To the Editor
The objective structured clinical examination (OSCE) was first incorporated into medical training over 40 years ago and has since become a staple in the education and evaluation of undergraduate medical students and residents. Reference Harden and Gleeson1 Trainees can be evaluated on virtually any medical skill or technique, including physical examination, communication, forming a differential diagnosis, acute management, and interpretation of laboratory results or imaging. OSCEs also allow for specific, individualized feedback, which can be given immediately after the examination.
The majority of published studies involving OSCEs in medical training are focused on undergraduate medical education, where feasibility and effectiveness in assessing competencies have been demonstrated convincingly. Reference Patricio, Juliao, Fareleira and Carneiro2 The main drawback is that OSCEs have a greater associated burden in terms of cost, space requirements, and examiner time commitment when compared to other examination modalities. Reference Patricio, Juliao, Fareleira and Carneiro2 In addition to undergraduate medical education, OSCEs have also been shown as an effective assessment and educational tool in many other training contexts, including medical residency (both medical and surgical), Reference Pugh, Touchie, Humphrey-Murto and Wood3–Reference Aras and Serim Demirgoren6 fellowship, Reference Avelino-Silva, Gil and Suemoto7,Reference Wolff, Balzora and Poles8 nursing, Reference Ha and Lim9 pharmacy, Reference Farahani, Farahani, Deters, Schwender and Laeer10 and dentistry. Reference Brown, Manogue and Martin11
While OSCEs have classically been done in person, the COVID-19 pandemic led to a transition to virtual OSCEs, achieved with the aid of teleconferencing applications. Reference Chan, Choa, Kelly, Maru and Rashid12,Reference Grover, Pandya, Ranasinghe, Ramji, Bola and Raj13 However, while OSCEs are a near-ubiquitous element of training in medical school and residency, they are much more rarely used in epilepsy fellowship training. This may be a missed opportunity to enhance the training of epilepsy fellows.
In 2019, a yearly formative OSCE for pediatric and adult EEG/epilepsy fellows was designed and implemented, with the goal of enhancing education and preparing trainees for the Canadian Society of Clinical Neurophysiologists (CSCN) EEG Examination. 14 The examination is offered in French and English. Stations include technical EEG issues, short cases, and long cases. The technical EEG station requires examinees to recognize technical issues with an EEG (e.g., artifact) and explain how to remedy them. The short cases involve a series of 1 to 2-page EEG excerpts on paper; examinees review each short case and then answer short questions. The long case requires examinees to review a routine video EEG on a computer, and then write a written report summarizing the findings. We also initially included a communication station that required examinees to disclose a new diagnosis of epilepsy to a standardized patient; however, this was later discontinued as examinees did not find it relevant to the CSCN examination. After each examination, we send participants in the formative OSCE an anonymous electronic questionnaire to solicit feedback. The questionnaire was sent after the CSCN examination so that participants had the option to anonymously report if they had been successful.
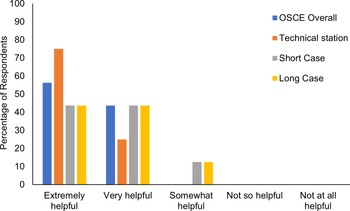
In the five years we have been offering the formative OSCE, the interest and feedback from participants have been universally positive. Despite pandemic-related interruptions, 18 trainees have taken the examination in that time, including three pediatric neurology residents and 15 epilepsy fellows. Sixteen participants (89%) completed the post-test anonymous survey, with 56% rating the OSCE “extremely helpful” and the remaining 44% “very helpful” (Fig. 1). The technical station was rated the highest of the three stations. Fourteen participants reported their outcomes on the CSCN examination, with two stating that they did not take the CSCN examination that year. The CSCN examination includes three components: clinical, technology, and physiology; 13/14 (93%) reported passing all elements while one individual (7%) reported only failing the clinical element (Fig. 2).
