Impact statement
Given the increasing mental health needs during infectious disease outbreaks, psychological interventions that are culturally acceptable and effective should be given priority for under-resourced countries. This systematic review provides important insights into the benefits of psychological interventions in addressing common mental health issues of outbreak-affected populations in low- and middle-income countries (LMICs). Brief psychoeducational interventions with stress management principles were helpful in addressing common mental health issues, including depression, anxiety, post-traumatic stress symptoms and sleep problems associated with emergencies of infectious disease outbreaks in LMICs. Overall, non-specialist delivered, brief sessions are more likely to be valuable in addressing mental health issues that arise in outbreaks. Filling the existing knowledge gap with quality evidence will contribute to the development of the standardised, evidence-based and contextually relevant intervention guidelines that are applicable to LMICs. Therefore, future efforts should focus on improving access to quality data that can inform evidence-based decisions.
Introduction
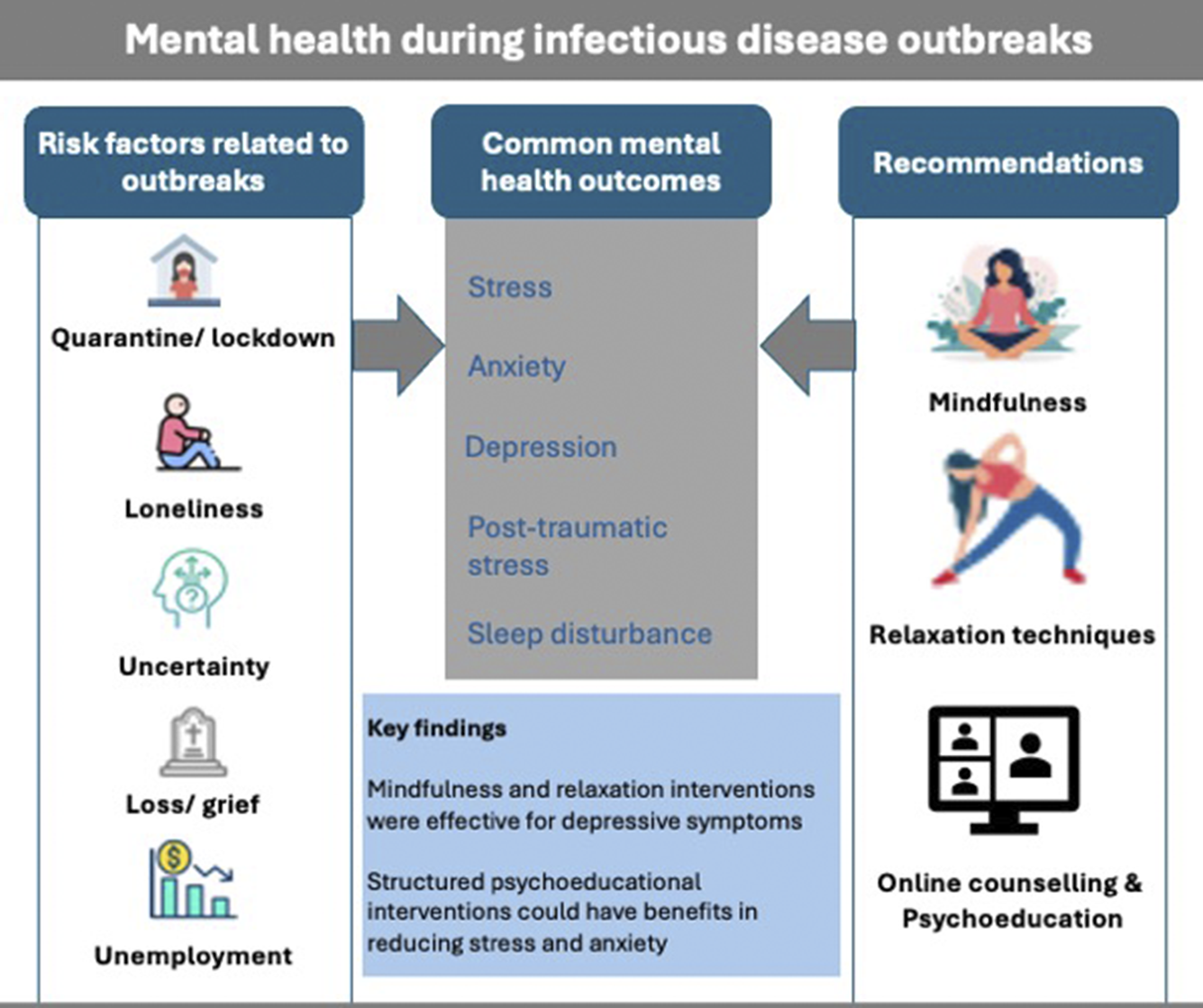
Infectious disease outbreaks have had a devastating impact on lives and livelihoods around the globe (Baker et al., Reference Baker, Mahmud and Miller2021), and are a threat to planetary health and development (Huremović, Reference Huremović2019). The profound impacts of intermittent disease outbreaks include increased mortality, reduced effectiveness of health systems, social inequity and economic crisis (Sampath et al., Reference Sampath, Khedr and Qamar2021). Disease outbreaks pose a significantly increased risk to the mental health of affected individuals and communities, particularly in low- and middle-income countries (LMICs) where health system resilience is low and the treatment gap is high (Jacob, Reference Jacob2017).
