Age-related muscle and bone loss are closely linked and may share common risk factors including diet( Reference Sirola and Kröger 1 ). Iron may be important for osteoporosis and fracture prevention via its cofactor roles in bone collagen synthesis and vitamin D synthesis( Reference Hutton, Tappel and Udenfriend 2 −3 ). However, to date, no epidemiological studies have explored the potential for iron to reduce long-term fracture risk. The present study aimed to investigate prospective associations between iron intake and serum ferritin with fracture risk in older British men and women.
This case-cohort study was based on a random sub-cohort of 4000 participants and 1502 participants with fractures who were enrolled in the prospective EPIC-Norfolk cohort study of 25,639 men and women aged 39–77 years. An informed consent was obtained from all participants and the study was approved by the Norwich District Health Authority ethics committee. Iron intake from foods was estimated from a 7-day diet diary and serum ferritin concentrations using a fluoroimmunoassay. After excluding those with incomplete data, fracture risk at the hip, spine and wrist was calculated for sex-specific quintiles of iron intake and serum ferritin using Prentice-weighted Cox proportional hazard ratios (HRs). All analyses were adjusted for age, family history of osteoporosis, body mass index, smoking, physical activity, steroid medication, menopausal status and HRT (women only), energy intake, dietary calcium intake, calcium supplements and vitamin D supplements, and were performed using STATA (version 11, STATA Corp, USA).
Fifty eight percent of the study population were women and mean (SD) age was 60 (10) years. Mean iron intake was 13·4 (4·1) and 10·9 (3·4) mg/d for men and women, respectively, and mean serum ferritin was 115·6 (85·2) and 64·7 (52·8) ng/ml, respectively. Iron intake and ferritin correlated significantly in men (r = 0·16; P < 0·05) but not in women (r = −0·02; P > 0·05). After the median follow-up of 12·6 years, adjusted spine fracture risk was significantly lower in women in Q5 of both iron intake (P = 0·008) and serum ferritin (P = 0·018) compared to those in Q1. The association across all quintiles was also significant (iron intake: HR 0·85, 95%CI 0·73–0·99, P-trend = 0·041; ferritin: HR 0·78, 95% CI 0·65–0·94, P-trend = 0·009). No such associations were found at the hip and wrist in women, and at any site in men.
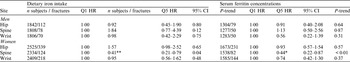
Iron intake in Q1 and Q5 ranged from 3–10 mg/d and 16–42 mg/d in men, and from 2–8 mg/d and 13–30 mg/d in women, respectively. Serum ferritin concentrations in Q1 and Q5 ranged from 9–48 ng/ml and 169–447 ng/ml in men, and from 8–25 ng/ml and 95–443 ng/ml in women, respectively.
Q5 is significantly different from Q1: *P < 0·05; **P < 0·01.
This prospective study found inverse associations between dietary intakes of iron and serum ferritin with spine fracture risk in women only, possibly due to a higher number of fracture events in women. The potential role of iron in bone health should be explored further.


