Non-adherence to medication regimens is believed to increase the probability of relapse in patients with schizophrenia and to contribute significantly to costs. Weiden & Olfson (Reference Weiden and Olfson1995) estimated that non-adherence accounts for approximately 40% of rehospitalisation costs for patients with schizophrenia in the 2 years after their discharge from in-patient treatment. Also, given that 25% to 80% of patients at some point in their treatment fail to take their medication correctly (Reference BattagliaBattaglia, 2001; Reference Conley and KellyConley & Kelly, 2001), the system-wide costs of non-adherence could be substantial. Hughes et al (Reference Hughes, Bagust and Haycox2001) highlighted the need for more information on the consequences of non-adherence, to allow economic evaluations to reflect its potential impact.
Patients who do not take their medication are likely to require more treatment and support from a range of services. Several other factors are thought to be associated with resource use and costs, but little is known about their relative impacts. The objectives of this study are to identify patient, medication and environmental factors associated with the costs of supporting people with schizophrenia. In particular, we seek to gain information on the nature of the relationship between non-adherence and resource use.
METHOD
Study sample
In 1993 and 1994 the Office of Population Censuses and Surveys (OPCS; now the Office for National Statistics) conducted a number of cross-sectional epidemiological surveys of psychiatric morbidity among adults living in Great Britain. For the present analysis we used data from the survey report on adults living in institutions between April and July 1994 (Reference Meltzer, Gill and PetticrewMeltzer et al, 1996). A sampling fraction was applied to each of the following categories for institutions that accommodate people with mental illness: residential accommodation; National Health Service accommodation; private hospitals, homes and clinics; and unregistered accommodation. The survey data for these analyses were provided by the UK Data Archive (http://www.data-archive.ac.uk). We included in the analyses all patients who, at the time of the survey, reported that they had been prescribed antipsychotic medication. No other inclusion or exclusion criterion was applied in selecting sample members. This gave a study sample of 658 people.
Non-adherence measurement
Adherence has been defined as ‘the extent to which a person's behaviour coincides with medical or health advice’ (Reference Haynes, Haynes, Sackett and TaylorHaynes, 1979) or ‘the degree of conformity between treatment behaviour and treatment standards’ (Reference GaebelGaebel, 1997). The assessment of non-adherence in our study was based on self-report by survey respondents. The assessment related to current medications only and was based on survey responses to two questions: ‘Do you sometimes not take your medications even though you should?’ ‘Do you sometimes take more medication/pills than the stated dose?’ In the analyses that follow, we do not make a distinction between those who deliberately did not take their medication and those who forgot to take it. Because we relied on self-reported information, it is likely that patients who were unaware of mistakes they were making in their medication regimen have been incorrectly classified as being adherent; our analyses may thus underestimate the prevalence of non-adherence ‘for any reason’.
Cost measurement
Data on the frequency of use of in-patient care, out-patient care, external services (including services provided by community psychiatric nurses, occupational therapists, social workers, community psychiatrists, home helps and volunteer workers), day care and sheltered employment for the period of 1 year were available from the survey. Data for general practitioner services related to a 2-week period.
Potentially associated variables
Data from the survey were extracted on age, gender, education, general level of health, illness severity, in-patient contact for mental health reasons in the past year, self-reported use of illegal drugs (drug misuse), self-reported misuse of alcohol, level of support from family or friends, and familiarity with medication. The data allowed us to identify patients from ethnic minorities but did not allow differentiation between White ethnic groups.
Levels of general health were reported by patients on a five-point scale which we collapsed to three levels: very good/good, average and poor/very poor. Identifying those who had psychotic disorders involved asking patients what was the matter with them, asking staff what was the matter with the patient, asking residents and carers whether the patient was taking antipsychotics or receiving antipsychotic injections, and establishing whether patients had had contact with any health care professional for treatment of a psychotic illness. Severity of neurosis was based on the Revised Clinical Interview Schedule (CIS–R, Reference Lewis, Pelosi and ArayaLewis et al, 1992), a standardised instrument for assessing symptom prevalence and severity in minor psychiatric disorders. Although administered by non-clinicians, the CIS–R has been shown to correlate closely with standard clinical assessments (Reference Lewis, Pelosi and ArayaLewis et al, 1992). Support from an adult to whom the patient feels close was gauged from the question: ‘How many adults who live/are staying here with you do you feel close to?’ Medication familiarity was represented by a duration of medication greater than 2 years.
A variable was created to identify the sample from which each patient was drawn, differentiating people living in hospitals from those in ‘other’ settings (residential care homes, group homes or hostels). With regard to in-patient service use, patients resident in hospital were asked about visits to hospitals other than the one in which they lived.
Statistical analyses
More than a quarter of the sample (172 patients, 26.1%) had missing data for one or more of the variables potentially associated with in-patient service use and costs: 118 (17.9%) patients were missing one variable only, 35 (5.3%) had two missing values, 16 (2.4%) had three missing values and 3 (0.5%) had four missing values. The variables with the greatest rate of missing values were length of time on medication (12.8% missing) and social support (12.6% missing).