Although the impact of infectious disease outbreaks is on a wider population, specific groups of people are particularly vulnerable, including people directly affected by the disease, people with pre-existing health conditions and disabilities and frontline healthcare workers (Singu et al., Reference Singu, Acharya and Challagundla2020). Evidence shows that the prevalence of several mental health problems such as post-traumatic stress disorder (PTSD), depression and anxiety symptoms doubled during infectious disease outbreaks and pandemics (Schindell et al., Reference Schindell, Fredborg and Kowalec2024; Hossain et al., Reference Hossain, Tasnim and Sultana2020; Yuan et al., Reference Yuan, Zheng and Wang2022). For instance, a 76% prevalence of PTSD symptoms and 48% prevalence of anxiety-depression symptoms were recorded during the Ebola epidemic in Siera Leone in 2015 (Jalloh et al., Reference Jalloh, Li and Bunnell2018). Similarly, a 64% prevalence of psychological distress and 40.7% prevalence of PTSD was reported among Severe Acute Respiratory Syndrome (SARS) survivors in Hong Kong in 2004 (Lee et al., Reference Lee, Wong and McAlonan2007). The COVID-19 pandemic had a huge impact on population mental health and contributed to a more than 25% increase in cases of depression and anxiety globally (World Health Organization, 2022).
People with pre-existing mental health conditions were impacted to a greater extent than others (Boden et al., Reference Boden, Cohen and Froelich2021). This may be for two reasons: in addition to being susceptible to the experience of stress common to everyone, mental health services are often disrupted, as occurred worldwide during the COVID-19 pandemic. Access to basic counselling services, medication adherence programmes, social support mechanisms and emergency mental health services also collapsed. The impact was more severe when countries closed schools and workspaces and imposed restrictions in movement and quarantine measures. In addition, mental health services were often de-prioritised, community services were suspended and facilities were changed to quarantine facilities (Yirdaw et al., Reference Yirdaw, Moussallem and Alkasaby2024). With all the added risks to people with mental conditions, maintenance of mental health services was important, as a part of wider response measures. However, the capacity of health systems in LMICs to quickly develop plans and to respond to mental health needs was very limited and the process often is slow (Kola et al., Reference Kola, Kohrt and Hanlon2021). While in some countries, online options using telemedicine or digital technology enabled mental health services to bridge some gaps, LMICs struggled to adapt and maintain mental health service delivery (Arenliu et al., Reference Arenliu, Uka and Weine2020). For instance, during the COVID-19 pandemic in China, several key challenges were noted (Duan and Zhu, Reference Duan and Zhu2020): (i) little attention was given to the practical implementation of psychological interventions, (ii) little effort was made to align interventions into community healthcare services, (iii) there was a shortage of professionals and resources and (iv) there were restrictions to entry to isolation centres to receive appropriate care. During the COVID-19 pandemic in Africa, mental health interventions were not often included in planning, due to the lack of political commitment, low prioritisation of mental health during emergencies compared with other response activities and the scarcity of financial and human resources allocated to mental health activities (Yirdaw et al., Reference Yirdaw, Moussallem and Alkasaby2024; Walker et al., Reference Walker, Alkasaby and Baingana2022).
