Introduction
Mental disorders are prevalent worldwide. Estimates indicate that one in three individuals will develop a mental disorder during their lifetime (Chesney et al., Reference Chesney, Goodwin and Fazal2014; Steel et al., Reference Steel, Marnane, Iranpour, Chey, Jackson, Patel and Silove2014; Vigo et al., Reference Vigo, Thornicroft and Atun2016). While many mental disorders respond well to treatment, having a mental disorder can result in a considerable burden for the individual because of the health loss experienced, as well as the stigma and marginalisation that can be associated with having a mental disorder (Schofield et al., Reference Schofield, Shrestha, Percival, Passey, Callander and Kelly2011). In 2017, mental disorders and substance use disorders constituted 14.4% of the global disability and were the second largest of any group (Institute for Health Metrics and Evaluation, 2020a).
Those with mental disorders may have periods of reduced ability to participate in the labour force, which can result in a lack of income for the individual (Schofield et al., Reference Schofield, Shrestha, Percival, Passey, Callander and Kelly2011). The lack of participation in the labour force can also contribute to substantial societal cost because of production loss and reduced income taxation – besides the direct treatment cost (Schofield et al., Reference Schofield, Shrestha, Percival, Passey, Callander and Kelly2011). In addition to epidemiological measures such as morbidity and mortality, the importance of mental disorders can also be investigated through cost-of-illness studies within health economics. Previous systematic reviews have documented the cost for various mental disorders (Luppa et al., Reference Luppa, Heinrich, Angermeyer, Konig and Riedel-Heller2007; Fajutrao et al., Reference Fajutrao, Locklear, Priaulx and Heyes2009; Konnopka et al., Reference Konnopka, Leichsenring, Leibing and Konig2009; Stuhldreher et al., Reference Stuhldreher, Konnopka, Wild, Herzog, Zipfel, Lowe and Konig2012; Chong et al., Reference Chong, Teoh, Wu, Kotirum, Chiou and Chaiyakunapruk2016; Jin and Mosweu, Reference Jin and Mosweu2017). Most reviews have focused on common mental disorders (e.g. depression, anxiety) and on schizophrenia and eating disorders, but the cost of some mental disorders such as developmental disorders and intellectual disability disorders has not yet been examined in a systematic review. Additionally, past systematic reviews have focused on a specific country or a region and not on the economic burden worldwide and some are more than a decade old, resulting in a significant gap in the current literature.
The aims of this systematic review were to identify cost-of-illness studies for mental disorders worldwide and to explore the distribution of the cost between disorders. To explore the cost distribution, we extracted data on key parameters such as types of mental disorder, methodology, cost categories, geographical location, etc., and assessed the study quality of the included studies. In particular, we focused on prevalence-based studies reporting the societal cost per patient by mental disorder, study quality and by country in our investigation and examined the percentages of the direct cost and indirect cost.
Methods
Within the field of health economics, a wide range of economic analyses are available (e.g. cost-of-illness analysis, cost-effectiveness analysis, cost-utility analysis and cost-benefit analysis), supporting decision making and mental health practices (Knapp and Wong, Reference Knapp and Wong2020). Cost-of-illness studies aim to estimate the total cost or excess cost of people diagnosed with a disease of interest (Akobundu et al., Reference Akobundu, Ju, Blatt and Mullins2006). Historically, there are three broad types of cost categories: direct cost, indirect cost and intangible cost. Direct cost refers to health care resources such as diagnostic, treatment and rehabilitation and non-health care resources such as transportation, household expenses and community-based services. Indirect cost refers to costs related to production loss from morbidity and mortality borne by the individual, society and/or the employer. Intangible cost refers to the psychological pain experienced by people with mental disorders and their families but these costs are seldom included in cost-of-illness studies (Tarricone, Reference Tarricone2006; Jo, Reference Jo2014). The perspective used in a cost-of-illness study defines which cost categories to include. The broadest perspective is the ‘societal’ where all costs in a society are examined regardless of who pays the costs. Therefore, both direct and indirect cost have to be included and preferably also intangible cost, but not all studies report the direct and indirect cost disaggregated from the societal cost. Cost-of-illness studies can use either a prevalence or an incidence approach (Jo, Reference Jo2014). Prevalence-based studies, the most common approach of cost-of-illness studies, provide useful information for health planners (e.g. which disorders are associated with larger cost, what are the major cost categories, how are health investments distributed). Incidence-based studies can be used in cost-effectiveness evaluations of preventive initiatives and disease management (Jo, Reference Jo2014).
