The aims of therapy for bipolar disorder are to alleviate acute symptoms, restore psychosocial functioning, and prevent relapse and recurrence. The benefits of pharmacotherapy have dominated the literature on treatment. However, the efficacy of prophylaxis in research settings has not been matched by effectiveness in clinical practice. Lithium prophylaxis protects only 25-50% of people with bipolar disorder against further episodes (Reference Dickson and KendallDickson & Kendall, 1986), and the introduction of newer medications has not improved prognosis (Reference ScottScott, 1995a ).
Since the 1980s there has been a greater emphasis on stress-diathesis models. This has led to the development of new aetiological theories of severe mental disorders which emphasise psychological aspects of vulnerability and risk, and has also increased the acceptance of cognitive therapy as an adjunct to medication for individuals with treatment-resistant schizophrenia and with severe and chronic depressive disorders (Reference Scott, Wright, Frances and HalesScott & Wright, 1997). Research in bipolar disorder has been limited, but there is evidence that cognitive therapy may benefit this patient group.
IS THERE A PSYCHOLOGICAL MODEL OF BIPOLAR DISORDER?
At present, psychological theories of bipolar disorder have been insufficiently researched, and there are few insights to aid our understanding and explain how therapy achieves its effects (Reference Lam and WongLam & Wong, 1997; Reference Scott, Stanton and GarlandScott et al, 2000; Reference Palmer, Scott, George and BirchwoodPalmer & Scott, 2001). However, it is possible to use an adaptation of Beck's original cognitive model of depression and mania to increase its applicability to bipolar disorder (Reference Beck, Rush and ShawBeck et al, 1979; Reference ScottScott, 1995b ; Reference Beck and SalkovskisBeck, 1996). The description of this model should not be regarded as an empirical explanation of the aetiology of this disorder, but it provides a framework for understanding its psychopathology, and how cognitive and behavioural approaches may be targeted at specific symptoms and problems. Other psychological models of bipolar disorder, such as the ‘interacting cognitive subsystems’ and the ‘behavioural engagement system’ theories, are also being explored.
Early descriptions
Beck's original cognitive model suggests that depressed mood states are accentuated by patterns of thinking that amplify mood shifts. For example, as people become depressed they become more negative in how they see themselves, their world and their future (called the ‘negative cognitive triad’). Hence they tend to jump to negative conclusions, overgeneralise, see things in all-or-nothing terms, and personalise and self-blame to an excessive degree (cognitive distortions). Changes in behaviour, such as avoidance of social interaction, may be a cause or a consequence of mood shifts and negative thinking. Cognitive vulnerability to depression is thought to arise as a consequence of dysfunctional underlying beliefs (e.g. ‘I'm unlovable’), which develop from early learning experiences and drive thinking and behaviour. It is hypothesised that these beliefs may be activated by life events that have specific meaning for that individual (e.g. rejection by a significant other).
Beck's original model suggested that mania was a mirror image of depression and was characterised by a positive cognitive triad of self, world and future, and positive cognitive distortions. The self was seen as extremely lovable and powerful, with unlimited potential and attractiveness. The world was filled with wonderful possibilities, and experiences were viewed as overly positive. The future was one of unlimited opportunity and promise. Hyperpositive thinking (stream of consciousness) was typified by cognitive distortions, as in depression, but in the opposite direction: for example, jumping to positive conclusions (‘I'm a winner’, ‘I can do anything’); underestimating risks (‘there's no danger’); minimising problems (‘nothing can go wrong’); and overvaluing immediate gratification (‘I will do this now’). Thus, cognitive distortions provided biased confirmation of the positive cognitive triad of self, world and future. Positive experiences were selectively attended to, and it was suggested that in this way underlying beliefs and self-schemata that guide behaviours, thought and feelings were maintained and strengthened. It was also suggested that dysfunctional beliefs were likely to involve high levels of social desirability (Reference Winters and NealeWinters & Neale, 1985). Examples of such underlying beliefs and self-schemata include ‘I'm special’ and ‘being manic helps me to overcome my shyness’.
