-score Ms = 58.24, 57.80, 54.01, 42.90 from 6 through 58 months). Lastly, the Moderate-increasing trajectory has the smallest group size (11%; n = 131) and mothers in the trajectory showed a slight linear increase of MDS across 6 and 58 months (M Int = 1.01; SE = 0.06, p < .001; M LinearSlope = 0.05, SE = 0.01, p < .001). These mothers started with MDS below the clinical cutoff at 6 months (T-score M = 58.41), which was equivalent levels of MDS at 6 months in the Moderate-decreasing trajectory. Then, they showed a linear increase over time, and reported clinical levels of MDS T-scores on average at 58 months (T-score Ms = 61.19, 60.97, 64.43 at 15, 24, 58 months).
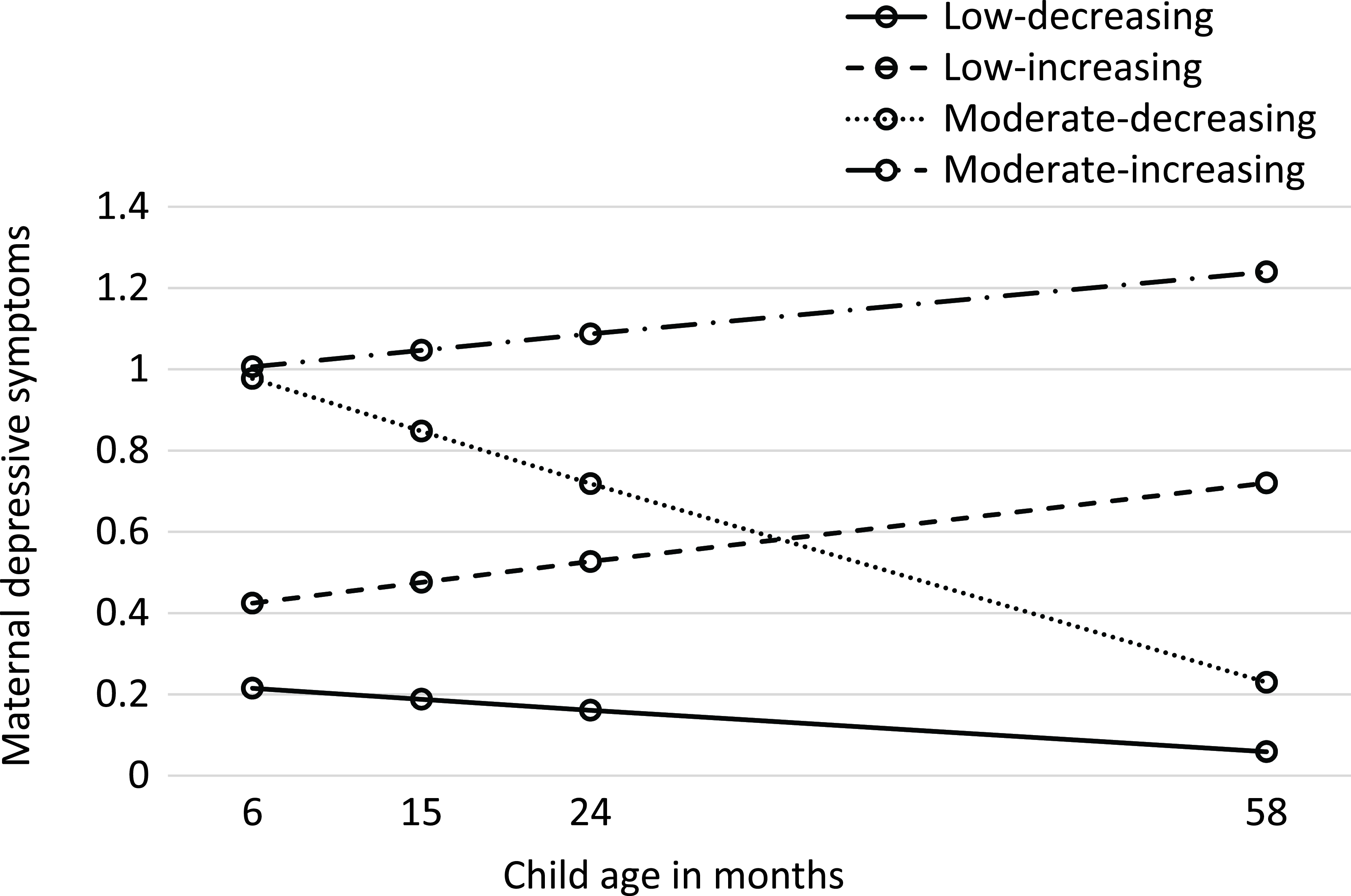
Figure 1. Estimated trajectories of maternal depressive symptoms from 6 to 58 months. The Y-axis indicates square-root transformed means of maternal depressive symptoms of each profile at 6, 15, 24, and 58 months. The original scores for each trajectory are as follows: (a) low-decreasing (0.12 at 6 months; 0.13 at 15 months; 0.10 at 24 months; and 0.02 at 58 months); (b) low-increasing (0.29, 0.42, 0.40, and 0.55 at 6, 15, 24, and 58 months); (c) moderate-decreasing (1.06, 1.05, 0.78, and 0.11 at 6, 15, 24, and 58 months); and (d ) moderate-increasing (1.12, 1.41, 1.42, and 1.65 at 6, 15, 24, and 58 months).
Predictors of trajectory membership
