Cannabis use is more common in people with psychotic disorders compared with people without psychoses. Reference Hall and Degenhardt1 This is perhaps surprising given the widely held clinical opinion that cannabis can cause deterioration or impair recovery from psychotic disorders.
Experimental studies and surveys of users provide evidence that cannabis intoxication can produce transient psychotic and affective experiences and can have detrimental effects on motivation and memory. Reference D'Souza, Abi-Saab, Madonick, Forselius-Bielen, Doersch, Braley, Gueorguieva, Cooper and Krystal2–Reference Thomas4 Evidence from a recently conducted systematic review Reference Moore, Zammit, Lingford-Hughes, Barnes, Jones, Burke and Lwis5 also indicates that cannabis may increase the incidence of psychotic outcomes, independently of intoxication effects. Given these effects on mental state, it seems plausible that continued use of cannabis following the onset of a psychotic disorder may increase the severity or duration of psychotic symptoms, decrease adherence to treatment and impair longer-term outcome.
One reason people with psychosis may use cannabis is that the perceived benefits such as a reduction in anxiety and increased sociability Reference Dixon, Haas, Weiden, Sweeney and Frances6,Reference Schofield, Tennant, Nash, Degenhardt, Cornish, Hobbs and Brennan7 outweigh any perceived harmful consequences. However, it is also possible that the clinical impression of cannabis use resulting in a worse outcome in psychosis is confounded by other factors associated with poor prognosis such as alcohol or other illicit drug use.
Most studies that have examined the effects of substance use on psychosis have been either cross-sectional or case–control designs, but such approaches are limited, particularly in their ability to distinguish the direction of any associations observed. This ability to examine the direction of association is particularly important given the reports of increased cannabis use following onset of psychosis. Reference Ferdinand, Sondeijker, van der Ende, Selten, Huizink and Verhulst8,Reference Hides, Dawe, Kavanagh and Young McD9
In this review we examine the strength of evidence, from longitudinal studies, that cannabis use in people with psychosis impacts negatively on illness severity, adherence to treatment or other adverse outcomes, independently of the effects of alcohol and other drugs or other confounding factors.
Method
Study samples
Studies were included if they were longitudinal studies of people with psychosis, or case–control studies nested within longitudinal designs, where cannabis use was measured at a time prior to the outcome being measured. Cohorts of individuals with dual diagnosis of psychosis and cannabis misuse or dependence were excluded, as there could be no comparison group of people who did not use cannabis to determine if it had any affect on outcome.
The following diagnostic groups were included for psychosis: schizophrenia, schizophreniform, schizoaffective or psychotic disorders, non-affective or affective psychoses, psychosis not otherwise specified (NOS), psychotic symptoms, delusions, hallucinations or thought disorder. Primary outcomes that we specified a priori as being markers of progression of disease and relevant to this review were: relapse, readmission, change in symptom scores (positive, negative or global psychopathology symptoms), harm to self or others (including violence, criminality, suicide attempts and mortality), non-adherence to treatment, engagement with services, employment, homelessness, social functioning, quality of life and patient or carer satisfaction.
Literature search
We searched the following databases from their inception to November 2006: MEDLINE, EMBASE and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) on OVID; PsycINFO on WebSPIRS; ISI Web of Knowledge and ISI Proceedings; Zetoc (British Library database of journal and conference contents); BIOSIS on EDINA; Latin American and Caribbean Health Sciences (LILACS); and Caribbean Health Sciences Literature (MedCarib). An experienced research librarian (M.B.) and three investigators (G.L. T.H.M.M .and S.Z.) developed the search strategy. We searched using the format ((psychosis OR schizophrenia OR hallucinations OR delusions OR synonyms) AND (substance abuse AND synonyms)), using text words and indexing (MeSH) terms (full details available from the authors on request). The search was restricted to studies on humans but not by language or publication status. We searched reference lists of included studies, and wrote to experts in the field and study authors to find other published and unpublished studies of relevance.
Study selection and data extraction
We examined all titles and abstracts, and obtained full texts of potentially relevant papers. Working independently and in duplicate, we read the papers to determine if they met our inclusion criteria using eligibility record forms. At the abstract stage we had more lenient inclusion criteria and included studies with broad descriptions of mental health problems and of drug use. These papers were obtained in full, and rejected if the data were not provided separately for people using cannabis or for people with psychotic disorder as defined by our criteria. Where information was only available as an abstract, authors were contacted for further information; if this was not forthcoming then the study was excluded. Disagreements were resolved by consensus, and data extracted independently and in duplicate.
Quality assessment
We assessed quality by recording how potential non-causal explanations, particularly bias and confounding, were accounted for in each study. We assessed information on sampling strategy, response rates, missing data, attrition and attempts to address reverse causation, intoxication effects and confounding. All relevant MOOSE (Meta-analysis Of Observational Studies in Epidemiology) guidelines Reference Stroup, Berlin, Morton, Olkin, Williamson, Rennie, Moher, Becker, Sipe and Thacker10 were followed.