Beck's model of depression is well tested, with reliable and valid questionnaires applied in research settings. The model of mania, in contrast, is largely derivative, based on careful observation of patients in a manic state. Interestingly, a recent study of patients with bipolar disorder demonstrated that, between episodes of illness, patients show patterns of cognitive vulnerability similar to those of individuals with major depressive disorder (Reference Scott, Stanton and GarlandScott et al, 2000). In comparison with healthy control subjects, patients with bipolar disorder had more fragile, unstable levels of self-esteem, higher levels of dysfunctional attitudes (particularly related to need for social approval and perfectionism), over-general memory and poorer problem-solving skills. Scott et al (Reference Scott, Stanton and Garland2000) argued that even though it was not possible to determine whether these cognitive dysfunctions are a cause or a consequence of bipolar disorder, it was noteworthy that the difficulties persisted between episodes in patients who adhered to their prophylactic medication regimen. Furthermore, the beliefs identified (e.g. ‘I'm different’) are potentially dysfunctional when a positive or negative valence is applied to them.
Recent reformulations
Although Beck's earlier description (now termed the Linear Schematic Processing Model) has clinical validity, it fails to take into account the well-recognised biological aspects of vulnerability to bipolar disorder. Beck (Reference Beck and Salkovskis1996) has now concluded that a more complex model of cognitive processing (the Integrative Model) is needed to replace the original theory. Beck's reformulation includes two key additions: the concepts of ‘modes’ and ‘charges’, and further refinements about precipitants of shifts in mood and thinking. Modes are an integrated network of subsystems (cognitive, affective, motivational and behavioural schemata) which can act in synchrony to produce goal-directed strategies. Charges (energy levels) explain activation of the modes, and account for shifts from quiescent states (normal) to activated states (abnormal). Importantly for the cognitive theory of bipolar disorder, modes can be activated by external and internal events, and when this occurs congruent memories are also activated. An orienting schema, described by Beck as a ‘kind of algorithm’, sets the conditions necessary for activating the mode. It rapidly assigns a preliminary meaning to a situation and activation is spread across the network as the relevant mode is activated. In turn, this mode activates the schema. When a person is in a depressed or hypomanic/manic mode state the orienting schema requires less evidence to make the ‘match’.
The Integrative Model offers a possible explanation of the development of depression, mixed states or hypomania. It also argues that belief in the meaning of distorted thoughts leads to dysfunctional mood states. The goal of cognitive therapy is therefore to change dysfunctional interpretations as well as underlying dysfunctional beliefs (thus changing construct accessibility). Beck writes that therapy for dysfunctional modes involves deactivation, modification or neutralisation by the construction of an adaptive mode. This is achieved through interventions such as restructuring absolute and conditional rules (core schemata) that shape interpretations, or by learning new skills, which can be applied in adverse circumstances and inhibit the action of dysfunctional beliefs.
IS THERE A CLINICAL RATIONALE FOR USING COGNITIVE THERAPY?
The above description represents an unproved but important theoretical model (Reference Palmer, Scott, George and BirchwoodPalmer & Scott, 2001). While research continues on this and other models, clinicians should remember that there are some obvious and pragmatic reasons why cognitive therapy may benefit patients with bipolar disorder. First, cognitive therapy shares the characteristics of a clinically effective short-term psychological intervention (Reference ScottScott, 1995c ). Specifically, the therapy is highly structured and based on a coherent model, provides the patient with a clear rationale for the interventions made, promotes independent use of the skills learned, attributes change and progress to the individual's rather than the therapist's skilfulness, and enhances the individual's sense of self-efficacy. The second reason why cognitive therapy may be beneficial is that the clinical picture can be formulated into an acceptable generic or specific cognitive therapy model for all patients. At a specific level, understanding bipolar disorder and its impact on the individual requires a conceptualisation that encompasses cognitive (thoughts, images and beliefs), behavioural, effective, biological and environmental areas of the individual's life.
