Introduction and Background
“We’re like a bridge over a river. You don’t think about us, but we make it much easier to get to the other side.” – Dr Ted Wun, CTSA hub Director at UC Davis
Since the beginning of the Clinical and Translational Sciences Award (CTSA) Program, a key emphasis has been placed on improving the quality and efficiency of clinical and translational research. The CTSA Program aims to promulgate innovations, both scientific and operational, that improve the efficiency, effectiveness, quality, safety, impact, and informativeness of clinical and translational science, as emphasized in the most up-to-date version of the Funding Opportunity Announcement (FOA, PAR-21-293) [1]. The range of innovation in translation should occur across the translational research spectrum, encompassing first-in-human studies, implementation in medical practice, and dissemination towards community health. CTSA hubs are required to demonstrate expertise and capabilities in human subjects protections and responsible conduct of research, as well as show continuous quality improvement (CQI). The new FOA includes a newly proposed CQI program at each CTSA hub, which is expected to engage in a strong ongoing cycle of data collection and decision-making to gradually improve both program and research processes. However, no document regarding these objectives for the CTSA, even prior to the pandemic, offers a clear explanation of what quality and efficiency mean. This lack of clarity is severely limiting to any effort aimed at achieving excellence.
Challenges associated with quality and efficiency of translational research are part of the “translational science agenda,” “major rate-limiting translational problems that are the focus of translational science,” and “scientific priorities for translational science” as suggested by Dr Christopher Austin [Reference Austin2], former Director of the National Center for Advancing Translational Sciences (NCATS). The scientific priorities for translational science he proposed and spotlighted include clinical trial designs, clinical trial operational efficiency, clinical trial participant recruitment, retention, and diversity, and single/harmonized Institutional Review Board (IRB), among other key priorities. It was precisely the recognition of this need that brought about the Trial Innovation Network (TIN) as a collaborative approach dedicated to identifying and removing critical roadblocks to execute better, faster, more cost-efficient clinical trials while simultaneously emphasizing the desire to study and understand the innovative process behind trial design and implementation [3]. In fact, from March 2020 to December 2020, the TIN’s three Trial Innovation Centers, Recruitment Innovation Center (RIC), and 66 CTSA hubs provided 29 COVID-19-related consults, including 6 trial participation expressions of interest and eight community engagement studios [Reference Greenberg, Poole and Ford4].
What is Quality and Efficiency of Translational Research in Non-Pandemic Times?
Translation is the “process of turning observations in the laboratory, clinic, and community into interventions that improve the health of individuals and the public” [Reference Austin5]. In the steps of clinical trials, efficiency has often been conflated with saving of cost and time [Reference Bhatt6]. So, with translation, the question becomes: How can we speed up the process of turning observations into interventions while conserving resources? However, focusing on cost and time can compromise quality and slow down the implementation and dissemination of interventions to improve health. As shared by a CTSA quality/efficiency expert and stakeholder, “a reduction in quality can lead to the promulgation of implicit biases and inequities, a lack of rigor in trial design and the collection of data, or arriving at incorrect conclusions which then promulgate disinformation. Removing quality from the equation doesn’t just slow down research; it damages research, causes participants to assume unnecessary risk, and undermines the public’s trust.” (CTSA quality expert/stakeholder, email communication, January 25, 2022). In clinical trials, Good Clinical Practice (GCP) is the universal quality and safety standard for conducting clinical trials, encompassing data integrity and human participant protections [7]. The Clinical Trials Transformation Initiative (CTTI), a public-private partnership co-founded by Duke University and the U.S. Food and Drug Administration (FDA), has defined quality as “the absence of errors that matter to decision-making – that is, errors which have a meaningful impact on the safety of trial participants or credibility of the results (and thereby the care of future patients)”[8]. According to CTTI [9], “a high-quality, efficient clinical trial – one that can lead to fewer errors, lower expenses, faster enrollment, and more reliable results in your research” is supposed to demonstrate such critical characteristics as “clear and meaningful scientific questions, fit-for-purpose designs, ongoing dialogue with all stakeholders early and often.” In the context of ongoing discussions among our CTSA colleagues regarding research quality vs. efficiency, it is both interesting and commonsensical that efficiency is an important element, aspects of which must be considered and weighed against other factors in clinical trials that have been designed with CTTI’s quality approach.
What is Quality and Efficiency of Translational Research in Pandemic Times?
As Scott Gottlieb [Reference Gottlieb10], former commissioner of the FDA, correctly pointed out, “The US response to COVID-19 suffered from our inability to quickly enroll and complete rigorous studies that could provide more definitive evidence around not only which treatments worked to reduce the symptoms and severity of COVID-19, but also decisively establish which drugs were not effective.” The CTSA Consortium is in a unique position of helping meet the immediate needs of the research and translational science community, as well as of those of society writ large, only if we can figure out a nimble, flexible infrastructure that can adapt to the rising challenges of current and future pandemics, and if our infrastructure does not sacrifice quality in the pursuit of efficiency.
