Duration of untreated psychosis (DUP) seems to be related to poor outcome (Verdoux & Cognard, 2003). One way to find out if DUP is a marker rather than a cause of poor outcome (Reference McGlashanMcGlashan, 1999) might be to compare early detection programmes with non-early detection (control) programmes in a so-called parallel control design (Reference McGlashan and JohannessenMcGlashan & Johannessen, 1996; Reference McGlashanMcGlashan, 1998). An early detection programme aims to reduce DUP by generating information about early signs of psychosis and the importance of early treatment. However, as early detection programmes also imply intensive detection (Reference Padmavathi, Rajkumar and SrinivasanPadmavathi et al, 1998; Reference McGorry, Edwards and HarrisonMcGorry et al, 1999), it has been suggested that the advantages of early detection might be over-shadowed by recruitment of many patients with a long DUP (Reference McGorryMcGorry, 2000). Indeed, in a recent quasi-experimental study, Krstev et al (Reference Krstev, Carbone and Harrigan2004) found that an early detection programme was associated with lower DUP for most recruited patients, but it also accumulated an over-representation of patients with a ‘very long duration of untreated psychosis’ (DUP 43 years). This paper therefore focuses on the following research questions. Does an early detection programme recruit more or fewer patients with a long DUP than control programmes?
Are the patients with a very long DUP in an early detection programme different from the patients with a long DUP in a non-early detection programme regarding gender, age, symptoms and premorbid function?
METHOD
This study is part of the Scandinavian TIPS study (Early Treatment and Intervention in Psychosis), a multisite investigation of the relationship between DUP and outcome in consecutively admitted patients with first-episode schizophrenia-spectrum disorders. From 1 January 1997, the specialist psychiatric services in four healthcare sectors established equivalent treatment programmes for patients with first-episode psychosis. In two of the healthcare sectors (comprising all of Rogaland County, Norway; population 370 000), an extensive early detection programme was added. The programme consisted of educational campaigns and specialised early detection teams, with the intention of bringing patients with first-episode psychosis even earlier into the specialised treatment system and thus decrease the DUP. The programme is elaborated elsewhere (Reference Johannessen, McGlashan and LarsenJohannessen et al, 2001). The two other participating healthcare sectors (Ullevål sector, Oslo County, Norway and mid-sector, Roskilde County, Denmark: collective population 285 000) established the same treatment programmes, but did not implement an early detection programme. These sectors were the basis of the parallel control sample. Both the Regional Committee for Medical Research Ethics and the Data Inspectorate approved the study.
Patients
All possible patients with first-episode psychosis from these sectors admitted to in-patient or out-patient treatment were assessed without delay at first contact. Patients were eligible for participation in the study if they met the following inclusion criteria: living in the catchment area of one of the four healthcare areas, age between 18 (15 in Rogaland County) and 65, meeting the DSM–IV (American Psychiatric Association, 1994) criteria of schizophrenia, schizophreniform disorder, schizoaffective disorder (narrow schizophrenia-spectrum disorder), brief psychotic episode, delusional disorder, affective psychosis with mood incongruent delusions, psychotic disorder not otherwise specified (non-narrow schizophrenia-spectrum disorders), actively psychotic, not previously adequately treated for psychosis, no neurological or endocrine disorders with relationship to the psychosis, no contraindications to antipsychotic medication, understands/speaks one of the Scandinavian languages, IQ over 70 and willing and able to give informed consent.
During 1997–2000 a total of 423 patients with first-episode psychosis met the diagnostic criteria, of these, 26 were not asked to enter the study due to either severe language problems (16), inability to give consent (three) or other reasons (seven). The remaining 397 were considered study-appropriate and before they were asked to sign an informed consent form were given detailed verbal and written information about the study's assessment and treatment procedures, including their right to withdraw at any time. A total of 93 patients refused to participate (Reference Friis, Melle and LarsenFriis et al, 2004) and three more withdrew their consent and demanded that their data were erased. The remaining 301 patients formed the study sample. This paper is based on these patients (age ≥ 18 years: non-early detection group=14; early detection group = 14).
