Introduction
In many sports, the incidence of sport-related concussions increases from early to late adolescence.Reference Tsushima, Siu, Ahn, Chang and Murata1 Macpherson et alReference Macpherson, Fridman, Scolnik, Corallo and Guttmann2 showed that in children and youth 1–18 years of age in Ontario, Canada, there was a linear increase in concussion-related visits to emergency departments and primary physicians’ offices for appropriate diagnostic codes from 2003 to 2010 and that hockey and skating were the most frequent causes of sport-related concussions. In hockey, the most frequent mechanisms of concussions are bodychecking and other collisions in youth age 12–18,Reference Kontos, Elbin and Sufrinko3 and in professionals, player-to-opponent contact caused 88% of concussions.Reference Hutchison, Comper, Meeuwisse and Echemendia4 Bodychecking was banned in women’s hockey worldwide in 1990 by the International Ice Hockey Federation, and in Canada, this ban was adopted in all levels of women’s hockey. In male hockey in Canada, due to parental concern about concussion and other injuries noncontact leagues have developed which disallow bodychecking at any age. However, the majority of leagues within Hockey Canada, amateur hockey’s main organization in Canada, permit bodychecking in boys’ hockey beginning at age 13, and these leagues have higher concussion rates.Reference Cusimano, Taback and McFaull5–Reference Macpherson, Rothman and Howard8 However, in the leagues permitting bodychecking, there is uncertainty about the permissible age for bodychecking. Indeed, it was parental concern that led to raising the permitted age to age 13 in 2013 where it has remained.9,10 There have been several reports about bodychecking in youth hockey from pediatric organizations in Canada and the USA with some support for raising the permissible age for bodychecking.Reference Brooks and Loud11 The changes in attitude about bodychecking were also informed by data showing differences in concussion incidence in boy’s hockey between Canadian provinces related to the permissible age for bodychecking.Reference Emery, Kang and Shrier12 However, at this time, age 13–14 is still the permitted age for bodychecking in the leading hockey organizations in Canada and the USA.
Although several studies have documented the incidence of acute concussions in hockey related to player age and bodychecking, there have been no longitudinal studies assessing the long-term consequences of bodychecking in concussed youth hockey players with persisting concussion symptoms (PCS) also known as post-concussion syndrome, the most common long-term consequence of concussion. Our center has focused on long-term consequences of sport concussions by obtaining follow-up through return clinic visits and questionnaires.Reference Schwab, Wennberg, Grenier, Tartaglia, Tator and Hazrati13–Reference Tator, Davis and Dufort17 The purpose of the present study of youth hockey was to assess the mechanisms of concussion, the incidence and duration of PCS due to bodychecking and other mechanisms in a consecutive case series of youth hockey players in order to inform prevention strategies. Youth hockey is an important sport in North America because of the number of players, and the safer it is, the more enjoyable it will be for participants and the greater likelihood that parents will endorse it.
Methods
The concussion center at the Toronto Western Hospital began in 1995 with a name change in 2015 from the Canadian Sports Concussion Project to the Canadian Concussion Centre (CCC). From inception, we have been a referral center for concussion care and research with a focus on injury prevention, diagnosis, and long-term management of concussion consequences, such as PCS and chronic traumatic encephalopathy (CTE). The present study is a consecutive cohort series of 87 youth ice hockey players ages 10-18 who sustained concussions in the years 1997–2017: 1997–2000, n = 8; 2000–2010, n = 29; and 2011–2017, n = 50. All patients were referred to one of the co-authors (CHT) with a special interest in sports-related concussions. During this time, the clinic treated approximately 800 patients with sports and non-sports concussions. Follow-up clinic visits were in-person or virtual, and follow-up also included periodic, mailed questionnaires to assess longitudinal recovery. In the absence of reliable biofluid or imaging biomarkers for concussion or PCS, the diagnoses of concussion and PCS were based on the symptoms and signs recorded at the initial and follow-up visits. The definition of concussion with PCS used in the present study is one or more symptoms lasting a minimum of one month after concussion which is consistent with the 5th International Consensus Conferences of the Concussion in Sport Group last held in 2016.Reference McCrory, Meeuwisse and Dvorak18 This definition of PCS was used in our recently developed MRI criteria for PCS,Reference Panwar, Hsu, Tator and Mikulis19 and all PCS patients with MRI in the present study conform to these MRI criteria.
