Malnutrition is an important and still rather under-recognised problem in health care( Reference Waitzberg, Caiaffa and Correia 1 – Reference Vanderwee, Clays and Bocquaert 8 ). Malnutrition refers to negative deviations from a normal nutritional status, and it has been defined as inadequate nutritional status, undernourishment due to poor dietary intake, poor appetite, muscle wasting and weight loss( Reference Chen, Schilling and Lyder 9 ). Elia( Reference Elia 10 ) defined malnutrition as a nutritional condition in which an insufficient or disproportionate intake of energy, protein and other nutrients adversely affects tissue/body form (shape, size and composition) and function, and clinical outcomes.
Malnutrition increases the chance of complications. It worsens the immune function, leading to a higher risk of infections, and impairs wound healing. Moreover, malnutrition impairs the quality of life and increases the length of hospital stay and costs of health care( Reference Green 11 – Reference Meijers, Halfens and Wilson 17 ).
Prevalence rates of malnutrition vary enormously internationally( Reference Meijers, Schols and Van Bokhorst-de van der Schueren 7 , Reference Donini, De Felice and Cannella 18 – Reference Westergren, Lindholm and Axelsson 22 ), since in European nursing homes, the prevalence rates of malnutrition have been found to range between 2 and 74 %( Reference Volkert, Kreuel and Heseker 23 – Reference Meijers, Halfens and Van Bokhorst-de van der Schueren 25 ). These variations can partly be explained by differences in methodology and instruments used to measure malnutrition, and also resident characteristics can have an influence( Reference Westergren, Wann-Hansson and Bergh Börgdal 26 ). For instance, age, sex, morbidity and care dependency are related to malnutrition( Reference Stratton, Green and Elia 4 , Reference Chen, Schilling and Lyder 9 , Reference Gaskill, Black and Isenring 19 , Reference Meijers, Halfens and Van Bokhorst-de van der Schueren 25 – Reference Aliabadi, Kimiagar and Ghayour-Mobarhan 29 ), as well as to infections( Reference Vitale 30 ), physical disabilities( Reference Oliveira, Fogaça and Leandro-Merhi 31 ) and polypharmacy( Reference Heuberger and Caudell 32 , Reference Jyrkkä, Mursu and Enlund 33 ).
The aim of the present study was to investigate whether resident characteristics influence possible differences in malnutrition prevalence between countries, when using the same measurement methodology and instruments. The present hypothesis was that various resident characteristics influence differences in the prevalence rates of malnutrition between The Netherlands, Germany and Austria.
The following research questions will be investigated: (1) What is the prevalence rate of malnutrition in nursing homes in The Netherlands, Germany and Austria? (2) Are the characteristics of malnourished residents different in the three countries? (3) Which resident characteristics influence malnutrition? (4) Is the prevalence of malnutrition in nursing homes in The Netherlands, Germany and Austria different when controlling for the resident characteristics that influence the difference in malnutrition prevalence?
Methods
For the present study, data were used from the National Prevalence Measurement of Care Problems (in Dutch, Landelijke Prevalentiemeting Zorgproblemen (LPZ)), which is executed annually. Since 2004, the LPZ has been measuring the prevalence, prevention and treatment of malnutrition and quality indicators of nutritional care. It involves an annually conducted measurement in different health care settings (hospitals, long-term care and home care)( Reference Halfens, Meesterberends and Meijers 34 ). In 2008, the LPZ measurement expanded internationally to Germany and Austria (LPZ-International). In each country, data are gathered with the same instruments according to the same procedure. These countries conduct the same standardised measurement, supported by the project group of the LPZ( Reference Nie van, Schols and Lohrmann 35 ). In each country, the coordination of the LPZ is carried out by a national project group led by a national coordinator. The Dutch LPZ project group facilitates each participating country with all documents and a website in their own language to enable them to promote, support and carry out the measurement. Each year, the national coordinators have an international research group meeting to discuss relevant issues and updates concerning possible changes in questionnaires, measurement procedures and cooperations( Reference Bartholomeyczik, Reuther and Luft 20 , Reference Schönherr, Halfens and Meijers 36 , Reference Nie van, Meijers and Schols 37 ).