As demonstrated in Table 3, we compared all three trajectories with elevated risk to the Low-decreasing trajectory (reference group) to examine early risk and resilience factors that differentiate high-risk trajectories from Low-decreasing. Relative to those in the Low-decreasing trajectory profile, mothers in Low-increasing were less likely to live in safer neighborhoods and to report social support, and more likely to report higher IPV. Also, relative to mothers in Low-decreasing, mothers in Moderate-decreasing and Moderate-increasing were more likely to experience higher financial strain and IPV, and less likely to report social support. Next, we compared between three risk trajectories to investigate early proximal and broader contexts associated with maternal membership of distinct MDS trajectories. Relative to mothers in the Low-increasing trajectory, those in Moderate-decreasing reported higher financial strain and IPV. Mothers in the Moderate-increasing trajectory, relative to those in Low-increasing, showed higher financial strain and IPV, and lower social support. Lastly, mothers in the Moderate-increasing trajectory reported lower social support than those in Moderate-decreasing.
Table 3. Multinomial regression: trajectory profile membership predicted by SES, neighborhood, and interpersonal context
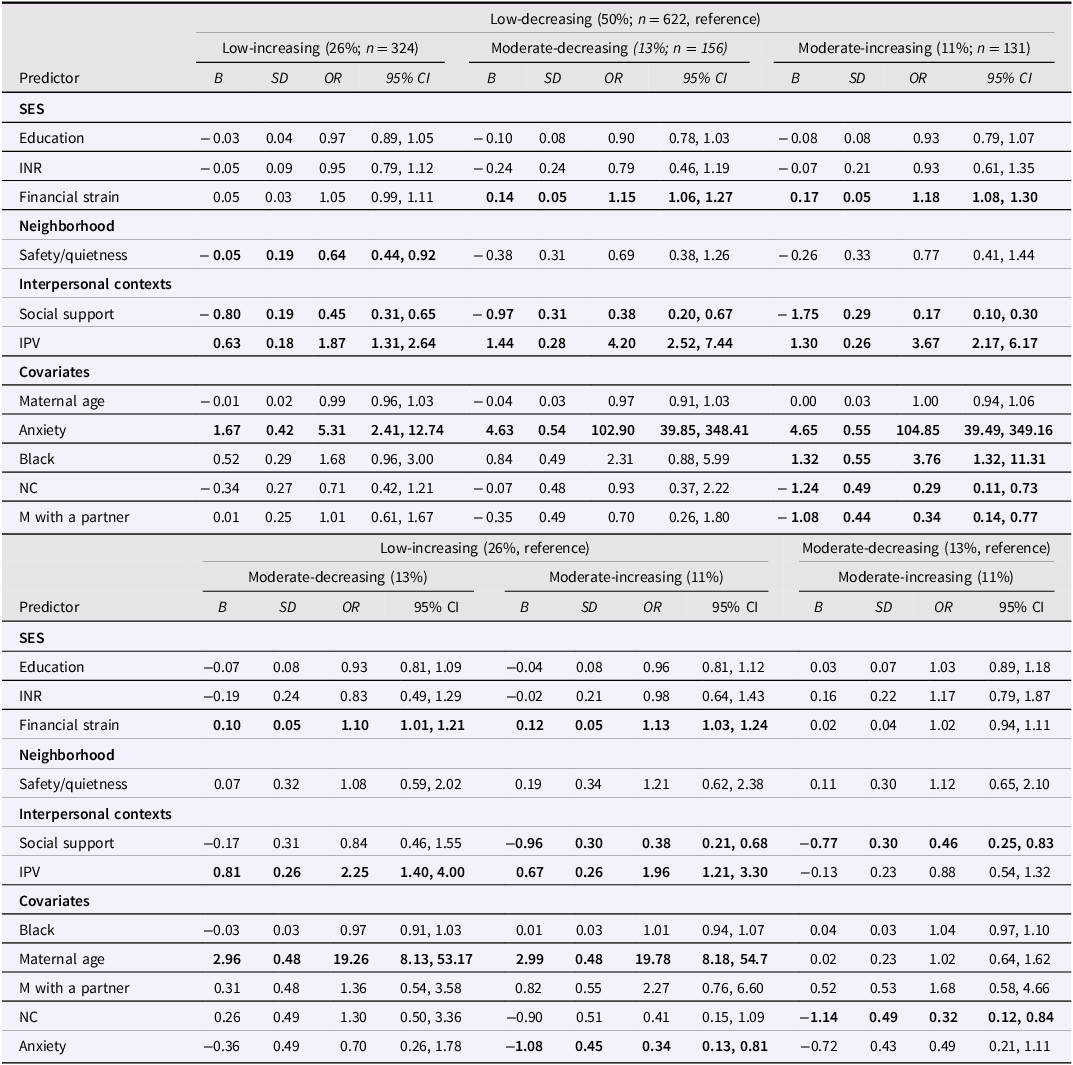
Note. SES = socioeconomic status; INR = income-to-needs ratio; IPV = intimate partner violence; M with partner = the mother living with a partner; B indicates a posterior coefficient estimate; SD indicates one-tailed posterior standard deviation; bold text indicates statistically significant coefficients or odds ratios with the 95% confidence interval.
In regard to covariates, mothers with greater anxiety symptoms were more likely to belong to three high-risk trajectories, compared to Low-decreasing. Similarly, compared to the Low-increasing trajectory, more anxious mothers tended to fall into Moderate-decreasing and Moderate-increasing. Compared to White mothers, Black mothers tended to belong to the Moderate-increasing trajectory than the Low-decreasing trajectory. In addition, maternal relationship status, whether they lived with a spouse/partner, was a significant early indicator of a highest-risk trajectory, such that compared to mothers in the Low-decreasing trajectory, those not living with a spouse/partner were more likely to belong to Moderate-increasing.
Discussion
The current study examined trajectories and sociodemographic predictors of MDS across the first five years of the child’s life using a sample of low-income mothers living in rural areas of the US. We also found that lower levels of perceived SES, inadequate social support, and higher levels of IPV are key factors predicting high-risk trajectories of MDS (i.e., Low-increasing, Moderate-decreasing, and Moderate-increasing trajectories). The current study advances our understanding of heterogeneous changes in long-term MDS among low-income rural mothers, using a large, epidemiological sample of mothers with relatively racially diverse backgrounds. Moreover, our findings may have implications for interventions designed to foster resilience of new mothers who are susceptible to experiencing moderate to severe MDS.