Implementing the established good practice of enabling frontline workers to deliver basic psychological interventions as part of other response activities was also challenging due to complicated work procedures, heavy workloads and the lack of standardised training resources (Duan and Zhu, Reference Duan and Zhu2020). Given the significant mental health impact of outbreaks and associated public health counter-measures, the application of evidence-based interventions with alternative treatment and support solutions should be part of outbreak response plans.
While acknowledging the contribution of previous studies (Pollock et al., Reference Pollock, Campbell and Cheyne2020; Zace et al., Reference Zace, Hoxhaj and Orfino2021; Yang et al., Reference Yang, Sun and Hu2021), there is a huge paucity of quality evidence to inform effective psychosocial interventions to address mental health issues during infectious disease outbreaks. The most recent systematic review (in 2021) of all intervention types with different study designs found a huge evidence gap where no randomised controlled trials (RCT) were carried out in LMICs (Zace et al., Reference Zace, Hoxhaj and Orfino2021). The lack of evidence is partially due to difficulties in implementing research in outbreak contexts, challenges in the measurement of treatment outcomes and lack of quality data on a longer impact of trials. Our systematic review explores the literature to update the existing evidence gap with a body of evidence to inform effective psychological interventions to address mental health issues during infectious disease outbreaks in LMICs.
Methods
We searched for RCTs evaluating the effectiveness of psychosocial interventions in infectious disease outbreaks in LMICs. This systematic review is reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Inclusion and exclusion criteria
Psychosocial interventions are defined as strategies, activities, techniques and toolkits that address psychological and social problems and promote mental wellbeing. We used a broad definition of therapeutic practices, including but not limited to cognitive behavioural therapy, supportive therapy, interpersonal psychotherapy, counselling and mindfulness. Psychological interventions could be delivered through various means such as face-to-face modalities (whether group or one-to-one), or through the use of technology like telemedicine/teletherapy, or software-based interventions such as mobile applications.
The general inclusion criteria for this systematic review were: (i) trials with any type of psychological interventions, (ii) conducted in LMICs, (iii) studies must be RCTs, (iv) conducted among adults with age ≥18 years and (iv) carried out to address mental health conditions in infectious disease outbreaks.
Studies were excluded if they were: (i) included all age groups and not reporting on adults separately, (ii) focused on non-outbreak settings, (iii) used mixed interventions including pharmacological therapies concurrently, with no separate analysis of psychological interventions only, (iv) addressed only severe mental health conditions including psychosis and (v) published in other languages than English.
Literature search strategies
We searched six databases (Scopus, PubMed, PsycINFO, Embase, Cochrane library and CINAHL) and other sources including the manual search of Google Scholar. There were no restrictions on publication date, study type and design in the initial search. Databases were searched in 15 to 25 October 2023 without language restrictions. The keywords used for searching were psychological interventions, mental conditions, infectious disease outbreaks and the list of LMICS. Similar concepts, synonyms and medical subject headings (MeSH) were used for each keyword. Appropriate syntax was developed and used for each database. The search strategies used for the search are available in Supplementary Appendix 1.
Study selection
Studies identified from the search were screened by topic and exported to EndNote 20 software. Duplicates were removed from the EndNote and the remaining articles were then moved to Rayyan software for further duplicate identification and abstract screening. Studies that fulfilled most of the inclusion criteria were identified from the abstract screening. Full-text articles were searched by BAY and JAS. BAY and JAS double-checked the screened articles, resolved disagreements and assessed the full-text articles against the inclusion criteria independently.
Data extraction and management
Data extraction was done by BAY and JAS using the Cochrane Collaboration data collection form for RCTs. The extracted data includes publication year, study setting, population, country, sample size, type of intervention, number of sessions, session duration, method of delivery, outcomes, outcome measures, key findings and limitations.
Risk of bias assessment
Two of the authors (BAY and JAS) evaluated each study using the Cochrane Collaboration risk of bias tool (Higgins et al., Reference Higgins, Altman and Gotzsche2011). The tool formalises the judgment of specific features of a randomized control trial to assist review authors in identifying possible limitations and considerations for the assessing strength of the results of an article. This tool has five key domains for assessment: selection bias, reporting bias, performance bias, detection bias and attrition bias. Each study in the risk of bias assessment was judged under each category of bias as either low risk for bias, high risk for bias or unclear. Unclear suggests a lack of sufficient information or persistent uncertainty over the potential for bias under this category.