Design
The LPZ uses a cross-sectional, multi-centre design. For the present study, the data of LPZ-International collected in April 2009 and April 2010 in Dutch, German and Austrian nursing homes were analysed.
Instrument
Data were gathered using a standardised questionnaire at the patient level. As demographic data, age, sex, date of admission, co-morbidity, care dependency, weight, height and unintentional weight loss were measured. Malnutrition was operationalised and validated according to Meijers( Reference Meijers 38 ) and Meijers et al. ( Reference Meijers, Schols and Van Bokhorst-de van der Schueren 7 , Reference Meijers, Van Bokhorst-de van der Schueren and Schols 39 ). Residents were qualified as malnourished if they met one of the following criteria: (1) BMI ≤ 20 kg/m2 (age >65 years); (2) unintentional weight loss (more than 6 kg in the previous 6 months or more than 3 kg in the last month); (3) no nutritional intake for 3 d or reduced intake for more than 10 d combined with a BMI ranging between 20 and 23·9 kg/m2 (age >65 years).
Care dependency was measured with the Care Dependency Scale( Reference Dijkstra 40 , Reference Lohrmann 41 ). This scale consists of fifteen items, with a five-point Likert scale, and is validated for different settings in several countries( Reference Dijkstra, Buist and Moorer 42 – Reference Dijkstra, Tiesinga and Plantinga 45 ).
Since the original questionnaire and instruction material were in Dutch, these were translated by a professional translator into German. This translation was discussed by the Dutch project group (who spoke also German) with the project group in Germany and Austria until consensus was reached about the translation. The questionnaire was adapted to cultural differences. For instance, the nomenclatures for departments and professions that are present in German and Austrian nursing homes were adjusted to the local situation.
Sample
All Dutch, German and Austrian nursing homes were invited by (e)mail (including a flyer) and through publications in several professional journals to take part voluntarily in the LPZ measurement.
All residents of the participating nursing homes were invited to participate and included if they (or their legal representatives) gave informed consent. To get a more homogeneous sample, residents were included if they were at least 65 years old. Only those residents who were present at the day of the measurement and who were able to participate in the study were included. Residents were excluded when refusing to participate, not being available at the ward, being comatose or too ill and being terminal. In addition, data from 2009 of residents who participated both in 2009 and 2010 were excluded.
The present study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects/patients were approved by different ethical committees in the different countries. In addition, the LPZ team received ethical approval from the medical ethical committee of the Maastricht University Medical Centre in The Netherlands (oral informed consent). The ethical committee related to the Institute of Nursing Science at Witten/Herdecke University gave its approval for the measurement in Germany and the medical ethical committee of the Medical University Graz approved to carry out the study in Austria (Germany and Austria: written informed consent).
Data collection
The participating nursing homes chose a coordinator who was responsible for the measurement within the institution. The coordinators were trained collectively by each national LPZ project group on how to organise data collection, and how to use the questionnaire and the specially designed Internet data-entry program. Subsequently, all the coordinators trained the health care professionals who would perform the data collection. For this purpose, the coordinators received a protocol and training package from the Dutch project group to support them in training the health care professionals.
The assessment of the residents took place always by pairs of health care professionals (nurses, dietitians or doctors), one working on the resident's ward and one independent observer from another ward to enhance reliability.
Data analyses
Statistical analyses were performed using SPSS version 19 (SPSS, Inc.). χ2 tests, Student's t test or ANOVA (with post hoc analyses using the Bonferroni method) and OR were used to describe the differences in (malnourished) resident characteristics between The Netherlands, Germany and Austria. Resident characteristics involved variables such as age, sex, length of stay, type and number of diseases and care dependency. Univariate logistic regression analyses were performed to describe the relationship of each baseline independent variable with the prevalence of malnutrition. Independent variables were country (0 = The Netherlands, 1 = Germany and 2 = Austria) and resident characteristics such as age, sex, length of stay, type and number of diseases and care dependency. For identifying differences in malnutrition prevalence between the countries, P values were based on two-sided tests, and the cut-off point for statistical significance was set at P< 0·05.