Eligibility criteria
This systematic review was carried out in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher et al., Reference Moher, Liberati, Tetzlaff, Altman and Group2009). The project protocol was preregistered at the website International prospective register of systematic reviews (PROSPERO) before commencement (registration number CRD42019127783).
A PICO (Participants, Interventions, Comparisons, Outcomes) framework (Schardt et al., Reference Schardt, Adams, Owens, Keitz and Fontelo2007) was used to develop the inclusion and exclusion criteria. The predefined inclusion criteria were: (1) cost-of-illness studies or cost-analyses, (2) diagnosis of at least one mental disorder according to any published criteria (excluding dementia to follow the definitions of mental and substance use by the Global Burden of Disease Study (Institute for Health Metrics and Evaluation, 2020b)), (3) the sampling frame was based on the general population (e.g. not restricted by anything other than age and geographical location), (4) original results and (5) results reported in monetary units.
Systematic searches
The search strings for the systematic searches contained two parts. One part with comprehensive key terms for different mental disorder groups and another part with comprehensive key terms for cost studies. A detailed description is available in Online Resource 1. The systematic searches were conducted between May and June 2019 in the databases PubMed, EMBASE, Web of Science, EconLit, NHS York Database and PsychInfo. In order to make the study tractable, the searches were restricted to studies published between 1980 and May 2019. Animal studies and clinical trials were excluded. No restrictions regarding geographical location or language were used. Covidence (Kellermeyer et al., Reference Kellermeyer, Harnke and Knight2018), an online tool to assist the systematic review workflow, was used for the title/abstract screening. Two independent reviewers screened all titles/abstracts for eligibility, followed by full-text screening for potentially relevant articles according to the predefined inclusion and exclusion criteria. Any conflicts were resolved by consensus. We developed a hierarchy to force a study to have only one exclusion reason for the purpose of PRISMA reporting. However, some studies could have been excluded by more than one criterion. If a full publication was not available from online searching, a request to the university library was made. If a full publication was not available before the 6th of September 2019, the study was excluded.
Snowball searches
The systematic searches were supplemented with snowball searches. First, the reference lists from reviews and systematic reviews on this topic were screened (by title) in order to identify additional potentially relevant articles. Full texts were retrieved and screened by two independent reviewers. The same snowball procedure was used on the reference lists from the included studies from the systematic searches until no additional candidate studies were identified.
Quality reporting assessment
A modified version of the quality reporting checklist from Stuhldreher et al. (Reference Stuhldreher, Konnopka, Wild, Herzog, Zipfel, Lowe and Konig2012) was used to assess the reporting quality of the included studies (see eTable 1 in Online Resource 2). The revised checklist consisted of 14–15 items scored yes/no (only studies with a time period greater than 1 year could be allocated the item related to discounting (item number 7)). An objective and reliable assessment of study quality can be difficult. However, reporting certain features and principles is thought to correlate with reliable outcomes (Frederix, Reference Frederix2019). The quality reporting scores were standardised to a 10-point scale.
Data extraction and management
A data dictionary was developed to guide the extraction process. Information about author(s), publication year, title, country, city, diagnosis, diagnostic criteria, sample size, age, sex, data sources, study perspective, study period, reference year, currency, costing approach, cost categories, discount rate, production loss method and cost unit was extracted from every study. Different assumptions and decisions were made during the data extraction phase. Some studies reported estimates for more than one time period (e.g. cost for the year preceding index diagnosis, a year after diagnosis, 2 years after diagnosis, etc.). In that case, we only extracted the latest, most comprehensive estimates. If a study did not report the reference year, it was set to 1 year prior to the publication date. If a cost estimate was not explicitly stated in the text/table/figure, the study was excluded based on the lack of availability of a result in monetary unit. If the cost estimates were reported only for subgroups (e.g. by sex or age group) and if these subgroups were mutually exclusive and comprehensively exhaustive, the cost estimates were extracted by summing the costs across the different strata. If estimates for a disorder of interest were aggregated with unknown disorders or disorders not of interest, the estimates were excluded. In cases where the lower age limit was stated with ‘less than’, the limit was assumed to be the earliest onset of the disease (see eTable 2 in Online Resource 2), and in cases where an age group was reported with ‘ + ’ (e.g. 65 + years), the age limit 99 years was assumed. Transfer payments were not extracted since these are not a cost for society but a redistribution of resources. If estimates included transfer payment, the amount was subtracted and if it was not possible to subtract because of lack of information of the size of the transfer payment, the estimate was not extracted. If two or more studies reported estimates from the same dataset with an overlap in time, only the study with the most comprehensive estimates was kept.