In order to prevent biases in the sample and to minimise the loss of degrees of freedom, missing values for the variables potentially associated with costs were replaced using multiple imputation as described by Schafer (Reference Schafer1997) and Little & Rubin (Reference Little and Rubin1987). The procedure uses observed data multiple times to estimate missing data, creating equally plausible versions of the complete data. Each of the data-sets is then analysed, and the results combined using Rubin's rules for scalar estimands (Reference RubinRubin, 1987) to produce one set of estimates and standard errors that incorporate missing-data uncertainty. We carried out this procedure using the NORM software (Version 2 for Windows; Reference SchaferSchafer, 1999), which creates multiple imputations by a data augmentation algorithm, a special kind of Markov chain Monte Carlo technique. Schafer (Reference Schafer1997) noted that if the proportion of data missing is relatively low, five imputations suffice to achieve efficient estimations of changes in the standard errors of parameters. This is the number of imputations we have used. Imputed values were restricted to the observed range of values in the data.
Each of the five data-sets was analysed as follows. A generalised linear model (GLM) was used to test patient, medication and environmental factors for their association with total costs. With respect to in-patient and external service use costs, a significant proportion of the study population did not use these services and so a two-part model was used: the first part modelled the probability that costs were incurred, and the second part modelled the intensity of costs among those who did use the services (Reference MullahyMullahy, 1998). The probability that costs were incurred was estimated with a logit model, whereas the estimation of the intensity of costs was based on a GLM. Within the GLM a link function can be specified to allow the estimates of the parameters to be directly derived in the linear scale, and the algorithm outlined by Manning & Mullahy (Reference Manning and Mullahy2001) was used to select the distributional form of the GLM based on an extension of the Park test. In all models, factors achieving significance at the 0.05 level were deemed statistically significant. These analyses were performed using STATA version 7 data analysis software (STATA, 2001).
Predicted costs were derived for each of the three cost outcomes: in-patient service costs, external service costs and total costs. For in-patient and external services costs, the predictions were estimated as the product of the estimated probability of use and the expected intensity of costs. We calculated the predicted costs for a hypothetical case and then repeated the estimation for the same case with each of a number of single changes in other factors. In order to estimate the confidence intervals around these predictions, a bootstrapping algorithm, incorporating 1000 repetitions, was used. This allowed us to obtain estimates of the standard error around each of the predictions.
Each of the parameters estimated from the five data-sets – odds ratios and coefficients from the logit and generalised linear models, and estimates of the predicted costs – were then combined in NORM, as described above, to arrive at one set of estimates.
RESULTS
At the time of the survey from which we obtained our data, 658 patients were taking antipsychotic medication. Table 1 provides demographic statistics comparing patients resident in hospital with those in other types of institutions. The rate of reported non-adherence was lower in the subsample of patients resident in hospital (11.2%) compared with patients in other types of institutions (21.2%). As noted above, these percentages are likely to be underestimates, because they do not measure non-adherence of which the patient is unaware, and do not address the problem of deliberate misreporting.
Table 1 Demographic characteristics of the patients surveyed
| Resident in hospital (n=304) | Resident in other institutions (n=354) | |
|---|---|---|
| Age, years (mean (s.d.)) | 43.0 (12.6) | 44.8 (10.6) |
| Male gender (%) | 71.1 | 68.4 |
| Ethnicity: White (%) | 89.5 | 95.5 |
| Education (%) | ||
| A-levels or higher | 11.2 | 12.4 |
| O-levels | 12.5 | 16.2 |
| No O-levels | 76.3 | 71.4 |
| General health (%) | ||
| Good | 50.3 | 47.7 |
| Fair | 33.6 | 41.2 |
| Poor | 16.1 | 11.1 |
| Diagnosis of schizophrenia (%) | 72.0 | 63.3 |
| Severity of neurosis: CIS-R score (mean (s.d.)) | 12.9 (10.9) | 10.5 (9.7) |
| ‘Yes’ response to survey question (%) | ||
| Mental health hospital stay | 12.8 | 17.8 |
| Drug misuse | 7.2 | 9.3 |
| Alcohol misuse | 6.1 | 6.7 |
| Lives with adult to whom patient feels close | 55.7 | 66.2 |
| More than 2 years on medication | 52.8 | 78.6 |
| Self-reported non-adherence (n (%)) | 34 (11.2) | 75 (21.2) |
In-patient services
The mean observed in-patient cost was £7487 per annum. The results of the two-part model looking at factors associated with in-patient service use and costs are presented in Tables 2 and 3. A total of 151 patients reported an in-patient stay in the past year. The use of in-patient services was significantly associated with living in a residential care home, group home or hostel; membership of an ethnic minority group; non-adherence to medication regimen; and having been prescribed an antipsychotic medication for less than 2 years. Patients identified as belonging to an ethnic minority were two-and-a-half times as likely to have used in-patient services. Those living in a residential care home, group home or hostel were over one-and-a-half times as likely to report use of in-patient services compared with hospital residents, as were patients reporting non-adherence as compared with those reporting adherence, and those who had been taking medication for less than 2 years compared with those taking medication for 2 or more years.