The development of mRNA vaccines, although exceptional and indicative of the great scientific progress of our current times, has also shed light on the hurdles – in terms of regulatory mechanisms, supply chains, and, more importantly, societal trust – that prevent faster development pathways, especially at a global scale where any attempt at convergence necessitates much broader and deeper collaboration [Reference Knezevic, Liu, Peden, Zhou and Kang11]. However, the focus on COVID and the restrictions of COVID may yield longer-term implications that point to a need for a different model. Many advances in the speed of initiating and conducting COVID trials came from the transfer of responsibilities from other projects initiated before the pandemic. During the initial months of the pandemic, researchers worried that widespread and lengthy shutdowns would slow the pace of scientific discovery. Being away from their labs for weeks or months would mean having to restart certain projects or abandon experiments [Reference Joseph12]. Ideal efficiency would have been a research enterprise that could not only sustain pre-existing research but also advance pandemic-specific research. Is that even possible?
This unprecedented public health emergency has underscored the necessity of generating cross-trial and cross-disease insights through data harmonization, an integrated learning clinical trials system, and advancing capacities for system flexibility and surge capacity [Reference Austin2]. The CTSA RIC COVID-19 Recruitment + Retention Toolkit [13] includes multiple strategies designed to address the pandemic’s nationwide disruption of clinical trial recruitment and implementation due to closing and reopening of study sites, social distancing, and personal protective equipment (PPE) requirements, remote work options for staff, and balancing existing studies with those of urgent need. However, further insights can still be gleaned from the lived experiences of the last few years.
Methods
This article is part of the Environmental Scan of Adaptive Capacity and Preparedness (AC&P) [Reference Volkov, Ragon, Doyle and Bredella14], implemented by a special AC&P Working Group approved by the CTSA Steering Committee in 2021. The overall purpose of the AC&P Working Group and this scan was not to evaluate, test, generalize, quantify, or validate any hypotheses, approaches, or interventions, but rather to identify, curate, analyze, and share examples of practices, challenges, and lessons learned related to how CTSA hubs have used their expertise, resources, and collaborations to advance clinical and translational research during emergency. The AC&P Working Group utilized the data that had been – or was planned to be – collected through existing mechanisms, aligning with and contributing to the CTSA goals and processes. Data sources included the following: scientific publications and white papers on CTSAs’ (and other) AC&P-related activities; a sample of diverse (in size, maturity, location) CTSA hubs’ websites: public stories, news, highlights, measures; NCATS and other clinical and translational science organizations’ websites; de-identified information from select CTSA hub Research Performance Progress Reports (RPPRs); and feedback of CTSA expert/community reviewers and other stakeholders [Reference Volkov, Ragon, Doyle and Bredella14].
Relevant challenges, lessons learned, practices that work, cases, and recommendations from CTSA hubs and other institutions are presented and discussed within the five domains of the adapted Local Adaptive Capacity (LAC) Framework presented in Table 1 [Reference Volkov, Ragon, Doyle and Bredella14,Reference Jones, Ludi and Levine15]. Being overlapping, interdependent, and interacting by design, each of the domains serves a special role in hubs’ adaptive capacity.
Table 1. Local Adaptive Capacity domains and their features (adapted from Jones et al.) [Reference Volkov, Ragon, Doyle and Bredella14,Reference Jones, Ludi and Levine15]

Results
Asset Base
The LAC Framework defines “Asset Base” as the preexistent and available infrastructure and other assets with which to respond to a constantly evolving situation. In terms of innovating processes and enhancing quality and efficiency, the CTSA Consortium is advantageously positioned to provide resources to researchers, participants, communities, and other stakeholders in ways that maximize the benefits of translational science. It is not an overstatement to say that the COVID-19 pandemic has been a challenging “stress test” for the system. Next, we will share some examples of the accomplishments, newly identified hurdles or vulnerabilities in our processes and capabilities, and lessons learned from the current pandemic to be better prepared for future emergencies.