For the prevalence-based studies, the extracted estimates were recalculated into yearly cost, adjusted for inflation within the country until year 2018 and adjusted by the country's purchasing power parity (PPP) rate to the US price level. The PPP adjustment attempts to equalise the purchasing power between countries by removing price-level differences (OECD, 2020), which makes international comparison possible, but with the limitation that the PPP estimates do not reflect the real spending within a country. Inflation rates from the International Money Fund (International Monetary Fund, 2020) and PPP conversion rates for 2018 from the Organisation for Economic Co-operation and Development (OECD) Data (OECD, 2020) were used for the PPP adjustment, and if the PPP rates were not available, we used other sources (The World Bank, 2019; Quandl, 2020). The incidence-based studies with a lifetime perspective were not recalculated due to a lack of information about the time period.
All estimates were divided into broad disorder groups based on diagnosis: ‘substance use disorders’, ‘schizophrenia’, ‘mood disorders’, ‘neurotic disorders’, ‘eating disorders’, ‘personality disorders’, ‘intellectual disabilities’, ‘developmental disorders’, ‘behavioural disorders’ and ‘more than one mental disorder group’ (International Classification of Diseases 8 and 10 codes in eTable 2 in Online Resource 2).
To explore the distribution of the costs between mental disorders, we performed a descriptive analysis (mean, median, range and interquartile range) focusing on prevalence-based studies reporting societal cost per patient by disorder group. In the post-hoc analyses, we examined the distribution according to quality reporting score and the influence of two multi-site studies. Additionally, we display the distributions of the costs graphically, and for studies that provided sufficient data to fractionate the direct cost and indirect cost, we estimated the average percentages of direct cost and indirect cost of the societal cost. An interactive website is available at https://nbepi.com/econ, where all estimates and reference details are available for download. All analyses were performed in R version 3.5.1.
Results
Included studies
In total, the systematic searches resulted in 13 579 candidate studies after the removal of duplicates. In total, 439 studies were deemed potentially relevant based on their title/abstract and 112 studies were included after full-text review. An additional 31 studies were subsequently identified from snowballing reference lists, resulting in a total of 143 included studies. The references for these studies can be found in Online Resource 1, where we also provide reference details for the included studies sorted by country, disorder group and cost category (direct, indirect or both). The majority of studies were excluded because they were not full publications (e.g. conference abstracts only), contained no diagnostic criteria, and were not representative of the general population (e.g. veterans, only private insurance members or special facilities residents) (Fig. 1).