The approach outlined in Fig. 1 (adapted from Reference Basco and RushBasco & Rush, 1995) is particularly useful when working with individuals with bipolar disorder as it allows the therapist to emphasise a stress-diathesis model that may also include biological factors as precipitants of symptom shift. In order to use this approach, the therapist should first ask about the patient's own views on the causes of the disorder and the associated problems. The patient's aetiological theory is then incorporated within the framework of the model. Links between the individual's cognitions, behaviour, mood and other symptoms (particularly sleep disturbance) and the interaction between these and the environment (stressful events or experiences that are a cause or a consequence of other shifts) are emphasised. This rationale is used to engage the patient in cognitive therapy through monitoring and linking changes in thoughts, behaviours, feelings and the biological symptoms of bipolar disorder. The model also acknowledges that sleep disturbance may be a useful predictor of biological and/or psychosocial disruption and may act as an early-warning sign of shifts from euthymic to abnormal mood states (Reference Wehr, Sack and RosenthalWehr et al, 1987). When the connections between the biological and other aspects of their experience are exposed, patients are able to understand the reasons for using cognitive therapy as well as medication. This establishes the rationale for cognitive and behavioural interventions, and also provides a starting point to explore attitudes towards the use of, and adherence to, medication.
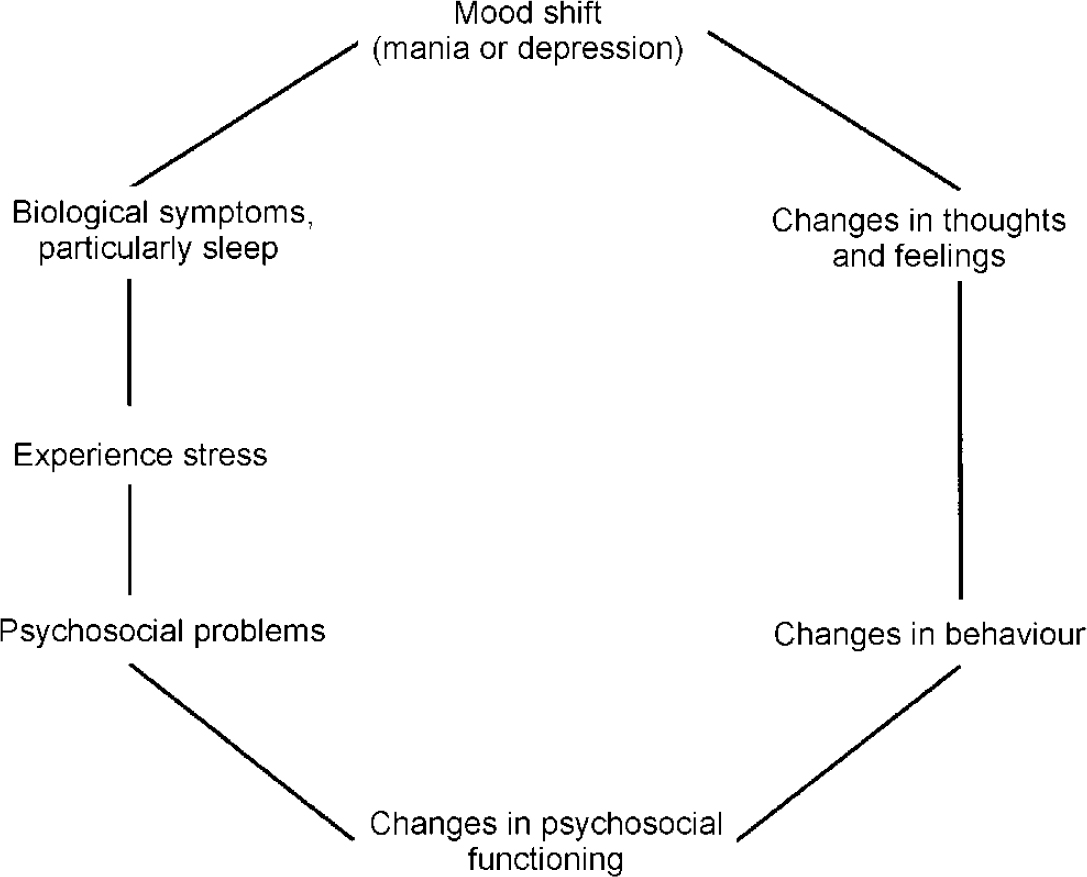
Fig. 1 Conceptualisation of bipolar disorder (adapted from Reference Basco and RushBasco & Rush, 1995).