To some, the CTSAs have been the “unsung heroes” of the COVID-19 pandemic [Reference Tomiyoshi16]. Despite effectively being the “infrastructure of research,” the CTSAs often have trouble explaining their role, even to medical audiences. During the pandemic, the activities performed at CTSA hubs have become more visible since they cover the gamut of research operations: from mining electronic health records and providing clinical facilities for conducting clinical trials to patient recruitment and even assisting in blood draws of COVID-19 patients who were also enrolled in COVID-19 treatment trials. At the UC Davis CTSA, other examples of their service portfolio during the pandemic include creation of a resource that allows researchers from the five UC Medical Centers to share COVID-19 patient samples for research purposes; coordination with the Center for Health Technology to create or refine secure electronic and virtual methods for communication with patients; and continuous extraction of medical records and information categorization for researchers to keep up with the evolving depiction of the disease and its symptoms. Two innovative uses of assets that characterized the successful adaptation of the UC Davis CTSA hub to the public health crisis were the formation of a clinical trial review committee, coordinating, preventing overlap, and avoiding overwhelming both health care teams and patients, and the creation of a so-called “Tiger Team” to guide the continuation of in-process, crucial clinical trials by guaranteeing the adoption of appropriate and necessary safeguards and safety protocols.
In their analysis of a survey of pre-approval mechanisms of the regulatory support units to facilitate access to investigational agents/medical devices during the COVID-19 pandemic, Gravelin et al. [Reference Gravelin, Wright and Holbein17] shared lessons they learned about the following key assets: deep regulatory knowledge is critical during a crisis; electronic submissions capabilities to the FDA are necessary for efficient access to experimental therapeutics; and a nimble reallocation of regulatory and legal resources is essential to enhance patient access during periods of high demand for investigational drugs and/or devices.
In yet another CTSA survey, Croker et al. [Reference Croker, Patel and Campbell18] analyzed feedback from 60 CTSA hubs for a better understanding of the biobanking strategies and challenges in response to the COVID-19 pandemic. According to the authors, the CTSA hubs were able to leverage their infrastructure and expertise, responding quickly to the biorepository needs of researchers during the pandemic, with “a major shift in biorepository model, specimen acquisition, and consent process from a combination of investigator-initiated and institutional protocols to an enterprise-serving strategy.”
In an effort to shorten the time frame of the translational science continuum (from bench to bedside), the University of Minnesota Medical School and the M Health Fairview system identified three pathways that could increase quality and efficiency for the CTSA [Reference Mendez19]. According to Dr Benson, the first step is to “develop a shared purpose,” whereby leadership and community partnerships may rely on key performance indicators (such as participant accrual rates, thematic study triage, and other research metrics) to help researchers pivot their activities rapidly and overcome traditional barriers to research. These indicators readily provide an accurate description of the institutional resources available to mobilize and provide best care to patients. Second, “communicate systematically” during the crisis in order to combat stress, confusion, and misinformation among patients and the general public. Evidence-based reviews of ongoing research, weekly collaborative problem-solving meetings, and daily research briefings to leadership were recommended. Finally, “leveraging big data and technology” is of great importance to offer new, potential therapies; rapid access to care to those who need it most urgently; and efficient allocation of scarce resources. For instance, M Health Fairview system partnered with UnitedHealth Group in Minnetonka, MN who owned the world’s largest COVID-19 patient database and together they launched a multisite trial, spearheaded by UMN Medical School, to study the use of metformin as preventative treatment of recently infected SARS-CoV-2 outpatients. These experiences led to a recommendation to utilize a “learning health system” approach, which connects scientists and their research directly to healthcare providers and the patients for whom they provide care.
One of the most pressing challenges brought about by the COVID-19 pandemic was the urgent need to provide mass testing to the American people. With this goal in mind, the National Institutes of Health (NIH) launched the Rapid Acceleration of Diagnostics (RADx) tech program [20], and with it came the related need to evaluate COVID-19 testing devices and the opportunity for the CTSA Consortium to build upon its well-established trans-institutional networks of multidisciplinary research capacity building. This was reflected in the work done at the Georgia CTSA by Drs. Nehl and Hellman when creating a “Test Verification Core” (TVC) to mobilize existing infrastructure and pivot resources to accommodate expedited evaluations through a number of key decision points, ranging from biorepository, specimen processing lab to biosafety level 3 labs, and COVID-19 testing drive-throughs [21]. None of the then-current Standard Operating Procedures (SOPs) had ever accounted for such processes, but the Georgia team managed to rapidly adapt by stepping back, looking at the long trajectory, studying milestones, and stamping those milestones with their collaborators and contributors along the way. This unprecedented achievement in evaluation processes yielded seven important recommendations on what is needed to effectively respond to crises (the Adaptive Capacity Case 1) [Reference Nehl, Heilman and Ku22].

