1. Introduction
Gambling disorder (GD) is characterized by repeated compulsive problematic gambling behavior accompanied by unsuccessful and uncontrollable urges to keep gambling, which leads to considerable distress and impairment [Reference American Psychiatric Association1]. Risk factors for developing GD include male gender, poor school performance and cognitive distortions surrounding gambling [Reference Yakovenko, Hodgins, el-Guebaly, Casey, Currie and Smith2, Reference Dowling, Merkouris, Greenwood, Oldenhof, Toumbourou and Youssef3]. Several distinct types of interventions exist to treat GD [Reference Petry, Ginley and Rash4–Reference Maynard, Wilson, Labuzienski and Whiting7], with cognitive behavior therapy (CBT) being one of the most widely used approaches [Reference Muench, Goslar, Hofmann, Leibetseder and Laireiter8].
Multiple studies have assessed which factors are the most related to the effectiveness of CBT in GD patients, particularly when considering clinical state immediately after the end of the intervention and during the first months following the intervention [Reference Tolchard9, Reference Gooding and Tarrier10]. Short-term effectiveness appears to be particularly related to psychopathological state at the beginning of the therapy (particularly lower depression and anxiety levels), followed by gender, older age, lower baseline gambling severity levels, lower comorbidity, and a more functional personality profile [Reference Merkouris, Thomas, Browning and Dowling11–Reference Jiménez-Murcia, Granero, Fernández-Aranda, Arcelus, Aymamí and Gómez-Peña13]. Long-term recovery has not been so widely studied, but it seems to be most associated with lower levels of psychopathology, sensation seeking and GD severity at the start of treatment [Reference Müller, Wölfling, Dickenhorst, Beutel, Medenwaldt and Koch14, Reference Mestre-Bach, Steward, Granero, Fernández-Aranda and Mallorquí-Bagué15].
Despite the evidence supporting the usefulness of CBT in the treatment of GD, some systematic reviews have underscored the paucity of evidence of effective treatment programs, and controversy has emerged in the interpretation of results [Reference Cowlishaw, Merkouris, Dowling, Anderson, Jackson and Thomas16, Reference Pickering, Keen, Entwistle and Blaszczynski17]. The very definition of recovery remains unclear and many outcome measures incorporate broader domains extending beyond disorder-specific symptoms. Few long-term studies on gambling relapse have been conducted, the durability of the therapeutic gains is unknown and the evidence about the effects of benefits from integrative therapies has been obtained from few studies with limited sample sizes [Reference Aragay, Jiménez-Murcia, Granero, Fernández-Aranda, Ramos-Grille and Cardona18, Reference Ledgerwood and Petry19]. Moreover, although controlled studies have shown positive results in the treatment of GD, indicating the effectiveness of interventions, many of these studies had multiple limitations [Reference Petry, Zajac and Ginley5, Reference Merkouris, Thomas, Browning and Dowling11, Reference Challet-Bouju, Bruneau, Victorri-Vigneau and Grall-Bronnec20]. Namely, the lack of a single comprehensive scale to measure all aspects of gambling recovery hinders uniform reporting practices across the field [Reference Pickering, Keen, Entwistle and Blaszczynski17] and the heterogeneity of populations markedly differ across studies, leading to discrepant results [Reference Petry, Ginley and Rash4]. There is progress still yet to be made as approximately 50% of individuals affected by GD will continue to have symptoms throughout life [Reference Müller, Wölfling, Dickenhorst, Beutel, Medenwaldt and Koch14, Reference Mestre-Bach, Steward, Granero, Fernández-Aranda and Mallorquí-Bagué15].
The capacity of CBT to treat GD has been analyzed through variable-level techniques (such as the correlation models, regression techniques, analysis of variance or path analysis), which are focused on examining the relationships between the potential variables (in this case, predictors and therapy outcomes) by considering the individuals as a group. In this sense, variable-level analyses tend to isolate clinically significant features in which individuals differ, since they are centered on the analysis of the potential correlational structure of the variables, their stability over time, and their predictive capacity for predetermined criteria. Therefore, variable-level approaches do not provide information on person-specific, intra-individual clinical states, nor on person-specific intra-individual dynamics.
An alternative to variable-level approaches are person-centered approaches (such as mixed growth modeling or developmental trajectories). These techniques focus attention on the intra-individual structure of variables with the aim of identifying groups of individuals who share particular attributes or relationships among attributes, with the consequent advantage of conceiving the individuals as a whole and not as the sum of isolated features [Reference Laursen and Hoff21, Reference von and Bogat22]. Although person-centered techniques have been used for exploring group differences in patterns of development, few studies have focused the study of GD based on developmental trajectories analyses [Reference Dowling, Merkouris, Greenwood, Oldenhof, Toumbourou and Youssef3,23–28]. To our knowledge only one study to date has been focused on GD trajectories after treatment [Reference Grune, Sleczka, Kraus and Braun29]. This person-centered approach would be in the line of precision treatments, adapted to the specific needs of each patient, their risk factors and the phenotypic characteristics of the patient’s disorder. This therapeutic perspective, based on the issue “which medication will work best for which patient” [Reference Mann, Roos and Witkiewitz30], is oriented to identify homogeneous subtypes of patients in order to predict response to treatment [Reference Kranzler and McKay31]. Thus, precision medicine is being extended to all areas of health, including mental health and addictions, improving prediction of response to treatment [Reference Evers32]. In this vein, Dowling et al. [Reference Dowling, Merkouris, Greenwood, Oldenhof, Toumbourou and Youssef3] identified several psychosocial risk factors associated with problem gambling such as sociodemographic variables, substance abuse, antisocial behavior, personality traits, the number of gambling activities and poor school performance. Moreover, other studies reported some variables associated with the poor treatment outcome failure as younger age [Reference Aragay, Jiménez-Murcia, Granero, Fernández-Aranda, Ramos-Grille and Cardona18], early age of onset and low school education [Reference Jiménez-Murcia, Granero, Fernández-Aranda, Arcelus, Aymamí and Gómez-Peña13], negative urgency [Reference Mestre-Bach, Steward, Granero, Fernández-Aranda and Mallorquí-Bagué15], high impulsivity levels [Reference Jara-Rizzo, Navas, Steward, Lopez-Gomez, Jimenez-Murcia and Fernandez-Aranda33], low coping skills, high sensation-seeking, low tolerance to boredom and craving [Reference Hodgins and el-Guebaly34]. Social support is also known to be associated with a positive response to therapy [Reference Jiménez-Murcia, Tremblay, Stinchfield, Granero, Fernández-Aranda and Mestre-Bach35–Reference Oei and Gordon37]. All these variables may contribute to the development of intervention programs based on precision medicine. As such, the aim of the present study was to estimate developmental trajectories of GD severity course during the 12 months following a manualized CBT program, and to identify the main variables associated with each trajectory.
