Suicide is a serious and global public health problem (Reference Bertolote, Fleischmann and LeoBertolote et al, 2003). It has been estimated that in the year 2000, 814000 people died by suicide worldwide (World Health Organization, 2001). It has also been estimated that for every suicide six people will suffer intense grief in the aftermath (Reference Clark, Goldney, Hawton and van HeeringenClark & Goldney, 2000). In the Western world, suicide rates for men vary between 5.5 per hundred thousand in Greece and 43.6 per hundred thousand in Finland, and for women they vary (per hundred thousand) between 1.4 in Greece and 15.6 in Denmark (World Health Organization, 1996). In those aged between 15 and 34, suicide is now one of the three leading causes of death worldwide (Reference Bertolote, Fleischmann and LeoBertolote et al, 2003).
Suicide – an issue for psychiatrists
Suicide as a behaviour associated with mental illness was being studied as far back as the 1880s (Reference MorselliMorselli, 1881). Recent studies show that in England and Wales the annual suicide rate is 10.0 per hundred thousand and in Scotland it is 17.3 per hundred thousand (Department of Health, 2001). Half of all people who die by suicide have had previous contact with mental health services, and half of this group (i.e. one-quarter of all people who die by suicide) have had contact in the year before death (Reference Appleby, Hawton and van HeeringenAppleby, 2000; Department of Health, 2001). Psychological autopsy studies have confirmed a major association with mental illness. As many as nine out of ten individuals who die by suicide have a mental disorder at the time of their death, with about five out of ten suffering from primary depression (Reference Clark, Horton-Deutsch, Maris, Berman and MaltsbergerClark & Horton-Deutsch, 1992; Reference Lonnqvist, Hawton and van HeeringenLonnqvist, 2000).
The assessment and management of suicide risk is clearly regarded by the public and by psychiatrists themselves as an important part of a psychiatrist’s job. In a themed issue of the BMJ, the Editor declared, ‘Many doctors are not good at communicating risk – yet increasingly it is one of their central tasks’ (Reference SmithSmith, 2003). It is self-evident that to be good communicators of risk we have also to be good at understanding the nature of risk and how to manage it in daily practice.
Approaches to risk assessment
Traditionally, risk assessment has focused on prediction: for example, in forensic psychiatry the psychiatrist predicts whether a patient is dangerous and therefore at risk of committing a violent act (Reference MonahanMonahan, 1981, Reference Monahan1996). Overall, however, predictions have not been impressive (Reference Webster, Bailes and HollonWebster & Bailes, 2004). In more recent times, risk assessment systems have attempted to unite research evidence with clinical practice. Risk assessment tools in forensic psychiatry have begun to incorporate aspects of risk management. Risk assessment has been reformulated as ‘the process of identifying and studying hazards to reduce the probability of their occurrence’ (Reference HartHart, 1998). In other words, there has been a shift from a preoccupation with prediction to making the central concern that of prevention.
There are three broad approaches to assessment of risk: clinical, actuarial and structured professional judgement. For an excellent review, we recommend Reference Douglas, Cox and WebsterDouglas et al(1999).
The clinical approach
In the clinical approach, decisions are made on the basis of clinicians’ judgement. This judgement is informed by the evidence base, but it is also subjective, intuitive and informed by experience. In suicide risk assessment, decisions are made about treatment, supervision and hospitalisation on the basis of professional opinion. Such decisions have been criticised on the grounds that they may be based on feeling as much as on evidence.
One problem with the clinical approach is the inaccuracy of clinicians’ predictions. In the history of forensic psychiatry and violence risk assessment there is considerable evidence to indicate poor predictive efficacy of clinical judgement alone (Reference MonahanMonahan, 1981; Reference Grove and MeehlGrove & Meehl, 1996). Governmental committees considering violence risk assessment have gone further, stating that clinical approaches cannot continue to be supported and that they are unsustainable in risk assessment (Scottish Executive, 2000).