Institutions and Entitlements
Among other enablers of quality and efficiency of research described in this article, adaptive capacity and preparedness of clinical and translational science organizations have been bolstered by an appropriate and responsive institutional environment. This has allowed fair access and entitlement of the CTR community to key assets provided by institutions and their partners and collaborators. At the University of Minnesota, the Clinical Research Support Center (CRSC) is administered by the UMN CTSA hub [23]. This allows researchers to access clinical research experts from the University and collaborators. Useful expertise and resources made available to investigators include regulatory, recruitment, informatics, contracts, financials, clinical research, IRB preparation, biostatistics, among a list of 20 research support groups. UMN’s CRSC was able to mobilize its resources rapidly and effectively to drastically reduce the clinical trial start-up process during the COVID-19 pandemic by relying on its strong asset base and pre-established collaborations [23].
At the New York University Langone Health’s CTSA hub preparedness, derived in part from their Hurricane Sandy experience in 2012, enabled more adaptability to the COVID-19 pandemic [24]. Looking to the CTSA hub for guidance, NYU Langone Health implemented regulatory and clinical measures (the Adaptive Capacity Case 2).

Another program that was able to leverage prior restructuring towards adaptive capacity was the Harvard Catalyst’s Connector program. The transition of their clinical research centers (CRCs) to a service-based model in 2018 allowed the Connector program to assist clinical investigators with study design, protocol development, IRB review, specimen collection, data gathering, analysis, and dissemination of results and offer translational support and give investigators opportunities to collaborate [Reference Barlow25]. After supporting hundreds of investigators for two years, the program was able to direct its translational navigation teams to focus on COVID-19 studies.
The CTSA hub at the University of Chicago continues to oversee that institution’s locally supported Clinical Research Center program [26]. That program was able to flexibly assign staff and space to the start-up and implementation of COVID-19 vaccine trials, allowing those studies to rapidly launch and begin enrollment even before the principal investigators had hired study staff, thus cutting months off the timeline for these critical trials.
In the responses to the survey of clinical research professionals (CRPs) administered by Case Western Reserve University CTSA hub, the universal theme was adaptability across institutions experiencing the immense impact of the COVID-19 situation on their research activities [27]. Promptly responding to the pandemic restrictions, all areas of research administration continued providing essentially uninterrupted service to the research teams in their communities while taking measures to ensure staff safety – allowing safe and efficient access to and coordination of key institutional assets.
During the COVID-19 pandemic, CTSA pharmacies experienced serious challenges, including drug shortages threatening patient care, PPE shortages threatening the health and lives of pharmacy staff and their ability to safely compound drugs, and lockdowns requiring alternative strategies to deliver drugs to patients, according to MacArthur et al. [Reference MacArthur, Bentur and MacArthur28] Key practices that worked in this field (and may endure) included dramatic increase in off-site work by pharmacists, loosening of restrictions on supplying medications to research participants on protocols, novel methods of interacting with contract research organizations and research study monitors, expanded vaccination and clinical practice. The authors recommend preparation for future public health challenges, pointing out that many of the CTSA pharmacy-related changes were initially prompted by drug and PPE shortages, so as soon as a health emergency is recognized, response and adaptation measures can be implemented on an institutional basis to stockpile drug, PPE and other supplies, and control their use locally.
One of the lessons learned from a healthcare system that is part of a clinical and translational science network can be that an interplay of local and regional considerations and capacities may influence clinical outcomes and linked research when dealing with a pandemic emergency. Craig Coopersmith, MD, director of the Emory Critical Care Center, shared the view that intense planning, the skill of care teams, and a later arrival of COVID-19 illness in Georgia likely influenced the outcome of a lower number of deaths than what most researchers internationally reported for critically ill COVID-19 patients using mechanical ventilation [29,Reference Auld, Caridi-Scheible and Blum30]. He explained that “As soon as it became clear that COVID-19 was spreading globally, our care teams got to work establishing an organizational structure, acquiring equipment, aligning resources across a large health system, preparing personnel and developing clinical protocols… We were able to build on the foundation of our pre-existing care models and infrastructure of the Emory Critical Care Center to ready our teams to fight the COVID-19 pandemic.”
Underscoring the importance of institutional biorepositories that historically have not been sufficiently funded to support patient-oriented research, Croker et al. [Reference Croker, Patel and Campbell18] argued that utilization of the institutional biorepository model may help minimize delays in human subjects regulatory approvals and, with well-developed institutional linking procedures, decrease difficulties in linking specimens to detailed clinical information. Some action items suggested by the authors for better preparedness and adaptation include federal rapid response grants for deployment of biobanking resources in case of global health crises; fostering trusting relationships among investigative and clinical care teams and developing a shared “play book” for facilitating research specimen collections in the context of a crisis; promoting and supporting biospecimen sharing across CTSA hubs that may propel high-impact research with sufficient scale, statistical power, and positive patient outcomes (e.g., as an extension of other CTSA collaborations, such as N3C, the National COVID Cohort Collaborative).