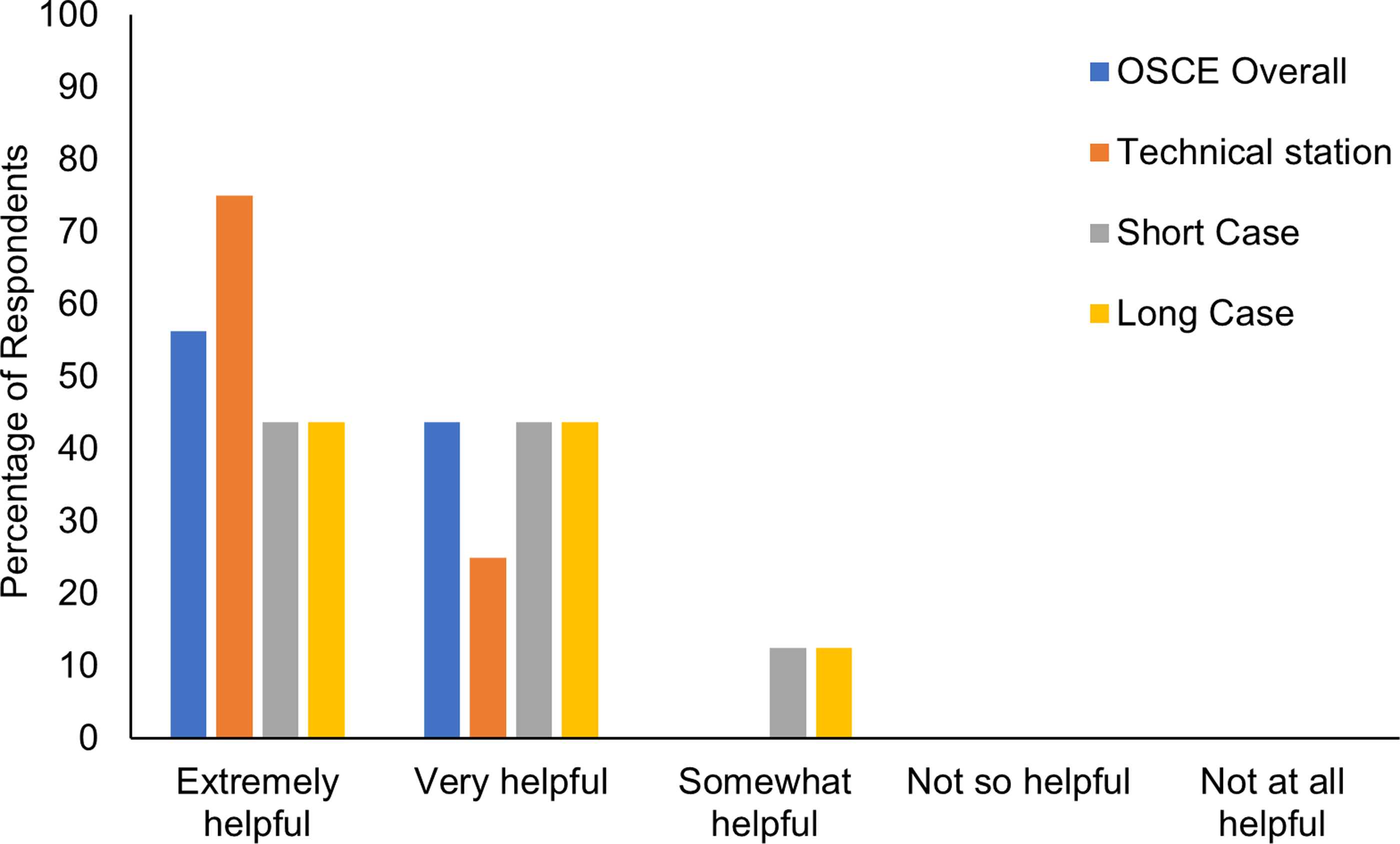
Figure 1: Participant feedback regarding utility of formative objective structured clinical examination. OSCE = objective structured clinical examination.
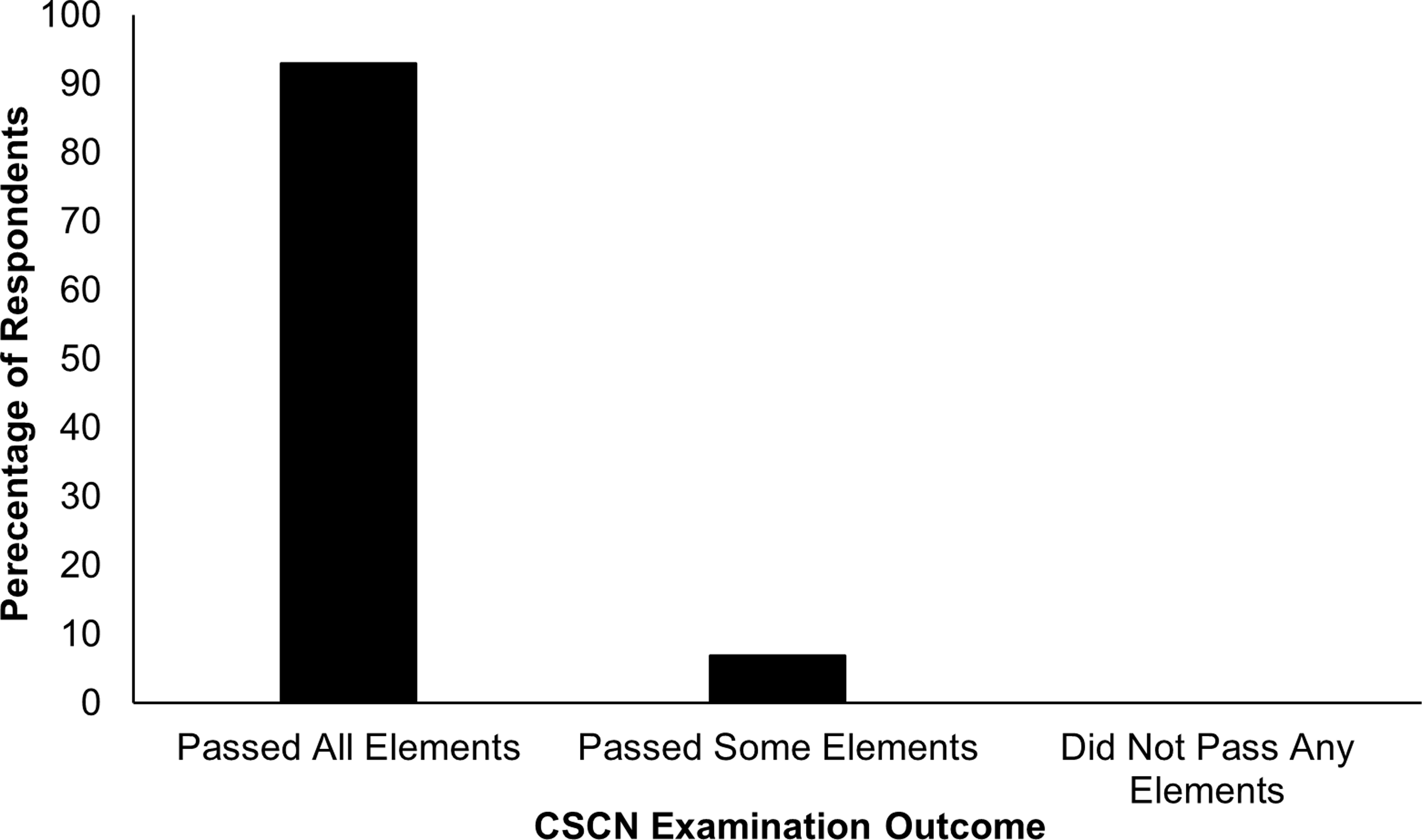
Figure 2: Participant-reported outcomes on canadian society of clinical neurophysiologists EEG examination. CSCN = Canadian Society of Clinical Neurophysiologists.
The experience with this formative examination suggests that OSCEs may be an underused tool in the training of epilepsy fellows. A review of the literature for publications related to OSCE and epilepsy training revealed only a study by Valentine et al, reporting on the utility of OSCE in training residents to give a diagnosis of psychogenic non-epileptic seizures. Reference Valentine, Kurzweil, Zabar and Lewis15 A standard epilepsy fellowship involves primarily reading and reporting EEG and attending epilepsy clinics, and there is often little to no observed history-taking, counseling, or neurologic examination, so fellows tend to receive very little feedback in these areas. While OSCEs have been noted to be expensive and labor-intensive in general, our formative epilepsy OSCE has been run with essentially no financial cost and with only one or two staff present (an additional examiner is necessary if the communication station is included).
While our formative examination focused on preparing trainees for a specific qualifying examination, the greatest potential for OSCE in epilepsy fellow training may lie in the evaluation and improvement of communication skills. Difficult conversations are common in epilepsy practice and include explaining the initial diagnosis of epilepsy, counseling on seizure safety precautions, and discussing sudden unexpected death in epilepsy. Reference Donner and Buchhalter16 A good epileptologist must be able to communicate clearly and sensitively with patients and their families. An OSCE gives supervising epileptologists the opportunity to assess the level of expertise trainees have with these conversations and give appropriate feedback.
The emergence of teleconferencing tools that facilitate virtual OSCEs may hold particular potential in epilepsy training when compared to surgical residencies and fellowships or other specialties in which procedural or physical examination skills are more important. While in-person evaluation has its traditional advantages, virtual OSCEs allow for evaluation of trainees spread over a wide geographical area and also eliminate the need for a physical space in which to hold the examination.