We found four distinct trajectories of MDS differentiated by various levels of initial MDS with differing patterns of change, including Low-decreasing (50%), Low-increasing (26%), Moderate-decreasing (13%), and Moderate-increasing (11%) trajectories. These trajectories are similar to those reported in prior work, which commonly identified three to six distinct trajectories of postpartum and later MDS across early childhood (e.g., Campbell et al., Reference Campbell, Matestic, von Stauffenberg, Mohan and Kirchner2007; Choe et al., Reference Choe, McDonough, Sameroff and Lawrence2020; Putnick et al., Reference Putnick, Sundaram, Bell, Ghassabian, Goldstein, Robinson, Vafai, Gilman and Yeung2020). Our findings add to this literature by demonstrating that mothers with low-income backgrounds show similar patterns of changes in longitudinal MDS as those identified in higher-SES samples. Previous research examining depression among rural mothers has documented that mothers in rural communities are at a higher risk of developing depressive symptoms, both in the postpartum period (Mollard et al., Reference Mollard, Hudson, Ford and Pullen2016) and outside of the postpartum period (Groh, Reference Groh2013; Simmons et al., Reference Simmons, Yang, Wu, Bush and Crofford2015). However, this pattern was not observed in our sample of low-income, rural mothers living in North Carolina and Pennsylvania. Given the limited amount of existing literature focusing on rural mothers, most of which used small, community samples and diverse assessment tools across studies, it is challenging to make direct comparisons between the findings of the current study and prior research. Our findings regarding heterogeneity in MDS among rural mothers may reflect the fact that rural mothers in the U.S. are not homogenous but rather diverse in terms of risk and protective factors (e.g., Ku & Blair, Reference Ku and Blair2023), which is one of the unique contributions of the present study to the field. Future studies may investigate MDS in rural areas across various regions of the U.S
In regard to the second aim of the current study, examining predictors of MDS trajectories, we found that mothers in all three of the high-risk trajectories of MDS tended to report higher financial strain, lower social support, and higher levels of IPV, compared to women in the Low-decreasing trajectory. We also observed that mothers who perceived their neighborhood as more dangerous and noisier were more likely to display relatively greater initial symptoms at 6 months postpartum with a gradual increase over time (i.e., Low-increasing trajectory). Importantly, we found that satisfaction with social support was the most salient predictor in differentiating mothers in the Moderate-decreasing trajectory from those in the Moderate-increasing trajectory.
A notable finding from the current study was that lower subjective SES, indexed by greater perceived financial strain, predicted high-risk trajectories. Specifically, mothers who reported higher financial strain were more likely to belong to Low-increasing, Moderate-decreasing, and Moderate-increasing trajectories than Low-decreasing. Moreover, greater financial strain also differentiated mothers in the Moderate-decreasing and Moderate-increasing trajectory relative to those in the Low-increasing trajectory. Our analyses revealed that when multiple indicators of SES were considered simultaneously in an analytic model, perceived financial strain predicted trajectory membership of MDS, above and beyond the traditional objective measures of SES, such as education and INR. These findings support prior findings that individuals’ perceived SES has important implications for mental health, independent from objective SES (Franzini & Fernandez-Esquer, Reference Franzini and Fernandez-Esquer2006; Goodman et al., Reference Goodman, Huang, Schafer-Kalkhoff and Adler2007; Kim & Radoias, Reference Kim and Radoias2021). Furthermore, this evidence is consistent with prior work suggesting that subjective SES may even have a stronger influence on individuals’ psychological functioning, assessed at discrete points in time, than objective SES across studies with diverse populations (Adler et al., Reference Adler, Epel, Castellazzo and Ickovics2000; Newland et al., Reference Newland, Crnic, Cox and Mills-Koonce2013). In contrast, we found no association between objective SES and trajectory membership. One plausible reason for this nonsignificant association could be the restricted range of SES in our predominantly low-income sample, which may have limited our ability to detect associations between objective SES and trajectory membership. Mothers with depressive symptoms could also be more likely to perceive their socioeconomic status as low. These mothers may be more susceptible to experiencing feelings of inferiority, and may perceive their socioeconomic situations as stressful and unsupportive and even perceive their social environment as distrustful and less cohesive (Wilkinson, Reference Wilkinson1999). Mothers experiencing depressive symptoms also may report amplified negative perceptions of subjective SES, such as struggles to make ends meet and support their families’ living expenses, relative to objective SES standing.