This work used and integrate both person-centered and variable-level approaches: a) in the first stage, Latent Class Growth Analysis was used as a person-centered procedure, which aimed is to investigate how a single outcome variable (GD severity measured at multiple time points) defined a latent class model in which latent classes correspond to different growth curve shapes for the outcome variable; and b) in the second stage, the exploration of what sociodemographic and clinical variables were related with the previous empirical developmental trajectories based on analysis of variables procedures.
Based on the existing scientific evidence [Reference Dowling, Merkouris, Greenwood, Oldenhof, Toumbourou and Youssef3], we hypothesized that distinguishable GD trajectories would be latent in our sample, and that poor progress in gambling recovery would be related to poorer pre-treatment psychological state and more maladaptive personality profiles [Reference Jiménez-Murcia, Del Pino-Gutiérrez, Fernández-Aranda, Granero, Hakänsson and Tárrega38]. Cognitive distortions and higher levels of psychopathology have all been linked to greater levels of GD severity, and it is for these reasons we hypothesize that these very factors will distinguish our groups [Reference Yakovenko, Hodgins, el-Guebaly, Casey, Currie and Smith2, Reference Del Prete, Steward, Navas, Fernández-Aranda, Jiménez-Murcia and Oei39]. The identification of variables associated with the classification obtained in the latent class analysis could potentially allow for the development of more effective intervention programs for treatment-seeking patients.
2. Material and methods
2.1. Participants
The sample included consecutively admitted patients who met DSM-5 criteria for GD. Patients voluntarily sought outpatient treatment at a specialized Gambling Disorder Unit at Bellvitge University Hospital in Barcelona, Spain, and completed manualized a CBT intervention program between January-2007 and October-2017. Since the number of women was very low (n = 14) and the high asymmetry in the distribution of the sex could bias results, only men were included in our analyses. Therefore, the final sample included n = 603 treatment-seeking male patients, aged between 19 and 75.
Table 1 includes a description of the sample at the beginning of the study (pre-treatment, baseline state).
2.2. Psychological assessment
The assessment included specific measures of GD, global psychopathology and personality traits. Table 1 includes the Cronbach’s alpha (α) coefficients estimated in the study sample for the questionnaires used.
2.2.1. Diagnostic questionnaire for pathological gambling according to DSM criteria
This 19-item questionnaire assesses the DSM-IV [Reference American Psychiatric Association40] diagnostic criteria for pathological gambling. Then, all patient diagnoses were reassessed and recodified post hoc via a computerized system and, in our analysis, only patients who met DSM-5 criteria for GD were included. Convergent validity with the external gambling scores in the original version was very good (r =.77 for representative samples and r =.75 for gambling treatment groups [Reference Stinchfield41]. Internal consistency in the Spanish adaptation used in this study was α =.81 for the general population and α =.77 for gambling treatment samples [Reference Jiménez-Murcia, Stinchfield, Alvarez-Moya, Jaurrieta, Bueno and Granero42]. In this study, the total number of DSM-5 criteria for GD was analyzed (α =.76 in the sample).
Table 1 Sample description at baseline (n = 603).
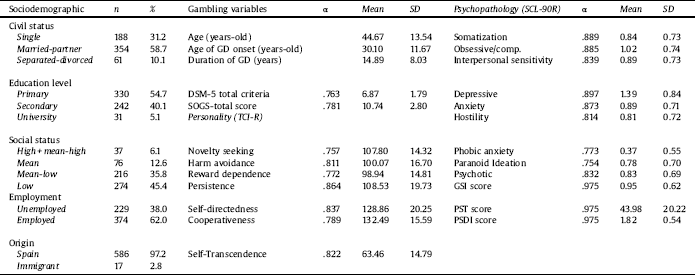
Note. SD: standard deviation. α: Cronbach’s alpha in the study sample.
2.2.2. South oaks gambling screen (SOGS)
This questionnaire is commonly used to evaluate gambling severity in research and clinical settings. It includes 20 items to assess cognitions and behaviors related to problem gambling. The validated Spanish version of the SOGS has shown high internal consistency (Cronbach’s alpha α =.94) and good test–retest reliability (r = 0.98) [Reference Echeburúa, Báez, Fernández and Páez43]. The internal consistency in the study sample was adequate (α =.78).