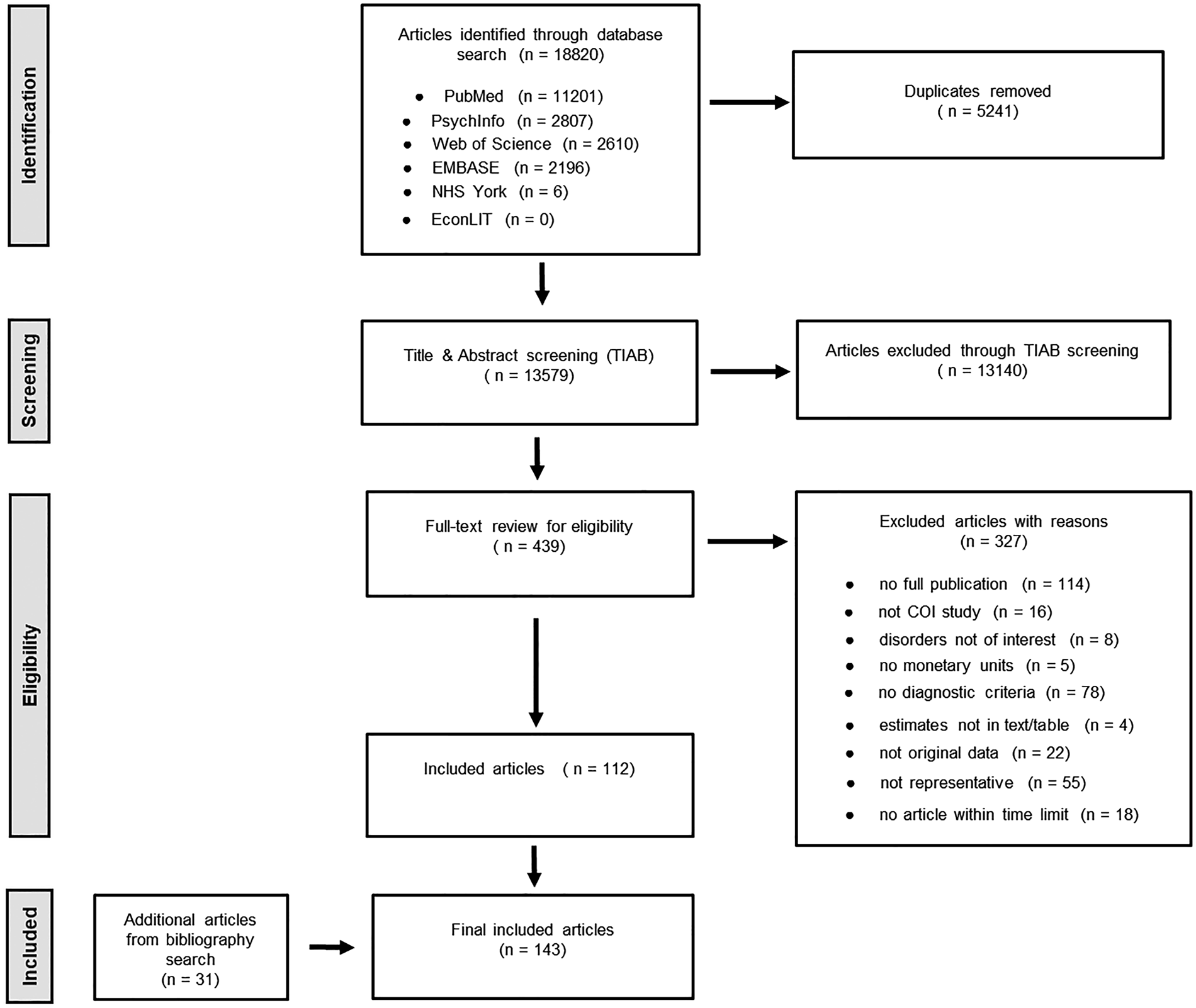
Fig. 1. PRISMAFootnote 1 diagram.
Description of studies
Studies from all countries and territories were included, but the vast majority were from high-income countries – the most common countries were the USA (24 studies), UK (23 studies) and Germany (23 studies). Three studies reported estimates for an African country (Ghana, Nigeria and South Africa) and only one study reported estimates for South America (Colombia). The number of studies by country is available in eTable 4 in Online Resource 2.
The disorder group most often investigated was mood disorders (54 studies), followed by schizophrenia (40 studies) and neurotic disorders (28 studies). Four of the nine disorder groups were investigated in fewer than ten studies worldwide and the disorder group least examined was intellectual disabilities, followed by eating disorders (six and seven studies, respectively). Additionally, 21 studies reported estimates for multiple disorder groups and six studies reported estimates on a combination of two or more disorder groups. A figure showing the number of studies per disorder group is presented in eFig. 1 in Online Resource 3.
The majority of studies (130 studies; 90.9%) used a prevalence-based approach, 12 studies (8.4%) used an incidence-based approach and one study used both (0.7%) (shown in eTable 3a and b in Online Resource 2). A total of 2884 cost estimates from the included studies were extracted. The number of estimates extracted from each study varied substantially, since one study could include estimates for more than one country, more than one disorder group and for several cost categories. Fifty-five studies reported only direct cost, five studies reported only indirect cost (the production loss) and the majority, 80 studies, reported societal cost. Furthermore, three studies reported intangible cost besides direct and indirect cost.