A univariate logistic generalised estimating equation (GEE) regression analysis was performed to estimate the OR of countries regarding the prevalence of malnutrition. The dependent variable was malnourished/not malnourished; the independent variables were two dummy variables indicating country (with The Netherlands as the reference category). GEE analysis corrects for the dependency of observations of individuals within institutions by adding a ‘within-subject correlation structure’ to the regression model. An exchangeable correlation structure was used, which means that correlations between individuals within the institutions are assumed to be the same. For building the association model, all variables that were significantly different between the three countries and related to malnutrition (both with P< 0·10) were seen as possible influencing variables (or confounders) in the GEE analyses. For that purpose, in the multivariate logistic regression analysis, all factors that were related to country and malnutrition difference (with P< 0·10) were added to the univariate model step by step so that the mean of both regression coefficients of the dummy variables for country changed. Only the covariates that led to a significant change (more than 10 % of the regression coefficients) were included( Reference Twisk 46 ).
In the final multivariate model (corrected model), the OR of malnutrition in nursing homes in The Netherlands, Germany and Austria were estimated when controlling for the influencing resident characteristics. In this analysis, we focused on the change in the OR of malnutrition between the countries in the uncorrected model (univariate, without controlling for influencing resident characteristics) compared with the corrected model (multivariate, controlling for the observed influencing resident characteristics, see Table 5). Before the multivariate analysis, data were assessed for congruence with regression assumptions.
Results
Response
In the present study, 214 nursing homes with 19 876 residents were included in the analyses: 133 nursing homes from The Netherlands (n 14 123), sixty-one nursing homes from Germany (n 3973) and twenty nursing homes from Austria (n 1780). The response rate was significantly higher in The Netherlands (92·9 %) than in Germany (82·9 %) and Austria (80·8 %). The reasons for not taking part in the measurement were refusing to participate (64·3 %), not being available at the ward (27 %), being comatose or too ill (5·7 %) and being terminal (3·0 %).
Resident characteristics
In Table 1, the characteristics of the included residents are shown separately for The Netherlands, Germany and Austria. Dutch residents were more often male, had a shorter mean length of stay, were less dependent of care and had fewer diseases than residents in Germany and Austria.
Table 1 Resident characteristics, number and kind of disease, care dependency and malnutrition prevalence (Mean values and standard deviations; percentages)

CVA, cerebrovascular accident.
* Values were significantly different between The Netherlands and Germany.
† Values were significantly different between The Netherlands and Austria.
‡ Values were significantly different between Germany and Austria.
The most prevalent diseases in all the three countries were dementia (42·1 % in The Netherlands, 55·2 % in Germany and 60·8 % in Austria), CVD (41·2 % in The Netherlands, 70·0 % in Germany and 59·0 % in Austria) and motor disorders (27·0 % in The Netherlands, 41·9 % in Germany and 41·7 % in Austria).
Malnutrition prevalence
The prevalence of malnutrition also differed significantly between the countries (P< 0·05; Table 2).
Table 2 Prevalence of malnutrition (Number of prevalence of malnutrition and percentages; odds ratios and 95 % confidence intervals)

* Reference group.
In Germany and Austria, the prevalence was somewhat higher than in The Netherlands (20·0 and 22·7 % v. 18·0 %, respectively).
Relationship between resident characteristics and malnutrition
Table 3 shows the prevalence of the different characteristics for the malnourished and not malnourished residents. Malnourished residents had more diseases and were older, more care dependent and more often female than those not malnourished. Furthermore, a significant difference was found between the malnourished and not malnourished residents concerning the type of prevalent diseases such as infectious disease, cancer, diabetes mellitus, blood disease, dementia, diseases of the digestive tract, injury resulting from accidents and total hip replacement. No significant difference was found in the length of stay.
Table 3 Patients with malnutrition (M+)/without malnutrition (M−) and patient characteristics (Odds ratios and 95 % confidence intervals)
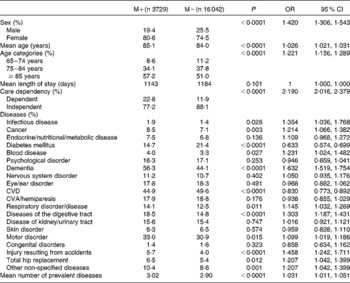
CVA, cerebrovascular accident.