As discussed in Wigginton et al., [Reference Wigginton, Cunningham and Katz31] disruption of research due to the COVID-19 pandemic disproportionately affected researchers at high-risk for health issues (e.g., older, immunocompromised) and those with child- and family-care concerns. Institutions needed to not only mitigate the risk of returning to work but also alleviate workforce disparities that predominantly affect women, lower-income staff, and trainees. Proposed adaptive strategies to support and prepare the research workforce for future serious disruptions include promotion and tenure clock deferrals, alternative work arrangements, trainee fellowship support, and optimized paid/unpaid leave policies. These issues are also discussed to greater extent in the Integrating Special and Under-represented Populations article [Reference Hoyo, Shah, Dave and Volkov32] and the Training of Translational Workforce paper (E-Scan of TS Workforce, unpublished data, 2022).
Knowledge, Information, and Learning
The challenging task of improving quality and efficiency of any target or system requires the system’s ability to collect, analyze, and disseminate knowledge and information in support of implementation, improvement, adaptation, and other activities. Building the field’s capacity in this and other areas, the CTTI seeks to develop and drive adoption of practices that will increase the quality and efficiency of clinical trials. The CTTI website (https://ctti-clinicaltrials.org/) provides a number of useful publications, case studies, and other resources. Specific to this domain, CTTI conducted a survey of members of the clinical trials ecosystem to identify and synthesize useful lessons for conducting clinical trials during the COVID-19 pandemic. The resulting list of such practices includes a good deal of “knowledge, information, and learning-” related strategies and activities (the Adaptive Capacity Case 3) [Reference Shannon33,34].

The University of Minnesota CTSA hub worked together with researchers and research participants, healthcare providers, and community partners to accelerate research discoveries to deal with the pandemic and beyond, support researchers and research participants, and strengthen their adaptive knowledge and information capacity in the following ways[35]:
-
Sharing their knowledge, information, and expertise with dozens of COVID-19 research study teams by guiding them on study protocols, regulatory requirements, informatics, biostatistics, financial management, recruitment, and more to support the University’s critical COVID-19 research.
-
Creating faster access for researchers to high-quality COVID-19 data via developing a special registry that houses the electronic medical records of COVID-19 patients while protecting patients’ privacy and using best practices for securing, managing, and provisioning access to data of those who chose to share their records for research purposes.
-
Making it easier to find important information for potential COVID-19 study participants. For instance, a special COVID-19 filter has been added to StudyFinder, a website that helps Minnesotans identify UMN studies that need volunteers [36].
-
Providing COVID-19-focused research training. Specifically, UMN CTSI collaborated with the Human Research Protection Program (HRPP) and Fairview Research Administration to create a “Research 101” training video for Bethesda Hospital’s COVID-19 workers [23].
Among numerous CTSA examples of creating opportunities for sharing experiences, learning from others, interdisciplinary networking, and finding potential collaborators are Georgia CTSA hub’s Speed Networking on COVID-19 via Zoom session, where attendees presented their research in 3 minutes or less with the goal of sharing knowledge with colleagues and seeking new collaborators [37] and an informational session on “How to Recruit Subjects into Human Trials: Recruiting, Enrolling and Conducting Research Virtually” [38]. In another instance of rapid learning, adopting, adapting, and sharing knowledge with stakeholders, the Southern California CTSA hub developed a “COVID-19 Recruitment and Operations Guide” [39]. Based on presentations and content from the 2020 USC Regulatory Science Symposium (October 2020) and reopening guidelines from Emory Healthcare and Georgia CTSA, their toolkit suggests important considerations for promoting and ensuring diversity in clinical research, engaging better uses of technology by participants, and operational how-tos for doing high-quality, efficient, and equitable research during the pandemic time.
Knowledge, information, and learning cannot be restricted to the academic environment. Stanford’s CTSA-funded Office of Community Engagement sponsored eight virtual Town Hall meetings (in English and Spanish), which were attended by thousands of community members. At these Town Halls, health experts provided the public with evidence and resources needed to augment understanding of key COVID-19 issues. Given the heightened community interest in research studies, a COVID Study Directory was launched to enhance engagement with research participants [Reference O’Hara40].
Innovation
The CTSA network has helped the clinical and translational enterprise alter the course of the pandemic by offering an enabling environment to foster innovation, experimentation, and the ability to explore pragmatic solutions to overcome challenges and take advantage of new opportunities. The following are examples of how CTSA hubs initiated, promoted, and supported promising research initiatives in the fight against COVID-19 and beyond.