Results
Description of studies
Results of search
Our literature search, expert advice and search of reference lists yielded 15 303 references. Of these, 226 (1.5%) were thought to possibly have data relevant for our review, and 212 of these were excluded following a more detailed assessment using eligibility forms (Fig. 1).
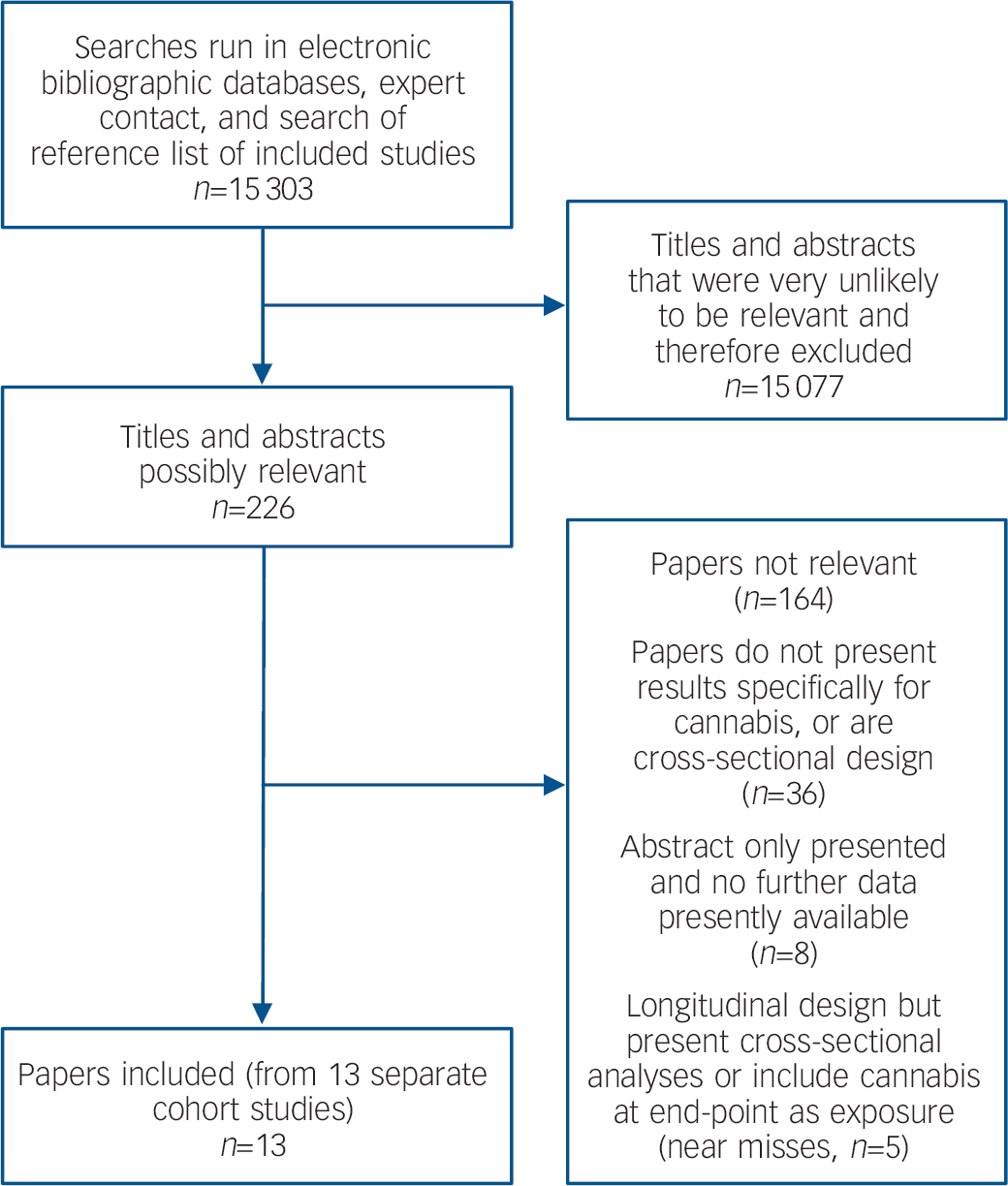
Fig. 1 QUOROM (Quality of Reporting of Meta-analyses) flow chart.
Included studies (for any outcome)
We found 13 publications reporting data from 13 cohort studies. Seven studies examined first-episode or recent onset psychoses (onset within 5 years): the Brisbane Reference Hides, Dawe, Kavanagh and Young McD9 and Melbourne Reference Wade, Harrigan, Edwards, Burgess, Whelan and McGorry11 studies in Australia (Melbourne study included after additional information provided by authors); the Calgary Reference Pencer, Addington and Addington12 and Calgary Early Psychosis Program (CEPP) Reference Coldham, Addington and Addington13 studies in Canada; the South London Hospitals Reference Grech, van Os, Jones, Lewis and Murray14 and Manchester studies Reference Stirling, Lewis, Hopkins and White15 in the UK; and the HGDH research group study in first-episode psychosis, a multicentre trial based in both North America and Western Europe. Reference Green, Tohen, Hamer, Strakowski, Lieberman, Glick and Clark16 Six studies included both incident and prevalent cases of psychosis: the Navarra Reference Martinez-Arevalo, Calcedo-Ordonez and Varo-Prieto17 study; the Madrid-A Reference Arango, Calcedo, Gonzalez and Calcedo18 and the Madrid-B Reference Arias Horcajadas, Romero and Calo19 studies, all based in Spain; the Homburg Reference Caspari20 study in Germany; and the Sydney-A Reference Degenhardt, Tennant, Gilmour, Schofield, Nash, Hall and McKay21 and Sydney-B Reference Grace, Shenfield and Tennant22 studies in Australia.