Data synthesis
The extracted and collated data were summarised in tables, with data captured including study design, participants, settings, sample size, intervention type, duration of each intervention and outcome measures. A narrative synthesis was done to analyse the differences, patterns and similarities of interventions. No meta-analysis was conducted due to the high heterogeneity of the trials in several aspects such as differences in the quality of the data, outcome measure, intervention type, session duration and delivering agents.
Results
Characteristics of the included studies
Of 10,890 screened articles, 2,809 duplicates were removed. After removal of duplicates, 5,955 articles were excluded because they did not fulfil at least one of the inclusion criteria – not outcome of interest, population of interest, intervention of interest or not a systematic review. The full text of 166 articles was reviewed to check whether they fulfilled all the inclusion criteria. In the first round of full-text review, we excluded 104 articles because they were not mental health related (76 articles), not the right population (16 articles), not an intervention (two articles) and not in English (eight articles). Finally, we selected 17 articles that fulfilled all the inclusion criteria (Figure 1).

Figure 1. PRISMA flow diagram of search results.
All the included trials were conducted in five countries during the COVID-19 pandemic from 2020 to 2023: these were seven from China (Fan et al., Reference Fan, Shi and Zhang2021; Li et al., Reference Li, Chen and Ye2023; Li et al., Reference Li, Li and Jiang2020; Liu et al., Reference Liu, Qiao and Xu2021; Sun et al., Reference Sun, Lin and Goldberg2022), six from Iran (Ghazanfarpour et al., Reference Ghazanfarpour, Ashrafinia and Zolala2022; Khosravi et al., Reference Khosravi, Aghababaei and Kazemi2022; Mirhosseini et al., Reference Mirhosseini, Heshmati and Behnam2022; Shabahang et al., Reference Shabahang, Aruguete and McCutcheon2021; Shaygan et al., Reference Shaygan, Yazdani and Valibeygi2021; Shaygan et al., Reference Shaygan, Yazdani and Rambod2023), two from Turkey (Dincer and Inangil, Reference Dincer and Inangil2021; Hosseinzadeh, Reference Hosseinzadeh2022), one from India (Gupta et al., Reference Gupta, Kumar and Rozatkar2021) and one from Jordan (Alkhawaldeh, Reference Alkhawaldeh2023). As shown in Table 1, half of these trials (n = 8) were conducted among COVID-19 patients and six trials (n = 6) were among frontline healthcare workers involved COVID-19 response. The remaining studies focused on college students (n = 2) and pregnant women (n = 1). In terms of setting, 13 trials were conducted in hospital-based settings, four (n = 4) were in community-based health centres and one (n = 1) quarantine facility. The total number of study participants included in all trials was 1,687 and the sample size in each study ranged from 35 to 118. Table 1 provides an overview of the characteristics of the included studies.
Table 1. Characteristics of the included studies in this systematic review (N=17)

Outcome measures
Of the 17 included trials, 14 of them targeted anxiety symptoms only and 10 of them assessed both anxiety and depression as a primary outcome (Table 2). Stress, post-traumatic stress symptoms, psychological distress, resilience, burnout, sleep quality and self-efficacy were primary outcomes in one or more trials. The tools used to measure these outcomes vary significantly in type, item, validation and cut-off point. Four trials used combined tools to assess depression, anxiety and stress altogether; these were: the Depression, Anxiety and Stress Scale (DASS-21) (Gupta et al., Reference Gupta, Kumar and Rozatkar2021; Hosseinzadeh, Reference Hosseinzadeh2022; Li et al., Reference Li, Li and Jiang2020) and the Hospital Anxiety and Depression Scale (HADS) (Ghazanfarpour et al., Reference Ghazanfarpour, Ashrafinia and Zolala2022). Another five trials evaluated depression independently using the Patient Health Questionnaire (PHQ-9), (Zhou et al., Reference Zhou, Kong and Wan2022; Sun et al., Reference Sun, Lin and Goldberg2022) the Hamilton Depression Rating Scale (HAMD), (Liu et al., Reference Liu, Qiao and Xu2021) and the Self-rating Depression Scale (SDS) (Li et al., Reference Li, Chen and Ye2023; Fan et al., Reference Fan, Shi and Zhang2021). Several tools were used to assess anxiety independently including the State Anxiety Scale (Dincer and Inangil, Reference Dincer and Inangil2021) Self-rating Anxiety Scale (Fan et al., Reference Fan, Shi and Zhang2021; Li et al., Reference Li, Chen and Ye2023), Hamilton Anxiety Rating Scale (Liu et al., Reference Liu, Qiao and Xu2021), COVID-19 Anxiety Questionnaire (Shabahang et al., Reference Shabahang, Aruguete and McCutcheon2021), Short Anxiety Inventory (Shabahang et al., Reference Shabahang, Aruguete and McCutcheon2021), State Trait Anxiety Inventory (Shaygan et al., Reference Shaygan, Yazdani and Rambod2023) and the Generalised Anxiety Disorder Questionnaire (Sun et al., Reference Sun, Lin and Goldberg2022; Zhou et al., Reference Zhou, Kong and Wan2022). The lack of consistency in the use of outcome measures and a lack of clarity on the degree of cultural validation of the tools across studies was observed.