The actuarial approach
The actuarial approach to risk assessment has been promulgated as a reaction to concerns about clinical judgement. This approach, popularised in forensic psychiatry in the USA, uses assessment methods that are formal, algorithmic and follow objective procedures for classifying risk. The ultimate goal is to arrive at a probability or numerical statement of the risk of a future outcome: for example, patient A has a 40% chance of committing a violent act in the next 3 years. In forensic psychiatry, the actuarial approach may be the most accurate approach to date for the assessment of violence and sexual offending (Reference Dvoskin and HeilbrunDvoskin & Heilbrun, 2001).
One problem, however, is that risk probabilities or predictions do not inform clinicians about the circumstances, severity or imminence of the act in question. The risk statement about patient A may be mathematically ‘correct’, but it is of limited usefulness in informing management, especially in the short term. In clinical practice the formulation, based on patient-centred information, is the central concern. Another, more crucial, problem is the inability of this approach to take into account fluctuations in the level of risk as circumstances change.
Structured professional judgement
Structured professional judgement is an approach to risk assessment and not a specific instrument. The aim is to combine the evidence base for risk factors with individual patient assessment. Structured professional judgement assists but does not replace psychiatric opinion. Clinicians make a structured assessment, which is used in the formulation of a risk management plan. This by necessity brings risk assessment and management into the domain of multidisciplinary teams.
Structured professional judgement is useful not only for supporting evidence-based practice, but also for increasing the transparency of decision-making for the purposes of clinical governance. Risk assessment instruments based on structured professional judgement (for example, the HCR–20 Assessing Risk for Violence; Reference Webster, Douglas and EavesWebster et al, 1997) have been used largely in forensic settings and have not lent themselves to use by general psychiatrists in ordinary clinical settings. Until recently no such system has been available for use by psychiatric teams working with patients at risk of suicide (Reference Bouch and MarshallBouch & Marshall, 2003).
Types of risk factor in suicide
Suicide risk factors can be categorised as static, stable, dynamic and future (Reference Bouch and MarshallBouch & Marshall, 2003). Static risk factors are fixed and historical: for example where a patient has a family history of suicide. Stable risk factors are long term and likely to endure for many years, but are not fixed: for example in a patient who has a diagnosis of personality disorder. Actuarial methods rely solely on the assessment of static and stable risk factors (Box 1).
Box 1 Static and stable risk factors for suicide
-
• History of self-harm
-
• Seriousness of previous suicidality
-
• Previous hospitalisation
-
• History of mental disorder
-
• History of substance use disorder
-
• Personality disorder/traits
-
• Childhood adversity
-
• Family history of suicide
-
• Age, gender and marital status
Dynamic risk factors (Box 2) are present for an uncertain length of time. They may fluctuate markedly in both duration and intensity: for example where a patient has acute anxiety symptoms. In the short term, a single event may trigger dramatic changes to a number of risk factors, thus multiplying the overall risk.
Box 2 Dynamic risk factors for suicide
-
• Suicidal ideation, communication and intent
-
• Hopelessness
-
• Active psychological symptoms
-
• Treatment adherence
-
• Substance use
-
• Psychiatric admission and discharge
-
• Psychosocial stress
-
• Problem-solving deficits
Future risk factors (Box 3) can be anticipated and will result from the changing circumstances of the individual: for example the forthcoming discharge of a patient from an acute in-patient unit.
Box 3 Future risk factors for suicide
-
• Access to preferred method of suicide
-
• Future service contact
-
• Future response to drug treatment
-
• Future response to psychosocial intervention
-
• Future stress
Static and stable risk factors often give an indication of an individual’s general propensity for suicide. They do not, however, capture the fluctuating nature of risk. Assessing dynamic and future risk factors is essential for considering the particular conditions and circumstances that place individuals at special risk. More importantly, assessment of dynamic and future risk factors will inform clinical management. A comprehensive risk assessment provides a formulation of risk based on static, stable, dynamic and future risk factors to inform risk management strategies. This is only possible using structured professional judgement.