Results for the 13 studies are summarised in online Table DS1. Overall, of the 52 outcomes reported from these studies, cannabis was associated with statistical evidence of a worse outcome in 14, and a better outcome in 7 of these. There was no evidence of association in either direction for the other 31 outcomes. Seven studies looked at people with schizophrenia only (or related spectrum disorders), but the other six included people with other psychoses too. All of the seven associations with better outcomes in cannabis users were in studies that included individuals with any psychosis rather than specifically schizophrenia or related spectrum disorders.
The variety in outcome and exposure measure definitions used, as well as the content of statistical results presented, meant that it was not possible to pool results in a meta-analysis, and we therefore use a narrative synthesis to summarise the findings from this systematic review.
Excluded studies
We identified five studies of people with psychosis that did not meet all our inclusion criteria but which we considered to be ‘near-misses’. Reference Addington and Addington23–Reference Pencer and Addington27 These were all longitudinal studies but they either presented data only from cross-sectional analyses, or employed a measure of cannabis use that could have included individuals increasing or initiating use secondary to the outcome studied. All of these studies, including the seminal work by Linszen et al, Reference Linszen, Dingemans and Lenior25 reported associations between cannabis use and worse outcomes. Further details of these studies are available at www.bristol.ac.uk/psychiatry/research/psychotic.html.
Results for relapse or rehospitalisation
We found four studies of relapse and three studies addressing rehospitalisation. Two studies used definitions for relapse based on the Brief Psychiatric Rating Scale (BPRS) scores; the Brisbane Reference Hides, Dawe, Kavanagh and Young McD9 study reported a dose-response association between cannabis use (days per week) and increased relapse of psychosis, and a strong association between cannabis misuse and relapse was also reported in the Melbourne study. Reference Wade, Harrigan, Edwards, Burgess, Whelan and McGorry11 Relapse was also increased by cannabis use in the Navarra study, Reference Martinez-Arevalo, Calcedo-Ordonez and Varo-Prieto17 with evidence strongest for continued use during follow-up (64% relapse in individuals using cannabis at baseline and follow-up compared with 17% in non-users). Similarly, the Madrid-B study reported weak evidence for association between cannabis dependence and increased relapse. Reference Arias Horcajadas, Romero and Calo19 Neither of these two latter study reports provided the definition of relapse used.
Cannabis misuse was associated with a greater rehospitalisation index (0.98 readmissions per year compared with 0.35 for the non-misuse group) in the Homburg study, Reference Caspari20 and similarly with a greater number of admissions in the Madrid-B study. Reference Arias Horcajadas, Romero and Calo19 In the Navarra study, risk of readmission was similar in individuals who used cannabis regularly at baseline only, but not at follow-up, compared with controls (13% and 17% respectively), though there was some evidence for increased readmission in those using cannabis regularly both at baseline and at follow-up (43% v. 17%, P=0.08). Reference Martinez-Arevalo, Calcedo-Ordonez and Varo-Prieto17
Results for severity of symptoms
Overall we identified seven studies that examined psychopathology symptom scores that included measures of psychosis, mood, aggression and cognitive function. The HGDH Reference Green, Tohen, Hamer, Strakowski, Lieberman, Glick and Clark16 study, a treatment trial of olanzapine v. haloperidol in first-episode schizophrenia, and the Sydney-A study Reference Degenhardt, Tennant, Gilmour, Schofield, Nash, Hall and McKay21 were the only studies to measure change in symptom scores from baseline to follow-up or adjust for baseline scores.
Positive symptoms
In the Sydney-A study, Reference Degenhardt, Tennant, Gilmour, Schofield, Nash, Hall and McKay21 cannabis use was associated with a small increase in BPRS score that persisted after adjusting for prior BPRS scores. In the HGDH study, cannabis misuse was not significantly associated with a change in the Positive and Negative Syndrome Scale (PANSS) total score from baseline to follow-up in either of the two trial arms of the study. Reference Green, Tohen, Hamer, Strakowski, Lieberman, Glick and Clark16 However, change in score was less in both arms for the cannabis misuse group compared with non-users, though no combined analysis of the two trial groups was presented, thereby reducing statistical power.