2.2.3. Symptom checklist-90 items-revised (SCL-90-R)
This is a 90-item self-report tool used to assess global psychopathology through nine primary symptom dimensions (obsessive-compulsive, depression, anxiety, hostility, interpersonal sensitivity, phobic anxiety, somatization, paranoid ideation and psychoticism) and three derived global indices [global severity index (GSI), positive symptom total (PST), and positive symptom distress index (PSDI)]. Good psychometrical properties were found in Spanish samples [Reference Derogatis44]. Internal consistency ranged between α =.77 for phobic anxiety to α =.98 for the global composite indexes in the study sample.
2.2.4. Temperament and character inventory–revised (TCI-R)
This is a 240-item tool used to measure four temperament dimensions (harm avoidance, novelty seeking, reward dependence and persistence) and three character scales (self-directedness, cooperativeness and self-transcendence) of personality. The adaptation of Spanish version of the questionnaire obtained good psychometrical properties [Reference Gutiérrez-Zotes, Bayón, Montserrat, Valero and Labad45]. Internal consistency ranged between α =.76 for novelty seeking and α =.86 for persistence in the study sample.
2.2.5. Other sociodemographic and clinical variables
Additional sociodemographic data were taken using a semi-structured, face-to-face clinical interview described elsewhere [Reference Jiménez-Murcia, Aymamí-Sanromà, Gómez-Peña, Álvarez-Moya and Vallejo46], including the following variables:
2.2.5.1. Socio-demographic variables
Sex, current marital status (single, married or with a stable partner, divorced or separated, widowed), social status by means of Hollingshead [Reference Edgerton, Melnyk and Roberts27], currently receiving personal income, currently in employment, receipt of social aid, number of co-inhabitants, presence of overcrowded living conditions (i.e., having to share a bedroom with a person who is not one’s partner), age (in years), personal income (monthly average, in euros) and family income (monthly average, in euros).
2.2.5.2. Current state of physical and mental health
Current treatment for physical health problems, smoking habit, alcohol consumption, consumption of illegal substances, regular consumption of non-prescription medication, current treatment for psychological problems, past treatment history for psychological problems, presence of close relatives who have or have had psychological problems requiring treatment
2.2.5.3. Gambling profile
Main gambling activity was identified and for each gambling activity, the following were measured: age of initiation, duration, frequency, bets (average and maximum), current treatment for gambling behavior, previous life history for gambling behavior treatment.
2.2.5.4. Gambling behavior
Total past debts accumulated by the subject due to gambling, total current debts accumulated by the subject due to gambling, cognitive distortions attributable to gambling (gambling expectations, illusion of control, predictive control, interpretative bias).
2.3. Procedure
All participants were assessed in two face-to-face clinical interviews by expert clinical psychologists with more than 15 years of experience in the field of behavioral addictions, who also guided the administration of questionnaires. In the first clinical interview, the psychologists or psychiatrists who attended the patient proposed participation in the project, providing informed consent, which was signed in the case of acceptance. The decision on participation in the study was autonomous and voluntary. The head of the project (SJM) ensured that the care or services they would receive at the hospital would not be affected regardless of their decision. In addition, if the patient decided to withdraw from the study once participation had begun and/or wanted to withdraw their data from the database, they could do so by contacting the head of the project. The therapist leading the CBT group gave the patients a calendar with all the scheduled sessions (including follow-up sessions) at the beginning of the treatment program. The same clinical psychologist (who did the first interview and the assessment) carried out the CBT therapy intervention and weekly case discussions were held between the therapists and the rest of the team at the Unit.
The present study was approved by the Ethics Committee of Bellvitge University Hospital and all patients provided signed informed consent. Psychological measures were obtained by experienced clinical psychologists at the Department of Psychiatry of Bellvitge University Hospital.
Data analyzed in this study correspond to data taken at the start of the CBT program, immediately following CBT, and measures obtained during the 12 months following the end of the program (data was obtained 1, 3, 6 and 12 months after the completion of the CBT program).
The Cognitive-behavioral therapy (CBT) intervention utilized in this study was carried out in a group format (averaging approximately 10 patients-per-group). It consisted of 16 weekly outpatient sessions lasting about 45 min each. The aim of the intervention was to train patients to implement CBT strategies in order to attain full recovery (defined as the absence of gambling episodes). The general topics addressed in the program included psychoeducation regarding GD (its onset and course, vulnerability factors, diagnostic criteria, bio-psychosocial models, etc.), stimulus control (such as money management and the avoidance of potential triggers), response prevention strategies (alternative and compensatory behaviors), the acquisition of new, healthy behaviors to replace GD, cognitive restructuring focused on illustrating and rectifying false beliefs of control over gambling, reinforcement and self-reinforcement, skills training and relapse prevention techniques. The therapists who conducted the groups are the same clinical psychologists who performed the first interviews and evaluations. These three therapists share the same background in CBT training, extensive experience in motivational interviewing, as well as a deep knowledge of the manualized treatment protocol used at the unit. In relation to adherence to treatment, the variables considered are compliance with guidelines, self-monitoring, etc. and three categories of compliance were established: good, regular and bad, depending on the level of fulfillment of the instructions provided by the therapist.
A full description of this CBT program has been previous published [Reference Jiménez-Murcia, Aymamí-Sanromà, Gómez-Peña, Álvarez-Moya and Vallejo47] and its short- and long-term effectiveness has been described elsewhere [Reference Mestre-Bach, Steward, Granero, Fernández-Aranda and Mallorquí-Bagué15, Reference Jiménez-Murcia, Álvarez-Moya, Granero, Neus Aymami, Gómez-Peña and Jaurrieta48, Reference Jiménez-Murcia, Granero, Fernández-Aranda, Arcelus, Aymamí and Gómez-Peña49].