Data about the mechanisms and symptoms of concussion were obtained from patient self-report often assisted by reports from team coaches, physicians, parents, and siblings. A collision was defined as a collision of players which was not an intentional check whereas hits other than body checking denote an intentional contact with another player that was not a bodycheck according to the players and any additional reports from parents, coaches, and other witnesses as available. Follow-up time was the time elapsed between the date of the index concussion defined as the concussion that led to the initial referral to our center and the date of the most recent follow-up visit or returned questionnaire if PCS was still present. Players who had complete recovery are listed in Table 3, and the date a player reported complete recovery at a clinic visit or by questionnaire was used to calculate the duration of symptoms.
Imaging by CT or MRI was obtained in 64.4% of the players, and those with evidence of trauma more severe than concussion, including cerebral contusion, intracerebral bleed, intracranial hematoma, or diffuse axonal injury were excluded from the study according to our published criteria.Reference Panwar, Hsu, Tator and Mikulis19
Continuous variables were summarized as mean and standard deviation or medians and interquartile ranges (IQRs) and compared with two-sample t test or Kruskal-Wallis rank sum test, as appropriate. Categorical variables were summarized as number and percentage and compared using the Fisher exact test. Statistical analyses were performed using R version 4.0.3, and descriptive statistics were performed using the “tableone package.”
This research was approved by the Research Ethics Board of the University Health Network.
The CCC has had an Advisory Board since its inception involved in planning research and clinical activity. The Board is composed of lay persons including several with lived experience of concussion in sports and recreation and other mechanisms. The Board is involved in organizing an Annual Public Forum at which research studies including the present study are planned, presented, and discussed.
Results
Patient Characteristics and Follow-up Times
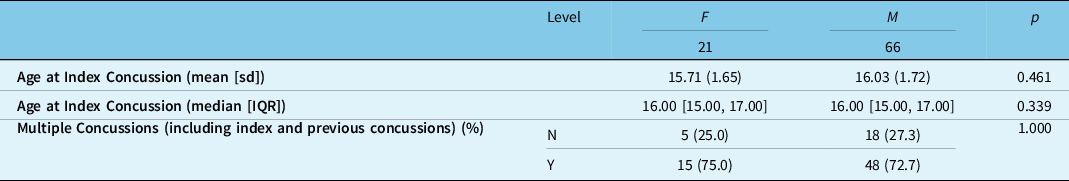
Table 1 shows that 87 players were included in the study, ages 10–18, 66 males and 21 females, with mean age 15.95 years ± 1.69, median age of 16, and no significant difference between median age of girls and boys. The mean and median number of total clinic visits and questionnaires was 2 and 2.3, respectively, with a range of 1-6. The mean and median follow-up time from index concussion to most recent follow-up by visit or questionnaire was 34.8 months and 24 months, respectively. At the time of entrance to the study, 66 (75.9%) had sustained multiple concussions and 20 (23.0%) had sustained a single concussion with 1 unknown.
Table 1: Demographic characteristics of the 87 concussed hockey players, ages 10-18
Mechanisms and Features of the Index Concussion
Table 2 shows that in the 87 players, the index concussion occurred by bodycheck in 34 (39.1%) which was the highest single cause of concussion in this case series. Eleven of the bodychecks were in open ice, 21 were against the boards, and 2 were in unknown locations. In the remaining 53 players, the mechanisms were falls (5), fighting (4), collisions (11), multiple mechanisms (4), struck by objects such as sticks or pucks (9), elbow to the head (9), hits other than bodychecking (8), and unknown in 3.