Regular cannabis use at baseline was associated with increased level of positive symptoms at follow-up in the South London Hospitals study, Reference Grech, van Os, Jones, Lewis and Murray14 and in the Homburg study Reference Caspari20 cannabis misuse was associated with 2 of 12 symptom sub-scales examined (increased thought disturbance and hostility). Cannabis was not associated with the positive symptom sub-scale of the PANSS in the Madrid-B study Reference Arias Horcajadas, Romero and Calo19 or with scores on the Scale for the Assessment of Positive Symptoms (SAPS) in the Manchester study. Reference Stirling, Lewis, Hopkins and White15
Negative symptoms
Regular cannabis use was not associated with negative symptoms scores in the South London Hospitals, Reference Grech, van Os, Jones, Lewis and Murray14 the Manchester, Reference Stirling, Lewis, Hopkins and White15 or the Homburg Reference Caspari20 studies. However, an association between cannabis dependence and a reduced score on the PANSS negative symptom scale at follow-up was observed in the Madrid-B study. Reference Arias Horcajadas, Romero and Calo19
Other measures
Cannabis misuse was not associated with depression score in the Sydney-A study, Reference Degenhardt, Tennant, Gilmour, Schofield, Nash, Hall and McKay21 with anxiety or depression sub-scales used in the Homburg study, Reference Caspari20 or with Overt Aggression Scale score in the Madrid-A study. Reference Arango, Calcedo, Gonzalez and Calcedo18 Neurocognitive ability at follow-up was greater on five out of nine sub-scales in people who had used cannabis at baseline in the Manchester study. Reference Stirling, Lewis, Hopkins and White15
Results for measures of response to treatment
A variety of other outcomes reflecting response to treatment were investigated in these studies. These included symptom score defined response to treatment, Reference Green, Tohen, Hamer, Strakowski, Lieberman, Glick and Clark16 length of in-patient stay, Reference Grace, Shenfield and Tennant22 course of illness, Reference Grech, van Os, Jones, Lewis and Murray14 presence of deficit schizophrenia, Reference Stirling, Lewis, Hopkins and White15 global assessment scale (GAS) score, Reference Caspari20 service contact, Reference Stirling, Lewis, Hopkins and White15 productivity or employment, Reference Pencer, Addington and Addington12,Reference Caspari20 marital status, Reference Caspari20 living alone Reference Caspari20 and quality of life. Reference Pencer, Addington and Addington12
In the South London Hospitals study Reference Grech, van Os, Jones, Lewis and Murray14 there was some evidence that individuals who had used cannabis frequently at baseline had a more continuous course of illness than people who had not used cannabis regularly (crude odds ratio (OR)=2.4, 95% CI 0.9–6.9). Cannabis was not associated with treatment non-response in the HGDH study, Reference Green, Tohen, Hamer, Strakowski, Lieberman, Glick and Clark16 or with service contact or GAS score in the Manchester Reference Stirling, Lewis, Hopkins and White15 and Homburg Reference Caspari20 studies respectively.
In the Calgary study, Reference Pencer, Addington and Addington12 cannabis use at baseline was associated with decreased levels of productivity or employment, as well as reduced quality-of-life measures at follow-up. There was suggestive evidence that people who used cannabis in the Homburg study Reference Caspari20 were more likely to be single and less likely to be employed or living alone than individuals who did not use cannabis, though none of these associations were statistically significant.
Two studies also observed associations between cannabis use and improved outcomes; in the Manchester study Reference Stirling, Lewis, Hopkins and White15 a state of deficit schizophrenia was less common in people who had used cannabis at baseline compared with non-users, and in the Sydney-B study Reference Grace, Shenfield and Tennant22 there was weak evidence that cannabis use at baseline was associated with a clinically important shorter duration of admission (13 days v. 21 days, P=0.07).
Results for adherence to treatment
Three studies examined cannabis use in relation to subsequent adherence to treatment. In the Madrid-B study Reference Arias Horcajadas, Romero and Calo19 cannabis dependence at baseline was associated with non-adherence during follow-up. A dose-response model of increasing baseline cannabis use in the CEPP study Reference Coldham, Addington and Addington13 was also associated with increased levels of non-adherence in the crude analysis, though this association was eliminated after adjustment for confounding. Similarly in the Navarra study, Reference Martinez-Arevalo, Calcedo-Ordonez and Varo-Prieto17 continued cannabis use during follow-up (but not use of cannabis at baseline only) was weakly associated with reduced adherence compared with non-users (36% v. 67%, P=0.06).
Methodological quality of included studies
We assessed the degree to which the potential effect of confounding and bias were minimised within each study (summarised in Table 1). Although a number of factors could have led to overestimation of the true causal association between cannabis use and poorer outcomes of psychosis in these studies, perhaps the most likely of these is confounding, particularly by use of alcohol and other drugs; and baseline measures of illness severity and level of functioning (that may have led to reverse causation effects).