Issues for evidence-based management
Numerous studies have clearly delineated the risk factors associated with suicide, and lists of these are ubiquitous in psychiatric texts. Suicide remains an infrequent outcome, however. It has not been possible to delineate causal factors. Prediction of suicide has revealed unacceptably low specificity. In other words, there has been a high rate of false positives. Many treatment studies make suicidality an exclusion criterion. Although a strong association with mental illness has been clearly shown, it has not been proven that specific treatments are ‘anti-suicidal’. For example, of drug treatments only lithium (Reference Tondo, Jamison and BaldessariniTondo et al 1997, Reference Tondo, Baldessarini and Hennen1998) and possibly clozapine (Reference Meltzer and OkayliMeltzer & Okayli, 1995; Reference Duggan, Warner and KnappDuggan et al, 2003) appear to have specific anti-suicidal effects.
Traditionally in mental health services the responsibility for management of suicidal patients (especially where there is imminent risk or high long-term risk) devolves to consultant psychiatrists. This may in part be because of the anxiety experienced by more junior staff when feeling ‘responsible’ for patients whom they perceive to be at risk of dying as a direct result of their actions (or inaction). Isabel Menzies Lyth, in a series of ground-breaking studies which looked at nursing systems in both general and psychiatric hospitals, referred to ‘the reduction of the impact of responsibility by delegation to superiors’ as a means by which such anxieties could be diffused (Reference Menzies LythMenzies Lyth, 1988).
Perhaps because of this upward delegation to consultant psychiatrists there is an emphasis on a biomedical approach. The main risk is perceived as being directly due to mental illness, and the main interventions considered are medication, hospitalisation or both as treatments of mental illness. There is good face validity that such interventions are helpful at times, albeit that there is a lack of evidence that they lead to the prevention of suicide. What may be overlooked, however, is that both interventions are major risk factors in themselves.
Treatment with medication may give access to a method for suicide (Reference Kapur, Mieczkowski and MannKapur et al, 1992). The National Confidential Inquiry found that over one-third of suicides by people in contact with mental health services in the 12 months before death resulted from self-poisoning with psychotropic medication (Department of Health, 2001). Side-effects such as akathisia (Reference Power and CowenPower & Cowen, 1992) increase suicide risk. Problematic side-effects may also lead to a negative attitude to, or outright rejection of, treatment (Reference De Hert, Peuskens, Hawton and van HeeringenDe Hert & Peuskens, 2000). Rebound phenomena may also be important. The abrupt discontinuation of lithium leads to sharply elevated risk of suicide (Reference Baldessarini, Tondo and FaeddaBaldessarini et al, 1996).
The National Confidential Inquiry found that 16% of suicides by people in contact with mental health services in the 12 months before death occurred during in-patient admission. With regard to suicides in the community, 30% occurred in the 3 months after discharge from psychiatric hospital (Department of Health, 2001). The recurrence of severe mental disorder such as severe depression associated with hospitalisation leads to a cumulative risk of suicide (Reference Davies, Naik and LeeDavies et al, 2001).
With a predominantly biomedical approach, social and psychological risk factors are given much less weight and psychosocial interventions, basic engagement strategies (carried out by community mental health teams) and social systems interventions (supporting and involving patients’ social networks) may as a consequence be relatively neglected (Reference Bridgett and PolakBridgett & Polak, 2003a , Reference Bridgett and Polak b ).
Clinical illustrations
A significant number of patients in contact with mental health services are at long-term high risk of suicide. Consider, for example, Peter.
Clinical illustration 1 Peter
Peter is now 25 years old, and he has had contact with the local psychiatric service since he was 18. His early years were characterised by parental neglect and abuse. He developed a drug habit at the age of 14, with harmful use of both cannabis and amphetamines, and became alcohol dependent in his 20s. Contact with mental health services was because of psychotic episodes, initially short lived, but progressing in both duration and severity. A series of admissions followed, each of which was characterised by psychotic symptoms, drug misuse and social adversity. A diagnosis of paranoid schizophrenia with an episodic course and progressive deficit was established.