Georgia Clinical & Translational Science Alliance demonstrated its ability to find quick, pragmatic solutions when its Rapid Response Team coordinated 48-hour approval for treatment of coronavirus patients [41]. In January 2020, utilizing lessons from the response to H1N1, Zika, and Ebola, the Georgia CTSA Quality & Efficiency program finalized their SOP for the Rapid Response Team to expedite high-priority studies of experimental therapeutics for pre-award approval. Rapid, effective implementation of studies and treatment were bolstered by robust SOPs, proactive identification of key personnel, and cross-departmental collaboration real-time together and in parallel (e.g., IRB, the Office of Clinical Research, Grants and Contracts).
The Case Western Reserve University CTSA hub, interested in how the pandemic was affecting clinical research professionals (CRPs) across the spectrum, surveyed CTSA hub-affiliated CRPs seeking to gain feedback and perspectives grounded in their first-hand experiences [27]. While researchers were halting or modifying operations, the hub partners were processing the changes and assisting investigators in navigating new options like electronic consent, shipping study drugs to participants, and starting in-home research visits. Respondents also reported that most staff operations were successfully transitioned to remote conduct, while observing some extra positive outcomes associated with such transition.
To further boost urgently needed experimentation and innovation, the University of Minnesota CTSA hub utilized a number of pragmatic strategies to both overcome and study the pandemic challenges (the Adaptive Capacity Case 4) [23].

The Michigan Institute for Clinical & Health Research and hub partners established the Center for Drug Repurposing (CDR) back in 2019 with the purpose of finding new uses for existing drugs and clinically evaluated compounds that have already cleared key steps in drug development pathways, such as safety testing in humans. Repurposing existing therapeutic interventions may reduce discovery times through having established safety profiles and reduced regulatory burden [42]. For instance, a study from CDR used artificial intelligence-powered image analysis of human cell lines during infection with the novel coronavirus and revealed several drug contenders already in use for other purposes – including one dietary supplement – that have been shown to block or reduce SARS-CoV-2 infection in cells [Reference Mirabelli, Wotring and Zhang43]. According to Jonathan Sexton, PhD, one of the senior authors on the published findings, these therapies were ready for phase two clinical trials as their safety had already been established [42].
The University of Minnesota Clinical Research Support Center's (CRSC’s) proactive and responsive approach to research support demonstrated capacity for real-time adaptability to future needs and emergencies, leading to the development of the CRSC Rapid Study Start-up process, a collaborative effort with the University research community to get research up and running faster and more efficiently [Reference Odlaug, Crevel and Tosun44]. Utilizing CRSC’s “all hands on deck” approach coupled with the Center’s smooth transition from a fully in-person support center to a virtual environment, experts from their CTSA hub, in collaboration with the UMN Masonic Cancer Center Clinical Trials Office, helped with all aspects of initiating the “Phase 1 Cell Therapy Trial for COVID-19” study, providing support for study planning and coordination, biostatistics, financials, IRB submissions, regulatory issues, and more. As a result, the start-up time from concept to initiation was reduced to 45 days compared to the typical timeline of up to six months.
Flexible Forward-looking Decision-making and Governance
In their article depicting the strategies employed to rapidly develop and implement COVID-19 diagnostic testing, Jeffrey Moran and collaborators [Reference Moran, Kessler and Moylan45] discussed specific examples of how the CTSA Consortium adopted a team science approach to leverage interactions between the CTSA labs, state departments of health, and other state-associated labs to create a science- and state-based public health response to the pandemic. Their recommendations for how to effectively address future pandemics and how to influence future diagnostic testing methods and beyond are summarized in the Adaptive Capacity Case 5.

Decision-making entities may benefit from following a well-developed guidance, articulated in Lurie et al. [Reference Lurie, Manolio, Patterson, Collins and Frieden46], with actions for the research enterprise to take before and during a public health emergency. The guidance’s components and actions include identifying topic area experts and questions to address common scenarios and ensuring conditions for rapid data collection (inclusive of key generic study protocols and survey instruments pre-approved by IRB). There should be a pre-established, on-call research “ready reserve” of clinicians, scientists, and government, academia, industry experts. Response plans should detail processes for activating research response (including an “incident commander for research”). Potential research needs are to be prioritized, including likely knowledge gaps and research questions. Relatedly and importantly, concerns of affected communities must be understood, based on previous emergency experience and community-based research.
Even with the resources, effort, and intent to potentially implement such protocols, the broader system essentially ends up rediscovering the same needs and again calling for the actions to address them [Reference Greenberg, Poole and Ford4]. The ramifications of decisions during a pandemic result in a loss of scientific advancement in other ongoing, slow-moving syndemics that foster and accelerate the impact of current and future pandemics [Reference Griffith, Holliday, Enyia, Ellison and Jaeger47]. As of January 2021, 2043 trials registered with ClinicalTrials.gov were terminated, withdrawn, or suspended due to the COVID-19 pandemic [Reference Orkin, Gill and Ghersi48]. The troubling trend had continued, and by April 2022, 2930 trials registered with ClinicalTrials.gov were impacted by the pandemic, affecting more than 1.2 million participants and interrupting plans to recruit more than 5.9 million future participants [Reference Carlisle49]. Is this an outcome that was envisioned as a high-quality and efficiency outcome of the clinical and translational science enterprise? How might we envision an agile and nimble clinical and translational research enterprise that fosters the continued operations of this vast, complex enterprise – while addressing the needs of the pandemic?