Table 1 Summary of quality of studies included for outcomes in psychosis
| Cohort label | Response rate at baseline | Loss to follow-up, % | Masking of outcome assessment | Adjusted for baseline illness severity | Adjusted for alcohol and other drugs | Impact of adjusting for confounders |
|---|---|---|---|---|---|---|
| Brisbane Reference Hides, Dawe, Kavanagh and Young McD9 | 88% of participants approached | 15 | No | Yes | Yes | Association persisted after adjustment, but no indication as to extent of confounding |
| Calgary Reference Pencer, Addington and Addington12 | Not mentioned | 29 | No | No | No | Some associations eliminated after adjusting for symptoms at follow-up |
| CEPP Reference Coldham, Addington and Addington13 | All first 200 incident cases | 22 | No | No | Adjusted for alcohol use | Association with baseline cannabis use eliminated by adjustment |
| HGDH Reference Green, Tohen, Hamer, Strakowski, Lieberman, Glick and Clark16 | Not mentioned | 0.4 | No | Yes for 1 of 2 outcomes (measured score change) | No | Not assessed |
| Homburg Reference Caspari20 | All those identified as cases included | Cannabis misuse group, 31; non-misuse group, 33 | No | No | Some adjustment, as cases excluded if mainly used drugs other than cannabis | Not assessed |
| Madrid-A Reference Arango, Calcedo, Gonzalez and Calcedo18 | 63 of 70 eligible (90%) | 0 | No | No | No | Not assessed |
| Madrid-B Reference Arias Horcajadas, Romero and Calo19 | Not mentioned | 0 | No | No | 1 of 5 outcomes studied was adjusted for alcohol/other drugs | Not assessed |
| Manchester Reference Stirling, Lewis, Hopkins and White15 | 100% | 38 | No | No | No | Associations for 2 cognitive tests eliminated after adjusting for age at onset; 5 other associations persisted |
| Melbourne Reference Wade, Harrigan, Edwards, Burgess, Whelan and McGorry11 | Not mentioned | 18 | No | Yes | Yes | Reduced estimate by 15% |
| Navarra Reference Martinez-Arevalo, Calcedo-Ordonez and Varo-Prieto17 | 94% | 17 | No | No | No. Cannabis use was associated with alcohol and other drug misuse in sample | Not assessed |
| South London Hospitals Reference Grech, van Os, Jones, Lewis and Murray14 | 119 with baseline data from 227 consecutive admissions (52%) | 18 | Masked to baseline cannabis; unclear if masked to follow-up use | No | No | Reduced estimates by approximately 20–80% |
| Sydney-A Reference Degenhardt, Tennant, Gilmour, Schofield, Nash, Hall and McKay21 | Not mentioned | 22 for psychosis outcome observations | No | Yes | No, but alcohol and other drugs had non-significant effect on outcome and thus omitted from final model | Reduced estimate by 35% |
| Sydney-B Reference Grace, Shenfield and Tennant22 | Out of 167 patients, 45 had drug screens done (27%) | 0 | No | No | No other illicit substances detected in urine for whole of sample, but no adjustment for alcohol misuse | Not assessed |
Of the 13 studies included in this review, only five studies (Brisbane, Reference Hides, Dawe, Kavanagh and Young McD9 Melbourne Reference Wade, Harrigan, Edwards, Burgess, Whelan and McGorry11 , Navarra, Reference Martinez-Arevalo, Calcedo-Ordonez and Varo-Prieto17 Sydney-A Reference Degenhardt, Tennant, Gilmour, Schofield, Nash, Hall and McKay21 and HGDH Reference Green, Tohen, Hamer, Strakowski, Lieberman, Glick and Clark16 ) made any adjustment for measures of illness severity at baseline. Only three studies (Brisbane, Reference Hides, Dawe, Kavanagh and Young McD9 Melbourne Reference Wade, Harrigan, Edwards, Burgess, Whelan and McGorry11 and Madrid-B Reference Arias Horcajadas, Romero and Calo19 ) adjusted for both alcohol and other drug use, though this was for only one of the five outcomes in the Madrid-B study. In the Homburg study Reference Caspari20 some adjustment for alcohol and other drug use was done by exclusion of individuals mainly using drugs other than cannabis. In the Sydney-A study, Reference Degenhardt, Tennant, Gilmour, Schofield, Nash, Hall and McKay21 alcohol and other drug use were excluded from the adjusted model as they were not associated with the outcome, and were therefore unlikely to have substantially confounded the relationship with cannabis. One study adjusted for alcohol use only (CEPP), Reference Coldham, Addington and Addington13 and one other (Sydney-B) Reference Grace, Shenfield and Tennant22 made some adjustment for other drug (but not alcohol) use.
A further potential mechanism by which overestimates of association may have resulted is by lack of masking of exposure status when assessing outcome. In fact, a statement that outcome measurement was performed masked to cannabis exposure was only evident in one of the studies (South London Hospitals). Reference Grech, van Os, Jones, Lewis and Murray14 A summary of study quality issues in relation to the different outcomes studied is presented below.