2.4. Statistical analyses
Statistical analyses were carried out with MPlus8 for Windows. The trajectories were estimated using the SOGS-total scores obtained during the first year after completion of the CBT, which was defined as a measure of gambling problem severity. Due to the strong association between the decreases in severity and the initial (baseline) gambling severity, estimation was carried out including baseline SOGS-total scores as a covariate. Latent Class Growth Analysis (LCGA) was used, defining the robust maximum likelihood (MLR) estimator in the Analysis command (full information on this method is presented in: [Reference Enders and Bandalos50, Reference Graham51] and using Lo-Mendell-Rubin [Reference Lo, Mendell and Rubin52] as a measure to determine the number of classes. LCGA constitute a special type of Growth Mixture Modeling, with the peculiar consideration that individuals within a class are homogenous and therefore variance and covariance estimates for the growth factors within each class are set to zero [Reference Kreuter and Muthén53, Reference Jung and Wickrama54]. TYPE = MIXTURE in MPlus syntax was defined and the MODEL command set at 0, 1, 2, 3 and 4 the time scores for the slope growth factor to define a linear growth model with equidistant time points (at post-therapy and at months 3-6-9-12 of the follow-up). In the estimation procedure, solutions with quadratic and cubic components were tested, but they were rejected because these potential solutions did not provide substantively better statistical adjustment and/or models with better clinical interpretation, and therefore simpler solutions with linear components were selected for the sake of parsimony. The selection of the number of trajectories was based on [Reference Nylund, Asparouhov, Muthén and Muthén55]: a) the lowest Akaike (AIC) and Bayesian information criterion (BIC) indexes for the model (compared with other solutions); b) entropy (measure of the model’s discriminative capacity, that is, its ability to identify individuals following the different trajectories) above.80; c) high on-diagonal average values (around.80) in the matrix containing the probabilities of membership (that is, high average latent class probabilities for most likely latent class membership by latent class); d) enough sample size in a class/trajectory to allow for statistical comparisons; and e) adequate clinical interpretability.
The distribution of the characteristics of participants (sociodemographic, personality and psychopathological levels) across the identified trajectories was examined with chi-square tests for categorical variables and analysis of variance (ANOVA) for quantitative variables. The list of features examined included the sociodemographic variables measured at the beginning of the study, gambling related variables at baseline, psychopathology and personality at baseline, psychopathology at the end of the therapy program, adherence to the therapy program and the presence of relapses during the program and during the follow-up episodes (relapses were defined as the presence of gambling episodes). Cohen’s-d coefficient measured effect size for pairwise comparisons (|d|>0.20 was considered low effect size, |d|>0.50 moderate effect size and |d|>0.80 good effect size [Reference Kelley and Preacher56]. Increase in Type-I error due to multiple statistical comparisons was controlled with Simes’ correction method, a familywise error rate stepwise procedure which offers more powerful test than the classical Bonferroni correction [Reference Simes57].
Finally, a multinomial logistic regression was performed to model the predictive contribution of the measures at the beginning of the study (defined as independent variables) on membership in the 5 groups obtained in the LCGA (defined as the dependent variable). The multinomial regression is a generalization of logistic regression to multiclass problems (i.e. categorical criteria with more than two levels), and therefore it allows for the prediction of the probabilities of the different levels of a categorically distributed dependent variable considering a set of independent variables. In this study, due to the large set of independent variables, three separate models were obtained: a) for the sociodemographic variables (civil status, education level, social position index, employment status and origin of the sample); b) for gambling related variables and global psychopathological state (patients’ age, GD duration, DSM-5 total criteria for GD, debts due to gambling and SCL-90R GSI); and c) for personality traits (TCI-R scores). The final models presented in this study retained only those independent variables with a significant contribution on the criterion.
3. Results
3.1. GD course trajectories
Table 2, contains the goodness-of-fit and the mean estimates for the candidate models obtained in the LCGA, with a number of trajectories ranging from 2 to 5 groups. Solution models for more than 5 trajectories were not considered due to small group size to allow for subsequent statistical comparisons (for example, the 6-classes model included a group with only 3 participants). The final model selected was the 5-trajectory solution (Fig. 1 includes the shapes for the SOGS evolution from baseline to the year following treatment). This model yielded the lowest AIC-BIC indexes (AIC = 12633.1, BIC = 12,791.5 and adjusted sample-size BIC = 12,677.2), excellent entropy (.877), very high on-diagonal values in the matrix with the average latent class probabilities (between.868 and.917), and good clinical interpretability.
Table 2 Goodness-of-fit indexes for LCGA candidate solutions.
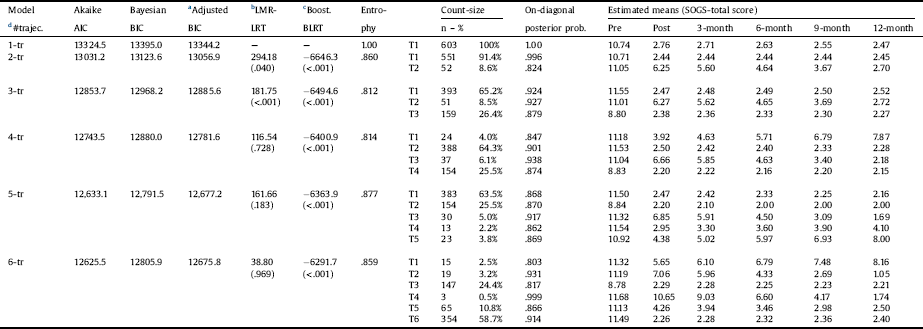
Note.
a Sample-size adjusted BIC.
b Lo-Mendell-Rubin Adjusted Likelihood Ratio Test: value (significance).
c Boostrapped Likelihood Ratio Test (BLRT): loglikelihood ivalue (significance).
d Number of trajectories.