Table 2: Bodycheck vs. other mechanisms of the index concussion in players with concussion

Table 3: Comparison of body check vs other mechanisms in patients with concussion
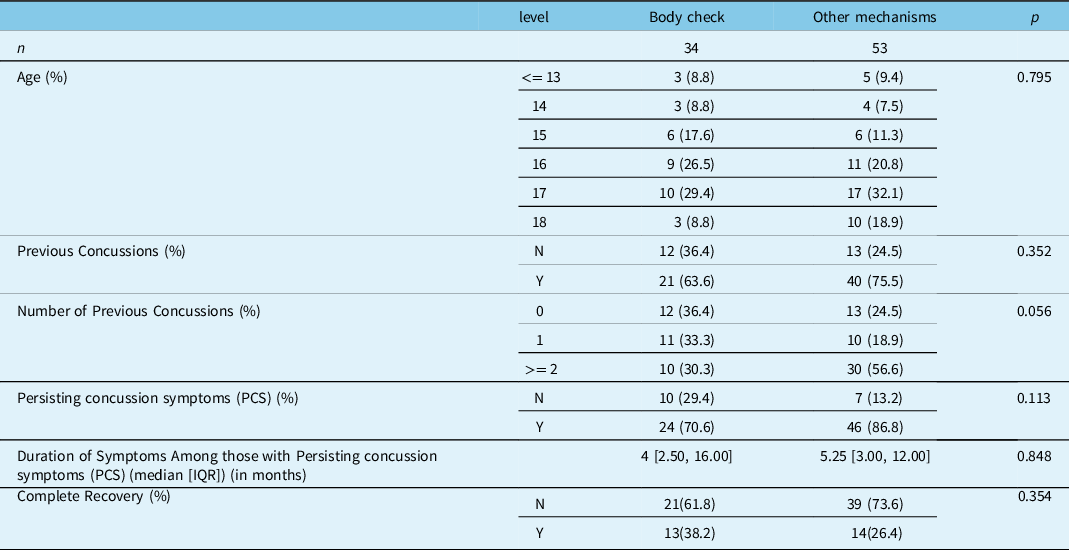
Persisting concussion symptoms (PCS) are defined as a minimum of one persisting symptom for a minimum of 1 month.
Complete recovery was determined at the last follow-up visit or questionnaire.
Concussion plus PCS in Relation to the Mechanism of Concussion, the Number of Previous Concussions, and the Sex of the Players
Table 3 indicates PCS occurred in 70 (80.4%) of the 87 of concussed players. PCS occurred in 24 of the 34 (70.6%) patients concussed by bodychecking, and in 46 of the 53 (86.8%) patients with concussions due to other mechanisms (p = 0.113). Table 3 also shows that 27 (31.0%) of the 87 players had complete recovery at the follow-up times shown in Table 1: in the bodycheck group, 13 (38.2%) of 34 had complete recovery, and in the other mechanisms group, 14 (26.4%) of 39 had complete recovery.
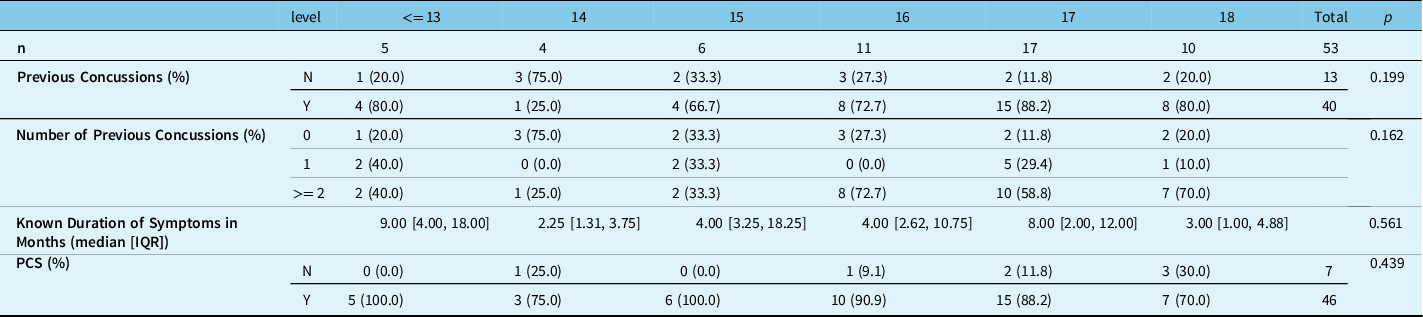
Table 4 shows there were more PCS cases in males than females but similar duration of PCS in both sexes. Tables 5 and 6 show the large number of players in all age groups with previous concussions, and the longer duration of PCS in months after concussions due to bodychecking compared with concussions from other mechanisms.
