Digital health technology use in general practice (GP) consultations
The use of technology, including electronic information systems and digital decision support tools, in practice has become ubiquitous. In keeping with patient-centred models of care, technology allows personalization of healthcare and empowers patients to take more control of their health (Young Reference Young2016). Technology has impacted the way a GP consultation is run, it has also impacted the teaching and learning of GP registrars and continuing professional development (Awadallah et al. Reference Awadallah, Czaja, Fainstad, McNulty, Jaiswal, Jones and Rumack2021; Michels et al. Reference Michels, Scherpbier, Karppinen, Buchanan and Windak2020). The implementation of electronic information and communication has also become part of standard consultations, augmenting the traditional in-person, face to face consultation.
Traditional methods of information seeking and communication amongst clinicians include use of hard-copy resources and in-consultation information seeking from another health care professional (Davies & Harrison Reference Davies and Harrison2007). Reasons for not using technology, such as unfamiliarity, excessive time required, and perceived inaccuracy, (Hermes-DeSantis et al. Reference Hermes-DeSantis, Hunter, Welch, Bhavsar, Boulos and Noue2021) are no longer limiting. We now see the increasing use of technology in GP consultations, which has also been shown to help practitioners check information, provide explanations, and provide information for patients outside the consultation by way of signposting further explanation and self-help (Stevenson et al. Reference Stevenson, Hall, Sequin, Atherton, Barnes, Leydon, Pope, Murray and Ziebland2019). Increasing use of technology in practice also allows for the timely acquisition of data and improved analytics, which holds the promise of being able to improve patient care and foster precision medicine (Foadi & Varghese Reference Foadi and Varghese2022; Sharma, Doherty & Dong Reference Sharma, Doherty and Dong2017). Routinely collected electronic health records in GP include diagnostic, therapeutic, prescription, and disease control information (Youens et al. Reference Youens, Moorin, Harrison, Varhol, Robinson, Brooks and Boyd2020). There is potential for use of technology to help identify disease progression, efficacy of management, and signal issues before they are conveyed to the general practitioner (Brown et al. Reference Brown, Smeeth, van Staa and Buchan2017).
Digital decision support tools
Digital decision support tools are designed to improve healthcare delivery by enhancing medical decisions with targeted clinical knowledge, patient information, and other health information (Sutton et al. Reference Sutton, Pincock, Baumgart, Sadowski, Fedorak and Kroeker2020). It is primarily used at the point-of-care to assist clinicians. Examples include digital decision support tools which integrate with electronic health information systems to provide real-time access to clinical guidelines and up-to-date information in the clinical environment (Australian Government Department of Health 2021). Digital decision support tools systems have been proposed as a way to reduce medication errors and adverse events (The Royal Australian College of General Practitioners 2022).
The use of digital decision support tools has transformed ways in which human memory systems operate, replacing semantic memory (the memory of facts) with transactive or external memory (the memory of where facts can be retrieved (Sparrow, Liu & Wegner Reference Sparrow, Liu and Wegner2011). This is an example of ‘cognitive offloading.’ The increasing availability of digital decision support tools renders other options of cognitive offloading, such as hard-copy resources and in-consultation information seeking with another healthcare professional, less attractive by comparison (Firth et al. Reference Firth, Torous, Stubbs, Firth, Steiner, Smith, Alvarez-Jimenez, Gleeson, Vancampfort, Armitage and Sarris2019). There is evidence to suggest increasing clinical experience and expertise, is associated with less reliance on in-consultation information seeking (Magin et al. Reference Magin, Morgan, Wearne, Tapley, Henderson, Oldmeadow, Ball, Scott, Spike, McArthur and van Driel2015; Morgan et al. Reference Morgan, Wearne, Tapley, Henderson, Oldmeadow, Ball, van Driel, Scott, Spike, McArthur and Magin2015).
Additional work in understanding Australian GPs’ use of digital decision support tools will inform resource allocation and strategies to improve use of evidence-based tools to improve practitioner workflow and patient care. In this study, we analysed a large dataset of Australian GPs to: (i) quantify digital decision support tools use; (ii) explore GPs’ sentiments around its use; and (iii) explore the association between digital decision support tools use with practitioner and practice.
