Bipolar disorder is a serious mental illness frequently associated with several unfavourable outcomes during the progression of illness, such as functional decline and cognitive impairment.Reference Sajatovic, Strejilevich, Gildengers, Dols, Al Jurdi and Forester1 In addition, robust evidence suggests that patients with bipolar disorder also have a two to four times higher mortality rate and at least a 10-year reduction in life expectancy compared to individuals in the general population.Reference Crump, Sundquist, Winkleby and Sundquist2 In particular, cardiovascular and cerebrovascular diseases are among the leading causes of premature deaths in patients with bipolar disorder.Reference Crump, Sundquist, Winkleby and Sundquist2, Reference Tsai, Lee, Kuo and Chen3 To date, the literature suggests that cardio-metabolic adverse effects of psychotropic drugs are one of the possible risk factors for the elevated mortality from cerebrovascular diseases in patients with bipolar disorder.Reference Correll, Detraux, De Lepeleire and De Hert4 For the treatment of bipolar affective symptoms, mood stabilisers, antipsychotic drugs and antidepressants are among the standard medications across several treatment guidelines. Although there are still conflicting data on the association of the risk of stroke and psychotropic medications, a recent systemic review and large-scale meta-analysis suggest that antipsychotics and antidepressants generally increase the risk of coronary heart disease and stroke.Reference Correll, Detraux, De Lepeleire and De Hert4 In contrast, the literature on the mood stabiliser–related cerebrovascular outcomes is currently inconsistent and limited. A recent population-based retrospective cohort study found that lithium use was significantly related to a reduced risk of stroke in patients with bipolar disorder.Reference Lan, Liu, Lin, Lan, McInnis and Chan5 However, another recent retrospective chart review did not find a significant association between lithium therapy and the risk of stroke.Reference Prosser and Fieve6 Despite the evidence that there are associations between the risk of stroke and use of anticonvulsants such as carbamazepine in populations with epileptic disorder,Reference Olesen, Abildstrom, Erdal, Gislason, Weeke and Andersson7, Reference Chuang, Chuang, Lin, Chang, Lu and Chang8 data on the risk of stroke following exposure to valproic acid, carbamazepine and lamotrigine specific to patients with bipolar disorder is still lacking. This knowledge gap and safety concerns merit evidence-based research on whether the use of mood stabilisers is more likely to increase the risk of stroke in patients with bipolar disorder. In this study, we aimed to investigate the association between acute exposure to mood stabilisers and risk of stroke in a large cohort of patients with bipolar disorder derived from a nationwide, population-based insurance claims database. In addition, we explored the effects of combination therapy of mood stabilisers and antipsychotic drugs on the risk of stroke. A case–crossover study design was applied to reveal the acute exposure effects of mood stabilisers on the incidence of stroke. The design of case–crossover study has the advantage that the study participants serve as their own controls and can remove the effects of unmeasured time-invariant confounders. We hypothesised that acute exposure to mood stabilisers increased the risk of stroke in patients with bipolar disorder.
Method
Data sources
The data sources were derived from the Taiwan National Health Insurance Research Database (NHIRD). In Taiwan, National Health Insurance was implemented in 1995 and covers 98% of the 23 000 000 Taiwanese population. The NHIRD contains registration files and medical claim data, which enable researchers to follow-up on the medical services of beneficiaries longitudinally. The Psychiatric Inpatient Medical Claims (PIMC) database of NHIRD includes patients whose admitting diagnostic codes range from ICD-9 codes 290 to 319 between 1 January 1996 and 31 December 2012 (n = 256 880).9 Each year, the National Health Insurance Bureau randomly reviews the medical records to verify the diagnoses. To date, this database has been used for research purposes and has been the source for numerous epidemiological and clinical studies published in peer-reviewed journals. The Institutional Review Board of Taipei City Hospital approved the protocol for this study, with a waiver of informed consent because of the deidentified and retrospective nature of the data (study ethical approval number: TCHIRB-10510110-E).