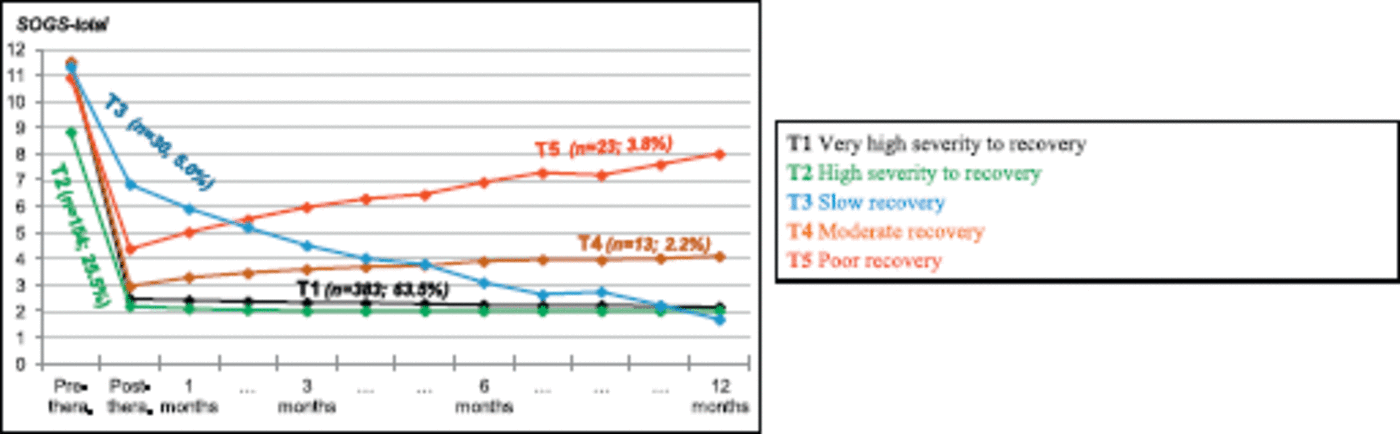
Fig 1. Course trajectories: from pre-treatment to 12-months following the CBT program (n = 603).
3.2. Comparison between trajectories at baseline
Tables 3 and 4 include the comparison between trajectories in terms of sociodemographic and clinical variables taken at the start of the CBT program (at the beginning of the study).
Trajectory T1 (n = 383, 63.5%) represented patients with very high GD severity at baseline (mean SOGS = 11.5) and good progress to recovery (mean SOGS = 2.5 at post-treatment and 2.2 at the end of the follow-up period). This group was characterized by the high scores in psychopathology (as determined by the SCL-90-R) and high scores in novelty seeking at baseline.
Trajectory T2 (n = 154, 25.5%) represented patients with high GD severity at baseline (mean SOGS = 8.8) and good progress to recovery (mean SOGS = 2.2 at the end of the treatment and 2.0 at the end of the follow-up period). This class is characterized by the lowest scores in psychopathology state at baseline, low scores in novelty seeking and harm avoidance and high scores in reward dependence, persistence, self-directedness and cooperativeness. Trajectory T2 also included the highest proportion of patients that were married or living with a stable partner, but the lowest proportion of patients with debts due to gambling behavior.
Trajectory T3 (n = 30, 5.0%) represented patients with high levels of GD severity at baseline (mean SOGS = 11.3) and slow progress to recovery (mean SOGS = 6.85 at post-therapy and 1.7 at the end of the follow-up period). This trajectory included patients with moderate levels of psychopathology and high scores in novelty seeking and reward dependence at baseline.
Trajectory T4 (n=13, 2.2%) represented patients with very high GD severity at baseline (mean SOGS = 11.5) and moderate progress in obtaining recovery (mean SOGS = 3.0 at post-CBT and 4.1 at the 12-month follow-up). This trajectory grouped patients with worse psychopathological state at baseline, high scores in harm avoidance and low scores in persistence. Trajectory T4 also included the highest proportion patients that were single, as well as the highest percentage of patients with debts due to gambling behavior.
Trajectory T5 (n=13, 2.2%) represented patients with very high GD severity at baseline (mean SOGS = 10.9) and poor progress at the end of the follow-up period (mean SOGS = 4.4 at post-treatment and 8.0 at the 12-month follow-up). This class agglomerated patients with moderate psychopathological impairment and low scores in reward dependence and persistence.
Fig. 2 contains a radar-chart to graphically illustrate the main differences between trajectories for the psychological variables registered at baseline (z-standardized means have been plotted to allow for easier interpretation due to the different scale ranges).
3.3. Comparison between trajectories considering therapy outcomes
The top of Table 5 includes comparisons between trajectories considering compliance with the therapy guidelines and the presence of gambling episodes (relapses) during CBT. Trajectories T1 and T2 did not differ in these two outcomes, and they were characterized by a high proportion of participants with good compliance and a low presence of relapses. Contrarily, trajectories T3-T4-T5 featured a high proportion of participants with moderate to bad compliance with therapy guidelines and a higher proportion of relapses.