Table 2 Factors associated with the use of in-patient services (658 observations; P=0.0001, pseudo R 2=0.0665)
| Independent variables | Odds ratio (of using services) | P |
|---|---|---|
| Resident in ‘other’ institution (n=354)1 (relative to resident in hospital: n=304) | 1.65 | 0.019 |
| Screened positive for schizophrenia: n=443 (relative to not screened positive for schizophrenia: n=215) | 1.02 | 0.907 |
| Age | 0.98 | 0.107 |
| Male: n=458 (relative to female: n=200) | 0.70 | 0.106 |
| Higher qualifications or A-levels: n=76 | 1.39 | 0.253 |
| O-levels: n=102 (relative to no O-level qualification: n=480) | 0.98 | 0.926 |
| Non-White: n=48 (relative to White: n=610) | 2.43 | 0.012 |
| Average general health: n=250 | 0.90 | 0.637 |
| Poor general health: n=87 (relative to good general health: n=321) | 0.69 | 0.278 |
| CIS-R score2 | 1.01 | 0.526 |
| Non-adherent to medication regimen: n=109 (relative to adherent: n=549) | 1.62 | 0.054 |
| Lives with adult to whom patient feels close: n=403 (relative to not living with adult to whom patient feels close: n=255) | 1.50 | 0.180 |
| Reports illegal drug use: n=55 (relative to non-use: n=603) | 1.36 | 0.351 |
| Reports moderate or high alcohol dependence: n=42 (relative to no alcohol dependence: n=616) | 1.89 | 0.098 |
| Two or more years on medication: n=439 (relative to <2 years on medication: n=219) | 0.58 | 0.033 |
Table 3 Factors associated with the costs of in-patient services (151 observations)

| Independent variables | Coefficient | P |
|---|---|---|
| Resident in ‘other’ institution: n=911 (relative to resident in hospital: n=60) | -0.085 | 0.240 |
| Screened positive for schizophrenia: n=97 (relative to not screened positive for schizophrenia: n=54) | 0.062 | 0.377 |
| Age | 0.0025 | 0.443 |
| Male: n=99 (relative to female: n=52) | 0.0030 | 0.967 |
| Higher qualifications or A-levels: n=24 | 0.029 | 0.803 |
| O-levels: n=28 (relative to no O-level qualification: n=99) | 0.14 | 0.245 |
| Non-White: n=18 (relative to White: n=133) | 0.27 | 0.072 |
| Average general health: n=58 | 0.067 | 0.382 |
| Poor general health: n=17 (relative to good general health: n=76) | 0.068 | 0.632 |
| CIS-R score | -0.0034 | 0.282 |
| Non-adherent to medication regimen: n=39 (relative to adherent: n=112) | 0.059 | 0.521 |
| Lives with adult to whom patient feels close: n=101 (relative to not living with adult to whom patient feels close: n=50) | 0.100 | 0.204 |
| Reports illegal drug use: n=20 (relative to non-use: n=131) | -0.047 | 0.638 |
| Reports moderate or high alcohol dependence: n=15 (relative to no alcohol dependence: n=136) | 0.056 | 0.659 |
| Two or more years on medication: n=87 (relative to <2 years on medication: n=64) | -0.051 | 0.502 |
Among those using in-patient services, the only factor found to approach a statistically significant association with in-patient costs was ethnicity. Non-White patients reported greater costs than White patients. This observed association, however, was based on a small sample of non-White patients (n=18). Figure 1 illustrates overall in-patient costs for different case types derived by multiplying the expected probability and intensity of use of the service. Ethnicity clearly has a major effect on in-patient costs: non-White patients are predicted to incur costs of approximately £7000 more per annum. Patients reporting non-adherence are predicted to have excess in-patient costs of approximately £2500 per year.