While there are no perfect answers, there may be a way to learn how to frame the issue of quality and efficiency of translational science during a pandemic. Based on the information collected using the LAC model in this article, one is left questioning if the sole focus during a pandemic is to rapidly transform non-pandemic operations of the translational research enterprise into addressing the needs of the pandemic.
An important omission to quality and efficiency of research during the pandemic was a lack of discussion of how the impetus to pivot resources, keep the research enterprise going, and innovate – while searching for solutions to overcome the pandemic – had an unintended consequence of exacerbating structural health disparities. The overreliance on new technology for recruitment purposes, the dearth of easily accessible and/or diverse bio-data repositories, and the lack of bi-directional, culturally competent communication with Special and Underserved populations were detrimental to the CTSA hubs’ mission of delivering scientific solutions to all, going beyond the narrow scope of clinical trials, and advancing the CTSAs’ leadership role for more equitable healthcare [Reference Volkov, Hoyo and Hunt50,Reference Hoyo, Shah, Dave and Volkov32].
Paton & Buergelt [Reference Paton and Buergelt51] believe that disaster preparedness and response involve a two-pronged interactive goal of transformative capacity building and adaptive capacity, where "transformative" is a novel, level-shifting, discontinuous gain of capabilities, and where "adaptive capacity building" is sustained, socio-culturally embedded, and continuous. Translational science has seen both dynamics, where the iterative, slow process of the scientific method of questioning leads to better solutions for health and well-being (think in the COVID situation about the two decades of work to advance messenger RNA platforms for vaccine delivery) and where transformative capacities have occurred (think the re-use of quarantine/shelter-in-place from the Middle Ages to stop bubonic plague to support public health mitigation measures in the early days of the COVID-19 pandemic). Paton & Buergelt [Reference Paton and Buergelt51] propose a Community Engagement Theory based on fieldwork from prior natural disasters in Oceania. In their theory, achieving transformative and adaptive capacity in response to a disaster requires moving from community participation to collective efficacy to empowerment to trust. That movement is supported by knowing particular community properties (place attachment, sense of community, sense of social/group identity) and community-based leadership with the governance for constructive conflict scenario planning.
Implications and Conclusion
During the COVID-19 pandemic, the prevailing narrative of many commentators for reform of the vast US clinical and translational research enterprise is that the enterprise has never functioned as a single national coordinated system. As Angus [Reference Angus, Gordon and Bauchner52] commented, “each investigator network brings its own culture, methods, and operational features. Every decision requires agreement among numerous investigators, many of whom may have no prior experience working together.” It has led to statements that the “FDA and the NIH should have the authority to prioritize among therapies those that have the most promise and accelerate enrollment of studies to evaluate these high-priority medicines” [Reference Gottlieb10]. However, that narrative is not a new one; it has been explored after multiple other public health emergencies. Solutions are needed for how the clinical and translational research enterprise can improve quality and efficiency.
The former Director of the Centers for Disease Control and Prevention, Dr Frieden, and his collaborators [Reference Frieden, Lee, Bochner, Buissonnière and McClelland53] were astute in their understanding that “public programs have a greater chance if they have straightforward, easy to remember metrics.” A robust evaluation process must operationalize and capture the transformative and adaptive capabilities, where the "transformative" are new methods and the "adaptive" can be the measures of “objects” in the LAC model. Evaluation also needs to capture the key areas of community participation, collective efficacy, empowerment, and trust, as well as how they are modified by governance and by community affinity. And how to eventually spread the knowledge gains to other systems across the globe? One decade ago, the FDA recommended a four-step systems approach to the quality improvement of clinical trials, which can perhaps be applied to the broader operational paradigm for the clinical and translational research enterprise: (1) Say what you do, (2) Do what you say, (3) Prove it, and (4) Improve it [Reference Bhatt6].
Say what you do. The quality and efficiency of the US clinical and translational research should be carefully operationalized and based on the efficient and timely use of resources to reduce the errors which have a meaningful impact on the safety of trial participants or credibility of the results (and thereby the care of future patients). The essential nature of a resilient, nimble, and equitable research ecosystem during any pandemic must be emphasized [Reference Greenberg, Poole and Ford4,Reference Wigginton, Cunningham and Katz31]. Developing a disaster recovery plan and designating an emergency response team to carry out this plan can ensure operations are maintained in the event of a disaster [Reference Dotzert54].