Bipolar cohort
We first selected a cohort of patients from the PIMC database who were 15–65 years of age and had at least one psychiatric admission for a bipolar disorder (ICD-9 codes: 296.0–296.16, 296.4–296.81 or 296.89) between 1 January 1999 and 31 December 2012, but no psychiatric admission between 1 January 1996 and 31 December 1998, to enrol patients who had their first incident of bipolar disorder requiring admission to psychiatric hospital (n = 20 094) (Supplementary Figure 1, available at https://doi.org/10.1192/bjp.2018.203). Next, we excluded the patients who were diagnosed with stroke (ICD-9-CM codes 430.x–436.x) before the first psychiatric admission (n = 19 433). Through broadly searching all the claims data between 1 January 1999 and 31 December 2012, we finally identified 609 patients with an incident stroke (the index stroke) after the first psychiatric admission for bipolar disorder.
Case–crossover study
This study aimed to examine the association between the time-variant exposures to mood stabilisers and the risk of an acute stroke in patients with bipolar disorder within a short period. The case–crossover design is a standard method for assessing the effects of brief exposures on acute outcomes.Reference Wu, Wang, Gau, Tsai and Cheng10 With this study design, each participant serves as his or her own control. Potential factors during the 14-day window (1–14 days) before the stroke event, as detailed in a previous study,Reference Wu, Wang, Gau, Tsai and Cheng10 were compared with four individual 14-day control periods (every 13 weeks: 92–105 days, 183–196 days, 274–287 and 365–378 days before the stroke).
Exposure measurement of mood stabilisers
We obtained the data on the use of mood stabilisers from the prescription files of the NHIRD. The mood stabilisers included lithium, valproic acid, carbamazepine and lamotrigine, which are among the standard medications for the treatment of bipolar disorder. To estimate the dose effect of specific mood stabilisers on the risk of stroke, we calculated the defined daily dose for each mood stabiliser based on the dose information obtained from the Anatomic Therapeutic Chemical Classification System.11
Potential confounders
Sociodemographic and clinical characteristics were retrieved from the NHIRD, including age, gender, stroke type, Charlson Comorbidity Index score at the first psychiatric admission and number of psychiatric admissions within 1 year before the index stroke.Reference Charlson, Pompei, Ales and MacKenzie12 Potential confounders selected for adjustment in the analysis included the number of admissions to psychiatric hospital within 1 year before the index stroke, physical illnesses and concomitant medications. The potential factors comprised physical illnesses including hypertension, non-hypertensive cardiovascular diseases, hyperlipidaemia, diabetes mellitus, chronic kidney diseases, chronic obstructive pulmonary disease, chronic hepatic disease and cancer. Concomitant drugs included cardiovascular drugs, drugs used in diabetes, antithrombotic agents, respiratory drugs, corticosteroids, antipsychotics, antidepressants and benzodiazepines. These factors were selected because of their potential association with the risk of stroke.Reference Chen, Chen, Liu, Wu, Yang and Pan13
Statistical analyses
We conducted a two-step, multivariate, conditional logistic regression analysis. In the first step, we explored physical illnesses and concomitant drugs as the potential risk factors for stroke (Table 2). We conducted the multivariate regression based on the strategy of backward variable selection. The identified variables with a significant association (P < 0.05) were retained in the final model. In the second step, the identified risk factors in the first step as covariates, we conducted the multiple regression analyses to estimate the exposure effect of specific mood stabilisers on the risk of stroke.
Subgroup analyses were conducted to investigate the exposure effects of specific mood stabilisers on the various types of stroke, including ischaemic, haemorrhagic and other forms of stroke. We assessed the duration and the cumulative defined daily dose of each mood stabiliser on the risk of all-cause stroke and its subtypes, respectively. Furthermore, we examined the combined sets of specific mood stabilisers and the first- and second-generation antipsychotics on the risk of stroke. All statistical analyses were conducted with SAS statistical software (SAS for Windows, version 9.4; SAS Institute, Cary, NC). P-values <0.05 were considered significant.