Table 4: Comparison of PCS among males and females at different ages
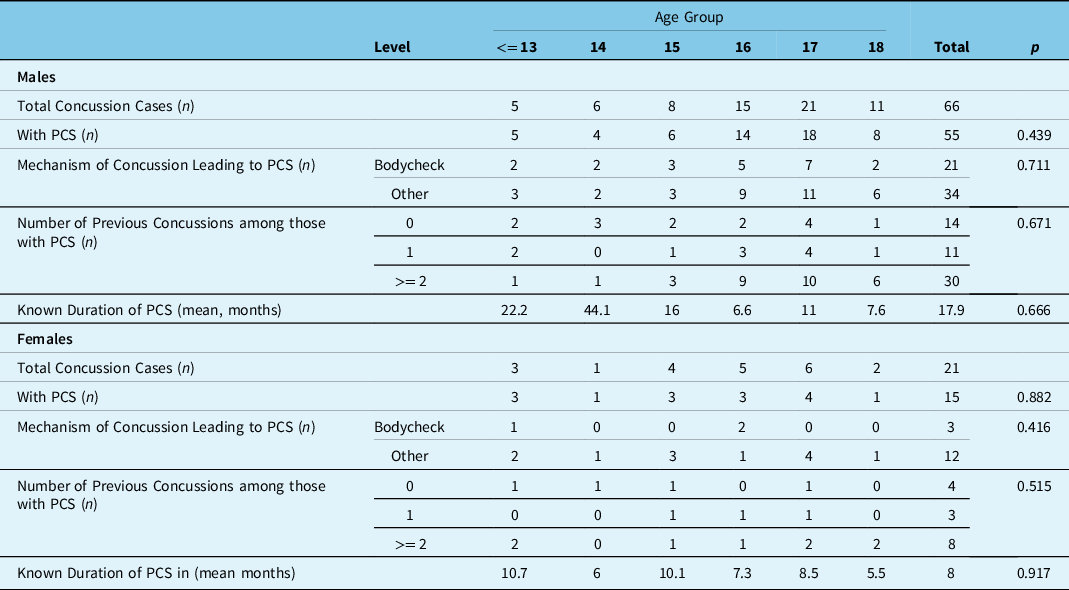
Table 5: Comparison of different ages in the 34 players with concussion caused by bodycheck
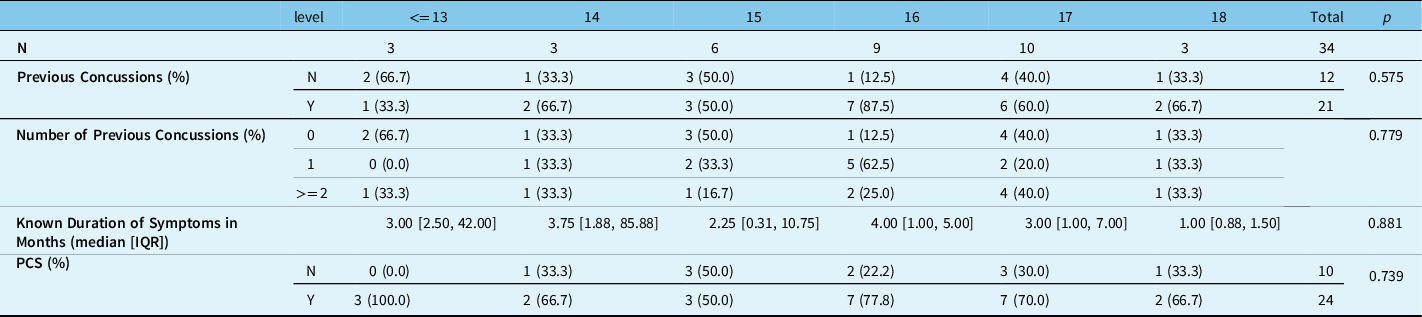
Table 6: Comparison of different ages in the 53 players with concussion caused by mechanisms other than bodycheck
Age of Permitted Bodychecking and potential for reduction of Concussion and PCS in relation to the Permitted Age of Bodychecking
Table 7 shows the projected relationship between the age of permitted bodychecking and the potential reduction in cases of concussion with PCS that would have occurred in each age group as the permitted age increases.