Methods
Design, setting and participants
We performed a secondary analysis of an existing data set in the Medicine in Australia: Balancing Employment and Life (MABEL) survey. This was a longitudinal panel survey of medical practitioners in Australia that ran from 2010 to 2018 (Joyce et al. Reference Joyce, Scott, Jeon, Humphreys, Kalb, Witt and Leahy2010). The MABEL survey focused on labour supply, career choices and rural medical workforce distribution. In the MABEL survey, participants were recruited from the Australasian Medical Publishing Company’s Medical Directory which is a national database of Australian doctors used for mailing purposes and updated regularly. The directory includes demographic characteristics that enable validation of the representativeness of the MABEL samples and to adjust for any response bias in sample weightings (Szawlowski et al. Reference Szawlowski, Harrap, Leahy and Scott2019). Data were collected from April 2018 to September 2018, and in this cohort, there were 27,829 Australian medical practitioners (of any type) who responded overall, with 3,126 respondents being general practitioners. Of the 3,126 general practitioner respondents, 2,674 (response rate 85% of all GP responses to the survey) provided a response regarding the use of digital decision support tools in clinical practice.
Australian general practice
General practice is a distinct primary care specialty in Australia. There are close to 32,000 GPs in Australia (Australian Government Department of Health and Aged Care 2024). Qualified general practitioners work as private contractors with a broad scope of practice, managing undifferentiated acute and chronic health problems across the lifespan in an unreferred patient population; providing continuing care for individuals with chronic conditions; undertaking preventive activities; and undertaking a range of population health interventions at the practice and community level (Australian College of Rural & Remote Medicine 2022). GPs in Australia often provide continuing care to patients as part of a community-based team care arrangement with other allied health professionals (The Royal Australian College of General Practitioners 2019). Most GPs are not salaried and operate on a fee-for-service model. Medicare is a universal, government-funded health insurance scheme in Australia. ‘Bulk-billing’ in this context refers to where a general practitioner accepts the Medicare benefit as full payment for a service, with no gap payment payable by the patient. With respect to technology use, 97% of GPs in Australia use a computer for their work, with 70% using electronic clinical documentation (Vandersman et al. Reference Vandersman, Moreira Pinto, Damarell and Tieman2020).
Outcome measures
The initial outcome variable measured was the response to the question, ‘In your last usual week at work, did you use digital health technologies/solutions for the following activities? Using digital decision support tools to help inform clinical decisions.’ In the MABEL questionnaire, ‘digital health technologies’ and ‘digital decision support tools’ are left open for interpretation by respondents. A prompt is provided in the survey, which suggests that ‘clinical dashboards, automated alerts, warnings and reminders, algorithms, and electronic clinical guidelines and pathways’ are forms of digital decision support tools.
‘Yes’ and ‘No but would like to’ responses were re-coded as 1, and ‘No and don’t need to’ responses were re-coded as 0. Representative and informative associated factors assessed included practitioner factors of age (provided in 5-year categories), gender, being Australian-trained versus overseas-trained (medical degree), stage of training and practice (year graduated), hours worked, and practice factors of socio-economic status of practice and rurality and other variables such an involvement in education and bulk-billing.
Further outcomes measured were based on the initial response to use of digital decision support tools including clustered five-point Likert scale ratings of positive sentiments (facilitators) towards the use of technology including that it (1) improves patient outcome and satisfaction, (2) improves care processes, (3) saves times for clinicians and patients, and (4) has widespread use amongst practice staff. Negative sentiments (barriers) included technology (1) not having sufficient support, (2) being incompatible with existing IT systems, (3 & 4) raising patient and clinician concerns about data privacy and security, and (5) being difficult and time-consuming to use.
Statistical analyses
Descriptive statistics were used to quantify the use of decision support tools and digital health for clinical audit and research. Reported are frequencies for categorical variables. A comparison of average five-point Likert scale ratings for facilitators and barriers regarding use of technology in GP consultations was also completed. A multivariable logistic regression model was used to determine positive practitioner and practice associations with the use of digital decision support tools in clinical general practice. The model was informed by theoretical considerations and factors of importance identified from literature. There were a limited number of candidate variables that had been collected in the MABEL survey and so all were included.
The resulting adjusted odds ratio is adjusted for other covariates, including confounders. A list of variables is given above in ‘outcome measures.’ The model estimated odds ratios with 95% confidence intervals. Statistical significance was inferred at two-sided p < 0.05. Statistical analysis was completed using R studio 2022.07.2 Build 576 (R version 4.2.1).