Along with the role of subjective SES, the current analyses also demonstrate that broader neighborhood contexts may contribute to differentiating trajectories of MDS. Specifically, we found that mothers who perceived their neighborhood as more dangerous and noisier tended to fall into the Low-increasing trajectory, characterized by low initial symptoms (i.e., approximately the average levels of symptoms of the entire sample at 6 months) with a gradual increase across early childhood, compared to those in Low-decreasing. This effect was only seen in the Low-increasing group in comparison with the Low-decreasing in the multinomial analysis. Importantly, we found that adverse neighborhood environments predicted increased MDS above and beyond the effects of subjective SES measures, suggesting a potential unique role of neighborhood characteristics in predicting MDS beyond potential associations with SES. For example, mothers who perceive their neighborhood as unsafe and noisy may experience intensified stress and anxiety (Cutrona et al., Reference Cutrona, Wallace and Wesner2006), which may exacerbate MDS over time. However, our analysis revealed that neighborhood environments did not significantly differentiate between other trajectories. Given that the current study is the first to explore the role of neighborhood environments in the trajectories of MDS, we can only speculate why and how differential associations emerged. Compared to the Low-decreasing and Low-increasing trajectories, mothers from the Moderate-decreasing and Moderate-increasing trajectories were socioeconomically underprivileged and lived in more dangerous neighborhoods in the postpartum. Those mothers may be worried about the environments in which they raise their infants and are likely to experience elevated MDS. A marginal difference in neighborhoods during the postpartum period may not differentiate the trajectories of MDS among mothers already experiencing elevated depressive symptoms during this time. Future research should consider investigating the role of neighborhoods in longitudinal MDS across diverse populations.
Supporting social buffering theory (Kikusui et al., Reference Kikusui, Winslow and Mori2006), our analyses also suggest that the quality of social relationships may serve as a significant role in the longitudinal manifestation of MDS across early childhood. Mothers reporting higher social support, indexed by greater satisfaction with their social relationships, were more likely to display persistently low MDS from 6 to 58 months (i.e., Low-decreasing trajectory), relative to those in the other three high-risk trajectories. Our results are also consistent with other findings from recent studies demonstrating that mothers who felt more supported within their family and broader social network were less likely to belong to high-risk trajectories, such as elevated, increasing, and chronically high trajectories of MDS (Choe et al., Reference Choe, McDonough, Sameroff and Lawrence2020; McCall-Hosenfeld et al., Reference McCall-Hosenfeld, Phiri, Schaefer, Zhu and Kjerulff2016). Furthermore, our analyses suggest that among high-risk mothers with elevated MDS, higher social support may be a strong resilience factor for both preventing and attenuating MDS over time. Specifically, we found that mothers who reported greater social support at 6 months were more likely to show a decrease in MDS through early childhood (i.e., Moderate-decreasing trajectory). In contrast, mothers reporting lower social support at 6 months tended to demonstrate persistently high and increasing levels of MDS over time (i.e., Moderate-increasing trajectory). Overall, the significant role of social support in the trajectories of MDS echoes the tendency for rural women, who often seek informal networks such as extended family and community support. This is because rural women may encounter personal and/or public stigma when seeking mental health care, and access to healthcare is limited (Gauri, Reference Gauri2013; Mollard et al., Reference Mollard, Hudson, Ford and Pullen2016). Social support from various sources may collectively promote emotional well-being for new mothers.
