Training in hand hygiene and professional feedback are core elements of infection prevention.Reference Schwappach and Gehring1 According to the World Health Organization (WHO), adherence among healthcare providers to recommended hand hygiene procedures ranges from 5% to 89%, with an overall average of 38.7%. To provide these competencies and intensify multiprofessional collaboration, regular training in hygiene proficiencies and team dynamics is necessary.2 Unfortunately, motivation to participate in these programs is low among healthcare workers such as medical students.Reference Qasmi, Mahmood Shah, Wakil and Pirzada3 As a consequence, hospitals use extrinsic motivation to ensure participation. Unfortunately, participation alone does not guarantee learning, and learning does not necessarily ensure good behavior in everyday life.
In a multicenter study, we identified an overplacement effect, a subtype of the overconfidence effect, as a possible barrier to incentive motivationReference Mubeen and Reid4 to attend to infection prevention and communication programs.Reference Bushuven, Juenger, Moeltner and Dettenkofer5 Overconfidence effects are impressive, popular and common heuristic errors found in multiple situations.Reference Dunning, Heath and Suls6, Reference Moore and Healy7 The effect is divided into 3 subeffectsReference Moore and Healy7:
1. Absolute overconfidence (overestimation): the belief that one is better than is quantifiable.
2. Relative overconfidence (overplacement): the belief that one is better than the median of a group.
3. Overprecision – the excessive belief concerning the correctness of one’s own assessment.
In the previously reported regional study on overconfidence in infection prevention in a communal healthcare association,Reference Bushuven, Juenger, Moeltner and Dettenkofer5 selection bias was one of the main limiting factors. Therefore, we tested our hypothesis in a nationwide group of participants. This article reports the results of our approach and adds more insight into heuristic influence on learning motivation in infection prevention.
Methods
The cross-sectional anonymous online-study was conducted over 12 months from 2017 to 2018. We used a previously tested a 6-point Likert questionnaire (Subjective Assessment of Training in Infection Prevention Skills version 2) with 61 items. This questionnaire was checked in a test phase for reliability and validity using factor analysis and varimax rotation. Items consisted of short statements like “I am well educated in providing feedback.” Answers were chosen from a list of 0 “completely disagree” to 5 “completely agree.”
After consultation with the institutional review board (State Medical Chamber Baden-Wuerttemberg, Stuttgart), the questionnaire was provided by e-mail by Enuvo GmbH Zuerich. Internet protocol (IP) addresses were blinded to the investigators. Participant recruitment was accomplished using announcements in social media (eg, Facebook, LinkedIn); using different Internet forums of medical professionals; and by e-mail to hospital hygiene departments, medical academies, and risk managers. Furthermore, members of the QuMIK (Quality and Management in Hospitals) network of Baden-Wuerttemberg were requested by e-mail to forward the survey link.
A statistical analysis of the completed forms was conducted with Excel software (Microsoft, Redmond, WA) and XLSTAT software (Addinsoft SARL, NY) using Mann-Whitney U, Friedman, and Wilcoxon tests. Significance was set at 0.05, with adjustments for multiple testing. A correlation analysis was conducted with Spearman rank correlation. Because of the anticipated selection bias for this study, the central questions were clustered at the beginning of the survey for a “completer/dropout” comparison. Subgroup analyses focused on age, sex, profession, education level, and workplace.
Results
Participants
Of 767 participants in >20 professions, 421 completed the survey. Of these, 63.9% were female. Most completers (45.6%) were 26–40 years old, and 15.9% were undergraduates. Professions of participants included physicians (36.6%), nurses (22.6%), paramedics (11.6%), and surgical nurses (11.2%). Also, 74.5% were employed in a hospital and 59.1% worked at tertiary-care hospitals.
Main results
Participants assessed their own level of education and adherence to clinical hand hygiene protocols to be better than those of students, colleagues of the same profession, and supervisors (Table 1 and Fig. 1). Effect sizes were moderate (Dz = 0.3–0.5) to strong (Dz > 0.5) for these findings. Recognition of indications of hand hygiene showed deficits for completers with “better than average” self-assessments: 15.1% did not recognize the need for hand hygiene before connecting a urinary catheter to a collection bag. Moreover, 21.5% of participants failed to identify the preparation of oral medication as an aseptic procedure, and 1.5% of participants failed to do so before vascular access. For ‘weaker’ indications, half of the participants believing themselves to have an above-average education found no indication for hand hygiene after using computer keyboards or after food consumption.