The included studies reported costs in various measures, e.g. cost per patient, national cost and excess cost per patient (comparing individuals with v. without the disorder of interest). The focus in the remaining part of the Results section is on societal cost per patient, but all estimates are available online (https://nbepi.com/econ). Consequently, all cost estimates presented from now are an aggregate of direct cost and indirect morbidity and mortality cost.
Societal cost per patient
Figure 2 shows the distribution of societal cost by country and mental disorder, ranked by societal cost per patient (619 estimates). Based on data from 34 countries, the data showed an expected distribution, with high-income nations ranking in the top part of the distribution (e.g. Australia, USA and UK). The same picture is seen without the PPP adjustment (eFig. 2 in Online Resource 3). Within each country, disorders such as schizophrenia and intellectual disabilities were generally associated with higher societal cost compared to neurotic disorders and eating disorders. The distribution of societal cost by mental disorder and study together with separate plots for the different disorder groups and cost per disorder ranked by USD PPP are presented in eFigs 3–5 in Online Resource 3, respectively.

Fig. 2. Societal cost per patient in US dollars adjusted by country's purchasing power parity and inflation until year 2018 (USD PPP 2018) by disorder group and country, ranked by USD PPP 2018.
The mean, median and interquartile range for societal cost per patient by disorder group in USD PPP are presented in Table 1. Developmental disorders only had two estimates and was left out in the following comparison because of the lack of data. The disorder group associated with the highest median societal cost per patient worldwide was schizophrenia with 13 256 USD PPP (mean 18 313; IQR = 13 671; range 3255–96 466). The disorder group associated with the lowest median societal cost per patient was eating disorders with 547 USD PPP (mean 1629; IQR = 364; range 41–38 183). Among 14 studies that reported direct and indirect cost separately from the societal cost per patient, the average contribution from indirect cost was almost half of the total with variation between the disorder groups (eTable 5 in Online Resource 2).
Table 1. Societal cost per patient in US dollars adjusted by country's purchasing power parity and inflation until year 2018 (USD PPP 2018) by disorder group

N, number of estimates (note one study can include several estimates for different countries); Qu, interquartile range.
Note: See eTable 3a in Online Resource 2 for study-by-study level detail about the cost reported
Two multi-site studies (Andlin-Sobocki et al., Reference Andlin-Sobocki, Jönsson, Wittchen and Olesen2005; Gustavsson et al., Reference Gustavsson, Svensson, Jacobi, Allgulander, Alonso, Beghi, Dodel, Ekman, Faravelli, Fratiglioni, Gannon, Jones, Jennum, Jordanova, Jonsson, Karampampa, Knapp, Kobelt, Kurth, Lieb, Linde, Ljungcrantz, Maercker, Melin, Moscarelli, Musayev, Norwood, Preisig, Pugliatti, Rehm, Salvador-Carulla, Schlehofer, Simon, Steinhausen, Stovner, Vallat, Van den Bergh, van Os, Vos, Xu, Wittchen, Jonsson, Olesen and Group2011) contributed a substantial proportion of the estimates for societal cost per patient (9.7%). Because the two studies applied uniform costing rules (and thus, were not truly independent observations), we undertook post-hoc analyses by describing the distribution of estimates with these two multi-site studies excluded. None of the other included studies had estimates for societal cost per patient for the disorder group intellectual disabilities or a combination of disorder groups. In general, the cost distributions shifted to the right and were more costly in this subset of estimates (eTable 6 in Online Resource 2). Schizophrenia was still associated with the highest median societal cost per patient (34 588 USD PPP) and eating disorders was still the least costly according to median societal cost (859 USD PPP). The cost distributions of this subset can be found in eFigs 6 and 7 in Online Resource 3.
Reporting quality of included studies
The median quality reporting score for the included studies was 7 (based on the standardised 10-point scale). Scores by study and item are available in eTable 7 in Online Resource 2. Most studies contained information about the study objectives and key cost-related items. In contrast, the items most often omitted were reports related to the handling of missing data and sensitivity analysis (only 20 and 28% of studies, respectively, reported these items). When we examined the distribution of the estimates for studies in the top half ranked by quality reporting score, there was little change in the overall pattern of findings. The descriptive analysis is presented in eTable 8 in Online Resource 2, with the associated plots in eFigs 8–10 in Online Resource 3.