Table 7: Potential reduction in the incidence of concussion and months of suffering from PCS in 20 males as the permitted age for bodychecking increases from 13 to 18
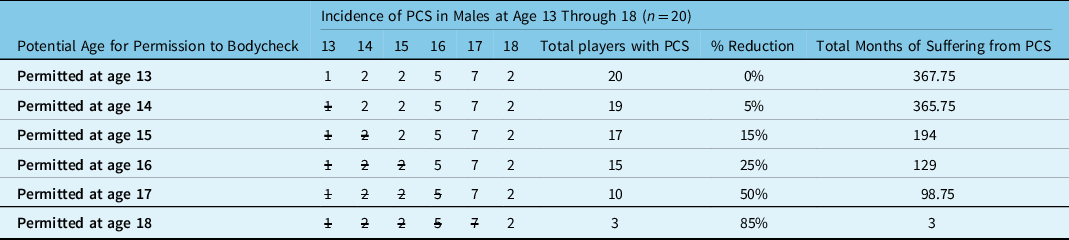
Note: Numbers without a slash indicate the number of concussions that would have occurred at various permitted ages for bodychecking, and the numbers with a slash indicate the eliminated concussions at various permitted ages for bodychecking. For example, if bodychecking was permitted at age 18, only 3 players in the present series of 20 would have suffered a concussion plus PCS, a reduction of 85%, and a reduction in the months of suffering PCS by 99%.
Discussion
Hockey is a great game for youth and Canada’s national game. Hockey provides excellent physical exercise, camaraderie, and teaches youth how to be team members and ideally should engender a sense of responsibility for their own health and well-being and also that of team members and opponents. However, injuries may occur, and thus, there is a long history of efforts to prevent neurotrauma in hockey and other team collision sports.Reference Tator20 Initially, hockey injury prevention programs were directed towards spinal cord injury and were ultimately successful after a combination of educational programsReference Cook, Cusimano, Tator and Chipman21 and rules changes including specific penalties against checking from behind.Reference Tator, Provvidenza and Cassidy22 Although there is one study of professional hockey players forced to retire because of multiple concussions and PCS,Reference Hiploylee, Wennberg and Tator15 to our knowledge, the present study is the first longitudinal study of youth ice hockey players with long-term data on the consequences of concussion. The study by Brooks et al23 in youth hockey players with persisting symptoms from concussion did not include the mechanism of the concussions and was cross-sectional and not longitudinal. Kriz et alReference Kriz, Stein and Kent24 reported hockey concussions in 145 youth players seen in three hospital-based outpatient sports concussion clinics in Massachusetts and Rhode Island and commented that symptoms from hockey concussions lasted an average of 44.5 days, longer than other sports, but the mechanism of the hockey concussions was not reported and long-term follow-up data was less than one year. There are several other studies of the incidence of concussions due to bodychecking in youth hockey. Emery et al 2011Reference Emery, Kang and Shrier12 measured the differences in concussion incidence due to bodychecking in youth hockey in Alberta and Quebec but did not measure long-term persistence of symptoms, although “severe concussions” were defined as causing “more than 10 days time loss from hockey.” In another report, Black et alReference Black, Macpherson and Hagel25 also studied concussions in youth hockey players with “severe concussions” with symptoms lasting at least 10 days, but long-term data were not collected. Many of these studies were valuable for injury prevention purposes because they provided evidence for the value of raising the permitted age for bodychecking to age 13–14-year-old players,Reference Black, Hagel, Palacios-Derflingher, Schneider and Emery26 but none of these had long-term data for PCS due to bodychecking. Emery et alReference Emery, Eliason and Warriyar27 studied 15–17-year-old hockey players in bodychecking versus non-bodychecking leagues in three cities in Canada and showed a much lower incidence of concussions in non-bodychecking cities, but there was no long-term follow-up recovery data.
There are many reasons for the lack of long-term, longitudinal cohort studies in youth with concussion plus PCS. For example, we studied 23 brain-injured ice hockey players of median age 19 almost all of whom had concussions, and in 15 players, we found non-compliance with respect to advice that had been given to never return to play.Reference Ackery, Provvidenza and Tator28 It is of interest that 15 (65%) had residual symptoms for at least two years, but the mechanism of the concussions was not recorded. We attributed their non-compliance to eagerness to return to play. However, this study also found reluctance to return for clinic visits or to complete follow-up questionnaires. It is likely that similar reasons account for the absence of cohort studies of players with concussion and PCS among youth ice hockey players. Another reason is that these young hockey players often change teams and locations, especially those wishing to pursue college or professional play, and also, they may be reluctant to admit the occurrence of concussion and persistence of symptoms.