He has made three significant suicide attempts and has also taken overdoses on a number of occasions, with less clear suicidal intent. The most significant attempt made on his life was 10 months ago. His mood had been low for several days and he reported having been ‘tortured by the voices’. He determined to kill himself by lying on a railway line. He left a suicide note addressed to his sister. He drank a large amount of alcohol and then went to the railway line. He was, however, seen by a railway worker, who raised the alarm and he was apprehended.
Adherence to treatment has been erratic in the past. For a period Peter was maintained on depot medication, but he became unwilling to take medication in this form. For the past few years he has been prescribed an oral antipsychotic. He reports good adherence, but at times when questioned further it has been suspected that he takes the medication only intermittently and at variable doses.
He has a limited social network and no friends. His only significant contact is with one of his two older sisters, whom he visits every month or so. Recently, he reported that he has continuing thoughts that life is not worth living, that he feels little hope for the future and that he is constantly anxious and worried. He talked of his belief that a group of people in the area where he lives wish to kill him, that they follow him about and are able to read his thoughts. He also talked of hearing voices in his head saying, ‘He’s useless… he hasn’t got the guts to do it… he should kill himself’. Despite this, he states that he does not wish to die and it is many months since he felt suicidal.
Multiple risk factors are clearly evident, as is the precariousness of his present situation. One can hardly be reassured that suicide risk is not high, even though his condition is relatively stable at present. A distressing life event, a change in circumstances or a temporary substance-induced alteration of mental state could easily tip him over into being at imminent risk. This can be illustrated diagrammatically, as in Fig. 1.
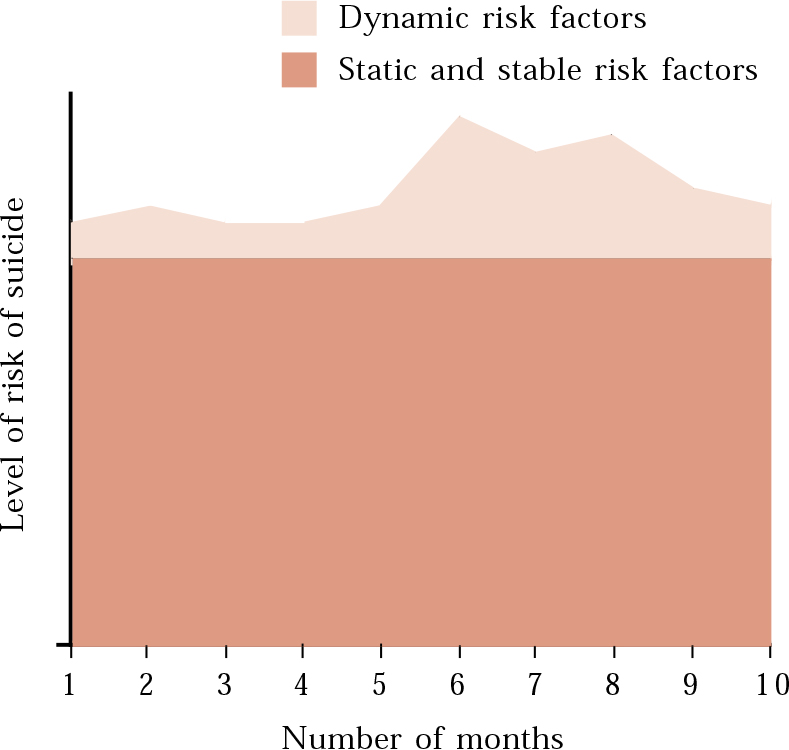
Fig. 1 Chronic high risk due to static and stable risk factors.