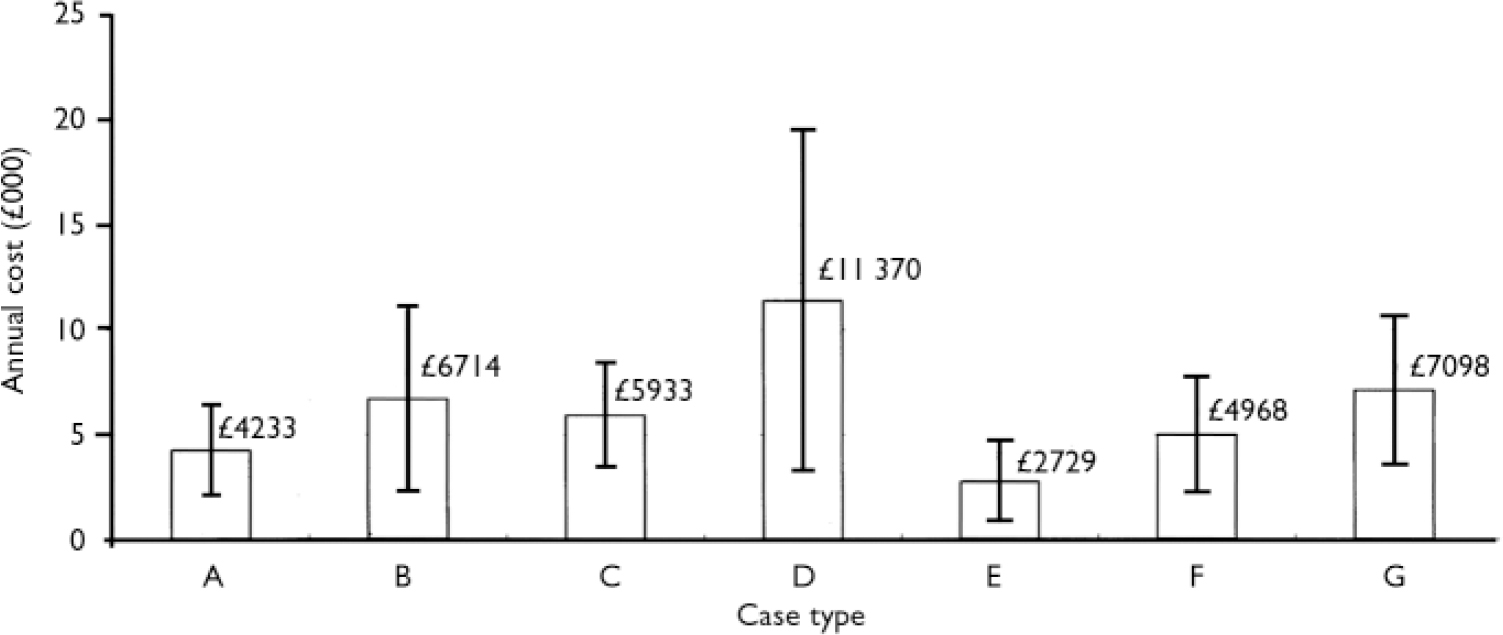
Fig. 1 Predicted in-patient costs: mean £7419, s.d.=£4256; minimum £ 1575, maximum £27452 (at 2001 unit costs) (Reference Netten, Rees and HarrisonNetten et al, 2001). A, male, age 45 years, White, no O-levels, screened positive for schizophrenia, good general health, resident in hospital, adheres to medication, no drug or alcohol misuse, lives with adult to whom he feels close, and on medication for >2 years; B, medication non-adherence; C, resident in hostel or group home; D, non-White; E, does not live with adult to whom he/she feels close; F, age 30 years; G, medication for <2 years. Vertical bars show 95% CIs.
External services
The mean observed annual cost of external services was £904. There was no reported use of external services by hospital residents. Use of external services was significantly associated with screening positive for schizophrenia or related disorders, ethnicity, the CIS–R score, non-adherence to medication regimen and length of time on medication (Table 4). Patients who screened positive for schizophrenia or related disorders were less likely to use external services compared with those who did not screen positive. Similarly, non-White patients were significantly less likely to use external services as compared with White patients. Increases in the severity of neurosis were associated with a lower likelihood of external service use. Patients who were non-adherent or who had been taking medication for 2 or more years were in each case over two-and-a-half times more likely to use external services compared with patients who were adherent and those who had been taking medication for less than 2 years, respectively.
Table 4 Factors associated with the use of external services (658 observations; P<0.0001, pseudo R 2=0.0910)
| Independent variables | Odds ratio (of using services)1 | P |
|---|---|---|
| Screened positive for schizophrenia: n=443 (relative to not screened positive for schizophrenia: n=215) | 0.66 | 0.025 |
| Age | 0.99 | 0.114 |
| Male: n=458 (relative to female: n=200) | 1.01 | 0.963 |
| Higher qualifications or A-levels: n=76 | 1.29 | 0.361 |
| O-levels: n=102 (relative to no O-level qualification: n=480) | 1.31 | 0.284 |
| Non-White: n=48 (relative to White: n=610) | 0.46 | 0.042 |
| Average general health: n=250 | 1.41 | 0.075 |
| Poor general health: n=87 (relative to good general health: n=321) | 1.36 | 0.300 |
| CIS–R score | 0.98 | 0.012 |
| Non-adherent: n=109 (relative to adherent: n=549) | 2.65 | <0.001 |
| Lives with adult to whom patient feels close: n=403 (relative to not living with adult to whom patient feels close: n=255) | 1.22 | 0.283 |
| Reports illegal drug use: n=55 (relative to non-use: n=603) | 1.40 | 0.304 |
| Reports moderate or high alcohol dependence: n=42 (relative to no alcohol dependence: n=616) | 1.40 | 0.374 |
| Two or more years on medication: n=439 (relative to <2 years on medication: n=219) | 3.03 | <0.001 |
Analysis of the factors associated with the cost of external services was based on a sample of 251 patients who had used these services in the past 12 months (Table 5). Patients who reported illegal drug use incurred significantly lower costs if they had accessed external services. Taking medication for 2 or more years was also statistically significant in its association with increased external service use costs. Even though non-adherence increases the likelihood of use of external services, the volume of use is lower, other things being equal. Indeed, the product of probability and intensity of use suggests that non-adherence is the most significant factor in increasing external service use costs, whereas costs are substantially lower for patients taking medication for less than 2 years (Fig. 2).