To calculate which resident characteristics influenced the differences found in the prevalence rates of malnutrition between the countries, the factors that showed a significant difference between the countries and between the malnourished and not malnourished residents (P< 0·1) were incorporated in a multivariate GEE analysis.
Possible influencing variables (GEE analyses and association model)
Tables 1 and 3 show that sex, age, age categories, mean number of diseases and care dependency, as well as infectious disease, cancer, diabetes mellitus, blood disease, dementia, CVD, respiratory disease, diseases of the digestive tract, motor disorder, injury resulting from accidents, total hip replacement or other non-specified diseases were possible confounders or influencing variables (P< 0·01). After entering these variables step by step in the univariate model, in the final multivariate model (corrected model; Table 4) the variables care dependency, CVD, diseases of the digestive tract, age, dementia, diabetes mellitus, sex, mean number of diseases, respiratory disease and other non-specified diseases were included as influencing variables for the difference in malnutrition prevalence in the three countries. The two most influencing resident characteristics (confounders) were care dependency and CVD. The confounders resulting from the analyses influence the OR of countries.
Table 4 Generalised estimating equation (GEE) – association model

* B1, comparing Austria with The Netherlands.
† B2, comparing Germany with The Netherlands.
‡ Variables in model: country (The Netherlands as a reference group, Germany and Austria) and malnutrition prevalence.
§ Corrected for variables: care dependency, age, sex, mean number of diseases and specific diseases (CVD, disease of the digestive tract, dementia, diabetes mellitus, respiratory disorder and other non-specified diseases).
After controlling for these variables in the final multivariate model (corrected model), the OR of malnutrition difference between the three countries declined. The OR of malnutrition prevalence declined when comparing the univariate model (without controlling for predictive resident characteristics) with the multivariate model (controlling for influencing resident characteristics) (see Table 4) between the countries (see Table 5). The OR of malnutrition between The Netherlands and Germany declined from 1·137 to 1·065 (P= 0·201). The OR of malnutrition between The Netherlands and Austria declined from 1·335 to 1·085 (P= 0·213). After controlling for the influencing resident characteristics (confounders), there were no differences any more; the OR declined to 1, implying that the differences in the prevalence rates of malnutrition declined.
Table 5 OR of malnutrition in The Netherlands, Germany and Austria, controlling for influencing resident characteristics (Odds ratios and 95 % confidence intervals)
* Reference group.
† Model includes variables: care dependency, age, sex, mean number of diseases and specific diseases (CVD, disease of the digestive tract, dementia, diabetes mellitus, respiratory disorder and other non-specified diseases).
The difference was not significant any more between The Netherlands and Germany and Austria when controlling for these influencing resident characteristics.
Discussion
The present unique large-scale study explored whether resident characteristics influence possible differences in malnutrition prevalence between The Netherlands, Germany and Austria, when using the same measurement methodology and instrument.
The prevalence of malnutrition differed significantly between the countries. The highest prevalence was found in Austria (22·7 %, The Netherlands 18·0 % and Germany 20·0 %). These prevalence findings are within the range of earlier internationally reported malnutrition prevalence rates. Data collected by the Nutrition Day survey showed a malnutrition prevalence of 16·7 % in nursing home residents in Germany( Reference Valentini, Schindler and Schlaffer 6 ). Furthermore, a study by Tannen et al. ( Reference Tannen, Schutz and Nie van 47 ) has shown comparable rates (15·1 %) collected in German nursing homes, and another study has shown the same rates (15·7 %) in Austrian hospitals( Reference Tannen and Lohrmann 48 ). A study in different aged care residents in Australia has shown a much higher prevalence rate. The prevalence of malnutrition across these facilities varied from 31·8 to 72·1 %( Reference Gaskill, Black and Isenring 19 ). In interpreting the differences between these studies, it must be realised that each study uses its own methodology as well as definition and operationalisation of malnutrition.