Data sources and analysis
Diagnosis was identified using the Structured Clinical Interview for the DSM–IV Axis I Disorders (SCID–I; Reference First, Spitzer and GibbonFirst et al, 1995). The DUP was measured as the time from the first onset of positive psychotic symptoms; the first week with the Positive and Negative Symptom Scale (PANSS; Reference Kay, Fiszbein and OplerKay et al, 1987) score of four or more on Positive Scale items one, three, five, six or General Scale item nine to the start of the first adequate treatment of psychosis, i.e. admission to the study. Multiple sources, including interviews with patients and relatives, were used to ascertain the length of this period. Analyses were performed with the Statistical Package for the Social Sciences (version 11.0).
RESULTS
The distribution of patients according to length of DUP is shown in Fig. 1. As shown in Fig. 1 the early detection programme had more patients with DUP <1 year than the non-early detection group. For all groups with longer DUP this was reversed. However, the difference was small-to-moderate for all levels of DUP, and the difference in percentage of patients with a DUP ≥2 years was not significant (χ2 = 1.52; d.f.=1; P = 0.22). The numbers of patients with a long DUP per 100 000 inhabitants per year were: early detection group, 1.11; non-early detection group, 2.02. To test if selective refusal could have biased the results, we recalculated the numbers including the patients who had refused to participate or had withdrawn their consent. This recalculation slightly increased the over-representation of patients with a long DUP in the non-early detection area, but the difference was still non-significant. When we compared patients with a long DUP there were relatively small differences in patient characteristics between the two programmes. Most patients had schizophrenia or schizoaffective disorder (early detection group, 88%; non-early detection group, 87%). The percentage of males was also nearly identical (75 v. 73). However, the age of patients with a long DUP was significantly lower in the early detection area (26 v. 33 years; t=2.49, d.f.=37, P=0.017), a difference which paralleled that in the entire early detection group and non-early detection group (Reference Melle, Larsen and HaahrMelle et al, 2004).
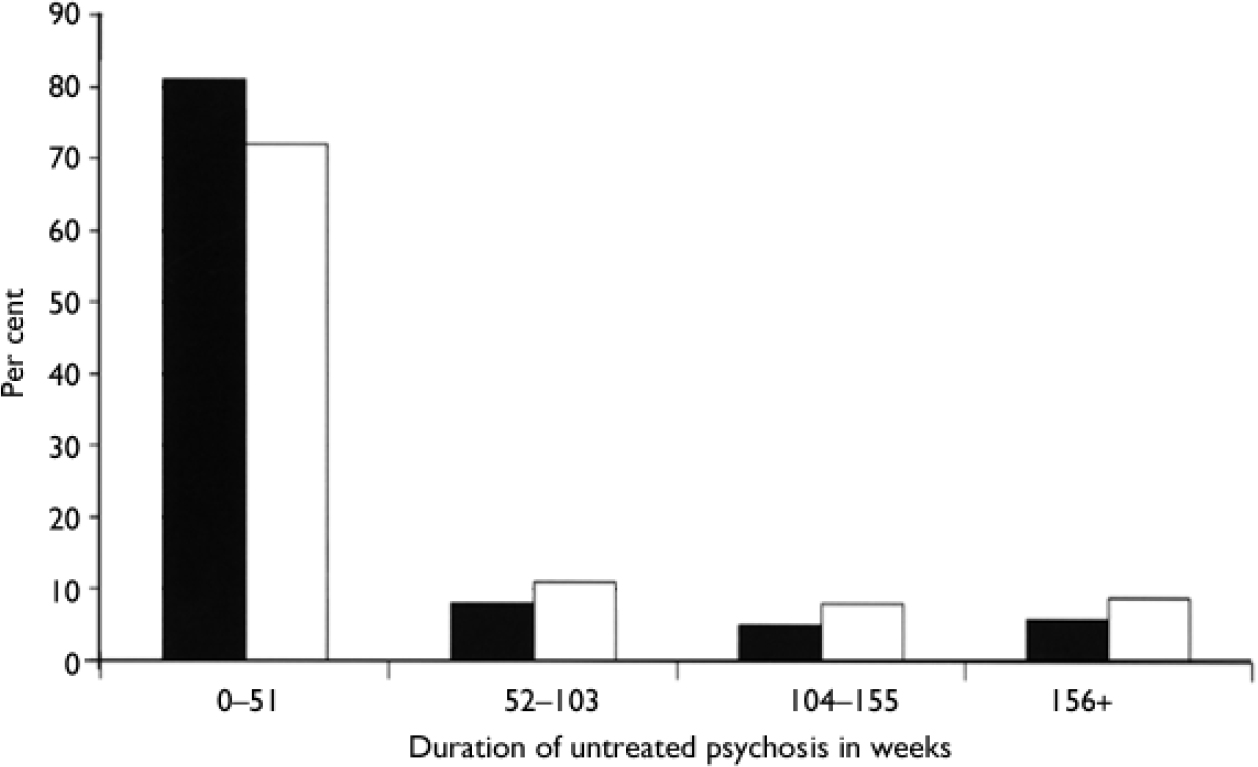
Fig. 1 Distribution of early detection (▪) and non-early detection (□) patients by duration of untreated psychosis.