Do what you say. Quality and efficiency can be advanced by integrating and optimizing the asset base, institutions and entitlements, knowledge and information, innovation, and flexible and forward-thinking decision-making and governance within the CTSA enterprise. There might be a need for a broader framework than LAC, which is one part of a comprehensive model for building community capacity for handling a disaster. An efficient clinical research network must be well-practiced with a track record of success prior to the pandemic [Reference Greenberg, Poole and Ford4].
Prove it. The number of ongoing, registered research studies actively enrolling that are suspended, terminated, or withdrawn during a pandemic will be no different than from in a non-pandemic state. While challenging, such a goal is not different from attempting to reduce hospital-acquired infections to zero. More resilient protocols to deal with emergent situations will be needed, such as contingency planning that was developed during the current pandemic.
Improve it. Reduce the number of ongoing, registered studies that are suspended, terminated, or withdrawn due to a pandemic to as close to zero as possible. Incentivizing stronger ties between public health agencies and academic research institutions is needed to ensure that decision-making at institutions and across communities is guided by the best available research for improvement [Reference Wigginton, Cunningham and Katz31]. Improvements in tagging research studies in clinical trial registries with key potential impacts on minoritized populations and with the distribution of anticipated numbers of under-represented research participants in clinical research are necessary. Such enhancements could reduce the risk of closure of clinical trials that would advance health equity.
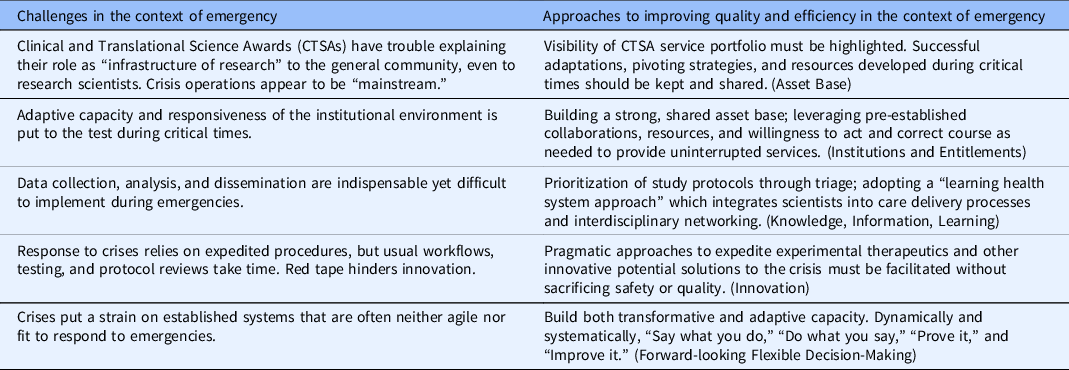
Significant lessons were learned and relearned based on the COVID-19 pandemic experiences. However, true quality and efficiency of the clinical and translational research enterprise will require a deeper appreciation of how communities as a whole, and the translational research community in particular, implement processes that reduce the suffering associated with local, national, and worldwide disasters. In Table 2, we summarize a set of challenges for the work of innovating processes to improve quality and efficiency during the times of emergency, as well as some strategies to build adaptive capacity to be able to address those barriers. It is by no means a comprehensive list of generalizable aspects; it is rather a good starting point, emphasizing a strong need for further, deeper research in this emerging area of science. Such research could include how the properties of the individual CTSA hubs (e.g., hub's region and size) may affect local resilience and adaptive capacity during a crisis. While the observations from this environmental scan (including innovative and enhanced, local and widespread approaches) are not intended to generalize to all settings, they can help CTSA hubs and other institutions develop strategies for better response and adaptation.
Table 2. Some challenges for improving quality and efficiency in the context of emergency and approaches to address them (derived from the Adaptive Capacity & Preparedness E-Scan)
Acknowledgements
The authors wish to extend a special thank you for the expert review and stakeholder feedback provided by Daniel Bouland (Clinical and Translational Research Institute, UC San Diego, CA, USA), Gerald Moose Stacy (Institute for Translational Medicine, the University of Chicago, Chicago, IL, USA), and Daniel Weisdorf (Deputy Director, the University of Minnesota Clinical and Translational Science Institute, Minneapolis, MN, USA). This work was supported, in part, by the following National Institutes of Health (NIH) National Center for Advancing Translational Sciences grants: UL1TR002389, UL1TR001422, UL1TR001442, UL1TR003142, UL1TR002494. The authors acknowledge the support of the University of Rochester Center for Leading Innovation and Collaboration (CLIC), grant U24TR002260. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosures
The authors have no conflicts of interest to declare.