The middle of Table 5 includes comparisons between trajectories in psychopathology at the end of the CBT program. T2 obtained the lowest means compared with all the other trajectories on many SCL-90-R scales, followed by trajectories T1 and T5. The highest levels of psychopathology were found in T3 and T4.
Finally, the bottom of Table 5 contains the presence of relapses during the 12-month follow-up period. T2 registered the lower proportion of patients who reported the presence of gambling episodes during this period (5.2%), closely followed by trajectory T1 (9.7%). The presence of relapse for trajectory T3 (20.0%) was statistically higher than the relapses registered for T1 and T2, and statistically lower than the presence of relapses obtained for T4 (46.2%) and T5 (47.8%).
3.4. Predictive model
Table 6 includes the results of the final multinomial logistic regressions. The final model for the sociodemographic variables retained only civil status as a significant predictor of the membership in the developmental trajectories classification. Results indicate that being single (versus being married or separated/divorced) increased the odds of being classified in trajectories 1, 4 or 5 versus being classified in trajectory 2. Regarding model 2 (which initially included patients’ age, gambling related variables and psychopathological state), significant predictors retained in the final model were the number of DSM-5 criteria for GD and SCL-90R GSI scores. This model indicates that higher gambling severity at baseline (higher number of DSM-5 criteria) decreases the odds of being classified in trajectory 1 or in trajectory 2 compared with being in the other trajectories, and that worse psychopathological state (higher GSI score) decreases the odds of being classified in trajectory 2 compared with being in any other trajectory. Finally, model 3 (which initially included all the TCI-R scores), retained novelty seeking (higher levels predict lower odds of being in trajectory 2 compared to trajectories 1 and 3), harm avoidance (higher levels predict lower odds of being in trajectory 2 compared to being in trajectories 1, 3 and 4) and self-directedness (higher levels predict higher odds of being in trajectory 2 compared to being in trajectories 1 and 5) as significant predictors.
Table 3 Comparison between trajectories in sociodemographic variables measured at the beginning of the study.
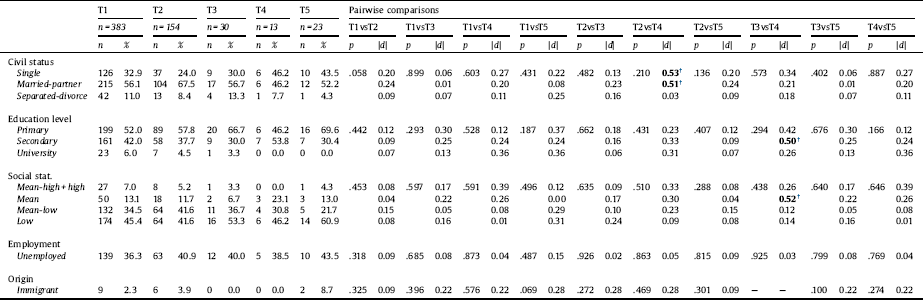
* Bold: significant comparison (.05 level).
† Bold: effect size in the moderate (|d|>0.50) to good range (|d|>0.80).
Table 4 Comparison between trajectories in clinical state (gambling variables, psychopathology and personality) at baseline.
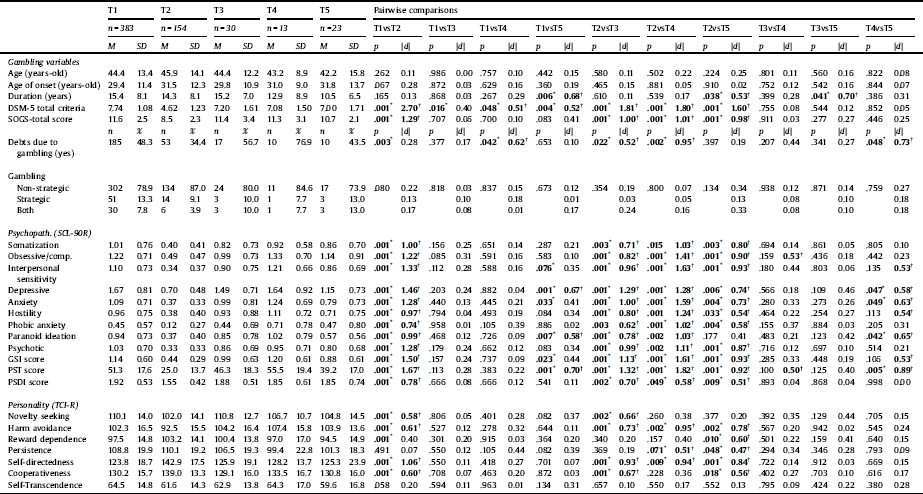
Note. M: mean. SD: standard deviation.
* Bold: significant comparison (.05 level).
† Bold: effect size in the moderate (|d|>0.50) to good range (|d|>0.80).

Fig 2. Radar chart with the main psychological variables differing between the trajectories (at baseline) (n = 603).
4. Discussion
This study used LCGA to obtain an empirical classification for a sample of patients who met clinical criteria for GD, based on gambling severity during the 12 months following a CBT program. SOGS total score was selected as a measure of change in the GD severity because it provides a wider range of scores based on scalar measures and this attribute statistically facilitated the identification of developmental trajectories with better fitting. T1 and T2 included the largest number of participants (in total n = 537, 89% of the sample), and were defined by high to severe gambling severity at baseline and good progress to recovery during the follow-up. Trajectory T3 (n = 30, 5.0%) included also participants with initial severe affectation and slow evolution to recovery. T4 and T5 included the least number of participants (in total n = 36, 6%), characterized by severe baseline gambling severity and poor progress during the follow-up period.