The MABEL study was approved by the University of Melbourne Faculty of Business and Economics Human Ethics Advisory Group (Ref. 0709559) and the Monash University Standing Committee on Ethics in Research Involving Humans (Ref. CF07/1102 2007000291). We report in accordance with the STROBE guidelines (von Elm et al. Reference von Elm, Altman, Egger, Pocock, Gotzsche, Vandenbroucke and Initiative2007).
Results
Descriptive statistics
The characteristics of study participants are outlined in Table 1. In response to whether they used electronic decision support tools to inform decisions, 2240 GPs responded in the affirmative, 280 responded no, but would like to and 154 responded no and don’t need to (Table 2 & Figure 1).
Table 1. Study characteristics
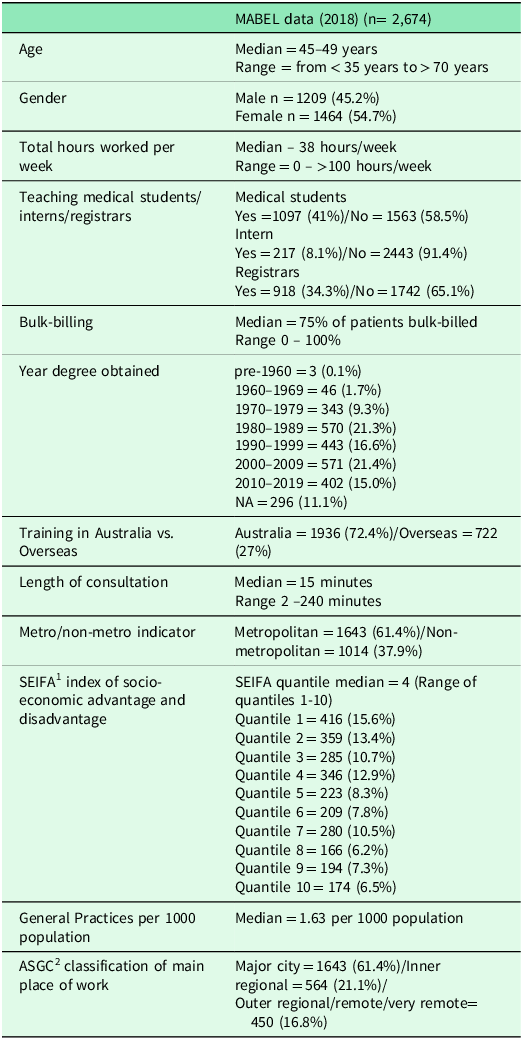
1 SEIFA = Socio-economic indexes for areas.
2 ASGC = Australian standard geographical classification.
Table 2. Use of digital health technologies/solutions