The importance of longitudinal studies of concussion and PCS is that such studies help to detect and treat the early and long-term consequences of concussion including mental health issues of anxiety, depression and PTSD, cognitive decline, and catastrophic conditions such as the second impact syndrome which lead to Rowan’s Concussion Law.Reference Tator, Starkes, Dolansky, Quet, Michaud and Vassilyadi29,Reference Tator, Starkes, Dolansky, Quet, Michaud and Vassilyadi30 Indeed, one of the first documented cases of this syndrome was in a 16-year-old Canadian ice hockey player who died in 1968 after a bodycheck and a witness at the inquest reported seeing “the deceased fall and hit the back of his head on the ice four days before the fatal accident” with brief loss of consciousness.Reference Fekete31
Another important reason for long-term studies of concussion with PCS is the development in athletes of CTE, the rare neurodegenerative disorder that can develop after a long interval of several years after concussions. It is suspected that concussion with PCS is an antecedent condition to CTE as in the case of Steve Montador, a professional ice hockey player whose case history and pathological findings were documented by our Centre, and whose life story was the subject of a book by Ken Dryden.Reference Dryden32 Indeed, the CCC has recently reported the presence of CTE in several other hockey players.Reference Schwab, Wennberg, Grenier, Tartaglia, Tator and Hazrati13
The lack of longitudinal studies and the reasons for the failure to report the long-term effects of concussion due to bodychecking are surprising since there have been major efforts in youth hockey to document concussions due to bodychecking in Canada, the USA, and Europe, as indicated above. It is interesting to note that a recent study in the USA of 600 concussed pediatric patients mostly concussed in sports had a one-year follow-up obtained by similar methodology to the present study which utilized a combination of clinic visits and mailed questionnaires, but there was no data on individual sports.Reference Rosenbaum, Locandro and Chrisman33
Bodychecking has been one of the most frequently studied causes of concussions in youth hockey and has been the subject of many papers with respect to injury prevention. The present authors have emphasized bodychecking because it was so readily identifiable, very frequent, and very damaging to the players included in this report. Indeed, although bodychecking was recognized in women’s hockey in the 1990s as injurious behavior and banned in all age groups in womens’ hockey, men’s hockey, especially boys’ hockey has lagged in effective measures. We have added new data to emphasize the need for further injury prevention measures against bodychecking in boys’ hockey. However, it is important to note that bodychecking represented less than half of all the cases with PCS and that additional attention to other prevention measures is needed to address the other readily identifiable causes of concussion and PCS such as elbowing to the head and fighting (Table 2). Also, the continuing toll of the hockey boards identified in the present study (Table 2) emphasizes the need for hockey organizations to move toward international size rinks. The boards in small rinks are a risk factor for head impacts and likely concussions as identified by Wennberg.Reference Wennberg34,Reference Wennberg35
In the present study, PCS occurred in 70 (80.4%) of the 87 concussed youth players including 24 of the 34 (70.6%) patients concussed by bodychecking. The potential severity of this condition is emphasized by one of our cases who remained symptomatic for 14 years (168 months). Most of the bodycheck cases were boys: only 3 of 21 girls had concussion from a bodycheck (Table 4).
The present study showed that bodychecking was the most frequent single cause of concussion with PCS among our case series of youth ice hockey players and accounted for 39.1% of the concussions with PCS. Thus, from a prevention standpoint the study calls attention to the adequacy of prevention strategies with respect to bodychecking. As noted above, women’s hockey eliminated bodychecking in 1991 via the International Ice Hockey Federation, and then subsequently bodychecking was eliminated for all ages in girls’ hockey. The beneficial effect of this prevention strategy is apparent in the present study with only 3 of the 15 or 20% of concussions with PCS in girls being due to bodycheck whereas in boys 21 of the 55 cases or 38% (p = 0.19) were due to bodychecking (Table 4). Further evidence about the importance of bodychecking as a cause of concussion comes from leagues which disallow bodychecking at all ages and show a lower incidence of concussion than leagues which allow bodychecking.Reference Emery, Palacios-Derflingher and Black36 In boys, the increased registration numbers in noncontact leagues are due largely to the concern about bodychecking causing concussion, and it is highly likely that additional strategies to prevent bodychecking as a cause of concussion in boys would be welcomed by hockey families because of the high toll identified in the present study. Another important injury prevention aspect is the finding that 21 of the 34 bodychecked concussed players were bodychecked into the boards (Table 2) which may call for additional prevention measures against this injurious behavior in youth hockey.