Results
Characteristics of the patients and controls
The study cohort included 19 433 patients with bipolar disorder, and 609 of them had incident stroke after the first psychiatric admission for bipolar disorder between 1 January 1999 and 31 December 2012. Therefore, the annual incidence of stroke was 54.8 cases per 10 000 person-years (95% CI, 41.6–69.9, based on the Poisson distribution). Among the 609 patients with incident stroke, 61.1% had their first psychiatric admission after 45 years of age (Table 1) and 69.2% had the first stroke after 45 years of age. The most common type of stroke was ischaemic (48.3%), followed by haemorrhagic (26.4%) and others (25.3%). Most of the patients (87.2%) had a Charlson Comorbidity Index score <3 at the first psychiatric admission. More than half of the patients (59.3%) did not have admission to psychiatric hospital within 1 year before the stroke.
Table 1 Demographic and clinical characteristics of 609 patients with bipolar disorder and incident stroke, 1999–2012
Factors associated with incident stroke
Multivariate conditional logistic regression analyses revealed that several factors exhibited a significantly higher risk of stroke, including cardiovascular disease (except hypertension) (adjusted risk ratio, 1.82; P < 0.001), respiratory drugs (adjusted risk ratio, 1.47; P < 0.001), antipsychotic medications (adjusted risk ratio, 1.35; P = 0.006) and long-acting benzodiazepines (adjusted risk ratio, 1.45; P < 0.001) (Table 2).
Table 2 Association between the risk of stroke and physical illnesses and concomitant drugs within the 14-day case period in patients with bipolar disorder and first-time stroke
a. Estimated by univariate conditional logistic regression.
b. Estimated by multivariate conditional logistic regression. We conducted the multivariate regression based on the strategy of backward variable selection. The variables with a significant association (P < 0.05) were retained in the final model.
* P < 0.05, **P < 0.001.
Mood stabilisers on the risk of stroke
In the conditional logistic regression analysis, mood stabilisers as a group were significantly associated with the risk of stroke in patients with bipolar disorder (adjusted risk ratio, 1.26; P = 0.041) (Table 3). Among the individual mood stabilisers, exposure to carbamazepine was associated with the highest risk of stroke (adjusted risk ratio, 1.68; P = 0.018). Subgroup analysis of the effects of individual mood stabilisers on the various types of stroke showed that carbamazepine increased the risk of ischaemic stroke (adjusted risk ratio, 1.81; P = 0.037), and valproic acid increased the risk of haemorrhagic stroke (adjusted risk ratio, 1.76; P = 0.022). In contrast, there was no association between the exposure to lithium and lamotrigine and the risk of any type of stroke.
Table 3 Association between the risk of stroke and the use of mood stabilisers within the 14-day case period in patients with bipolar disorder and first-time stroke
a. Estimated using multivariate conditional logistic regression. Adjusted for the risk factors crystallised in Table 2.
* P < 0.05, **P < 0.001.
We further analysed the dose-dependent relationship between the exposure of mood stabilisers and risk of stroke. Within the 14-day period before the index stroke, carbamazepine showed a positive correlation between cumulative duration of use and the risk of stroke (adjusted risk ratio, 1.06; P = 0.035) (Supplementary Table 1). Subgroup analyses of the dose-dependent effect on the various types of stroke again revealed that there was a positive correlation between cumulative duration of carbamazepine use and the risk of other types of stroke (adjusted risk ratio, 1.15; P = 0.047). On the contrary, the associations between the cumulative exposure of valproic acid, lithium and lamotrigine and the risk of stroke were not significant.