The above approach is generally well received, particularly in the early stages of cognitive therapy, when the patient is trying to make sense of the disorder and the proposed treatment. Virtually all aetiological ‘theories’ can be incorporated in the model outlined, giving the patient confidence that the therapist is listening to these ideas and is trying to help make sense of them.
OVERVIEW OF COGNITIVE THERAPY
The goals of cognitive therapy in patients with bipolar disorder are to facilitate acceptance of the disorder and the need for treatment; to help the individual recognise and manage psychosocial stressors and interpersonal problems; to improve medication adherence; to teach strategies to cope with depression and hypomania; to teach early recognition of relapse symptoms and coping techniques; to improve self-management through homework assignments; and to identify and modify negative automatic thoughts, and underlying maladaptive assumptions and beliefs (see Reference Basco and RushBasco & Rush, 1995; Reference ScottScott, 1995b ). At the first session, patients are encouraged to tell their story and to identify problem areas through the use of a life chart. Current difficulties are then classified under three broad headings, as intrapersonal (e.g. low self-esteem, cognitive processing biases), interpersonal (e.g. lack of social network) and basic problems (e.g. symptom severity, difficulties coping with work). These are explored in 20 therapy sessions, held weekly for about 15 sessions and then with gradually reducing frequency. After this active phase, two ‘booster’ sessions are offered to patients (at about weeks 32 and 38) to review the skills and techniques learned. The overall programme comprises the following approaches (Table 1).
Table 1 Typical cognitive therapy interventions in bipolar disorder
| General coping strategies | Relapse prevention |
|---|---|
| Education and increasing knowledge | Identifying and modifying dysfunctional beliefs |
| Discussing symptoms, effect on lifestyle | Stressful events (specific personal meaning) |
| Information about treatments and outcome | High-risk behaviours (alcohol, drug use) |
| Encouraging questions, providing information | Relapse ‘signature’: identify two or three symptoms that are early-warning signs of relapse (avoid using mood, as misattributed as health) |
| Self-regulation | |
| Sleep, eating, exercise routines | Identify three components: depression-specific, mania-specific and idiosyncratic |
| Structured daily diary | |
| Determine action plans, e.g. increasing self-regulation and self-monitoring | |
| Self-monitoring | |
| Mood, thoughts, behaviours | Identify and modify core beliefs |
| Changes in symptoms with events or treatment | |
| Crisis management strategies | |
| Adherence management | Hierarchy of coping: stepwise action plan |
| Assume patient will not always adhere to medication regimen | Avoidance of major decisions |
| Prior agreements for action with family and clinicians | |
| Explore fears, attitudes and thoughts | |
| Discuss advantages and disadvantages | |
| Identify factors that increase or decrease risk of non-adherence |
Socialisation into the cognitive therapy model and development of an individualised formulation and treatment goals
Therapy begins with an exploration of the patient's understanding of bipolar disorder and a detailed discussion of previous episodes, focusing on identification of prodromal signs, events or stressors associated with onset of previous episodes, typical cognitive and behavioural concomitants of both manic and depressive episodes, and an exploration of interpersonal functioning (e.g. family interactions). Early sessions include development of an understanding of key issues identified in the life chart, education about the disorder, facilitation of adjustment to the disorder by identifying and challenging negative automatic thoughts, and developing behavioural experiments particularly focused on ideas about stigmatisation and fragile self-esteem. Other sessions are dedicated to collating accurate information and enhancing understanding about the epidemiology, treatment approaches and prognosis of the disorder, and the development of an individualised formulation of the patient's problems which takes into account underlying maladaptive beliefs.