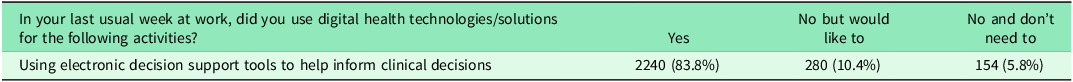
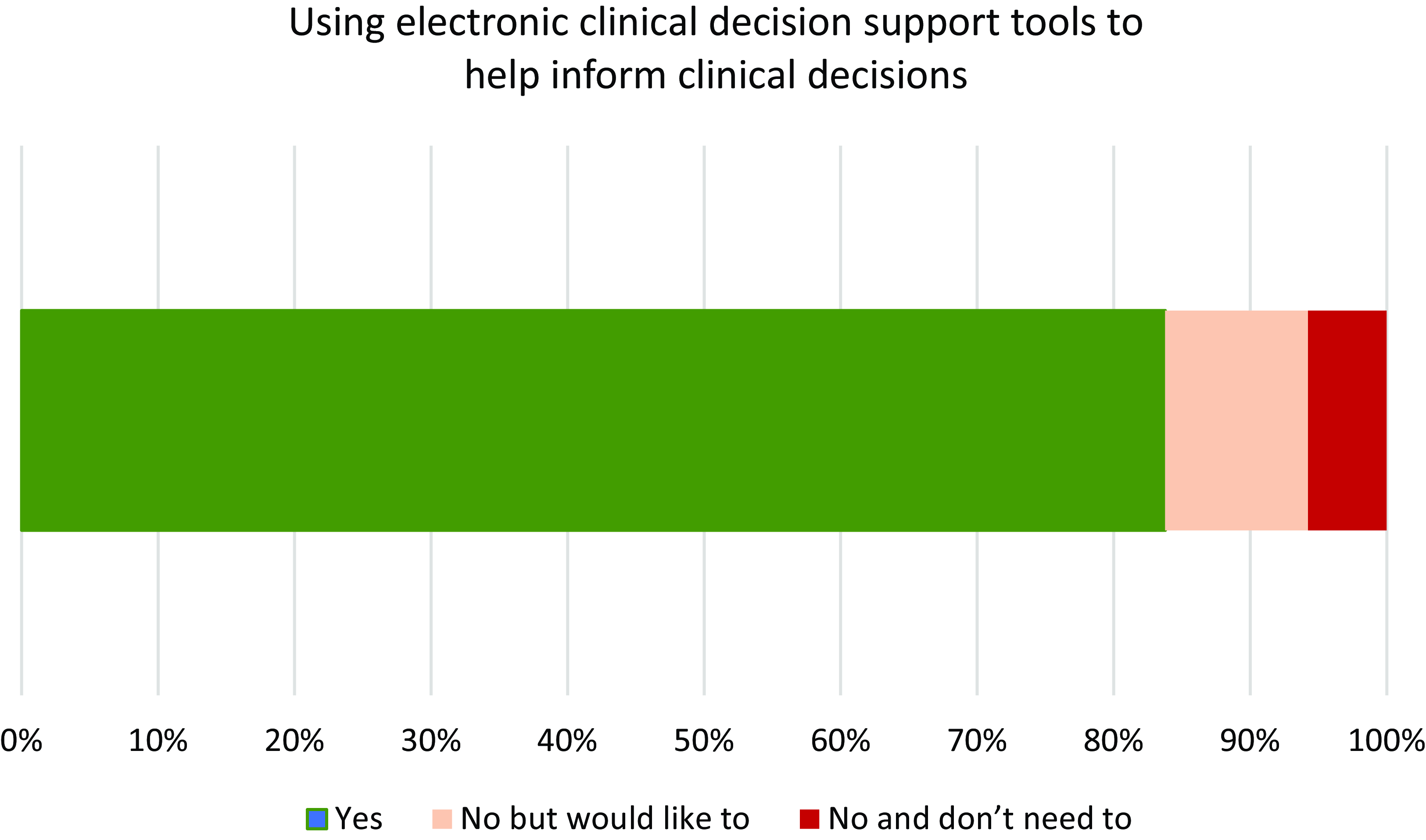
Figure 1. Use of elctronic health technologies / solutions by general practitioners for decision support.
Table 3 (and Figure 2) demonstrates that most respondents agreed with facilitators expressed about the use of digital health technologies and solutions in clinical practice. This was balanced by support for barriers regarding IT compatibility, support, and concerns about privacy. There was overall disagreement with the statement that digital health technologies and solutions are too difficult and time-consuming to use.
Table 3. Facilitators and barriers regarding the use of digital health technologies/solutions
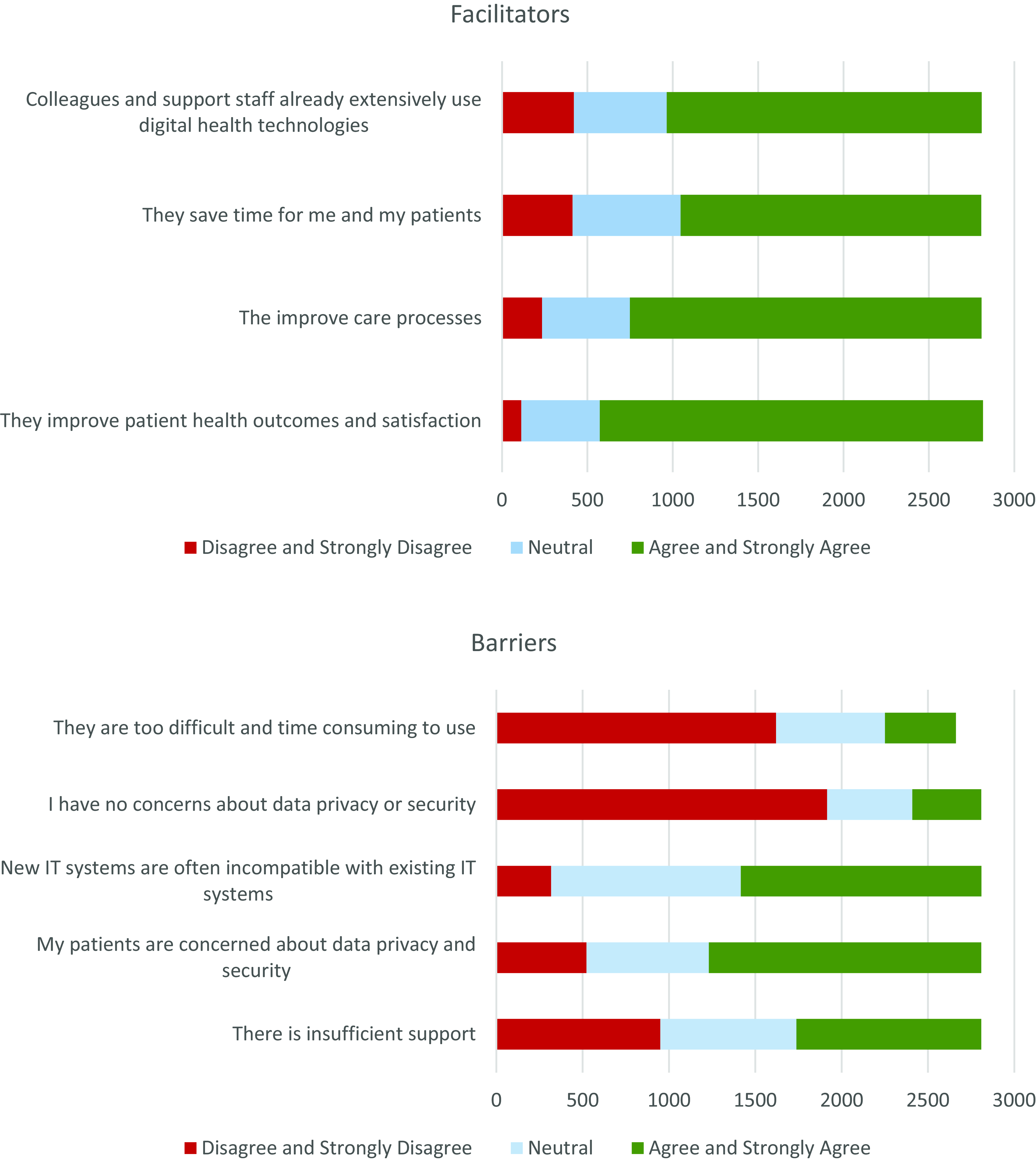
Figure 2. Facilitators and barriers regardin use of digital health technologies / solutions.
When comparing practitioner and practice characteristics with an increased likelihood of using digital decision support tools, being female (OR 2.13, (95% CI 1.41, 3.26), p < 0.001) and percentage of patients being bulk-billed (OR 1.08, (95% CI 1.01, 1.14), p = 0.016) was positively associated. Bulk-billing refers to when a general practitioner accepts the Medicare (government-funded) benefit as full payment of the fee for a service, with no gap (additional) payment payable by the patient. Some of the older age groups, in particular GPs aged 60-64 years (OR 0.21, (95% CI 0.05, 0.98), p = 0.042) were associated with a significantly lower likelihood of using digital decision support tools compared with those aged under 35 years. There were no significant associations between digital decision support tools use and age, involvement in education activities, location of practice, length of consultation, length of time in clinical practice, duration of consultation, and hours worked per week (table 4).