Studies of relapse or rehospitalisation
Relapse of psychosis as defined for the Brisbane Reference Hides, Dawe, Kavanagh and Young McD9 and Melbourne Reference Wade, Harrigan, Edwards, Burgess, Whelan and McGorry11 studies (and as implied for the Navarra study Reference Martinez-Arevalo, Calcedo-Ordonez and Varo-Prieto17 ) required a change in symptom severity between baseline and follow-up, reducing, though not eliminating, the possibility of confounding by factors related to illness severity. Furthermore, in the Brisbane study Reference Hides, Dawe, Kavanagh and Young McD9 results were adjusted for a wide range of potentially important confounders, including baseline symptoms, alcohol and drug use, and measures of social functioning and family environment. Results for the Melbourne study Reference Wade, Harrigan, Edwards, Burgess, Whelan and McGorry11 were adjusted for baseline symptoms and for alcohol and other drug use, and results for the Navarra study Reference Martinez-Arevalo, Calcedo-Ordonez and Varo-Prieto17 were adjusted for adherence and life stresses.
None of the studies that examined rehospitalisation however made any adjustment for illness severity at the time of discharge from the index admission, or for markers of social function or socio-demographic status (apart for adjustment for age and gender in the Homburg study Reference Caspari20 ).
Studies of symptom scores
For the studies that examined symptom scores as outcomes, only two studies adjusted for baseline scores or examined change in scores from baseline to follow-up (Sydney-A Reference Degenhardt, Tennant, Gilmour, Schofield, Nash, Hall and McKay21 and HGDH Reference Green, Tohen, Hamer, Strakowski, Lieberman, Glick and Clark16 ). None of the five other studies reporting associations between cannabis and symptom severity at follow-up took into account levels of symptom severity at baseline. In the Manchester study Reference Stirling, Lewis, Hopkins and White15 there was a strong association between cannabis use and fewer neurological soft signs at baseline, though this was not adjusted for in the associations reported with neurocognitive outcomes.
Studies of response to treatment
With regard to measures of response to treatment, course of illness as examined in the South London Hospitals study Reference Grech, van Os, Jones, Lewis and Murray14 implies change of symptom severity during follow-up and adjustments for age, gender and ethnicity were also made in this study. In the Manchester study Reference Stirling, Lewis, Hopkins and White15 there were no significant baseline differences in negative symptoms or social adjustment, indicating that the association with deficit schizophrenia is perhaps unlikely to be confounded by these. No adjustments for baseline severity of illness, or any other confounders however were made in the Sydney-B study, Reference Grace, Shenfield and Tennant22 where a weak association with length of in-patient admission was reported. Similarly in the Calgary Reference Pencer, Addington and Addington12 and Homburg Reference Caspari20 studies, no adjustments were made for level of productivity or quality of life at baseline, or for baseline marital, employment or accommodation status, when examining for associations with these measures at follow-up.
Studies of adherence
The CEPP study Reference Coldham, Addington and Addington13 results were adjusted for a wide range of potentially important confounders, but no adjustment for any confounders in relation to this outcome was done in the Madrid-B Reference Arias Horcajadas, Romero and Calo19 or the Navarra Reference Martinez-Arevalo, Calcedo-Ordonez and Varo-Prieto17 studies.
Discussion
As far as we are aware this is the first systematic review to examine whether use of cannabis has a detrimental effect on outcome in people suffering from a psychotic illness. We found relatively few longitudinal studies that have examined this hypothesis.
Use of cannabis was associated with increased relapse or rehospitalisation and with decreased treatment adherence fairly consistently across the studies that examined these outcomes. Associations between cannabis and psychotic symptoms or other psychopathology scores were more inconsistent, with only three studies presenting evidence of association with increased positive symptoms and one study reporting an association with decreased negative symptoms. Definitions for relapse in two studies Reference Hides, Dawe, Kavanagh and Young McD9,Reference Wade, Harrigan, Edwards, Burgess, Whelan and McGorry11 were based on increases in positive symptoms scores however, and both of these studies found evidence that cannabis use led to increased relapse. Evidence for associations with other measures of treatment response was also quite discrepant, with some studies reporting negative outcomes of reduced quality of life, productivity or a more continuous illness course in people using cannabis, but other studies reported associations with positive outcomes including shorter in-patient stays and reduced deficit schizophrenia in cannabis users.
Examination of non-causal explanations for association
The most important consideration when attempting to interpret the findings of this review is the methodological quality of the studies included in relation to bias and confounding. Only four of the thirteen studies (Brisbane, Reference Hides, Dawe, Kavanagh and Young McD9 Melbourne, Reference Wade, Harrigan, Edwards, Burgess, Whelan and McGorry11 Sydney-A Reference Degenhardt, Tennant, Gilmour, Schofield, Nash, Hall and McKay21 and HGDH Reference Green, Tohen, Hamer, Strakowski, Lieberman, Glick and Clark16 ) made any attempt to adjust for baseline illness severity measures. Access to, and use of cannabis, may be associated with premorbid level of functioning or illness severity, both of which are also likely to be related to clinical outcome.