With regard to premorbid function we investigated differences in childhood level and the course of social and academic functioning as defined by Larsen et al (Reference Lai sen, Friis and Haahr2004). We found no clear differences in childhood level between the groups, either for social or academic functioning. However, we found a clear difference for the course of social functioning. Whereas 69% of early detection patients having a long DUP had a deteriorating social course, only 37% of the patients in the non-early detection group had such a course. This difference was marginally statistically significant (χ2 = 3.89, d.f.=1, P=0.05).
As seen in Fig. 2, there was a clear difference between the groups in PANSS symptoms. The patients in the early detection group had clearly lower levels of positive as well as negative and general symptoms. The difference was statistically significant for all groups (positive: t=3.06, d.f.=36.72, P=0.002; negative: t=3.07, d.f.=36.87, P=0.004; general: t=2.56, d.f.=36,P=0.014).
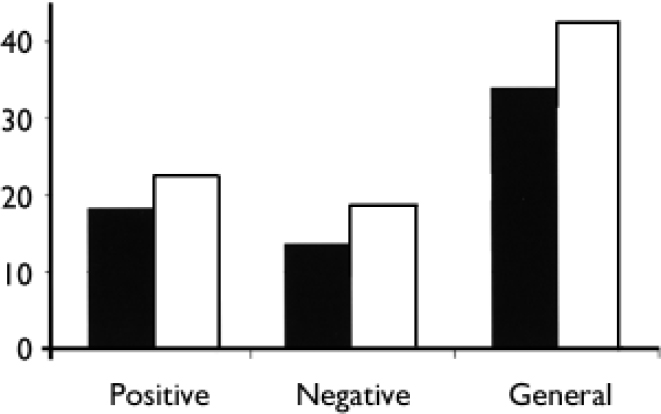
Fig. 2 Positive and Negative Syndrome Scale (PANSS) symptom score for those with a long duration of untreated psychosis in the early detection (▪) and no early detection (□) groups.
DISCUSSION
Number of long DUP patients
We did not replicate the finding of Krstev et al (Reference Krstev, Carbone and Harrigan2004) that an early detection programme recruited more patients with a long DUP. In fact we found that the early detection programme recruited slightly fewer of such patients. This indicates that an early detection programme does not necessarily recruit a large number of previously unrecognised patients with a long DUP. At least this seems to be the case in areas with a fairly well-functioning mental healthcare system. The situation might be different if an early detection programme was suddenly introduced in an area with a poorly developed system. Another source of bias might be the number of patients who refused to participate (Reference Friis, Melle and LarsenFriis et al, 2004). However, the number of patients with a long DUP who did not participate was lower in the early detection area than in the non-early detection area.
Symptom level and premorbid function
We also found that the early detection group of patients had lower symptom levels at admittance than the non-early detection group. This indicates that the programme meets its aim of recruiting patients with a shorter DUP by encouraging them to seek help with a lower symptom level (Reference Larsen, McGlashan and JohannessenLarsen et al, 2001). This also holds true for the patients with a long DUP. The early detection patients with a long DUP have probably had a relatively slow onset of psychotic symptoms as well as few symptoms that raise serious concerns in their social network. However, it is of interest that there was a higher percentage with deteriorating social functioning among the early detection group with a long DUP. This may indicate that the early detection programme has increased the awareness of the importance of social decline, so that patients with long-standing low-level symptoms are brought to treatment more easily.