Discussion
We found 143 cost-of-illness studies that covered 48 countries and many types of mental disorders. The majority of these studies used a prevalence-based approach in accordance with the previous literature (Drummond, Reference Drummond1992), but they varied widely by study perspective, cost categories, time period and reporting quality.
In line with earlier systematic reviews which focused on single mental disorders (Luppa et al., Reference Luppa, Heinrich, Angermeyer, Konig and Riedel-Heller2007; Fajutrao et al., Reference Fajutrao, Locklear, Priaulx and Heyes2009; Konnopka et al., Reference Konnopka, Leichsenring, Leibing and Konig2009; Stuhldreher et al., Reference Stuhldreher, Konnopka, Wild, Herzog, Zipfel, Lowe and Konig2012; Chong et al., Reference Chong, Teoh, Wu, Kotirum, Chiou and Chaiyakunapruk2016; Jin and Mosweu, Reference Jin and Mosweu2017), our systematic review confirmed that mental disorders constitute a substantial economic burden for societies and, additionally, that there was between-disorder variation in societal cost per patient. As expected, when examined by disorder and by country, overall patterns emerge, which are underpinned by many independent estimates. For example, in eFig. 5, we see that the distribution is underpinned by several hundred estimates (i.e. the distribution is ‘information rich’). These plots together with the summary statistics provide weight to the hypothesis that certain groups of mental disorders are more costly than others and that these rankings are relatively persistent between countries.
While only based on two studies, we note that the top median societal cost per patient (PPP adjusted) were developmental disorders (which includes autism spectrum disorders), followed by schizophrenia and intellectual disabilities. However, it is important to note that while disorders such as mood, neurotic and substance use disorders were less costly according to societal cost per patient, these disorders are much more prevalent and thus would contribute substantially to the total national cost in a country, as found in economic studies estimating the national burden of mental disorders in European countries (Gustavsson et al., Reference Gustavsson, Svensson, Jacobi, Allgulander, Alonso, Beghi, Dodel, Ekman, Faravelli, Fratiglioni, Gannon, Jones, Jennum, Jordanova, Jonsson, Karampampa, Knapp, Kobelt, Kurth, Lieb, Linde, Ljungcrantz, Maercker, Melin, Moscarelli, Musayev, Norwood, Preisig, Pugliatti, Rehm, Salvador-Carulla, Schlehofer, Simon, Steinhausen, Stovner, Vallat, Van den Bergh, van Os, Vos, Xu, Wittchen, Jonsson, Olesen and Group2011) and in China (Xu et al., Reference Xu, Wang, Wimo and Qiu2016). Our analysis examining the percentages between direct and indirect cost of the total societal cost per patient showed that almost half of the total cost was driven by indirect cost related to morbidity and mortality and thereby not direct resource consumption. Previous studies also showed that at least half of the total cost was related to indirect cost (Luppa et al., Reference Luppa, Heinrich, Angermeyer, Konig and Riedel-Heller2007; Chong et al., Reference Chong, Teoh, Wu, Kotirum, Chiou and Chaiyakunapruk2016; Jin and Mosweu, Reference Jin and Mosweu2017). This highlights the need for research to develop more cost-effective interventions related to prevention and treatment to reduce the health loss experienced and the premature mortality among people with mental disorders to reduce their economic burden in a society.
Our systematic review revealed gaps in the empirical literature – there were relatively few studies examining the economic cost associated with intellectual disabilities, eating disorders, personality disorders and developmental disorders. Worryingly, there is a lack of studies from low- and middle-income countries which affected our ability to make a comprehensive overview of the economic burden worldwide. Furthermore, there is a need for future economic studies to improve how they report their studies. For example, we found that the majority of the included studies did not report crucial information (e.g. whether sensitivity analyses were done). Previous systematic reviews of the cost-of-illness in mental disorder have also commented on this issue (Fajutrao et al., Reference Fajutrao, Locklear, Priaulx and Heyes2009; Stuhldreher et al., Reference Stuhldreher, Konnopka, Wild, Herzog, Zipfel, Lowe and Konig2012).
This review has been restricted to cost-of-illness studies, which have been criticised for not providing an adequate picture of a disease on a macroeconomic level and for not giving a meaningful or desirable alternative scenario (Department of Health Systems Financing Health Systems and Services: World Health Organization, 2009). They value an individual's life in terms of the individual's production to society and ignore other dimensions that might be more valued by the individual – and they do not traditionally give value to people outside the workforce. In addition, the studies seldom include future economic impacts such as changed demographic composition and increased labour productivity or increased health care consumption as a result of the individuals' growth in health (Department of Health Systems Financing Health Systems and Services: World Health Organization, 2009).