Cognitive and behavioural approaches to symptom management and dysfunctional automatic thoughts
With the aid of information gathered previously, sessions are used to help the patient learn self-monitoring and self-regulation techniques, which enhance self-management of depressive and hypomanic symptoms, and to explore skills for coping with depression and mania. This involves establishing regular activity patterns, daily routines, regular sleep patterns, developing coping skills, time management, use of support, and recognising and tackling dysfunctional automatic thoughts about self, world and future using ‘automatic thought’ diaries.
Dealing with cognitive and behavioural barriers to treatment adherence and modifying maladaptive beliefs
Problems with adherence to medication and other aspects of treatment are tackled, for example through exploration of barriers (challenging automatic thoughts about drugs; beliefs about bipolar disorder and self-reliance; or exploring attitudes to autonomy and control) and by using behavioural and cognitive techniques to enhance treatment adherence (Reference ScottScott, 1999). This and data from previous sessions are used to help the patient identify maladaptive assumptions and underlying core beliefs, and to commence work on modifying these beliefs.
Anti-relapse techniques and belief modification
Further work is undertaken on recognising early signs of relapse and developing coping techniques in fortnightly sessions. Examples include self-monitoring of symptoms, identifying possible prodromal features (the ‘relapse signature’), developing a list of ‘at-risk’ situations (e.g. situations that activate specific personal beliefs), high-risk behaviours (e.g. increased alcohol intake), combined with a hierarchy of coping strategies for each; identifying strategies for managing medication intake and obtaining advice regarding it; and planning how to cope and self-manage problems after discharge from therapy. Sessions also include typical cognitive therapy approaches to the modification of maladaptive beliefs, which might otherwise increase vulnerability to relapse.
DOES COGNITIVE THERAPY IMPROVE OUTCOME?
Encouraging anecdotal and single case reports on the use of cognitive therapy in patients with bipolar disorder have been published over the past 20 years (Reference Chor, Mercier and HalperChor et al, 1980; Reference Wright, Schrodt, Freeman, Simon and BeutlerWright & Schrodt, 1992; Reference ScottScott, 1995b ). There is also a growing number of reports on the use of individual and group therapy in small-scale open or randomised controlled trials (Reference CochranCochran, 1984; Reference Palmer, Williams and AdamsPalmer et al, 1995; Reference Bauer and McBrideBauer & McBride, 1997; Reference Perry, Tarrier and MorrissPerry et al, 1999; Reference Lam, Jones and BrightLam et al, 2001; Reference Scott, Garland and MoorheadScott et al, 2001).
The aim of Cochran's study was to apply cognitive therapy to enhance adherence to prescribed lithium treatment. It compared 28 patients randomly assigned to either six sessions of group cognitive therapy or standard clinic care (Reference CochranCochran, 1984). Following treatment, enhanced lithium adherence was reported in the therapy group, where only three patients (21%) discontinued medication, compared with the standard clinic care group, where eight patients (57%) discontinued medication. There were fewer hospitalisations in the group receiving cognitive therapy.
In an exploratory study by Palmer et al (Reference Palmer, Williams and Adams1995), six patients with bipolar disorder were offered cognitive therapy in a group format. The focus of the programme was psychoeducational, recognising the process of change, strategies for coping and interpersonal problems. Overall findings indicated that group therapy combined with mood-stabilising medications was effective for some of the participants. Improvements were found in symptomatology and in overall social adjustment. All participants improved on one or more measures, although the pattern of change varied across individuals. A more recent study by Palmer et al (presented at the annual meeting of the British Association of Behavioural and Cognitive Psychotherapists, Durham, UK, 1998; further details available from J.S. upon request) included a larger number of participants receiving group cognitive therapy (n=25) and a comparison group (n=12) receiving only treatment as usual. The results showed that there was no difference in mood state between groups, but, in comparison with the control group, cognitive therapy reduced non-specific symptomatology and increased social adjustment.