Table 2. Interventions, key findings and important limitations (N=17)

Key: N*, number of participants completed the study.
Intervention characteristics and effectiveness
Of 17 included trials, seven (n = 7) of them used CBT principles (Sun et al., Reference Sun, Lin and Goldberg2022; Hosseinzadeh, Reference Hosseinzadeh2022; Li et al., Reference Li, Chen and Ye2023; Ghazanfarpour et al., Reference Ghazanfarpour, Ashrafinia and Zolala2022; Shabahang et al., Reference Shabahang, Aruguete and McCutcheon2021; Liu et al., Reference Liu, Qiao and Xu2021), of which two (n = 2) of them combined mindfulness with CBT (Ghazanfarpour et al., Reference Ghazanfarpour, Ashrafinia and Zolala2022; Hosseinzadeh, Reference Hosseinzadeh2022). Five (n = 5) of the included trials used psychoeducational interventions based on training, cognitive restructuring, stress management, positive therapy and relaxation techniques (Shaygan et al., Reference Shaygan, Yazdani and Valibeygi2021; Shaygan et al., Reference Shaygan, Yazdani and Rambod2023; Mirhosseini et al., Reference Mirhosseini, Heshmati and Behnam2022; Liu et al., Reference Liu, Yang and Liu2022; Alkhawaldeh, Reference Alkhawaldeh2023). Two more trials used mindfulness techniques alone involving practical stress reduction exercises (Sun et al., Reference Sun, Lin and Goldberg2022; Li et al., Reference Li, Chen and Ye2023). The remaining trials used Narrative Exposure Therapy (NET) (Fan et al., Reference Fan, Shi and Zhang2021), Emotional Freedom Techniques (Dincer and Inangil, Reference Dincer and Inangil2021), Brief Eclectic Psychotherapy (Gupta et al., Reference Gupta, Kumar and Rozatkar2021) and individual counselling (Khosravi et al., Reference Khosravi, Aghababaei and Kazemi2022).
Of the 17 included trials, 13 of them delivered interventions remotely, two were delivered face-to-face (Alkhawaldeh, Reference Alkhawaldeh2023; Li et al., Reference Li, Li and Jiang2020) and other two used a hybrid approach (remotely and face-to-face) (Fan et al., Reference Fan, Shi and Zhang2021; Khosravi et al., Reference Khosravi, Aghababaei and Kazemi2022). Different digital tools were used to deliver interventions remotely such as mobile apps, websites, telephone calls and messaging platforms like WeChat, zoom and WhatsApp. Most of these used live video calls as a means of delivering established intervention models. The interventions varied by the number and duration of sessions. Overall, the number of sessions ranged from a single to 14 sessions, lasting for 15 minutes up to 2 hours per session. The delivering agents were trained healthcare workers including psychiatrists, nurses, psychologists and mental health experts.