Effect of combination therapy of mood stabilisers and antipsychotics on the risk of stroke
Considering that antipsychotic medications also increased the risk of stroke in the analyses (Supplementary Table 2), we evaluated the effect of the combination therapy of mood stabilisers and antipsychotic drugs on the risk of stroke. The findings regarding the combination therapy of each mood stabiliser and first- or second-generation antipsychotics on the risk of stroke are provided in Supplementary Tables 3 and 4. The findings showed that the combination therapy of carbamazepine and first-generation antipsychotics significantly increased the risk of all stroke (adjusted risk ratio, 2.09; P = 0.035) and ischaemic stroke (adjusted risk ratio, 3.70; P = 0.016) (Fig. 1).
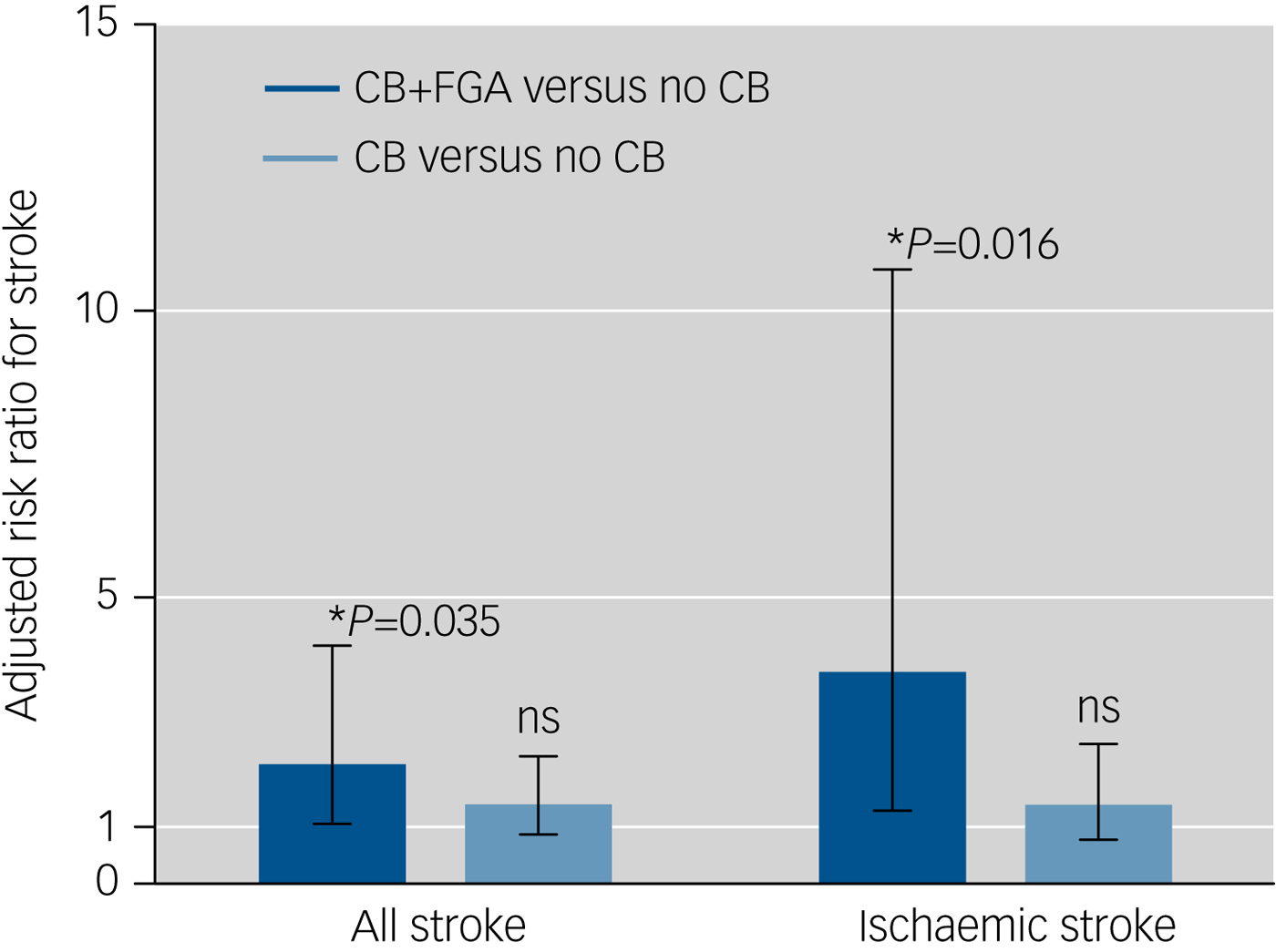
Fig. 1 Association between the risk of stroke and the combination therapy of carbamazepine and any first-generation antipsychotic drug within the 14-day case period in in-patients with bipolar disorder and first-time stroke (non-carbamazepine users as the reference group). Error bars show 95% CI of the adjusted risk ratio. Estimated by multivariate regression, *P < 0.05. Adjusted for the risk factors identified in Table 2. CB, carbamazepine; CB+FGA, patients using carbamazepine combined with any first-generation antipsychotics; FGA, first-generation antipsychotics; ns, not significant.
Discussion
Main findings
To the best of our knowledge, this is the first nationwide, population-based case–crossover study exploring the association between acute exposure of mood stabilisers and the risk of stroke in patients with bipolar disorder. In this study, the annual incidence of stroke was 54.8 cases per 10 000 person-years in the patients with bipolar disorder. Previously, a Taiwanese study of the general population suggested that the annual incidence of first stroke was 21.3 per 10 000 person-years for people aged 36–64 years.Reference Hu, Sheng, Chu, Lan and Chiang14 Therefore, our findings are in line with the literature indicating that patients with bipolar disorder actually have a two times higher risk of stroke as compared to the general population.Reference Crump, Sundquist, Winkleby and Sundquist2