Across distinct trajectories of MDS, IPV was an important predictor differentiating all high-risk trajectories (i.e., Low-increasing, Moderate-decreasing, Moderate-increasing) from the Low-decreasing trajectory. In addition, compared to mothers in the Low-increasing trajectory, those in Moderate-decreasing and Moderate-increasing reported greater IPV. Broadly, these findings extend the literature demonstrating that mothers’ exposure to and experiences related to their partner’s emotional and physical aggression predict elevated MDS, assessed at singular time points mostly during infancy and toddlerhood (Conway et al., Reference Conway, Cook, Cahir, Mensah, Reilly, Brown, Gartland and Giallo2021; Gustafsson & Cox, Reference Gustafsson and Cox2012; Ludermir et al., Reference Ludermir, Lewis, Valongueiro, de Araújo and Araya2010; Tsai et al., Reference Tsai, Tomlinson, Comulada and Rotheram-Borus2016). Similarly, early IPV may be a key factor differentiating persistently high MDS from lowest-risk (e.g., constant-low) and relatively low-risk MDS trajectories among mothers with diverse sociodemographic backgrounds (Denckla et al., Reference Denckla, Mancini, Consedine, Milanovic, Basu, Seedat, Spies, Henderson, Bonanno and Koenen2018; Giallo et al., Reference Giallo, Pilkington, McDonald, Gartland, Woolhouse and Brown2017; Wikman et al., Reference Wikman, Axfors, Iliadis, Cox, Fransson and Skalkidou2020). Exposure to severe physical and psychological IPV may significantly escalate stress as mothers would feel threatened and intimidated (Lutgendorf, Reference Lutgendorf2019). Furthermore, IPV often leads to adverse health outcomes (e.g., physical injuries, insomnia), financial hardships, and poor quality of life (Wong & Mellor, Reference Wong and Mellor2014). This may disrupt new mothers’ well-being and emotional adjustment as a new mother, possibly leading to elevated MDS. We found the Moderate-decreasing and Moderate-increasing trajectory groups reported the highest IPV at 6 months among all of the trajectory groups; yet, it is not clear from the current data why one group showed a decrease in MDS while the other showed persistently high symptoms over time. However, one possibility is that some mothers might experience changes in IPV over time due to a variety of factors, such as a change in partnership (Chang et al., Reference Chang, Dado, Hawker, Cluss, Buranosky, Slagel, McNeil and Scholle2010), thereby helping reduce MDS over time.
Our findings also highlight racial differences in patterns of longitudinal change in MDS. Specifically, the current analysis indicates that compared to White rural mothers, Black rural mothers tended to belong to the Moderate-increasing trajectory (the highest-risk group) than the Low-decreasing trajectory (the lowest risk group). In this context, it is crucial to discuss how structural racism and inequality can significantly impact Black mothers’ experiences in managing their depressive symptoms during the postpartum and early childhood phases of their child’s life. These impacts may go beyond individual-level experiences, but extend to systemic challenges that may disproportionately affect marginalized communities, particularly Black mothers (Jones, Reference Jones2000). The historical context of persistent racism and discrimination experience may exacerbate Black individuals’ depressive symptoms through perceived discrimination, racial bias, and microaggression may exacerbate depressive symptoms (Williams & Mohammed, Reference Williams and Mohammed2009), and this pattern is consistent with Black mothers and in particular the ones with young children living in rural communities (Odom & Vernon-Feagans, Reference Odom and Vernon-Feagans2010; Schulz et al., Reference Schulz, Israel, Zenk, Parker, Lichtenstein, Shellman-Weir and Laura Klem2006). In addition, intersections of race, gender, and poverty may compound the structural racism and inequality. Studies have shown that compared to White counterparts, Black mothers often have limited access to health care, and higher rates of poverty, unemployment, and housing instability (Williams & Mohammed, Reference Williams and Mohammed2009), all of which can contribute to health disparities. It is also possible that stigma and cultural norms prevailed in the Black communities may prevent Black mothers from actively seeking support and engaging in appropriate interventions (Kozhimannil et al., Reference Kozhimannil, Trinacty, Busch, Huskamp and Adams2011).