Our systematic review has several additional limitations. First, despite our rigorous search strategy, we cannot rule out that some relevant publications were not identified and included in our study. Another limitation has been the lack of standardisation for cost-of-illness studies and with that substantial heterogeneity in methodology, perspective, cost categories and health care system. This has restricted the types of cross-study comparisons that could be made in the systematic review. We have tried to accommodate this by only comparing studies according to societal cost per patient, but there were still variations in the studies' level of detail. Additionally, our analyses adjusted by PPP facilitated between-country comparisons, but this type of cost estimate does not reflect the actual spending within a country. Last, this review excluded papers with comorbidity between mental disorders and general medical conditions. How comorbidity affects the economic burden for the investigated mental disorders is therefore out of scope for this systematic review. However, comorbidity within mental disorders is pervasive (Plana-Ripoll et al., Reference Plana-Ripoll, Pedersen, Holtz, Benros, Dalsgaard, de Jonge, Fan, Degenhardt, Ganna, Greve, Gunn, Iburg, Kessing, Lee, Lim, Mors, Nordentoft, Prior, Roest, Saha, Schork, Scott, Scott, Stedman, Sorensen, Werge, Whiteford, Laursen, Agerbo, Kessler, Mortensen and McGrath2019) and people with mental disorders also have an increased risk for general medical conditions (Momen et al., Reference Momen, Plana-Ripoll, Agerbo, Benros, Børglum, Christensen, Dalsgaard, Degenhardt, de Jonge, Debost, Fenger-Grøn, Gunn, Iburg, Kessing, Kessler, Laursen, Lim, Mors, Mortensen, Musliner, Nordentoft, Pedersen, Petersen, Ribe, Roest, Saha, Schork, Scott, Sievert, Sørensen, Stedman, Vestergaard, Vilhjalmsson, Werge, Weye, Whiteford, Prior and McGrath2020). Future cost-of-illness studies should explore both the cost of mental disorders and the additional cost of comorbid medical conditions. This paper has focused on cost-of-illness studies and has explored the economic burden for mental disorders worldwide. Cost-of-illness studies do not include information about the benefits produced from the resources used and cannot be used to prioritise the scarce resources in societies. Consequently, future research should conduct cost-effectiveness or cost-benefit analyses to investigate where the money is best spent within each country.
In conclusion, our systematic review has identified many high-quality studies on the cost of mental disorders, and we confirm that mental disorders are costly for societies worldwide. The median cost varies by mental disorder type and also varies between countries. We believe that this review provides a solid evidence-base to inform health planners and funding agencies about the societal cost of mental disorders. We hope that our study can help guide policy-makers and yield more research into evidence-based allocation of health funds to reduce the cost of mental disorders on our society.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S204579602000075X
Availability of data and materials
Data used in the systematic review are available online: https://nbepi.com/econ
Acknowledgements
Thanks to Dr Dan Chisholm for his insightful comments on this manuscript and to Dr Carson Sievert for developing the interactive website.
Author contributions
Dr McGrath and Christensen had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: McGrath, Christensen, Plana-Ripoll, Iburg. Acquisition, analysis or interpretation of data: McGrath, Christensen, Lim, Saha, Cannon, Presley, Plana-Ripoll. Drafting of the manuscript: Christensen, McGrath, Plana-Ripoll, Iburg. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Christensen, Plana-Ripoll, McGrath. Obtained funding: McGrath. Administrative, technical or material support: Lim, Saha, Cannon, Presley. Supervision: McGrath, Plana-Ripoll, Iburg.
Financial support
The project is supported by the Danish National Research Foundation (Niels Bohr Professorship to John McGrath). John McGrath is employed by The Queensland Centre for Mental Health Research which receives core funding from the Queensland Health. Oleguer Plana-Ripoll has received funding from the European Union's Horizon 2020 research and innovation programme under the Marie Sklodowska-Curie grant agreement No 837180.
Role of the funder/sponsor
The funding sources had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The manuscript does not contain clinical studies or patient data.