Acute exposure of mood stabilisers and the risk of stroke
We found that acute exposure to mood stabilisers induced a 1.26-times higher risk of stroke in patients with bipolar disorder than no exposure. This result is consistent with the findings of a prior retrospective cohort study that suggested a 1.54-times higher risk of stroke in patients with bipolar disorder receiving mood stabilisers.Reference Lan, Liu, Lin, Lan, McInnis and Chan5 We further assessed the effect of individual mood stabilisers on the risk of various types of stroke in the present study. Among the anticonvulsant-type mood stabilisers (carbamazepine, valproic acid and lamotrigine), we found that acute use of carbamazepine significantly elevated the risk of stroke (adjusted risk ratio, 1.68), especially the ischaemic type (adjusted risk ratio, 1.81). Acute use of valproic acid only increased the risk of haemorrhagic stroke (adjusted risk ratio, 1.76). In addition, there was no association between acute exposure of lamotrigine and the risk of stroke. These findings are similar to those of previous studies of patients with epileptic disorders, which showed that use of carbamazepine carried a significantly higher risk of stroke compared with the use of valproic acid and lamotrigine.Reference Olesen, Abildstrom, Erdal, Gislason, Weeke and Andersson7, Reference Chuang, Chuang, Lin, Chang, Lu and Chang8 In a study of patients with epileptic disorders,Reference Olesen, Abildstrom, Erdal, Gislason, Weeke and Andersson7 valproate was found to be associated with a decreased risk of stroke compared with carbamazepine (adjusted hazard ratio, 0.86; 95% CI, 0.76–0.96). In another study,Reference Chuang, Chuang, Lin, Chang, Lu and Chang8 compared with patients with epileptic disorders who received carbamazepine, those who received lamotrigine had lower levels of circulatory markers for cerebrovascular diseases, such as total cholesterol, total homocysteine and folate.