The Life Goals programme developed by Bauer & McBride (Reference Bauer and McBride1997) is a structured, manual-based intervention which seeks to improve patients' management skills and their social and occupational functioning. Although outcome data are not yet available, an analysis of data on process goals showed that the manual could be used by therapists inexperienced in treating bipolar disorder. Furthermore, the programme was effective in terms of knowledge gained and goals achieved by patients (Reference Bauer and McBrideBauer & McBride, 1997).
Perry et al (Reference Perry, Tarrier and Morriss1999) undertook the largest study so far (n=68), using cognitive and behavioural techniques to help people identify and manage early-warning signs of relapse in a group of patients at high risk of further episodes of bipolar disorder. In comparison with the control group, the intervention group had significantly fewer manic relapses, significantly fewer days in hospital, higher levels of social functioning and better work performance. However, the intervention did not have a significant impact on depression, and the researchers suggested that more formal cognitive therapy might be important to produce significant changes in this area.
A pilot study by Scott et al (Reference Scott, Garland and Moorhead2001) examined the effect of 20 sessions of cognitive therapy in 42 patients with bipolar disorder. Patients were randomly allocated to this therapy in addition to treatment as usual, or to a waiting-list control condition of treatment as usual for 6 months followed by cognitive therapy plus treatment as usual. Preliminary results show cognitive therapy plus treatment as usual may offer some benefit to about 70% of these patients and is a highly acceptable treatment intervention (90% of subjects endorsed this approach). The results also suggest that cognitive therapy plus treatment as usual v. treatment as usual alone may lead to fewer relapses, as well as reducing levels of both depression and mania, and improving self-esteem and self-reported adherence to medication. An out-patient study of similar size (n=25) and design demonstrated comparable results, with additional significant improvements in social adjustment (Reference Lam, Jones and BrightLam et al, 2001).
CONCLUSION
Cognitive therapy appears to be an effective approach in the treatment of bipolar disorder; but the development of a more coherent and empirical model will require a greater understanding of individual vulnerability factors that may influence onset or outcome of episodes of mania, depression or mixed states. More research on commonly shared underlying beliefs in individuals at risk of this disorder, attitudes towards the disorder and views about its treatment will also aid our understanding of adjustment difficulties and psychological barriers to engagement or adherence to treatment and good outcome.
On the evidence available, it appears that cognitive therapy has particular characteristics that may benefit patients with bipolar disorder. Its collaborative, educational style, and the use of a stepwise approach and of guided discovery, make it acceptable to individuals who wish to take an equal and active role in their therapy (Reference Beck, Rush and ShawBeck et al, 1979; Reference ScottScott, 1995b ). This is important as many individuals with this disorder resist and challenge a didactic approach to treatment (Reference Miklowitz and GoldsteinMiklowitz & Goldstein, 1990). However, cognitive therapy is not the only short-term therapy that can be used: psychotherapies of proven effectiveness in major depressive disorder, such as interpersonal and family therapies, are also being piloted in bipolar disorder.
Finally, larger-scale treatment intervention studies will be needed to establish the effectiveness of cognitive therapy and to differentiate between the specific and non-specific benefits of therapy. Ultimately, it is important for clinicians and researchers to know not only whether the use of this form of therapy is indicated, but also whether it helps the individual with bipolar disorder because it enhances medication adherence, changes cognitive representations of the disorder, leads to the development of compensatory skills, or reduces vulnerability to relapse through schema change. Such research will also allow for the further exploration of the complex interplay between psychological, social and biological factors.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Clinicians need to consider more integrated psychobiosocial models of treatment for patients with bipolar disorder.
-
▪ Cognitive therapy offers a coherent clinical approach to the psychological and social problems associated with bipolar disorder.
-
▪ Techniques derived from cognitive therapy aimed at enhancing adherence or managing early-warning signs may be readily incorporated into day-to-day practice.
LIMITATIONS
-
▪ There is no psychological model that coherently explains the onset of mania.
-
▪ There are relatively few published trials of psychological treatments for bipolar disorders.
-
▪ No extended follow-up data are available on any longer-term benefits of adding cognitive therapy to usual treatment.





eLetters
No eLetters have been published for this article.