Case description
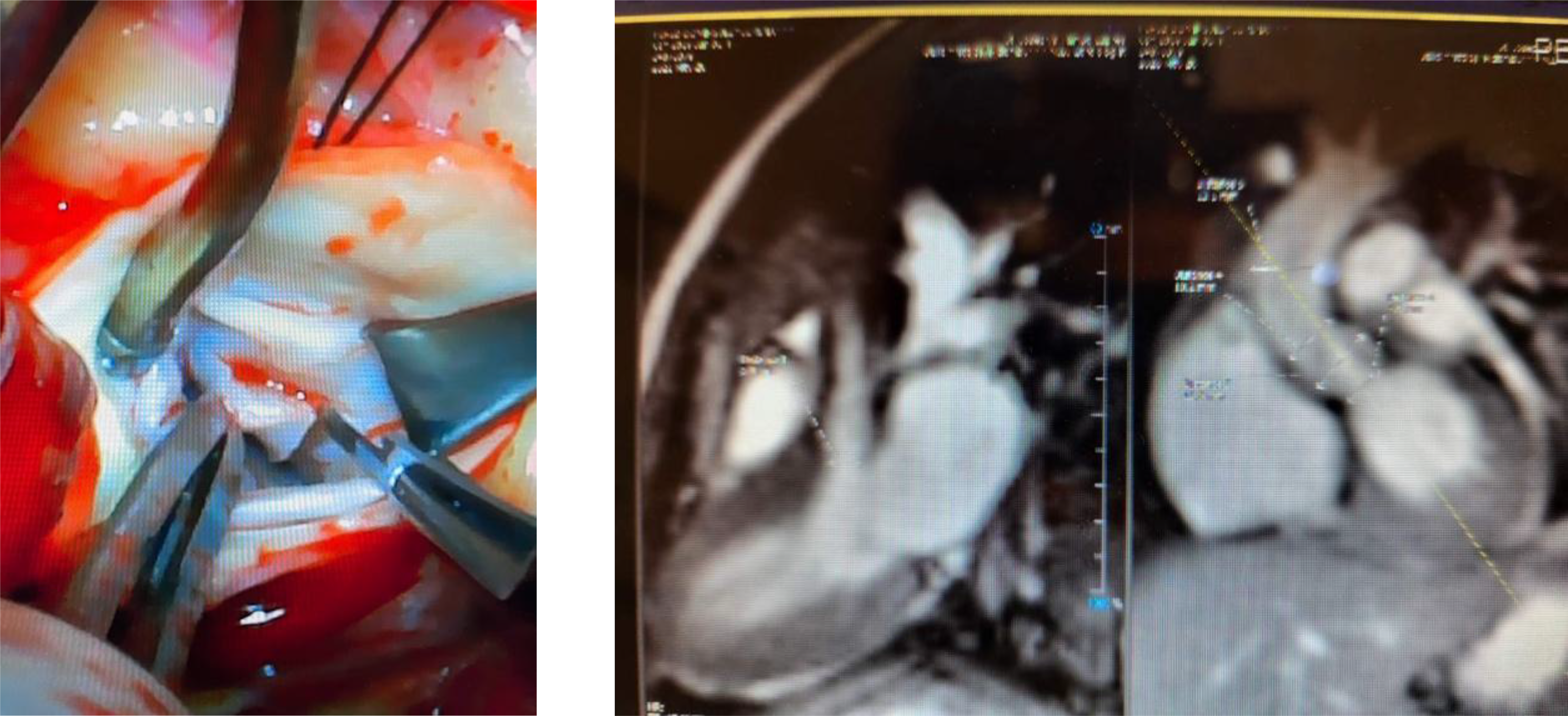
A 6-month-old female was evaluated for a heart murmur in January 2020. Echocardiogram at the initial visit was normal, hence the patient was discharged from further follow-up. She was referred due to persistent murmur at 1 year of age. Repeat echocardiogram showed a subaortic ridge with mild stenosis. Follow-up echocardiogram at 18 months of age showed a distinct oblong echogenic mass measuring 1.5 cm in the left ventricular tract. The tumour was attached to the base of the septum. Mild-to-moderate sub aortic stenosis along with mild aortic insufficiency noted. MRI of the heart showed a cardiac mass along the septal wall in the left ventricular outflow tract measuring approximately 1.7 cm, extending to the aortic valve annulus. This would be most consistent with a fibroma. This cardiac mass resulted in the narrowing of the left ventricular outflow tract to approximately 6 mm, creating outflow tract obstruction. Surgical resection of the tumour was performed in June 2021. During surgery, the tumour tissue was noted to be smooth, glistening, and pliable to nodular and indurated. The resected tumour showed an aggregate of multiple, variegated tissues that measured from 0.6 cm to 0.8 cm. Histopathology confirmed nodular fasciitis. This is shown below.

During follow-up, a small residual tumour was noted by echocardiogram but with no outflow tract obstruction. Dysplastic aortic valve with mild stenosis and mild insufficiency was also seen. Patient is currently active, asymptomatic, and full of energy.
Discussion
Nodular fasciitis has not been described in the heart to date. We would like to report on this rare cardiac tumour. Nodular fasciitis typically occurs in subcutaneous tissue, fascia, within vessels and muscles. It is generally a benign, soft tissue tumour composed of myofibroblasts. Reference Naidu and Lerman1 Nodular fasciitis is the most common of benign fibroblastic proliferative tumours of soft tissue and exceeds in frequency to any other tumour or tumour-like lesion in this group of tumours. The most frequent types are cranial fasciitis and intravascular fasciitis. The former tends to occur in infants. Reference Wagner, Wang, Lloyd, Lam and Khechoyan2 Reports suggest nodular fasciitis in other tissues do not generally recur after surgical resection. The USP6 gene has been linked to tumours in subcutaneous and intravascular tissues. Reference Sápi, Lippai, Papp, Hegyi, Sápi and Dezső3 However, a definitive relationship could not be established between the USP6 gene region rearrangement and the nodular fasciitis in our patient. More research needs to be conducted to find any other genetic relationship with nodular fasciitis in the heart.
We plan to follow the patient on a regular basis. At the last follow-up, in April 2023, the patient was doing well with no evidence of outflow tract obstruction. A dysplastic aortic valve with mild stenosis and insufficiency noted.
Financial support
None.
Competing interests
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.