Definition of long DUP
It might be argued that we ought to have used a different cut-off point than a DUP of 2 years. However, a different cut-off point (for instance, 1 year or 3 years), would have given similar results. We chose the 2-year cut-off, as the psychosis often seems to plateau after 2 years (Reference Birchwood, Todd and JacksonBirchwood et al, 1998).
Limitations and strengths
The results should be interpreted in the context of the following limitations. First, the early detection programme was implemented in an area with a previous study of patients with first-episode psychosis. Although the latter preceded the early detection programme and study, we cannot totally rule out the possibility that this study perhaps lowered the number of patients with a long DUP in the early detection programme. Second, the study was carried out in areas with a very well-developed, publicly funded healthcare system. Consequently, the threshold was low for seeking psychiatric treatment even in the control programme. Third, even if the study recruited a fairly high number of patients, the number of patients with a long DUP is, at best, moderate. Therefore, the possibility of random error has to be considered.
On the other hand, the study has several strengths. First, it comprises consecutively admitted patients from catchment areas. Second, we can document that selective refusal to participate cannot explain the results and, consequently, the generalisability should be high. Third, a comprehensive effort has been implemented to quality-assure data (Reference Friis, Larsen and MelleFriis et al, 2003).
In this context, the study seems to indicate that early detection programmes recruit patients with a lower symptom level than usual programmes. There is no indication that this implies a recruitment of many unidentified patients with a long DUP, at least in areas with a well-developed, publicly funded healthcare system. Therefore, there should be no reason to be concerned that the recruitment of a large number of patients with a long DUP should overshadow the benefits of an early detection programme.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Early detection programmes recruit patients with a lower symptom level than usual programmes.
-
▪ Early detection programmes recruit more patients that have had a premorbid deteriorating course of social functioning.
-
▪ We find no indication that early detection programmes recruit a higher percentage of patients with a long duration of untreated psychosis than usual programmes.
LIMITATIONS
-
▪ The early detection programme was implemented in an area where there had been a previous study of patients with first-episode psychosis.We cannot totally rule out the possibility that this study has perhaps reduced the number of patients with a long duration of untreated psychosis in the early detection programme.
-
▪ The study was carried out in areas with a very well-developed, publicly funded healthcare system. Consequently, the threshold was low for seeking psychiatric treatment even in the control programme.
-
▪ Even if the study recruited a fairly high number of patients, the number of patients with a long duration of untreated psychosis is, at best, moderate. Therefore, the possibility of random error has to be considered.
Acknowledgements
This paper is part of the TIPS project with the following research group: Thomas McGlashan, MD (principal investigator), Per Vaglum, MD (principal investigator), Svein Friis, MD, Ulrik Haahr, MD, Jan Olav Johannessen, MD, Tor K. Larsen, MD, Ingrid Melle, MD, Stein Opjordsmoen, MD, Bjørn Rishovd Rund, PhD, Erik PhD, Erik Simonsen, MD.
From the Department of Psychiatry, Yale University, New Haven, Connecticut, USA, Roskilde County Psychiatric Hospital Fjorden, Roskilde, Denmark; Rogaland Psychiatric Hospital, Haugesund Hospital, Ullevål University Hospital and the Departments of Psychiatry, Psychology and Behavioural Sciences, University of Oslo, Norway. The study was supported by the Norwegian National Research Council (nos 133897/320 and 154642/320), the Norwegian Department of Health and Social Affairs, the National Council for Mental Health/Health and Rehabilitation (nos 1997/41 and 2002/306), Rogaland County and Oslo County (P.V., J.O.J., S.F., T.K.L., I.M. and S.O.). Also funded by the Theodore and Vada Stanley Foundation, the Regional Health Research Foundation for Eastern Region, Denmark; Roskilde County, Denmark, Helsefonden, Lundbeck Pharma, Eli Lilly and Janssen-Cilag Pharmaceuticals (E.S. and U.H.). Also supported by a National Alliance for Research on Schizophrenia and Depression (NARSAD) Distinguished Investigator Award and National Institute of Mental Health grant MH-01654 (T.H.McG.) and a NARSAD Young Investigator Award (T.K.L.).





eLetters
No eLetters have been published for this article.