The most structured and intensive intervention was NET which involved up to two sessions per week with a session duration of 90–120 minutes and lasted for eight weeks. Sessions were delivered using a hybrid approach remotely (via the internet online, mobile phones, WeChat) and face-to-face in a one-to-one model in clinics (Fan et al., Reference Fan, Shi and Zhang2021). Study participants were followed up for 6 months after the intervention. The NET intervention was used to treat post-traumatic stress, depression and anxiety symptoms of COVID-19 patients admitted to hospitals. The intervention included three phases: (i) diagnostic interviews and psychoeducation, (ii) constructing a lifeline with a life events timeline and (iii) narrative of the exposure.
The effectiveness of these trials varied from non-significant change to high effect sizes in reducing depression, anxiety, stress, sleep problems and post-traumatic symptoms. The majority of the trials showed a significant reduction in depression, anxiety, stress and insomnia scores between baseline and post-treatment assessments. Brief psychoeducational interventions based on cognitive restructuring, mindfulness, relaxation and stress management techniques were effective in reducing perceived stress and anxiety symptoms, and to improve resilience and self-efficacy (Shaygan et al., Reference Shaygan, Yazdani and Rambod2023; Shaygan et al., Reference Shaygan, Yazdani and Valibeygi2021; Mirhosseini et al., Reference Mirhosseini, Heshmati and Behnam2022; Alkhawaldeh, Reference Alkhawaldeh2023). Also, brief mindfulness-based interventions (Sun et al., Reference Sun, Lin and Goldberg2022) and mindfulness-based stress reduction (Li et al., Reference Li, Chen and Ye2023) treatments were effective in addressing depression, anxiety and generalised anxiety disorder. Remotely delivered CBT and mindfulness-based CBT interventions showed promising but non-significant changes in reducing depression, anxiety, sleep and stress (Hossain et al., Reference Hossain, Tasnim and Sultana2020; Ghazanfarpour et al., Reference Ghazanfarpour, Ashrafinia and Zolala2022; Li et al., Reference Li, Li and Jiang2020; Liu et al., Reference Liu, Qiao and Xu2021; Gupta et al., Reference Gupta, Kumar and Rozatkar2021). Although NET had a statistically significant change in reducing post-traumatic stress symptoms, there was non-significant change in sleep quality, depression and anxiety scores (Fan et al., Reference Fan, Shi and Zhang2021). Similarly, brief Eclectic Psychotherapy (Gupta et al., Reference Gupta, Kumar and Rozatkar2021) and Individual Counselling (Khosravi et al., Reference Khosravi, Aghababaei and Kazemi2022) were non-effective in bringing significant changes in anxiety depression and perceived stress (Table 2).
Anxiety Sensitivity Index (ASI); BMSF (burnout measure short-from); CD-RISC (Connor-Davidson Resilience Scale); CVAQ (COVID-19 Anxiety Questionnaire); DASS (Depression, Anxiety, Stress Scale); DASSD (DASS-depression); DASSA (DASS-anxiety); DASSS (DASS-stress); HADS (Hospital Anxiety and Depression Scale); GAD (Generalized Anxiety Disorder); HADSA (HADS-anxiety); HADSD (HADS-depression); HAMA (Hamilton Anxiety Rating Scale); HAMD (Hamilton Depression Rating Scale); PREPS (Pandemic-Related Pregnancy Stress Scale); PCL-C (PTSD Checklist Civilian version); PHQ (Patient Health Questionnaire); PSS (Perceived Stress Scale); PSQI (Pittsburgh Sleep Quality Index); PTSS (Post-Traumatic Stress Symptoms); SAS (State Anxiety Scale); SDS (Self-rating Depression Scale); SHAI (Short Health Anxiety Inventory); STAI (State-Trait Anxiety Inventory); SRAS (Self Rating Anxiety Scale); SMD (Standard Mean Difference); SUD (Subjective Unit of Distress); SUPPH (Strategy Used by People to Promote Health).
Quality of the included studies
Of 17 included trials, 14 (82.3%) had at least one unclear domain with respect to the Cochrane Collaboration risk of bias checklist and 10 (n=10, 58.8%) had at least one domain with high risk of bias (Figure 2). Only one trial had a low risk of bias in all Cochrane risk of bias assessment items (Sun et al., Reference Sun, Lin and Goldberg2022). In most trials, blinding of study participants and outcome assessors was not carried out. Similarly, several trials had a recruitment bias due to not employing proper randomisation (Figure 2).