We found that the use of carbamazepine and valproic acid increased the risk of ischaemic and haemorrhagic strokes, respectively. The observed differences in the risk of distinct types of stroke following the use of carbamazepine and valproic acid may be because of their pharmacokinetic properties. Studies have shown that carbamazepine is a liver cytochrome p450 enzyme inducer, which can contribute to the elevated levels of several atherogenesis risk markers such as total cholesterol, C-reactive protein, homocysteine and carotid intima-media thickness.Reference Lopinto-Khoury and Mintzer15 The elevation of these atherogenesis markers can further increase the risk of ischaemic stroke.Reference Lorenz, Polak, Kavousi, Mathiesen, Volzke and Tuomainen16, Reference Miao and Liao17 On the other hand, the mechanisms underlying the association between the enzyme inhibitor valproic acid and the risk of stroke could be distinct from those seen with enzyme induction. For example, valproic acid can affect procoagulatory and anticoagulatory factors.Reference Chen, Xu, Luo, Yu, Li and Cui18, Reference Nanau and Neuman19 Therefore, valproic acid monotherapy could be a risk factor for hypocoagulation and haemorrhagic stroke.
Importantly, our finding that lithium did not elevate the risk of stroke in patients with bipolar disorder is in line with previous clinical reports.Reference Lan, Liu, Lin, Lan, McInnis and Chan5, Reference Prosser and Fieve6 In prior animal studies, lithium was demonstrated to inhibit the expression of vascular cell adhesion molecule-1,Reference Choi, Jang, Kang, Jung, Han and Kim20 infiltration of macrophages into the atherosclerotic plaqueReference Choi, Jang, Kang, Jung, Han and Kim20 and proliferation and migration of vascular smooth muscle cells.Reference Wang, Zhang, Chen, Wang, Wu and Liang21 These mechanisms are proposed to contribute to the protective effects of lithium against cerebrovascular diseases. Currently, treatment guidelines for bipolar disorder recommend that lithium is the first-line mood stabiliser used for both the acute and maintenance treatment. In particular, Lan et al Reference Lan, Liu, Lin, Lan, McInnis and Chan5 found that the long-term use of lithium reduced the risk of stroke in patients with bipolar disorder. In comparison, our data reveal that the acute use of lithium did not increase the risk of stroke. These findings suggest that lithium may be a reasonable treatment choice for both the acute and maintenance phases of bipolar disorder, particularly in those patients who are at high risk of cerebrovascular diseases.
In the subgroup analyses, we found that there was a positive association between cumulative duration of carbamazepine use and the risk of stroke within the 14-day period before the index stroke (adjusted risk ratio, 1.06). This finding may suggest a dose-dependent relationship between acute exposure to carbamazepine and the risk of stroke in patients with bipolar disorder. However, the association between the cumulative dose of carbamazepine use and the risk of stroke was not significant. One of the possible explanations for this inconsistency may be the relatively small sample size in the carbamazepine group within the 14-day exposure window before the stroke. Therefore, further studies with an adequate sample size are suggested to explore the dose-dependent relationship between acute exposure to carbamazepine and the risk of stroke in patients with bipolar disorder.
Combination therapy and the risk of stroke
No previous research has focused on the association between the risk of stroke and the combination therapy of mood stabilisers and antipsychotic drugs in patients with bipolar disorder. Our study showed that the combination therapy of carbamazepine and first-generation of antipsychotics significantly increased the risk of stroke, particularly ischaemic stroke. A previous study had found that first-generation antipsychotics elevated the risk of stroke.Reference Sacchetti, Trifiro, Caputi, Turrina, Spina and Cricelli22 The mechanisms involved may change the effects of platelet aggregation.Reference Zornberg and Jick23 With the consideration that carbamazepine is a liver cytochrome p450 enzyme inducer,Reference Janicak24 the use of carbamazepine would result in lower levels of antipsychotic medications and, therefore, be more likely to decrease the risk of stroke. The pharmacokinetic interaction of carbamazepine and first-generation antipsychotics consequently contradicts the synergic effects of these two drugs for the elevated risk of stroke observed in this study. Given that the distinct receptor profiles of antipsychotic medications can contribute to the different level of stroke risk,Reference Charlson, Pompei, Ales and MacKenzie13, Reference Sacchetti, Trifiro, Caputi, Turrina, Spina and Cricelli22 further research with detailed differentiation of prescribed antipsychotic medications is needed to validate our observations.