The trajectories obtained discriminative capacity in terms of psychopathology levels, personality traits at baseline, the degree of compliance with the therapy guidelines during the CBT program, and the presence of relapses during CBT and during the 12-month follow-up. T3 included patients with a severe baseline psychopathology, but with good progress during recovery (although these clinical improvements were slowly obtained). These patients may have benefited from a more intense treatment plan in order to attain complete gambling abstinence more quickly (for example, treatment plans with a greater number of sessions). Trajectories T4 and T5 had the lowest duration of the gambling problem, high psychopathology at baseline and low scores in reward dependence and persistence. They also obtained the highest proportion of participants with poor compliance during treatment and relapses were the highest for these groups. As a whole, these results seem consistent with a recent systematic review highlighting the pre-treatment predictors of short- and long-term GD treatment outcomes. This review found shows that less psychopathology at intake (mainly depression and anxiety levels) were the most consistent predictors of success after treatment across multiple time points, followed by older age, lower gambling severity at intake, education levels, and personality traits [Reference Merkouris, Thomas, Browning and Dowling11].
Another important aspect to consider is the course of the disorder. The results of the present study suggest that shorter GD duration is associated with poorer treatment outcomes, as described in previous studies [Reference Cowlishaw, Merkouris, Dowling, Anderson, Jackson and Thomas16, Reference Jimenez-Murcia, Aymamí, Gómez-Peña, Santamaría, Álvarez-Moya and Fernández-Aranda58]. A possible explanatory hypothesis to these findings would be related to the awareness of disorder and motivation to deal with the gambling problem [Reference Gómez-Peña, Penelo, Granero, Fernández-Aranda, Alvarez-Moya and Santamaría59]. It could be that the patients with the worse therapeutic evolution had undergone less negative consequences for their gambling behavior and, therefore, had less intrinsic motivation to change. It is possible that the goal of our program to obtain complete abstinence from all types of gambling may be too ambitious for patients with shorter GD duration [Reference Ladouceur, Lachance and Fournier60, Reference Stea, Hodgins and Fung61]. In addition, taking into account that therapeutic goals may change throughout treatment. In this vein, Stea, Hodgins & Fung [Reference Stea, Hodgins and Fung61] showed that half of subjects following a treatment program based on a brief motivational intervention modified their therapeutic goals as therapy progressed. The majority began the recovery process by assuming definitive abstinence from all types of gambling, however later on, more than 25% expressed their willingness to give up their problematic type of gambling, 10% bet in a controlled manner and only 20% continued with the decision to abandon all types of gambling. In fact, patients often return to gambling, to a greater or lesser extent, after having undergone treatment for their disorder and, more specifically, at 12 months of follow-up [Reference Hodgins and El-Guebaly62]. Although this does not always means therapy was a failure or a worsening of their gambling problem [Reference Müller, Wölfling, Dickenhorst, Beutel, Medenwaldt and Koch14]. Also at a 12-month follow-up, another study identified that 41.6% of subjects treated with an inpatient treatment program maintained complete abstinence from all types of gambling, while 29.2% of patients still met diagnostic criteria for GD, although another 29.2% still had some form of gambling, but did not meet diagnostic criteria [Reference Müller, Wölfling, Dickenhorst, Beutel, Medenwaldt and Koch14]. Considering this issue, some studies have explored the effectiveness of programs oriented to controlled gambling [Reference Ladouceur, Lachance and Fournier60, Reference Stea, Hodgins and Fung61, Reference Blaszczynski, McConaghy and Frankova63–Reference Ladouceur66]. Actually, it seems that in the community, most individuals who have had gambling problems end up recovering without having totally abstained from gambling behavior, during the process [Reference Slutske, Jackson and Sher25]. Therefore, although abstinence is the most common therapeutic goal in treatment programs [Reference Slutske, Piasecki, Blaszczynski and Martin67], it could be timely to explore other alternatives such as controlled gambling, in the context of personalized therapeutic approaches, discussing with the patient their own goals and objectives [Reference Müller, Wölfling, Dickenhorst, Beutel, Medenwaldt and Koch14, Reference Menchon, Mestre-Bach, Steward, Fernandez-Aranda and Jimenez-Murcia68]. However, focusing on T4 and T5, it is necessary to bear in mind that other associated factors may be personality traits such as lower reward dependence and low persistence. These traits could be defined as the presence of less interest in pleasing others, social withdrawal, detachment and distance in interpersonal interactions [Reference Merkouris, Thomas, Browning and Dowling11–Reference Jiménez-Murcia, Granero, Fernández-Aranda, Arcelus, Aymamí and Gómez-Peña13]. Likewise, they may show a tendency to easily abandon their goals at the slightest setback and or sign of frustration. Taking all these results together, we could consider that, perhaps, these patients could benefit from motivational interventions, as the systematic review and meta-analysis by Yakovenko et al [Reference Yakovenko, Quigley, Hemmelgarn, Hodgins and Ronksley69] demonstrated in terms of improvement of gambling problems at 1, 3 and 12 months of follow-up. Therefore, motivational interviews could help to improve their awareness of their condition, to make their therapeutic guidelines more flexible, and to set aims other than definitive abstinence. In addition, these patients could also be treated adding complementary interventions aimed at increasing the capacity for emotion regulation in order to better manage feelings of frustration, anger, anger, anxiety or sadness. Previous studies have shown the association between emotion regulation deficits and lack of persistence in treatment in subjects with substance use [Reference Hopwood, Schade, Matusiewicz, Daughters and Lejuez70]. Furthermore, emotion regulation is closely related to decision making [Reference Heilman, Crişan, Houser, Miclea and Miu71] and gambling disorder patients present marked deficits in decision making, as in the case of alcohol and substance use disorders [Reference Goudriaan, Oosterlaan, De Beurs and Van Den Brink72]. Finally, previous research has demonstrated the usefulness of combining standard CBT programs with treatments based on new technologies, such as serious games designed to improve emotion regulation strategies and self-control capacity [Reference Claes, Jiménez-Murcia, Santamaría, Moussa, Sánchez and Forcano73–Reference Fernández-Aranda, Jiménez-Murcia, Santamaría, Gunnard, Soto and Kalapanidas75], as well as in gambling disorder [Reference Tárrega, Castro-Carreras, Fernández-Aranda, Granero, Giner-Bartolomé and Aymamí76, Reference Jiménez-Murcia, Fernández-Aranda, Kalapanidas, Konstantas, Ganchev and Kocsis77]. Another alternative for these type of patients with poor response to treatment, as in the case of the patients grouped in T4 and T5, could be to include neurocognitive stimulation protocols aimed at training executive functions [Reference Gay, Boutet, Sigaud, Kamgoue, Sevos and Brunelin78, Reference Makani, Pradhan, Shah and Parikh79]. It should be borne in mind that perhaps they may even benefit from carrying out all these therapeutic strategies in individual treatment programs instead of in a group format. In sum, they may feel more comfortable in a treatment more tailored to their needs and without having to establish social relationships with the rest of the patients participating in the same group treatment program.