Figure 2. Risk of bias assessment for included trials using the Cochrane Collaboration’s Risk of Bias tool (N=17).
Discussion
This systematic review explored several electronic databases to identify and summarise RCTs that were conducted in LMICs, and to synthesise evidence on the effectiveness of psychological interventions in addressing mental health issues during infectious disease outbreaks. After a robust systematic search and careful screening, we found 17 RCTs eligible for this systematic review. These trials were all conducted during the COVID-19 pandemic from 2020 to 2023, showing the huge research gap before the COVID-19 pandemic in LMICs, despite many examples of devastating outbreaks. This systematic review found no included trials conducted in Africa or Latin America, again despite there being many examples here. Notably, most of the included trials were delivered remotely, despite there being very little robust evidence of this means of delivering treatments at the time. The trials were of interventions to address depression, anxiety, stress, sleep and post-traumatic stress symptoms among COVID-19 patients, frontline healthcare professionals involved in COVID-19 response, and college students in quarantine. A range of interventions were used including CBT, psychoeducational interventions, mindfulness techniques, NET and individual counselling with varying number of sessions and duration.
The systematic review found that brief psychoeducational interventions based on cognitive, relaxation and stress management techniques were effective for management of perceived stress and anxiety symptoms as well as in improving resilience, coping strategies and self-efficacy (Shaygan et al., Reference Shaygan, Yazdani and Rambod2023; Shaygan et al., Reference Shaygan, Yazdani and Valibeygi2021; Mirhosseini et al., Reference Mirhosseini, Heshmati and Behnam2022). These findings align with a report from a single-blind RCT in a high-income country (Morina et al., Reference Morina, Weilenmann and Dawson2023) in which a brief psychoeducational intervention was successful in reducing psychological distress, generalised worry and burnout among healthcare workers during the COVID-19 pandemic in Zurich, Switzerland. This trial recommended booster sessions to maintain the initial gains beyond six months. Brief psychoeducational interventions are non-intensive, flexible and can be delivered by non-specialists in any context including in outbreaks/pandemics.
Moreover, brief mindfulness-based intervention (Sun et al., Reference Sun, Lin and Goldberg2022) and mindfulness-based stress reduction interventions (Li et al., Reference Li, Chen and Ye2023) were effective in addressing depression, anxiety and generalised anxiety disorder. Similar findings have been reported from a systematic review and meta-analysis of 26 RCTs that mindfulness-based interventions reduced depressive symptoms significantly among adults affected by COVID-19 pandemic (Fu et al., Reference Fu, Song and Li2024).
Remotely delivered CBT and mindfulness-based CBT interventions showed promising but non-significant changes in reducing depression, anxiety, sleep and stress (Hossain et al., Reference Hossain, Tasnim and Sultana2020; Ghazanfarpour et al., Reference Ghazanfarpour, Ashrafinia and Zolala2022; Li et al., Reference Li, Li and Jiang2020; Liu et al., Reference Liu, Qiao and Xu2021; Gupta et al., Reference Gupta, Kumar and Rozatkar2021). Although CBT has superior benefits and is a first-line treatment for a variety of mental health conditions (Surmai and Duff, Reference Surmai and Duff2022), it may be more effective when it is provided intensively for longer sessions (over 12 sessions) over longer period of time (Levy et al., Reference Levy, Worden and Davies2020). Evidence shows that people who are taking CBT have shown a more gradual curse of change (Driessen and Hollon, Reference Driessen and Hollon2010), and the minimum number of sessions needed to address common mental health problems is between 7 and 14 sessions (Robinson et al., Reference Robinson, Kellett and Delgadill2020). Additionally, the use of active treatments (e.g., in standard interventions) for controls could also result in non-significant changes for CBT (Cuijpers, Reference Cuijpers2024).
Although, NET was superior in reducing post-traumatic stress symptoms to the control group, there was non-significant change in improving sleep quality, reducing depressive and anxiety symptoms (Fan et al., Reference Fan, Shi and Zhang2021). NET is one of the recommended therapies for the prevention and treatment of post-traumatic stress disorder (Megnin-Viggars et al., Reference Megnin-Viggars, Mavranezouli and Greenberg2019), and the results of our systematic review showed that NET is effective in reducing post-traumatic stress symptoms among COVID-19 patients. Even so, the therapeutic components of NET are designed to resolve traumatic symptoms, its broader efficacy beyond PTSD requires further investigation.