Surprisingly, there did not appear to be a greater likelihood of developing PCS among those with multiple concussions which confirmed our previous finding that the number of previous concussions sustained in sports and recreation did not increase the duration of PCS.Reference Tator and Davis16 Indeed, most of the concussed patients in our present and previous studies had persisting symptoms after a single concussionReference Hiploylee, Dufort and Davis14 which emphasizes the importance of preventing even a single concussion.
It is noteworthy that all concussed players in the present study were helmeted which reflects the fact that helmets have never been proven to prevent concussions in hockeyReference Daneshvar, Baugh, Nowinski, McKee, Stern and Cantu37 or other collision sports including American or Canadian football.Reference Daneshvar, Nowinski, McKee and Cantu38 The present study also shows that helmets do not prevent PCS. Helmets, full face shields, and mouthguards are mandatory in many youth ice hockey leagues, to prevent more severe brain injuries such as intracranial and intracerebral blood clots, and likely dental injuries and facial fractures, but not concussion.23
Rules against bodychecking among 13–14-year-old non-elite ice hockey players reduced the number of concussions in youth hockey.Reference Emery, Palacios-Derflingher and Black36 In 2012, the Canadian Paediatric SocietyReference Houghton39 recommended delaying bodychecking until age 13–14 which rule is currently in force by Hockey Canada. In 2014, an American pediatric society suggested delaying the introduction of checking until age 15, although this does not appear to have been enacted by this group or by USA Hockey.Reference Brooks and Loud11
In the present study, concussion with PCS caused by bodychecking occurred in all age groups: 83% of players in the 13–14-year-old category, and 69.2% in the 17–18-year-old category suffered from PCS, although the number of players in each category was small (Table 5). Concussions resulting from other mechanisms also occurred in all age groups. Indeed, the age-related data on the incidence of concussion with PCS in the present study highlights the importance of delaying the age at which bodychecking is allowed in order to prevent concussion with PCS in hockey.
There is a common misconception that introducing bodychecking at an early age can help prevent injuries such as concussion by ensuring that children are skilled in how to withstand a bodycheck, when in fact there is no data to support this.Reference Marchie and Cusimano40 Emery and Meeuwisse were the first to flag that player age is an important factor in the incidence of concussion. They reported that 13–14-year-old players were at the greatest risk of concussion from bodycheckingReference Emery and Meeuwisse41 and confirmed this in subsequent studies.Reference Emery, Kang and Shrier12,Reference Emery, Palacios-Derflingher and Black36 However, they provided no long-term data about the duration of symptoms. Kontos et alReference Kontos, Elbin and Sufrinko3 found that the 12–14 age group had a higher incidence of concussion based on athletic exposures compared with 15–18-year-old players and attributed this to 12–14-year-old boys having a greater weight and height discrepancy than 15–18-year-old boys. In the 13–15 age group, boys can differ in height and weight by as much as 55 cm and 53 kg, respectively.Reference Brust, Leonard, Pheley and Roberts42 No long-term follow-up data was provided about the duration of symptoms.