Furthermore, even basic socio-demographic characteristics such as social class or gender that are associated both with poor outcome Reference Lauronen, Miettunen, Veijola, Karhu, Jones and Isohanni28,Reference Munk-Jorgensen and Mortensen29 and with cannabis use Reference Hofler, Lieb, Perkonigg, Schuster, Sonntag and Wittchen30,Reference von Sydow, Lieb, Pfister, Hofler and Wittchen31 were only adjusted for in six of the studies. Most studies made no adjustment for alcohol or other drug use, though these are strongly associated with detrimental mental health outcomes Reference Jane-Llopis and Matytsina32,Reference Regier, Farmer, Rae, Locke, Keith, Judd and Goodwin33 and are therefore also likely to be confounders. They are also likely to serve as markers of other factors such as personality traits relating to risk taking and adherence with medical advice that could further confound the relationship between cannabis and outcome in psychosis. These methodological issues are particularly pertinent given that non-adherence is likely to result in poorer clinical outcomes generally.
Although some adjustment for confounding was undertaken in a number of studies, only the Melbourne, Reference Wade, Harrigan, Edwards, Burgess, Whelan and McGorry11 South London Hospitals Reference Grech, van Os, Jones, Lewis and Murray14 and Sydney-A Reference Degenhardt, Tennant, Gilmour, Schofield, Nash, Hall and McKay21 studies presented both crude and adjusted estimates that enable us to gauge the potential impact of confounding in these studies. Estimates were attenuated by between 15% and 80%, although only a limited number of potentially important confounders were adjusted for in these studies. Given that the range of confounders adjusted for was rather incomprehensive in most of the studies included in this review, confidence that the associations reported are specifically due to cannabis in these studies must therefore be rather low.
Clinical opinion has long been that use of cannabis results in a worse outcome in people with psychotic illnesses and the original study in this field by Linszen et al Reference Linszen, Dingemans and Lenior25 lent strong support to this view. This makes it particularly important that studies measure outcomes masked to cannabis exposure status to avoid overestimation of association due to observer measurement bias. The South London Hospitals study Reference Grech, van Os, Jones, Lewis and Murray14 was the only study to report such masking.
Reverse causation was unlikely to have been a problem as we only included longitudinal studies in this review. The Calgary, Reference Pencer, Addington and Addington12 CEPP Reference Coldham, Addington and Addington13 and South London Hospitals Reference Grech, van Os, Jones, Lewis and Murray14 studies however also included some results for measures of cannabis use at follow-up. Results for these measures (that showed stronger associations than for use at baseline only) were therefore omitted, as these associations could have resulted, in part, from reverse causation effects. On the other hand, results for individuals using cannabis at baseline but not at follow-up are likely to be underestimates of true effects of cannabis as they ignore the impact of continued use. However, following such a conservative approach for these studies seemed preferable in order to firmly establish direction of causality.
If cannabis is indeed a risk factor for causing psychotic illnesses Reference Moore, Zammit, Lingford-Hughes, Barnes, Jones, Burke and Lwis5 then it is perhaps surprising that these studies of the effects of cannabis on clinical outcome are so inconsistent, especially as our assessment of methodological quality suggests that insufficient attention was paid to addressing overestimation of causal effects in these studies.
Possible reasons for lack of evidence for association
It is also possible that studies underestimated the true impact of cannabis on the outcome of psychosis. Random misclassification of data is probably the most likely reason for underestimation of association. In particular, self-report measures of cannabis use are unlikely to accurately reflect the dose of psychoactive cannabinoids available in the brain given variations in potency of cannabis used, and amounts of cannabinoids inhaled and metabolised. Misclassification in accuracy of reporting is also likely, although in the Brisbane study Reference Hides, Dawe, Kavanagh and Young McD9 self-reports of cannabis use (as used in the analyses) showed good reliability with drug screens in a subsample of the cohort (Cohen's kappa=0.90). Repeated and detailed assessment of cannabis exposure during the follow-up period, but before outcome measurement, would help to reduce misclassification. However, most studies to date have used rather limited assessments of cannabis exposure, measured only before the follow-up period started.
Furthermore, loss to follow-up in cohort studies tends to be greater for individuals who have more severe mental health problems and for those with substance misuse. Such an effect of differential attrition would have led to underestimation of the strength of any association. The median loss to follow-up for these studies was 17% (range 0–38%), though the only study (Homburg Reference Caspari20 ) that examined whether attrition was different for cannabis using and non-using groups reported minimal difference across the two groups.
Apart from the possible effects of bias, lack of statistical power could also have led to lack of evidence for associations in some of these studies. None of the studies that failed to observe associations between cannabis use and clinical outcomes presented power calculations. If we assume that 20% of patients with psychosis relapse over a 1-year period if they do not use cannabis and 40% relapse if they use cannabis regularly, and that 25% of patients use cannabis regularly, then a power calculation indicates that a sample size of over 250 people with psychosis is required to have 80% power to detect this effect. This calculation is based on a large difference in relapse rates between cannabis users and non-users, and yet only one of the studies included in this review meets this required sample size.
Finally, it is also possible that variation in the diagnostic composition of the participants with psychoses across different studies, as well as differences in the measures of clinical outcome and definitions of cannabis exposure, might partly explain the diverse and at times conflicting results reported. For example, all of the associations between cannabis use and better outcomes were in studies that included individuals with any psychotic diagnosis, while studies of people with schizophrenia or related spectrum disorders appear to show more consistent evidence for poorer outcomes in those using cannabis.