The longitudinal nature and repeated assessments of MDS across the first 5 years of the child’s life are a significant strength of the current study. Furthermore, we characterized trajectories of MDS using a large sample of racially diverse mothers living in rural regions with high poverty rates, a population that has historically been neglected in research. This contributes to the existing literature, given that the majority of prior work conducted in developed countries, such as in the U.S. and Canada, has predominately included mothers with relatively high SES and/or mothers residing in urban areas (e.g., Ahmed et al., Reference Ahmed, Bowen, Feng and Muhajarine2019; Choe et al., Reference Choe, McDonough, Sameroff and Lawrence2020). In addition, our data elucidates the unique and varied roles of perceived SES versus objective SES, neighborhood environments, social support and IPV in predicting different trajectories of MDS. This more holistic approach may increase our understanding of experiences of rural low-income mothers at the individual, family, and neighborhood levels, and how these contexts may affect longitudinal trajectories of MDS. Considering the growing body of literature that acknowledges the significant influence of MDS on child development over time (e.g., Choe et al., Reference Choe, Deer and Hastings2023), future research may explore the dynamics of MDS and their impact on various aspects of child health, social-emotional well-being, and cognitive development.
Despite these strengths, our findings should be interpreted alongside the limitations of this study. We relied on maternal self-reported early experiences in the family and neighborhood, and lacked diagnosis in MDS by clinicians. This may inflate associations between mothers’ early experiences and MDS, such that mothers with severe depressive symptoms may interpret their financial situation as worse. Although the present study included extensive indicators of mothers’ postpartum experiences in adversity and protective factors, we lacked data on prenatal/birth-related predictors of early childhood MDS as well as prenatal depressive symptoms. Most of mothers with elevated depressive symptoms may show a gradual decrease in depressive symptoms after birth (Ahmed et al., Reference Ahmed, Bowen, Feng and Muhajarine2019); however, among some mothers, depressive symptoms may persistent throughout early childhood (Denckla et al., Reference Denckla, Mancini, Consedine, Milanovic, Basu, Seedat, Spies, Henderson, Bonanno and Koenen2018; Giallo et al., Reference Giallo, Pilkington, McDonald, Gartland, Woolhouse and Brown2017). Thus, we are mindful of the interpretation of the postnatal predictors of depression trajectory membership, especially the Moderate-increasing trajectory group. Finally, given that this sample is predominantly low-income, the regression coefficients might underestimate the effects.
The current findings have clinical implications for supporting mothers identified as high-risk for depression trajectories. Early detection of mothers who are susceptible to experiencing high-risk trajectory patterns is crucial. At the individual level, interventions targeting postpartum mothers should focus on managing financial stress, enhancing social support, and addressing IPV to prevent the escalation of depressive symptoms. Addressing neighborhood safety can also mitigate increasing depressive symptoms. Collaborative efforts involving healthcare professionals, mental health providers, community organizations, and policymakers are essential. Since a subgroup of new mothers may continue to struggle with MDS over time, there is a need for longitudinal support that extends beyond the postpartum period to help these mothers navigate evolving challenges. Given the sample’s diversity, cultural sensitivity is crucial, especially for diverse racial and socioeconomic backgrounds, such as Black mothers at higher risk of elevated depressive symptoms. In summary, these findings shed light on the heterogenous longitudinal manifestations of MDS among historically underserved mothers in early childhood, informing targeted interventions.. This characterization is an integral step in helping to develop and implement novel, evidence-based strategies to mitigate the adverse consequences and burden of depression on women and their children.
Acknowledgements
We would like to express our gratitude to all of the families, children, and teachers who participated in this research and to the FLP research assistants for their hard work and dedication to the FLP. This study is part of the FLP (https://flp.fpg.unc.edu/).
Funding statement
This research was supported by a grant from the National Institute of Child Health and Human Development, P01HD039667. Co-funding was provided by the National Institute of Drug Abuse, NIH Office of Minority Health, National Center on Minority Health and Health Disparities, and the Office of Behavioral and Social Sciences Research. This research was also supported by a grant from NICHD R01HD51502 and from the NIH Office of the Director, UG3OD023332 and UH3OD023332.
Competing interests
None.