The present study indicates that additional prevention measures could reduce concussions due to bodychecking in boys’ hockey. Table 7 demonstrates the potential value of raising the permitted age for youth bodychecking, assuming compliance with the rule. If hockey is made safer more parents will allow their children and youth to play. Table 7 shows that raising the permitted age of bodychecking in boys’ hockey to 17 from the current age of 13-14 could potentially reduce cases of concussion by 56% and reduce the number of days of suffering by 73.1%. It is important to note that there is recent evidence that increasing the permitted age of bodychecking would not increase the risk to players who then entered leagues in which bodychecking was permitted.Reference Eliason, Hagel and Palacios-Derflingher43 A permitted age of 18 would provide another sizeable reduction of cases by 88% and decrease in months of suffering from 368 to 3 months. Indeed, our studies of PCS show the seriousness of this condition because many sufferers never fully recover.Reference Hiploylee, Dufort and Davis14
We agree with Emery and BlackReference Emery and Black44 that in high-impact sports like hockey and football rule changes may have the greatest potential population health effect in reducing the risk of concussion in sport. In our view, the effect of concussion education is also of major importance as has been demonstrated in hockey by Cook et al.Reference Cook, Cusimano, Tator and Chipman21
Opponents to an age change for permissible bodychecking might also raise concern that the transition to college/university and professional hockey would be changed by raising the permissible bodychecking age to age 18, but we would argue that the health of the players is of paramount importance, and that at age 18 learning how to give or receive a bodycheck would be quickly acquired. Players who aspire for a hockey scholarship or career could enter contact leagues at that age.
Concussion plus PCS in hockey is not just a complication of youth hockey but occurs in adult hockey as well including at the professional level, where brain injury is also a major problem causing disability, financial loss, and canceled careers. We documented the toll of concussion with PCS in 35 National Hockey League players all of whom suffered career-ending concussion with PCS from 1995 to 2015 with costs to their teams and insurers of $135.5M USD.Reference Hiploylee, Wennberg and Tator15 It should be noted that in the NHL 88% of concussions are caused by player-opponent collisions, a major cause of which is bodychecking, and thus, rules about bodychecking in professional leagues should also be amended to reduce concussion and career-ending PCS and the later possibility of CTE, as in the case of Steve Montador.Reference Dryden32
Limitations
Given the biased case accrual pattern of our Concussion Centre, the data presented are not generalizable. For example, from the present long-term case series study it is not possible to determine what the annual reduction in concussion with PCS would be in the United States or Canada from raising the age of permissible bodychecking to age 18. Another limitation is that evidence about the mechanism of concussion was based on the narrative descriptions obtained from the players and their families, although often corroborated by witnesses, and thus is subject to recall bias. More accuracy in recording the mechanism of concussion might be available in the future such as the use of video replay to more accurately examine the etiology of hockey concussion as shown by Hutchison et al.Reference Hutchison, Comper, Meeuwisse and Echemendia4,Reference Hutchison, Comper, Meeuwisse and Echemendia45 Also, many patients continued to experience PCS after their last clinic visit or returned questionnaire, and thus, our recorded duration of PCS is an underestimate in youths who were still symptomatic at last visit or questionnaire.
Conclusions
Bodychecking is a frequent cause of concussion with PCS among male youth hockey players some of whom will have persisting symptoms for months to years. Greater attention should be given to preventing these injuries. Youth hockey leagues should raise the age of permissible bodychecking to 18 from the current age of 13-14. We show the potential to prevent 85% of bodycheck caused concussions by raising the permissible bodychecking age from its current age of 13-14 to 18 years of age. There is also the potential to eliminate years of suffering from bodycheck-induced PCS. Practitioners should consider advising youth hockey players and their parents/guardians to join noncontact leagues, especially players with previous concussions. This study also points to several other injury prevention measures for reducing the toll of concussions and PCS by efforts to stop fighting and elbowing to the head and checking into the boards, the latter of which could be reduced by increasing rink size to international hockey standards.
Acknowledgments
Several research assistants at the CCC assisted with data collection for this study including Connor Moore and Emma Prentice. Mozhgan Khodadadi, Research Manager at the Centre also assisted with data collection. All phases of this study were supported by funding from the University Health Network Foundation. The University Health Network Foundation had no role in the design and conduct of the study.
Conflict of Interest
The authors have no conflicts of interest.
Statement of Authorship
Charles H. Tator conceived and organized the study, examined all the patients, recorded all their findings, and wrote all versions of the manuscript, except the initial version.
Victoria Blanchet extracted the data from the patient’s charts, transferred it to summary sheets, performed the initial data compilations for the tables, wrote the first draft of the manuscript, and edited all subsequent versions.
Jin Ma performed the statistical analyses, worked on the tables, and edited all subsequent versions of the manuscript after the first version.