Table 4. Outcomes of logistic regression examining the likelihood of using digital decision support tools
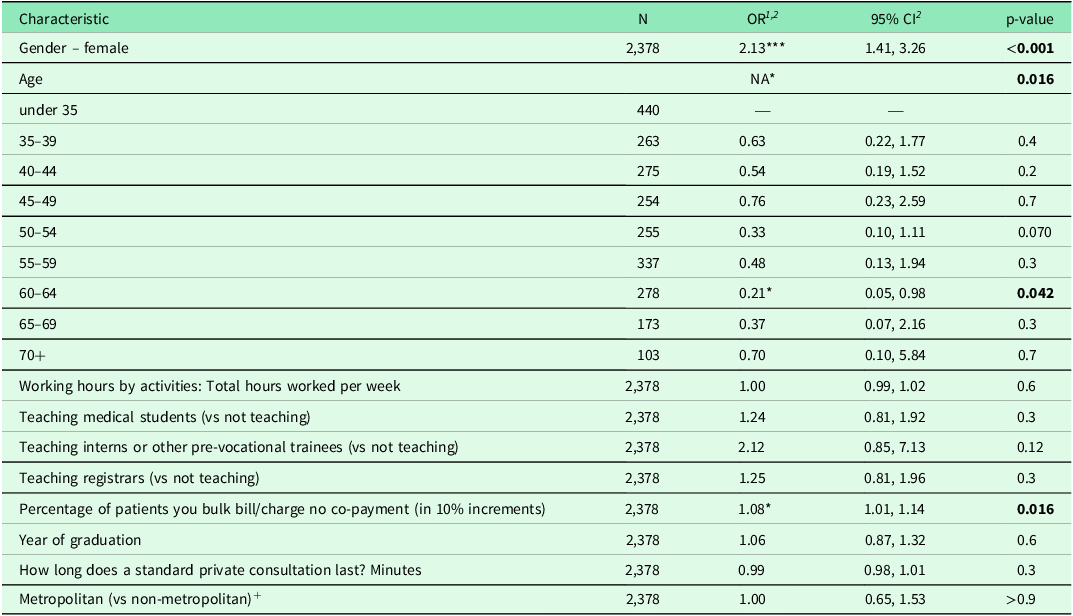
1 *p < 0.05; **p < 0.01; ***p < 0.001.
2 OR = Odds Ratio, CI = Confidence Interval.
+ Metropolitan and non-metropolitan areas defined by Australian Standard Geographic Classification and Rural, Remote and Metropolitan Area Classification.
Discussion
The majority of Australian GPs in this study utilize digital decision support tools in their everyday practice. The results of this study identify both the facilitators and barriers in the uptake of digital decision support tools use by Australian GPs. There was higher uptake amongst female GPs, bulk-billing practices, and younger GPs. The MABEL study compared closely with recent data from the Australian Government Department of Health and Aged Care (2022) examining the characteristics of Australian GPs except where there were proportionally less Australian and New Zealand-trained GPs (58.6%) working than responded in the MABEL study (72.4%). There is general concordance except in the Australian-trained versus overseas-trained responses, suggesting reasonable representation by the study data of the existing general practice population.
Perceived barriers to digital decision support tool uptake
Previous research identifies that trust in digital decision support tools is affected by concerns around accuracy (Ford et al. Reference Ford, Edelman, Somers, Shrewsbury, Lopez Levy, van Marwijk, Curcin and Porat2021) and the fear that such resources could be used against clinicians in the event of medico-legal controversies (Liberati et al. Reference Liberati, Ruggiero, Galuppo, Gorli, Gonzalez-Lorenzo, Maraldi, Ruggieri, Polo Friz, Scaratti, Kwag, Vespignani and Moja2017). There are also concerns about having to adapt consultations styles to a resource (Lugtenberg et al. Reference Lugtenberg, Weenink, van der Weijden, Westert and Kool2015; Porat, Delaney & Kostopoulou Reference Porat, Delaney and Kostopoulou2017), and it being a threat to physicians’ critical thinking and professional autonomy with over-simplification of complex clinical situations which do not account for the nuances of patient presentation or care (Greenes et al. Reference Greenes, Bates, Kawamoto, Middleton, Osheroff and Shahar2018; Sutton et al. Reference Sutton, Pincock, Baumgart, Sadowski, Fedorak and Kroeker2020). Many digital decision support tools remain unused as they are perceived as time-consuming and of little additional benefit for GPs (Bouamrane & Mair Reference Bouamrane and Mair2013). Such programmes also interrupt clinic workflow, with most alerts often being dismissed and contributing to ‘alert fatigue’ (Ancker et al. Reference Ancker, Edwards, Nosal, Hauser, Mauer and Kaushal2017).
Incongruous with previous research was that barriers to digital decision support tools uptake including ease of use were not identified as a concern for Australian GPs in this secondary analysis. This has been identified in previous studies of GPs as a barrier to the uptake of digital decision support systems (Ford et al. Reference Ford, Edelman, Somers, Shrewsbury, Lopez Levy, van Marwijk, Curcin and Porat2021; Short, Frischer & Bashford Reference Short, Frischer and Bashford2004). Concerns regarding data privacy have been previously elicited (Australian Government Department of Health 2021; Ford et al. Reference Ford, Edelman, Somers, Shrewsbury, Lopez Levy, van Marwijk, Curcin and Porat2021). Specifically, there is a lack of clarity regarding privacy and consent requirements regarding access to data. Respondents in this study identified both personal and patient concerns regarding privacy as barriers to digital decision support tools adoption. Incompatibility with of digital decision support tools with existing IT infrastructure was also identified as a barrier to their use in this study of Australian GPs, as has been previously highlighted in similar studies (Ford et al. Reference Ford, Edelman, Somers, Shrewsbury, Lopez Levy, van Marwijk, Curcin and Porat2021). Previous research has also identified concerns regarding the credibility of information provided, the time taken to upskill, time taken to access external resources, and lack of funding to cover implementation costs (The Royal Australian College of General Practitioners 2022).