Moving forward, more research is necessary to determine how best to incorporate OSCEs into epilepsy fellowship training. Incorporating standardized patients and/or actual people with epilepsy and their families could allow for more meaningful feedback on communication. The optimal timing for OSCEs is also important. Having a baseline OSCE at the start of training, followed by repeat testing every 4–6 months, would allow for staff and trainees to assess progress and enhance education. From a standardization of training perspective, accreditation bodies might consider mandating OSCEs as an essential element of epilepsy fellowship program curricula.
While we have focused on epilepsy, other fellowship training programs, both neurologic and non-neurologic, may consider whether incorporating OSCEs into their training curricula could be beneficial. As an example, neuromuscular fellowship program directors could consider whether their trainees have sufficient observed evaluations of technical skills such as nerve conduction studies and electromyography; if not, regularly scheduled OSCEs could potentially enhance the training of fellows in these programs. As well, communication skills are an important element of all medical specialties, and OSCEs allow the opportunity to ensure that such skills are being maintained at the fellowship level.
In summary, OSCEs offer the potential to enhance the training of epilepsy fellows and may improve performance on qualifying examinations. Fellowship programs should review curricula and consider whether OSCEs can be better implemented to improve the educational experience of their trainees.
Statement of authorship
KAM designed and executed the study, prepared figures, and drafted and edited the manuscript.
Funding statement
This study was supported by funding from the Fonds de Recherches du Québec – Santé (KAM).
Competing interests
In the past 36 months, Dr Myers has received research grants from Fonds de Recherche du Québec – Santé, Liam Foundation, Epilepsy Canada, Grand Défi Pierre Lavoie Foundation, and Pediatric Research Foundation. Dr Myers is on the Scientific Advisory Boards of the Koolen-de Vries Syndrome Foundation and Ring 20 Research & Support.