Table 5 Comparison between trajectories for therapy outcomes.
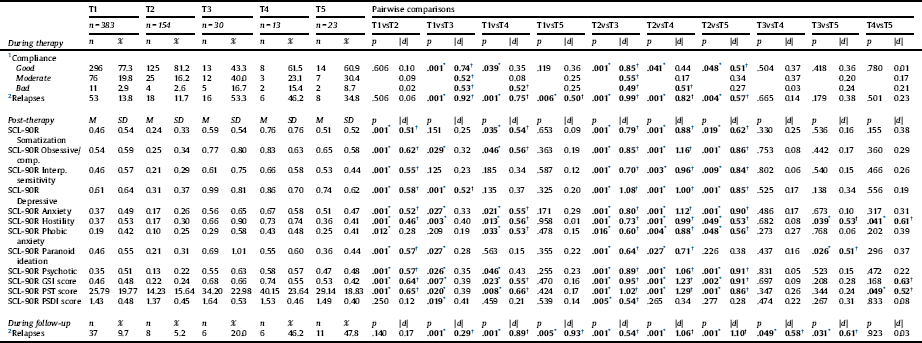
Note.
1. Compliance with therapy guideliness.
2. Presence of gambling episodes. M: mean. SD: standard deviation.
* Bold: significant comparison (.05 level).
† Bold: effect size in the moderate (|d|>0.50) to good range (|d|>0.80).
Table 6 Predictive models of the trajectory based on the measures at the beginning of the study: final multinomial regressions.
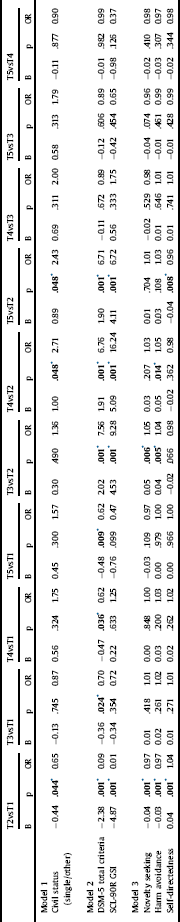
Note.
* Bold: significant parameter (.05 level).
This work should be evaluated within the context of several limitations. First, only the 12 months of follow-up after CBT treatment was covered, and therefore there is no way of knowing the extent to which the developmental trajectories may persist over time. Second, the presence of dropout during the study was 34.2%. It must be highlighted, however, that the developmental trajectories have been estimated with a full information method, which does not replace or impute missing data, but which handles incomplete information within the analysis using all the available information in the data set. This procedure has demonstrated good reliability/validity to produce unbiased parameter estimates for missing data in models from LCGA to structural equations procedures. This study has obtained empirical latent classes based on GD severity (like many longitudinal studies, which generate the developmental trajectories based on the evolution of a concrete measure) (232,426). Still, it would be very appropriate for future research to extend the generation of the groups by incorporating time-invariant and time-variant features.
Funding sources
We thank CERCA Programme/Generalitat de Catalunya for institutional support. This manuscript and research was supported by grants from the Ministerio de Economía y Competitividad (PSI2015-68701-R), Instituto de Salud Carlos III (ISCIII) (FIS PI14/00290 and Funded by Delegación del Gobierno para el Plan Nacional sobre Drogas (2017/I067) and co-funded by FEDER funds /European Regional Development Fund (ERDF), a way to build Europe. CIBERObn and CIBERSAM are both initiatives of ISCIII. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. GMB was supported by a predoctoral AGAUR grant (2018 FI_B2 00,174), grant co-funded by the European Social Fund (ESF) “ESF”, investing in your future. With the support of the Secretariat for Universities and Research of the Ministry of Business and Knowledge of the Government of Catalonia. TMM and CVA are supported by a predoctoral Grant of the Ministerio de Educación, Cultura y Deporte (FPU16/02087; FPU16/01453).
Declarations of interest
None.











Comments
No Comments have been published for this article.