In this round of the MABEL survey, ‘cost’ was not asked as a potential barrier to use of digital decision support tools. Our secondary analysis of this existing survey’s data would not be able to infer any further information about this. Introducing this as a potential variable would be difficult as some resources are only accessible by subscription and payment, and some are government- or industry-funded and so would be readily available without any associated cost.
Female GP’s use of digital decision support tools
The finding that being a female GP is positively associated with use of digital decision support tools and digital health technology solutions in Australia is novel and no existing literature provides any similar comparison. It has been demonstrated previously that female physicians spend more time in electronic health record documentation both during and after work hours (Rotenstein et al. Reference Rotenstein, Fong, Jeffery, Sinsky, Goldstein, Williams and Melnick2022). It has been posited that this increased engagement with electronic documentation complements the tendency for female physicians to provide greater person-centred care and achieve correspondingly better clinical outcomes (Ganguli, Rivara & Inouye Reference Ganguli, Rivara and Inouye2022). Digital maturity, referring to the use of digital technologies to promote the delivery of high-quality healthcare, was found to be greater amongst male GPs globally in one study (Teixeira et al. Reference Teixeira, Li, Laranjo, Collins, Irving, Fernandez, Car, Ungan, Petek, Hoffman, Majeed, Nessler, Lingner, Jimenez, Darzi, Jacome and Neves2022). Non-GP-specific research suggests that confidence in technology may be gendered, with women more anxious than men about IT use, reducing their self-effectiveness and increasing perceptions of IT requiring greater effort (Goswami & Dutta Reference Goswami and Dutta2016). Self-efficacy in the use of digital technologies is a key motivational construct underpinning their use (Rohatgi, Scherer & Hatlevik Reference Rohatgi, Scherer and Hatlevik2016) and women and men tend to differ in their levels of confidence in their capacity to acquire and use digital skills (European Institute for Gender Equality 2020). Further research would elucidate the reasons behind greater female engagement with digital health technology solutions.
Bulk-billing and digital decision support tool use
There was also a positive effect with respect to an increased likelihood of using digital decision support tools in a bulk-billing setting. The odds of using digital decision support tools increased by 8% for every 10% increase in the proportion of bulk-billed patients. If use of digital decision support tools is associated with better clinical outcomes given its benefits to both patients and practitioners, then this finding suggests that GPs can bulk-bill consultations and still provide evidence-based and safe care for patients with utilization of digital decision support tools. There is no previous research to suggest differences in quality of care with bulk- vs. privately-billed GP consultations and an analysis of consumer surveys demonstrated no change in patient perception of quality of care with bulk-billing consultations (Mu et al. Reference Mu, De Abreu Lourenco, van Gool and Hall2017). Some digital decision support tools such as the Therapeutic Guidelines are freely available to doctors in public hospitals, but paid for privately by GPs. There exists hence a financial disincentive for GPs and private practices to utilize digital decision support tools (The Royal Australian College of General Practitioners 2023).
A pattern of negative association was observed with being older and using digital decision support tools, particularly in those aged 60–64 years. A 2014 study found that older GPs, particularly over 50 years of age, were less likely to use a computer for clinical activity than younger counterparts (Henderson et al. Reference Henderson, Pollack, Gordon and Miller2014). Other research, not specific to medical practitioners, showed that despite increased uptake in technology use in the population, older adults engaged with it less, being more wary of the limitations of technology (Mahajan et al. Reference Mahajan, Lu, Spatz, Nasir and Krumholz2021).
There was no significant association between digital decision support tools use and location of practice, length of consultation, length of time in clinical practice, duration of consultation and hours worked per week. Given that most GPs use digital decision support tools, it may be cautiously interpreted that digital decision support tools and the infrastructure required to support this are readily available and more importantly, used by GPs. The previously identified concerns regarding digital decision support tools integration into existing information technology systems appear to not be a substantial barrier in the Australian GP context.