Table 5 Factors associated with the costs of external services (251 observations)

| Independent variables | Coefficient | P |
|---|---|---|
| Screened positive for schizophrenia: n=157 (relative to not screened positive for schizophrenia: n=94) | 0.21 | 0.153 |
| Age | 0.0010 | 0.892 |
| Male: n=176 (relative to female: n=75) | 0.12 | 0.454 |
| Higher qualifications or A-levels: n=35 | – 0.31 | 0.121 |
| O-levels: n=42 (relative to no O-level qualification: n=174) | 0.14 | 0.485 |
| Non-White: n=12 (relative to White: n=239) | 0.21 | 0.438 |
| Average general health: n=107 | 0.035 | 0.827 |
| Poor general health: n=30 (relative to good general health: n=114) | – 0.20 | 0.352 |
| CIS–R score | 0.0035 | 0.674 |
| Non-adherent: n=64 (relative to adherent: 187) | – 0.11 | 0.503 |
| Lives with adult to whom patient feels close: n=164 (relative to not living with adult to whom patient feels close: n=87) | – 0.019 | 0.910 |
| Reports illegal drug use: n=28 (relative to non-use: n=223) | – 0.47 | 0.035 |
| Reports moderate or high alcohol dependence: n=23 (relative to no alcohol dependence: n=228) | – 0.12 | 0.626 |
| Two or more years on medication: n=199 (relative to <2 years on medication: n=52) | 0.40 | 0.047 |
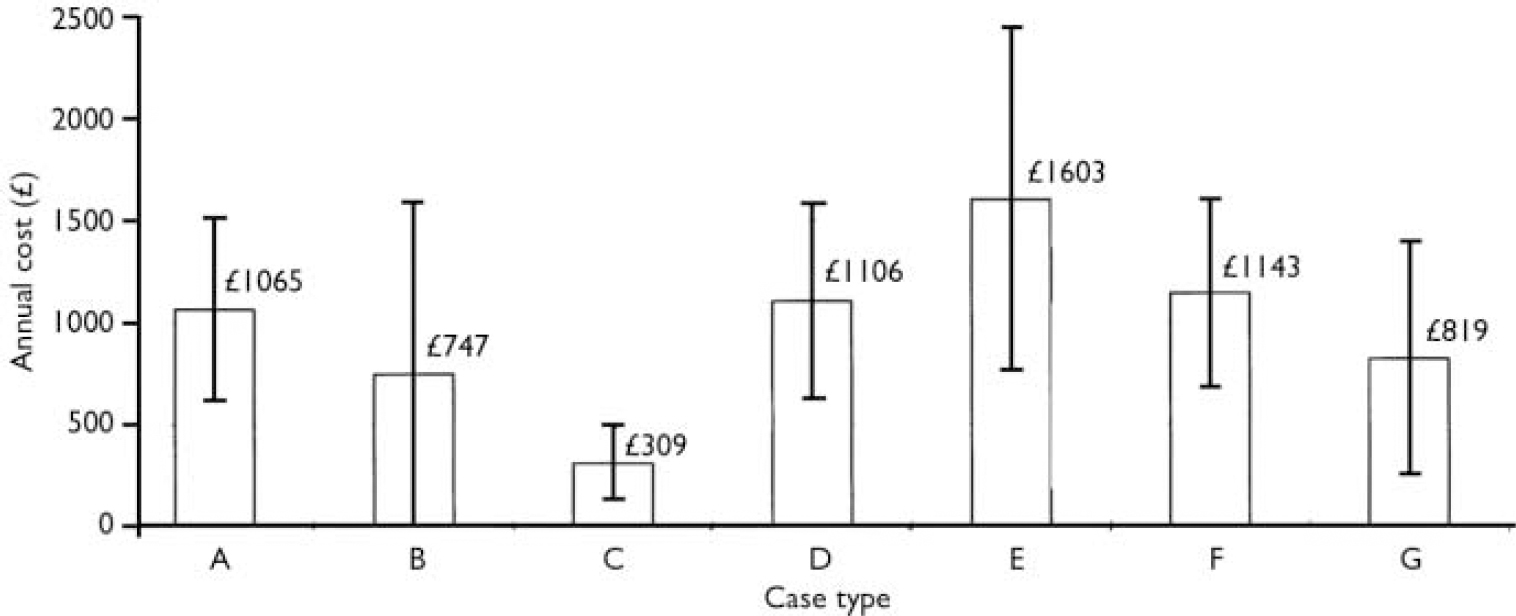
Fig. 2 Predicted costs of external services: mean £906, s.d.=£442; minimum £139, maximum £2722 (at 2001 unit costs) (Reference Netten, Rees and HarrisonNetten et al, 2001). A, male, age 45 years, White, no O-levels, screened positive for schizophrenia, good general health, resident in hospital, adheres to medication, no drug or alcohol misuse, lives with adult to whom he feels close, and on medication for >2 years; B, non-White; C, medication for <2 years; D, not screened positive for schizophrenia; E, non-adherence to medication; F, CIS–R score of 5; G, drug misuse. Vertical bars show 95% CIs.