A significant number of suicides occur in people who have had no contact with mental health services. Psychological autopsy studies provide a methodology by which such suicides can be analysed (Reference Hawton, Appleby and PlattHawton et al, 1998). A recent high-profile case for which a psychological autopsy was carried out is the death by suicide of David Kelly, the weapons inspector in Iraq.
Clinical illustration 2 Dr David Kelly
The Hutton Inquiry included an extremely detailed investigation into the circumstances of Dr Kelly’s death by Professor Keith Hawton, Director of the Centre for Suicide Research, Oxford, an eminent international expert in suicide (Lord Hutton, 2004: chapter 10). Professor Hawton had access to reports compiled by the forensic toxicologist and the Home Office forensic pathologist. He saw Dr Kelly’s personnel and general practitioner (GP) records, in addition to statements that his GP, friends, family, ambulance personnel and others had made to the police. He saw notes of recent interviews with Dr Kelly and watched a videotape of him giving evidence to the Foreign Affairs Committee. He personally interviewed the coroner, family members, friends and a member of Dr Kelly’s religious community and had discussions with the police. He saw phone records and e-mails sent and received in the days and hours leading up to the death.
Dr Kelly’s death by suicide was completely unexpected by all who knew him and ‘would not have been an outcome one would have predicted’. Risk factors were minimal. He was in good health, had no past psychiatric history and did not appear to be suffering from a mental disorder at the time of his death. He had given up alcohol following his religious conversion, but even before had only ever had a normal social level of consumption. He had never spoken of thoughts of suicide. He had good family supports, enjoyed his work, had no financial worries and had a deep religious faith. As a person he was a perfectionist, intensely private and not given to anger or its expression, but there was no suggestion of personality disorder or even abnormal personality traits. In the year or so before his death he was noted as showing some signs of tiredness and strain, having been increasingly busy at work over a 2-year period. He had not taken holidays and was less involved with interests outside work. Nevertheless, he was eating and sleeping well and able to enjoy vigorous walks.
The investigation into the Gilligan affair (Andrew Gilligan, BBC Radio 4 defence correspondent, who alleged that the government had altered information in a dossier relating to Iraq’s military capabilities) was the clear precipitant to Dr Kelly’s suicide. In particular, Professor Hawton remarked that it ‘challenged his identity of himself, his self-esteem, his self-worth, his image of himself as a valued and loyal employee and as a significant scientist’ and noted ‘his dismay at being exposed to the media’. Professor Hawton’s conjecture with regard to the latter was that ‘he would have seen it as being publicly disgraced’ and he further conjectured ‘that he had begun to fear he would lose his job altogether… that would have filled him with a profound sense of hopelessness’.
On the day of his death, in the late morning Dr Kelly sent a series of e-mails to colleagues, ex-colleagues and professional acquaintances which mentioned briefly the difficulties he was facing, but also conveyed a sense of ‘optimism’ regarding his intentions to return to working in Iraq. A short while later he emerged from his study appearing distressed and uncommunicative with his wife. An hour or two later he went for a walk, took an overdose of 30 coproxamol tablets and cut both wrists, which resulted in his death.
Such a situation is illustrated in Fig. 2.