Due to their simplicity and adaptability, these interventions have been recommended as appropriate to be delivered in global normative guidelines for some time, but their adaptation for delivery using different approaches including hybrid face-to-face and online, or via phone or video calls was novel and often brought about by necessity rather than being well established in evidence. The use of digital platforms in most included trials to deliver interventions remotely was deemed appropriate in outbreak/pandemic contexts, given contact limitations and scale of demand. This seemed to have proven to be acceptable, as evidenced by the high recruitment and completion rate, where more than 90% of participants completed all sessions in 80% (n=12) of the included trials. Despite the lack of access to digital technologies and low digital literacy in low-income settings, delivering interventions remotely using flexible approaches and multimedia platforms could strengthen the uptake of interventions as well as promote infection prevention and control in outbreaks/pandemics.
The current systematic review has several implications in filling the evidence gap in understanding how to effectively address mental health needs during infectious disease outbreaks. The lack of inclusion of issues related to culture in these studies on evidence-based practice is concerning. This is a topic that is often identified as important, and in fact efforts at adaptation, or even locally developed practice embedded in local cultures, are common, so there is a need for a high-quality research for informed decisions to equip health systems with more treatment options that properly incorporate sensitivity to culture during disease outbreaks. Importantly, it found some evidence for the value of established psychological interventions in what was a unique set of circumstances, requiring innovative approaches to delivery in LMICs. It found that these were often feasible and acceptable, with high adherence, though there may be bias associated with being part of a study. However, there are several limitations that need to be considered when interpreting the results of this systematic review. These are, but not limited to: (i) as the result of lack of consistency, for example in standard case definition and outcome measures, and lack of clarity on the cultural validation of the tools, it may be difficult to generalise effectiveness of results to other populations and contexts; (ii) most of the included trials did not examine sustained effectiveness and therefore longer-term effectiveness of the interventions is unknown; (iii) trials that were written and published in languages other than English were not included in this review and (iv) the overall quality of evidence from these trials is moderately high, although the quality of evidence from each trial varies significantly. Weaknesses of included trials included a lack of proper randomisation, blinding and small sample sizes.
Conclusion
Non-specialist delivered brief psychological interventions is likely to be valuable for addressing the huge mental health needs that arise in outbreaks. Overall, this review demonstrated that brief and remotely delivered psychoeducational interventions seem effective, feasible, cost-effective and time-efficient in the context of the COVID-19 pandemic, which provides valuable insights into their use in future outbreaks. The huge evidence gap in LMICs was marked – none of the included trials were from Africa and Latin America – despite Africa being where outbreaks are most common. Hence, addressing the huge research gap should be a priority to inform evidence-based and resource-efficient psychological interventions for outbreak/pandemic contexts in LMICs. While it was appropriate to innovate rapidly during the exceptional circumstances of the COVID-19 pandemic, future research should examine the use, applicability and scalability of digital interventions in LMICs, to better inform future outbreak preparedness and response. A particular consideration should also be given to the cultural adaptation of psychological interventions and mental health tools, in the context of still centralised production of normative guidance, which draws largely on evidence from high-income countries.
Open peer review
To view the open peer review materials for this article, please visit http://doi.org/10.1017/gmh.2025.22.
Supplementary material
The supplementary material for this article can be found at http://doi.org/10.1017/gmh.2025.22.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Acknowledgements
BAY, JE and MA are paid salaries from the UK Public Health Rapid Support Team (UK-PHRST) and they would like to thank the UK-PHRST for the time and resources devoted to this research. The UK-PHRST is funded by UK Aid from the Department of Health and Social Care and is jointly run by the UK Health Security Agency and the London School of Hygiene & Tropical Medicine. The views expressed in this publication are those of the authors and not necessarily those of the Department of Health and Social Care or other institutions with which the authors are affiliated.
Author contributions
BAY, JE and JAS conceptualised the study. BAY and JAS conducted literature search, article screening and selection. BAY and JAS did quality appraisal of the included studies. JE and MA assisted the data collection and synthesis. BAY drafted the original writing and JE, JAS and MA reviewed and edited it subsequently.
Competing interest
The authors declare that they have no conflict of interest.