Limitations
Although we identified a large number of potential studies for inclusion, most studies were not set up to directly address the aim of this review and were not able to meet our criteria for inclusion. As well as the possibility that we missed some studies during our searches, we excluded a large number of studies by requiring studies to be of longitudinal design as these provide the most reliable evidence for causal association in the absence of randomised controlled trials. Furthermore, the rather insubstantial nature of what constitutes a ‘poor clinical outcome’ means that it is more difficult to summarise results of studies in this review compared, for example, with reviews where disease incidence is the studied outcome.
We also excluded a large number of studies that examined the effects of substance use in general rather than specifically use of cannabis. As cannabis is the most frequently used illicit substance in most countries it could be argued that results for substance use (that excludes alcohol or tobacco) mainly reflect the effects of cannabis. However, even in such situations, the possibility of strong confounding by other drugs remains. Furthermore, although uncommon, substance use may at times be dominated by stimulant drugs such as amphetamines or cocaine. Reference Mueser, Yarnold and Bellack34
Implications for future research and clinical practice
Given that psychoactive compounds within cannabis can cause or increase psychotic experiences secondary to intoxication effects, Reference D'Souza, Abi-Saab, Madonick, Forselius-Bielen, Doersch, Braley, Gueorguieva, Cooper and Krystal2,Reference D'Souza, Perry, MacDougall, Ammerman, Cooper, Wu, Braley, Gueorguieva and Krystal3 and independently of such effects, Reference Moore, Zammit, Lingford-Hughes, Barnes, Jones, Burke and Lwis5 it is very plausible that cannabis might lead to increased positive symptoms and subsequently relapse or rehospitalisation in people with psychosis. Indeed, there is a widespread belief among psychiatrists that such a detrimental effect does exist. We were surprised how little empirical evidence is currently available to support this view. Our assessment of methodological quality suggests that although insufficient attention was paid to addressing overestimation of causal effects, low statistical power to observe associations was also likely to have been present in many of the studies.
Despite the clinical consensus and the plausibility of harmful effects, we believe it is important to establish whether cannabis is harmful, and if so, what the size of any harmful effect is. Trials of interventions for reducing cannabis use in people with psychosis may provide stronger evidence of possible detrimental effects of this drug, as this would be independent of confounding effects.
We also need to know what kinds of outcome are particularly susceptible to the influence of cannabis; whether clinical, employment status or other aspects of social functioning. An understanding of the effects of different potency preparations as well as of pattern of exposure is also required. Comparing the effects of cannabis with other psychoactive drugs would enable clinicians and patients to prioritise harm reduction plans.
Although most of the associations reported were with markers of poorer clinical outcome, some studies also reported better outcomes in individuals using this drug. It is possible that cannabis has differential effects on different outcomes, for example worsening positive symptoms but improving negative ones. Further research on the specific effects of cannabis on such outcomes may help our understanding of aetiological mechanisms, further elucidate why some individuals with psychosis choose to use cannabis, and suggest approaches that might be used by clinicians to engage this problem. Understanding to what extent any associations are mediated through indirect pathways resulting in poor outcome, such as reduced adherence, may also enable more specific targeting of focused interventions to improve long-term care in people with psychotic disorders.
Insufficient empirical evidence exists at present to adequately examine whether cannabis use has detrimental effects on the outcome of psychotic disorders, or to determine the pathways by which such effects are mediated, although these are important and clinically relevant questions.
Future studies to address these uncertainties should be of longitudinal design, with repeated measures of psychopathology, use of cannabis, alcohol and other substances, as well as baseline measures of function, illness severity and other characteristics that are known to be associated with poorer outcome in schizophrenia. Appropriate analyses should ensure that reverse causation effects are minimised, for example by using time-lagged measures of cannabis use where repeated measures are available. Reporting of both crude and adjusted estimates, with specific reporting as to which specific confounders have the greatest impact on the results would aid design of future studies. Use of clearly defined diagnostic categories and a more universal approach to measures of cannabis exposure and outcomes (that are measured masked to exposure status) would further help with interpreting and summarising future study findings.
Unlike the situation that exists for examining causal effects of cannabis on incidence of psychosis, adequately powered longitudinal studies of outcome of people with psychosis should be, in comparison, relatively easy to carry out given the widespread availability of large clinical samples.
Acknowledgements
We would like to thank the authors of the papers we considered for inclusion in our review; Cheryl Corcoran, Marie-Odile Krebs, Martin Lambert, John Stirling and Ingrid Melle for their helpful correspondence; and Blanca Bolea, Jorge Gaete and Juan Santos for help with translation. We are especially grateful to Jean Addington and Darryl Wade for providing us with additional data for us to consider for inclusion in our review.
This work was funded by the Department of Health, UK. S.Z. is funded through a Clinician Scientist Award funded by the National Assembly for Wales.





eLetters
No eLetters have been published for this article.