Table 1. Statistical Analysis of Selected Questionnaire Times with Mean, Standard Deviation (SD), Significance (P) and Intraindividual Effect Size (Cohen’s Dz) with Low (<0.3), Moderate (0.3–0.5) and Strong (>0.5) Effects
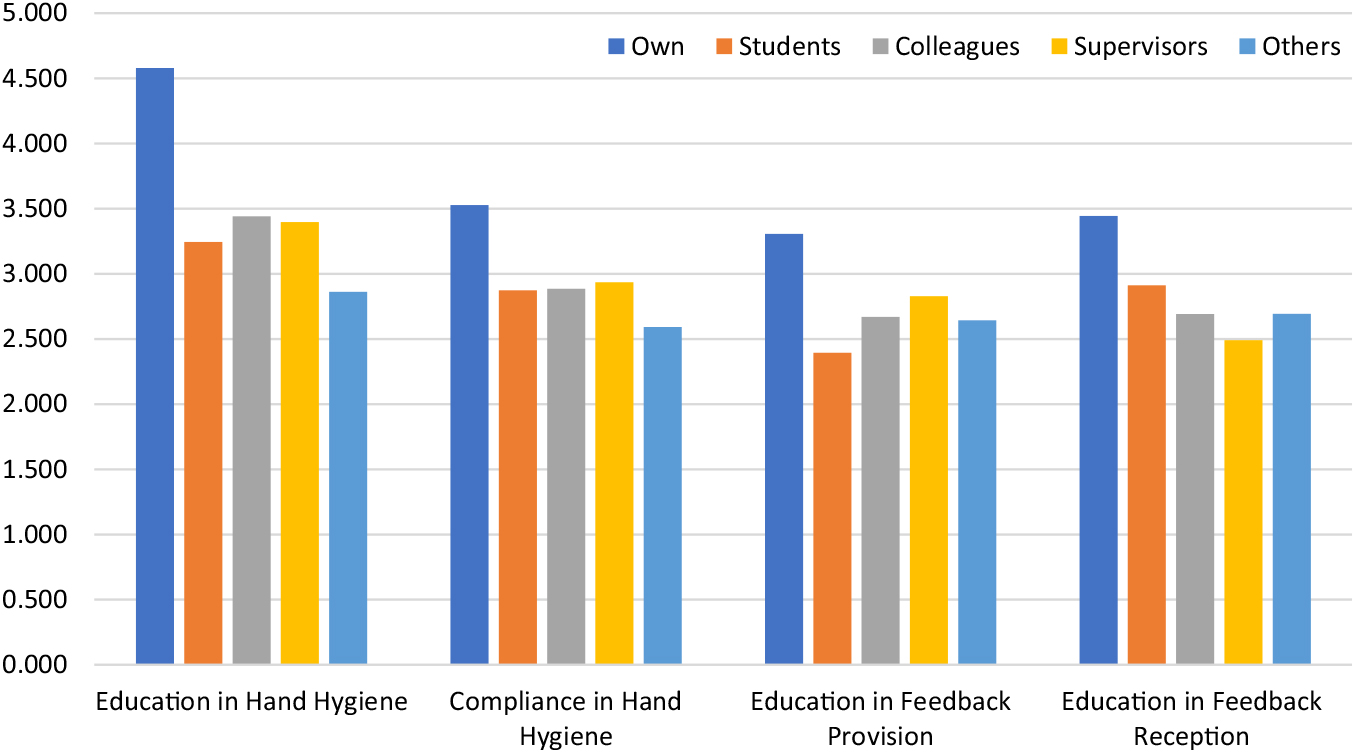
Fig. 1. Results of the assessment of one’s own and other’s education in hand hygiene and feedback competences. Assessment of one’s own skills was significantly higher in all item-comparisons.
Self-assessment correlated with subjective belief in participants’ own protocol adherence (P < .0001; r = −0.38). Participants with high self-assessments reported having skipped only a few hand hygiene occasions in the prior work week. Only 2.9% of the participants chose the realistic number of >10 per week. In contrast, 34.3% reported 100% compliance without errors or omissions.
High self-assessment in hand-hygiene significantly positively correlated with ratings of one’s own proficiency (r = 0.14–0.20) and the assessment of colleagues in the same profession (r = 0.12–0.20).
The ability to identify WHO criteria 1–3 showed no significant correlation with correct identification and self-assessment of education in hand hygiene. The only exception was the removal of contaminated clothes, which showed a weak positive correlation (P = .004; r = 0.14).
Self-assessment of providing feedback correlated positively with that for members of one’s own profession (r = 0.21–0.25) but not of other professions. Concerning feedback reception proficiency, a weak positive correlation between self-assessment and ratings of supervisors was detected (r = 0.10).
Regarding feedback provision and reception, half of the participants who rated themselves as having an above-average education reported low adherence to classical feedback rules. Reported corrective intervention when participants witnessed someone else skipping a hand hygiene occasion was either low or unrealistic: Only 8.6% of participants were realistic in answering that they omitted >10 feedback situationsReference Schwappach and Gehring1 per week. On the contrary, 39.7% reported having spoken up after every skipped occasion in their prior work week.
Subgroup analysis
Gender
There were no differences with respect to gender in assessment of one’s own or of others’ compliance and education. Women ranked the hand hygiene compliance of supervisors (P = .023) and feedback skills of students to be better (P = .005) than male participants did.