Total costs
The final model, a single GLM, examined factors associated with the total costs of all services (Table 6, Fig. 3). The mean observed total cost was £33 795 per annum. Type of residence was found to be statistically significant: people living in residential care homes, group homes or hostels incurred significantly lower total costs than hospital residents. Borderline statistical significance was observed for the effect of non-adherence to medication regimen (P=0.059) and length of time on medication (P=0.06). Patients who did not adhere to their medication regimen incurred higher total costs than those who did, and those taking medication for 2 or more years incurred higher total costs than those taking medication for less than 2 years. Predicted total costs for residents of care homes, group homes and hostels are less than half of the amount for hospital residents. Predicted excess total service use costs for patients reporting non-adherence is over £5000 per year.
Table 6 Factors associated with total cost of services (658 observations)

| Independent variables | Coefficient | P |
|---|---|---|
| Resident in ‘other’ institution: n=2691 (relative to resident in hospital: n=217) | -0.93 | <0.001 |
| Screened positive for schizophrenia: n=315 (relative to not screened positive for schizophrenia: n=171) | 0.052 | 0.161 |
| Age | -0.0013 | 0.386 |
| Male: n=335 (relative to female: n=151) | 0.0061 | 0.874 |
| Higher qualifications or A-levels: n=55 | 0.071 | 0.153 |
| O-levels: n=76 (relative to no O-level qualification: n=355) | 0.022 | 0.676 |
| Non-White: n=38 (relative to White: n=448) | 0.0066 | 0.933 |
| Average general health: n=186 | -0.0076 | 0.820 |
| Poor general health: n=66 (relative to good general health: n=234) | 0.027 | 0.634 |
| CIS-R score | 0.00083 | 0.615 |
| Non-adherent: n=91 (relative to adherent: n=395) | 0.095 | 0.059 |
| Lives with adult to whom patient feels close: n=298 (relative to not living with adult to whom patient feels close: n=188) | 0.062 | 0.110 |
| Reports illegal drug use: n=46 (relative to non-use: n=440) | -0.056 | 0.451 |
| Reports moderate or high alcohol dependence: n=31 (relative to no alcohol dependence: n=455) | -0.022 | 0.801 |
| Two or more years on medication: n=328 (relative to <2 years on medication: n=158) | 0.073 | 0.060 |
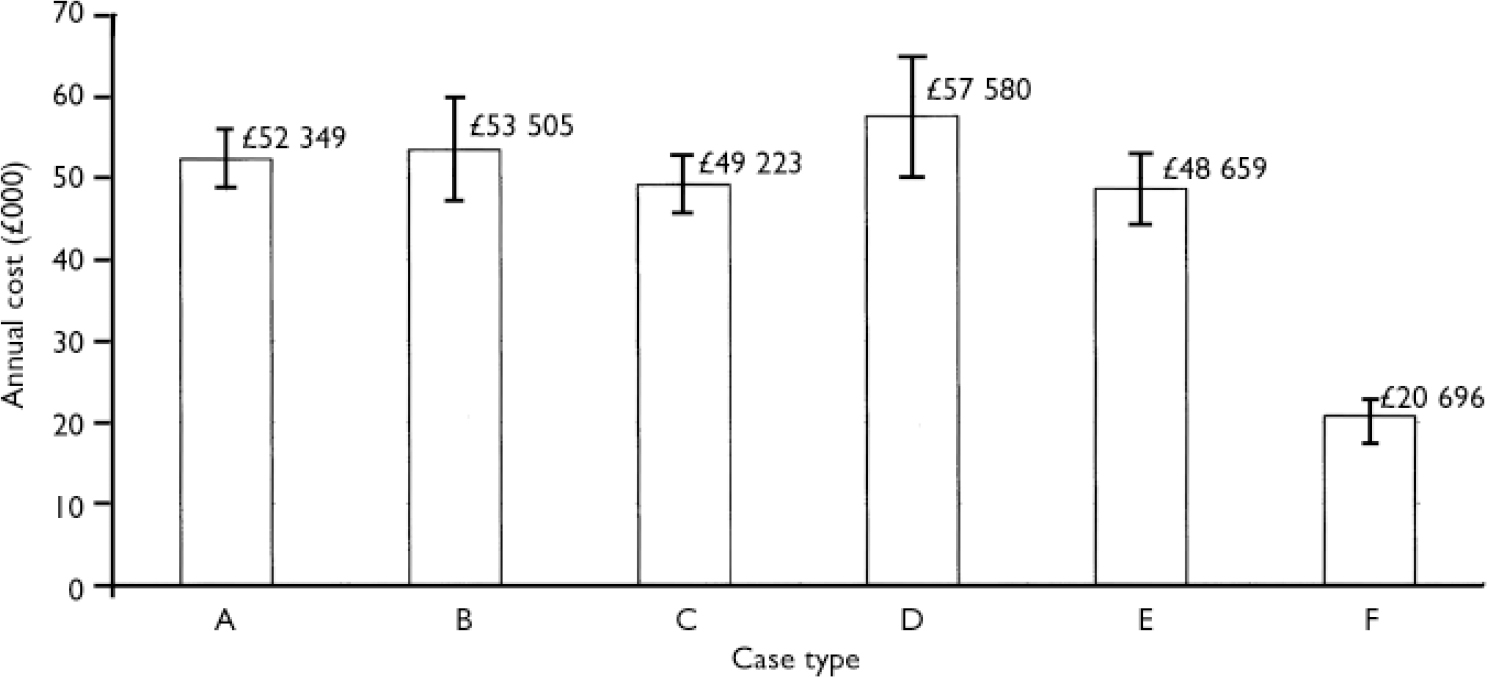
Fig. 3 Predicted total service use costs: mean £33 773, s.d.=£15 029; minimum £16 033, maximum £62 785 (at 2001 unit costs) (Reference Netten, Rees and HarrisonNetten et al, 2001). A, male, age 45 years, White, no O-levels, screened positive for schizophrenia, good general health, resident in hospital, adheres to medication, no drug or alcohol misuse, lives with adult to whom he feels close, and on medication for >2 years, no side-effects; B, higher qualifications or A-levels; C, does not live with an adult to whom he or she feels close; D, non-adherence to medication; E, less than 2 years on medication; F, resident in hostel or group home. Vertical bars show 95% CIs.