GP clinical reasoning, learning and considerations of digital decision support tools use
That the majority of GPs (83.8%) indicated that they were using digital decision support tools may reflect an overall acceptance of the role of technology in general practice functioning as users are likely to adopt technologies that align with their beliefs (Ertmer et al. Reference Ertmer, Ottenbreit-Leftwich, Sadik, Sendurur and Sendurur2012). This comes despite a potential barrier of the ‘double innovation problem’ where users must first learn the technology, before deciding how to then integrate it into workflow (Johnson et al. Reference Johnson, Jacovina, Russell, Soto, Crossley and DS2016). Given the rapid change of technological innovation and increasing number of digital health resources, a significant learning curve is presented to GPs to then adapt their practices to (The Royal Australian College of General Practitioners 2022).
Another concern regarding the use of digital decision support tools is the perception that technology will replace or erode the skill of clinical reasoning (Ford et al. Reference Ford, Edelman, Somers, Shrewsbury, Lopez Levy, van Marwijk, Curcin and Porat2021). The rapid availability of information via connected webs of resources can strengthen learners’ ability to scan information rapidly and efficiently (Ioncica, Dona & Militaru Reference Ioncica, Dona and Militaru2016). The replacement of semantic with transactive memory renders the style of ‘learning facts’ less important. There are concerns that a reliance on technology and ‘cognitive offloading’ will fragment attention spans and inhibit higher-order cognitive processes including reflection, inductive problem solving and critical thinking (Greenfield Reference Greenfield2009; Ioncica, Dona & Militaru Reference Ioncica, Dona and Militaru2016). The exact impact, for better or worse, of this change in memory use and learning styles on clinical reasoning skills in the general practice context is not well understood and would benefit from further research. This is especially important with the proliferation of different types of medical technologies and their hastened adoption by many GPs in the time of the COVID-19 pandemic.
Strengths and limitations
This study has several strengths. It uses an Australian-specific dataset with a large sample size and will likely be representative of the Australian general practitioner population, to determine digital decision support tools usage patterns, its sentiments, and its associations. The response rate, though modest, is high amongst medical practitioner who are known to be time-poor. The MABEL dataset collected multiple variables on technological use in clinical practice, enabling us to closely examine its associations with practitioner and practice characteristics. This study is primarily epidemiological in nature and confirms some, whilst refuting other, previously identified patterns of clinician use of digital decision support tools. The findings would be further informed by employing qualitative techniques to further elicit the reasons behind the observed findings. It also needs to be interpreted in the context of potential limitations.
The MABEL survey was designed to examine key determinants of labour supply and mobility with extensive piloting before implementation. The questions on facilitators and barriers were decided by the MABEL research team for the 2018 wave. This study is a secondary analysis of the MABEL dataset and the authors did not have input into the selection of questions on facilitators and barriers. There is always a need to be cautious in interpreting the findings from a secondary analysis of a larger data set, where survey questions regarding the use of digital decision support tools are not necessarily granular in detail and where collapsing outcome variables for statistical analysis can affect the effect estimate and inferences drawn from the data.
The data presented was collected in pre-COVID pandemic in 2018. There has been a significant change since then with respect to the amount of technological engagement involved in everyday GP. Nevertheless, the sentiments, facilitators and barriers to technology use and the uptake of digital decision support tools specifically can be interpreted independently of the administrative technologies such as telehealth and e-prescribing that became more utilized during the COVID-19 pandemic.
Conclusion
This study suggests that the majority of Australian GPs are using digital decision support tools and digital technology in their clinical practice. Whilst the previously identified barriers to digital decision support tools use including lack of knowledge, lack of trust and workflow disruption were not identified in this study of Australian practice, concerns regarding data privacy, information technology system incompatibility and lack of support remain. We found positive associations between digital decision support tools use and female gender, younger age, and increased bulk-billing rate. Understanding the facilitators and barriers to GP use of digital decision support tools may help further the understanding of the impact it has for workflow and clinical reasoning skills. Co-producing resources with GPs and actively addressing barriers and capitalizing on facilitators may encourage uptake and assimilation of new and beneficial technologies within existing workflow and practice systems in an unobtrusive manner.
Acknowledgements
Nil.
Funding statement
None – there is no funding to declare for this article.
Competing interests
There are no competing interests to declare.