Limitations
Several limitations of this study should be addressed when we interpret the results. First, we could not measure the severity of bipolar affective symptoms in the NHIRD. Considering that previous studies have found that the mood burden in bipolar disorder can increase the risk of vascular risk,Reference Fiedorowicz, Solomon, Endicott, Leon, Li and Rice25, Reference Chen, Chang, Chiang, Lin, Tsai and Huang26 further research is needed to explore whether bipolar affective symptoms responding to treatment with mood stabilisers could modulate the risk of stroke.
Second, claims data from before 1 January 1996 was unavailable in the PIMC database. Therefore, we cannot obtain the information regarding the mood episodes occurring much earlier in patients' lives. Although we excluded those patients who had at least a psychiatric admission between 1 January 1996 and 31 December 1998 for defining the study participants, this study could include patients with late-onset bipolar disorder or with chronic course of the illness. The association between mood stabilisers and risk of stroke observed in this study deserves to be validated in the future research by utilising the sample of new-onset bipolar disorder.
Third, this study could possibly exist prescription bias that patients with specific clinical characteristics may influence the choice of a specific mood stabiliser. Patients who received lithium treatment might have fewer manic or depressive episodes and be with good adherence to stroke-preventive medications, such as antihypertensive and anticoagulation drugs. On the other hand, patients who received carbamazepine treatment could be with chaotic course of illness and therefore be more prone to stroke. The case–crossover design in this study means that the prescription bias may be diminished because the study participants served as their own controls and the effects of unmeasured time-invariant confounders were removed. However, further research is needed to clarify the assignment of a specific mood stabiliser as a confounder on the estimation of the association between the specific mood stabiliser and risk of stroke.
Fourth, age is clearly a well-known risk factor for stroke, but this study did not illustrate its interaction with drug effect because of the design of case–crossover study in which the age of each participant was almost the same in the case and control windows. Nevertheless, the issue regarding the potential interaction of age with the association between mood stabilisers and stroke deserves future studies with the larger sample size of incident cases and the stratification analysis by age groups.
Fifth, an unhealthy lifestyle, such as physical inactivity, cigarette smoking and alcohol consumption, has been found to be a contributor to high vascular burden in patients with bipolar disorder.Reference Ward, White and Druss27 Such variables were not available in NHIRD. With these considerations in mind, we used a self-controlled study design to adjust for such unmeasured variables.
In conclusion, this study found that the risk of stroke varied among the different types of mood stabilisers used for the first-line treatment of bipolar affective symptoms. Among the individual mood stabilisers, acute use of carbamazepine appeared to carry the highest risk of stroke, followed by valproic acid. In contrast, lithium and lamotrigine did not increase the risk of stroke. These findings may offer a guide for the choice of mood stabilisers in patients with bipolar disorder who require acute therapy for affective symptoms and who already have the risk factors for stroke.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2018.203.
Funding
This research was supported by grants from the National Science Council, Taiwan (MOST 105-2314-B-532-006-MY3) and Taipei City Hospital (10501-62-015; TPECH 106-77). Neither of the funding sources had any role in conducting the research, analysing the data or writing this report.
Acknowledgment
We thank Yin Chi Chen, BS (Department of General Psychiatry, Taipei City Psychiatric Center, Taipei City Hospital) for data management and help with the statistical analyses. Ms. Chen declares that she has no competing interests.







eLetters
No eLetters have been published for this article.