Age
We detected significant differences between participants below and above 40 years of age: Younger medical professionals rated themselves as better educated in feedback reception skills than did older participants (P < .001). Furthermore, younger persons rated students to be better educated in hygiene (P = .004) and to have better feedback reception skills (P = .002).
Professions
Four main professions were represented: physicians, nurses, paramedics and surgical nurses. Between them, no differences in their answers could be detected.
Students
Students (n = 67) showed higher ratings for their own capabilities in hand hygiene and feedback than colleagues and supervisors (P < .05). There was no correlation between the years of education and self-assessment or ratings of others (P > .05).
Workplace
No differences between participants working in primary, secondary, tertiary or university hospitals or in out-of-hospital settings were detected.
Completers versus dropouts
A comparison of completers versus dropouts showed no significant difference in the assessments of others (P > .05). For self-estimation items, completers rated themselves better than dropouts did (P = .028). Dropouts who terminated the survey early (directly after self-assessment, items 1–5) rated themselves inferior to those who dropped out later (P = .002; r = 0.13).
Discussion
To our knowledge, this is the first investigation in Germany to test for absolute and relative overconfidence in hand hygiene and feedback competence in interprofessional and intersectoral healthcare workers.
Our results show overestimation of one’s own education in hand hygiene and feedback: despite high self-assessment, participants failed to identify relevant WHO indications for hand hygiene. They were not able to rate the realistic occurrence of skipped occasions, and they showed relevant gaps in knowledge and behavior for feedback techniques.Reference Ramani and Krackov8
Second, we detected overplacement consistent with prior studies,Reference Bushuven, Juenger, Moeltner and Dettenkofer5–Reference Moore and Healy7 namely that participants rated themselves to be of above-average education and proficiency. Overplacement was higher in the national survey than in the data from the regional study.Reference Bushuven, Juenger, Moeltner and Dettenkofer5
Neither overplacement nor overestimation in students and supervisors were dependent on age, working place, profession, or education level. Previous studies have shown differences along gender lines in assessment of one’s own skills, with women tending to rate themselves lower than men (although both are overconfident).Reference Blanch, Hall, Roter and Frankel9 In this study, this tendency was not detected.
These effects, together with the low tendency to speak up in case of erroneous or skipped hand disinfections, indicates that risks in infections prevention and medical education may affect patient safety. First, the detection of overestimation indicates that hand hygiene and feedback are mistakenly perceived to be “easy” skills. Challenging skills normally generate underestimation.Reference Moore and Healy7 Trainings in subjectively easy abilities may therefore be considered time-consuming and a waste of resources. Training motivation mainly depends on 3 aspects: value, self-efficacy, and controllability.Reference Pelaccia and Viau10 With a subjectively high level of education, the value of further training may be estimated to be low, especially if ‘others’ are perceived to be in need of more in-depth education.
Second, both effects emerge early in education and are independent of gender, age, profession and workplace. To compensate for overconfidence and collaboration impairment, educators could use interprofessional teaching formats to address all professionals, regardless of their educational level. Due to the high resistance of overconfidence, classical learning formats are known to fail to compensate for it. This indicates the need for reflexive and individual training.
Third, witnessed errors in hygienic hand disinfection were ignored, although feedback training was perceived to be satisfactory. This finding is consistent with results reported by Schwappach et al.Reference Schwappach and Gehring1 Although reflection by feedback is a core aspect of learning, feedback may be perceived to be negative and even harmful in the presence of overconfidence. With overconfidence developing in early stages of professional education, it seems to be advisable to integrate feedback and self-reflection as early as possible in medical education of infection prevention.
In addition, the missing correlation between self-assessment and quality of practice shows that self-assessment in infection control may be flawed and therefore unsuitable for the measurement of realistic training demands.
This study has several limitations including selection bias, which is a typical limitation of all surveys. Although the selection bias never can be ruled out completely, this study combined with the preceding workReference Bushuven, Juenger, Moeltner and Dettenkofer5 and findings in other settingsReference Dunning, Heath and Suls6 increase credibility and generalizability of the hypothesis. The comparison of drop-outs and completers as a surrogate parameter for “interest” or “motivation” is questionable because one’s attitude toward completing a survey is not completely related to interest but may also be linked to other social factors (eg, politeness).
In conclusion, our results show relative and absolute overconfidence for infection prevention among healthcare providers. The effects were independent of age, profession, educational level, working place and gender. Self-assessment did not correlate with actual education in hand hygiene and feedback. Although we found some limitations, flawed self-assessment and overconfidence in infection prevention competences should be considered relevant elements in the development and design of training and curricula for healthcare providers.
Author ORCIDs
Stefan Bushuven 0000-0001-6272-0714
Acknowledgments
We thank Dr. Alexandra Patin, PhD for proofreading the manuscript.
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.