DISCUSSION
Patterns of resource use and costs are associated with a range of patient characteristics, but differ by service type. Only medication non-adherence appears to exhibit a consistent association with greater resource use, and is a key factor in the use of in-patient and external services.
Important factors appear to relate to the degree of needs of the patient and the ability of the system to address them. For example, after standardising for severity of neurosis, illegal drug use and other factors, the use of in-patient services and the costs incurred as a result of use were associated with being from an ethnic minority. Also, patients taking medication for a significant length of time tended to make greater use of external services but were less likely to require in-patient services. The total cost of all services used was strongly associated with residence in hospital.
Limitations
The cross-sectional nature of the Psychiatric Morbidity Survey data does not allow for analysis of the direction of causation in the associations between service use, costs and potentially associated factors. The data-set does not include information on the nature of the physician–patient relationship or attitudes towards service provision, which may influence individual decisions about use of services by patients with schizophrenia. Also, supply-side factors could not be considered, although they are likely to affect the availability of and access to services, and hence costs. In particular, in-patient services are sometimes used in place of less costly out-patient mental health services if the latter are not available (Reference Sullivan, Jackson and SpritzerSullivan et al, 1996; Reference Salvador, Haro and CabasesSalvador et al, 1999).
The interpretation of significant v. non-significant results is complicated by the potential co-linearity of variables. Preliminary analysis of the Psychiatric Morbidity Survey data found significant associations between non-adherence and age, education, illness severity, alcohol misuse and residential setting (further details available from the authors on request). Other models with different combinations of variables were tested, but we have reported here those that best summarised the associations found.
Study strengths
Despite the above limitations, the analyses are unusual in attempting to identify the factors associated with the use and cost of services by employing data from a national representative survey. In particular, the link with non-adherence is examined closely.
Non-adherence
A significant association between non-adherence and service use and costs has also been observed by Glazer & Ereshefsky (Reference Glazer and Ereshefsky1996), who concluded that measures taken to improve adherence are likely to decrease total direct treatment costs. Meta-analyses of data from a number of countries concluded that a 50% improvement in adherence would decrease 1-year rehospitalisation rates by 12% (Reference Weiden and OlfsonWeiden & Olfson, 1995).