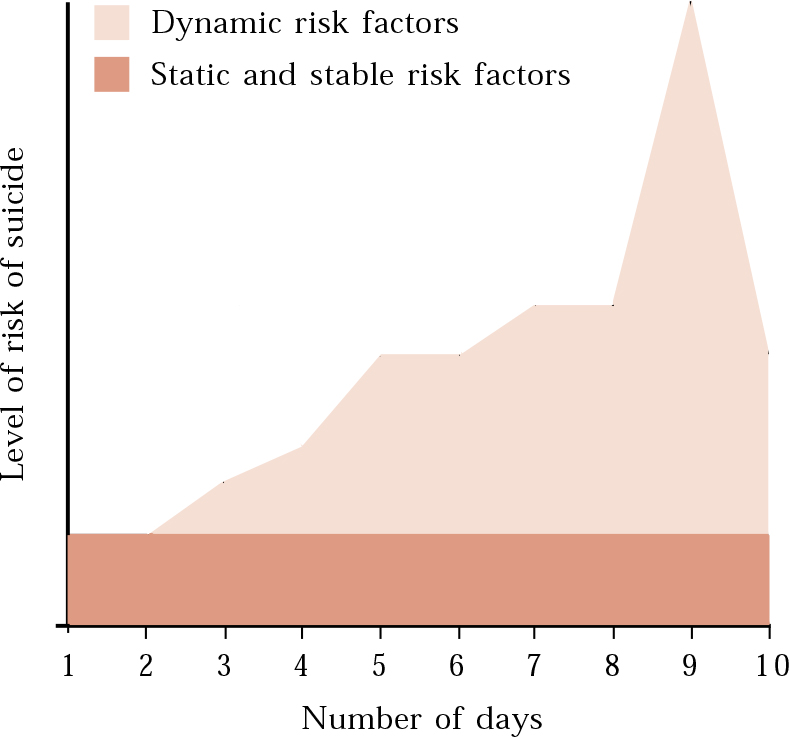
Fig. 2 Rapid onset and resolution of dynamic risk factors.
Discussion of clinical illustrations
Peter’s case shows a man at long-term high risk of suicide. This is because of a large number of static and stable risk factors. Dynamic risk factors are also present, which potentially could be reduced by a coordinated treatment plan combining psychological, pharmacological and psychosocial strategies. In addition, it is possible to anticipate the sorts of situation in which he will be at increased risk in the future. Although it may not be possible to predict his suicide, it is possible to use risk management strategies to reduce exposure to future risk factors (e.g. by removing toxic medication from his house) or to limit their impact (e.g. by using approaches aimed at maximising his attendance and his adherence to treatment). His risk management plan is shown in Box 4.
Box 4 Risk management plan for Peter
Short-term plans
-
1 Community psychiatric nurse (CPN) keyworker to persuade Peter that old medication should be removed from his home
-
2 CPN to arrange a home visit with a project worker from the voluntary sector with a view to befriending
-
3 CPN to encourage Peter to attend the resource centre (the base of the community mental health team), for both formal appointments and informal use of the drop-in facility
Medium- and long-term plans
-
1 CPN and psychiatrist to persuade Peter to see the clinical psychologist, to address his hopeless and pessimistic thinking and treatment-interfering beliefs, as a prelude to cognitive–behavioural therapy. CBT targets would be to improve problem-solving skills and strategies for coping with delusions and hallucinations
-
2 Psychiatrist to continue discussions with Peter regarding possible change of medication to clozapine
-
3 CPN to monitor and advise Peter regarding healthy lifestyle, including his drinking pattern and use of other substances
-
4 Voluntary-sector project worker to befriend Peter and help him to structure his day and introduce him to low-key social group activities
-
5 CPN to explore use of housing benefit to purchase home support to address basic aspects of the maintenance of his tenancy, including paying bills, relationships with neighbours and attending to basic domestic chores
-
6 To review the risk management plan after 3 months
The second case, that of David Kelly, illustrates a number of important cautions. First, suicide may not be predictable. Second, multiple risk factors are not always present in high-risk individuals. Only one or two risk factors present to a serious degree may be sufficient. Third, risk can escalate rapidly over a short period (and, if the outcome is not fatal, may just as quickly subside).
These cautions also apply, at least to some extent, to the first case. When suicide occurs in long-term high-risk patients such as Peter, the fact of suicide may not be surprising, but the circumstances and timing often are. Risk can also rapidly escalate and subside in just the same way.