Resident characteristics that were both related to country and malnutrition were seen as possible influencing variables (or confounders) in the GEE analyses. Being female, being older, having more diseases and having diseases such as CVD, disease of the digestive tract, dementia, diabetes mellitus, respiratory disorder and other non-specified diseases influence the chance of getting malnourished.
The present study revealed that the two largest confounders are being more care dependent and having a CVD. This finding is confirmed in other studies showing that malnourished residents are more care dependent. Other studies confirm the present findings on the relationship between malnutrition and CVD( Reference Colín-Ramírez, Orea-Tajeda and Castillo-Martínez 49 , Reference Teh, Wham and Kerse 50 ). Furthermore, the remaining confounders found in the GEE analyses have also been indicated by other studies. Residents have more often several diseases such as disease of the digestive tract and respiratory disorder( Reference Oliveira, Fogaça and Leandro-Merhi 31 , Reference Suominen, Muurinen and Routasalo 51 ). Other studies have shown that women are more at risk of getting malnourished( Reference Hickson 52 ). Gaskill et al. ( Reference Gaskill, Black and Isenring 19 ) found a relationship between malnutrition and an increased age and high level of care needs. Suominen et al. ( Reference Suominen, Muurinen and Routasalo 51 ) described similar patient-related factors that explain malnutrition in nursing home residents in Finland. Their logistic regression analyses have shown that impaired functioning, swallowing difficulties, dementia and constipation are associated with being malnourished( Reference Suominen, Muurinen and Routasalo 51 ). This is also in line with the present findings. Although the present study shows that resident characteristics influence differences in the prevalence rates of malnutrition between countries, it has never been studied using the same method and definition on a large scale in different countries.
There was no significant difference between The Netherlands, Germany and Austria after controlling for these influencing variables. In addition to resident characteristics, other influencing variables could also play a role in the difference in malnutrition prevalence between countries. Possible influencing variables could be differences in health care structure as nutritional care policies (e.g. nutritional screening policy, implementation of a nutritional care protocol/guideline, the policy of discussing malnourished residents in a multidisciplinary team) and care processes (e.g. preventive and treatment measures used). A study by Meesterberends et al. ( Reference Meesterberends, Halfens and Spreeuwenberg 53 ) has revealed that six factors, including resident-related, nursing-related and structure-related factors, explain the differences in the incidence rates of pressure ulcer between nursing homes in The Netherlands and Germany. Future studies must be performed to assess the specific contribution of these structural and process factors to differences in the prevalence rates of malnutrition in different countries.
Limitations
In the present study, data from three countries were analysed with different sample sizes. While the institutions participated voluntarily, no information was available about the degree of representativeness of the samples. However, to date, no other studies with such a large number of patients have been published.
Since there is no globally accepted ‘gold’ standard for malnutrition, we based the present study on a definition that meets those factors for which consensus exists( Reference Meijers, Van Bokhorst-de van der Schueren and Schols 39 ).
Finally, it might be possible that more and other resident characteristics that were not taken into account in the present study are likely to influence the risk of getting malnourished. Therefore, we assume that structural and process factors of malnutrition could also play a role.
Conclusion
Malnutrition is still a considerable problem; about 20 % of all nursing home residents in the present study were malnourished. There are differences between countries, which can be explained by resident characteristics. Since other country-related factors such as structural and process factors of malnutrition could also play an important role in influencing differences in the prevalence rates of malnutrition between countries, we recommend the investigation of these factors in future studies.
Acknowledgements
We thank Nutricia Advanced Medical Nutrition for providing an unrestricted grant. Nutricia Advanced Medical Nutrition had no role in the design, analysis or writing of this article.
N. v. N., J. M., J. S. and R. H. contributed to the design of the study. N. v. N., J. M., J. S., C. L., S. B. and R. H. helped in the data collection. N. v. N, J. M., M. S. and R. H. conducted the data analyses N. v. N., J. M., J. S., C. L., M. S. and R. H. wrote the manuscript. M. S. provided significant advice and consultation concerning statistical issues. N. v. N, J. M., J. S., C. L., M. S. and R. H. approved the final manuscript.
There are no conflicts of interest to report.