Symptom severity and patient satisfaction
Our finding that costs of external service use were associated with severity of neurosis was consistent with results from a study comparing service use in five European locations (Reference Knapp, Chisholm and LeeseKnapp et al, 2002). Further results from the latter study indicated, however, that satisfaction with services was only weakly associated with demographic and clinical characteristics (Reference Ruggeri, Lasalvia and BisoffiRuggeri et al, 2004). We would expect satisfaction with services to be partly reflective of use of services.
Ethnicity
There is little published evidence on the relationship between ethnicity and service use in the treatment of schizophrenia. A study in the USA found that among adolescents, White students received more services in the early stages of treatment than did African American students, but this difference diminished over time (Reference Cuffe, Waller and AddyCuffe et al, 2001). A survey of US Medicare recipients found that among people under age 65 years, Whites were one-and-a-half times as likely as African Americans to receive an ambulatory care service and 1.3 times as likely to have received individual therapy (Reference Dixon, Lyles and SmithDixon et al, 2001). In a study based on UK data from the Fourth National Survey of Ethnic Minorities, among respondents with similar scores on the CIS–R, Caribbean respondents were less likely to have used therapist or social work services (Reference NazrooNazroo, 1999).
Our findings suggests that people from ethnic minorities are disproportionately more likely to access in-patient services and less likely to access external services; this suggests a substitution effect between these two types of services. It is possible that this pattern is the result of a differential response to symptoms by clinicians. For example, it may be the case that non-White patients are more likely than White patients to be admitted to hospital. Also, Nazroo (Reference Nazroo1999) suggests the possibility that if the instruments used underestimate rates of mental illness among certain ethnic minority groups, a larger proportion of those who were ill in these groups would not receive treatment. Another factor in this pattern of service use may be the lack of social support to encourage patients to access services. In the sample, 63% of White patients reported that they lived with an adult to whom they felt close, whereas the corresponding rate for non-Whites was only 42%. One study has suggested that the incidence of schizophrenia in non-White ethnic minorities increased significantly as the proportion of such minorities in the local population fell (Reference Boydell, van Os and McKenzieBoydell et al, 2001). This supports the inference that social isolation is likely to influence the types of resources used for psychiatric services.
Residential care
A study of residents of psychiatric nursing homes found family contact to be associated with greater likelihood of service use (Reference Anderson, Lyons and WestAnderson et al, 2001). Our analysis, which focused on data relating to residents of residential care homes, group homes and hostels, did not replicate this result. Residents with one or more family members to whom they felt close were no more likely to use in-patient services (odds ratio 0.83, 95% CI 0.32–1.34) or external services (OR 1.43, 95% CI 0.60–2.25).
An interesting finding was that rates of external service use decreased as severity of neurosis increased. This result was consistent with a US-based study of residents of an intermediate care facility, which also observed an inverse relationship between severity of illness and service use (Reference Anderson and LewisAnderson & Lewis, 1999), and its explanation might be that patients with more serious symptoms are more likely to be in a psychiatric hospital.
Age
Cuffel et al (Reference Cuffel, Jeste and Halpain1996) observed a non-linear relationship between age and service use. Total costs for schizophrenia were higher for the youngest (18–29 years) and the oldest cohorts (65–74 years and 74+ years). Our results did not indicate an association of this kind.
Illegal drug use
Interestingly, patients who reported illegal drug use incurred significantly lower costs when external services were accessed. This suggests that once accessed, relatively limited use of these services was made by these patients. This may reflect a lack of consistency on the part of drug users in accessing services.
Implications of the study
Service use and related costs appear to be associated with non-adherence, the degree of needs of the patient and the ability of the system to address these needs. It is important, therefore, to encourage interventions that improve adherence to medication regimens, such as reinforcement, education (for both patient and family) and memory enhancement (Reference Kemp and DavidKemp & David, 1996; Reference Fenton, Blyler and HeinssenFenton et al, 1997), and to consider the needs of individual patients when designing the delivery of services. The use of atypical antipsychotic medications, by reducing negative symptoms and improving compliance, may reduce service use and costs (Reference Mauskopf, David and GraingerMauskopf et al, 1999; Reference Sartorius, Fleischhacker and GjerrisSartorius et al, 2002).
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Non-adherence to medication regimens appears to be consistently associated with greater use of health services and higher service use costs.
-
▪ Interventions that improve adherence, including psychosocial therapies and better-tolerated medication, should be encouraged as they are likely to reduce service use costs.
-
▪ Services for patients with schizophrenia should be designed to meet individual needs, including those of people from ethnic minorities.
LIMITATIONS
-
▪ The cross-sectional nature of the Psychiatric Morbidity Survey data does not allow for analysis of the direction of causation in the associations between service use, costs, patient characteristics and other factors.
-
▪ The data-set did not include information on the supply of services, access to services, the nature of the physician–patient relationship or attitudes towards service provision, which might all influence the individual decisions regarding use of services by patients with schizophrenia.












eLetters
No eLetters have been published for this article.