Applying structured professional judgement in suicide
Assessing and planning the management of a patient at risk of suicide involves a number of stages:
-
1 identifying whether the patient requires a full structured risk assessment: such an assessment is not necessary for all patients attending mental health services;
-
2 detailing the risk factors present: assessing static, stable, dynamic and future risk factors and paying particular attention to combinations that elevate risk, for example where a patient has a diagnosis of severe recurrent depressive disorder and has had numerous admissions for suicidality (Reference Davies, Naik and LeeDavies et al, 2001);
-
3 considering the individual formulation of risk: to what extent the risk is determined by static and stable risk factors and/or dynamic and future risk factors; whether any protective factors (such as concerns for dependent children and religious beliefs) that reduce the level of risk are operating (Reference Jacobs, Brewer, Klein-Benheim and JacobsJacobs et al, 1999);
-
4 considering possible interventions and the level of support required: if the risk is determined mostly by static and stable risk factors then long-term supportive/maintenance management strategies will be most appropriate; if there are significant dynamic and future risk factors, management strategies will be focused on attempting to modify them (such strategies will include building on protective factors, reducing exposure to particular situations, and pharmacological and psychosocial interventions);
-
5 anticipating the impact of possible interventions: interventions themselves (e.g. hospitalisation) may significantly affect a number of risk factors other than those immediately intended; it is therefore important to anticipate the potential impact before implementation;
-
6 developing the management plan: determining a coordinated set of interventions for those involved in the management of the patient (for an example see Box 4);
-
7 reviewing and revising the management plan in the light of any changes to dynamic and future risk factors: risk is fluid and constantly varying and thus continuous assessment is always necessary.
Conclusions
Psychiatrists are routinely expected to assess patients’ suicide risk and to take the lead role in developing treatment and management strategies to reduce any risk identified. The poor predictive efficacy of the traditional approach, based on clinical judgement, could be enhanced by the more comprehensive method of structured professional judgement. This is a systematic and transparent approach that combines the assessment of risk factors, formulation and risk management. Even though the interaction between risk factors is highly complex, risk assessment can be improved and perhaps even save lives (Reference Amsel, Mann and van HeeringenAmsel & Mann, 2001). Real-world approaches to structured professional judgement are now required to enable clinical teams to incorporate it into routine clinical practice (Reference Bouch and MarshallBouch & Marshall, 2003).
MCQs
-
1 Structured professional judgement:
-
a is based on the clinician’s intuition
-
b increases the transparency of the decision-making process
-
c takes into account fluctuations in the patient’s circumstances
-
d is a mathematically based approach
-
e takes account of static, stable, dynamic and future risk factors.
-
-
2 Static risk factors:
-
a are of no importance in determining the level of risk of suicide
-
b influence the type of treatment intervention chosen
-
c may change very slowly over time
-
d are always high in completed suicides
-
e may render a patient at high risk of suicide throughout life.
-
-
3 Dynamic risk factors:
-
a may change in response to treatment
-
b anticipate changes in the patient’s circumstances
-
c change only very slowly over time
-
d may change suddenly, leading to unpredictable suicide
-
e will never change throughout a patient’s lifetime.
-
-
4 Risk of suicide may be increased:
-
a if the patient has a family history of suicide
-
b when the patient is about to be discharged from hospital
-
c if the patient has immediate access to a preferred method of suicide
-
d if the patient has poor problem-solving abilities
-
e where the patient is known to make immediate contact with mental health services at times of suicidal ideation.
-
-
5 Management of patients at risk of suicide:
-
a should always include medication where there is a history of mental disorder
-
b should be reviewed in the light of changing dynamic and future risk factors
-
c might include cognitive therapy aimed at reducing hopelessness
-
d may be excessively biomedical owing to upward delegation of responsibility to consultants
-
e may involve considering interventions that result in increased risk owing to changes in dynamic risk factors.
-
MCQ answers
| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | F | a | F | a | T | a | T | a | F |
| b | T | b | F | b | F | b | T | b | T |
| c | T | c | F | c | F | c | T | c | T |
| d | F | d | F | d | T | d | T | d | T |
| e | T | e | T | e | F | e | F | e | T |





eLetters
No eLetters have been published for this article.