Gender minority adults (those with an identity that differs from their assigned sex at birth) are more likely than cisgender adults (those with an identity that corresponds to sex assigned at birth) to report symptoms of depression and anxiety and to self-harm and attempt suicide.Reference Reisner, Biello, Hughto, Kuhns, Mayer and Garofalo1,Reference Vance, Boyer, Glidden and Sevelius2 The few studies on the mental health of gender minority adolescents have used convenience sampling, which might introduce sampling bias; have been small and so might lack statistical power; or did not match cisgender comparators, preventing the estimation of differences by gender identity.Reference Veale, Peter, Travers and Saewyc3–Reference Connolly, Zervos, Barone, Johnson and Joseph5 In the one nationally representative study in New Zealand, symptoms of depression, anxiety, self-harm and suicide attempts were elevated in gender minority compared with cisgender adolescents;Reference Clark, Lucassen, Bullen, Denny, Fleming and Robinson6 however, the study did not examine the role of substance use or victimisation in these associations. Two US studiesReference Johns, Lowry, Andrzejewski, Barrios, Demissie and McManus4,Reference Reisner, Greytak, Parsons and Ybarra7 found that transgender young people reported more smoking, alcohol and illicit drug use as well as more victimisation than their cisgender peers, suggesting that these variables may have a role in the association between gender minority status and mental health.
The UK's Millennium Cohort Study (MCS), with its assessments of psychological distress, emotional and behavioural difficulties, self-harm and suicide attempts, as well as reports of substance use and victimisation ranging from insults to sexual assaults, in a nationally representative sample represents a unique opportunity to explore the association between gender identity and mental health.
Method
Setting and participants
The MCS is a birth cohort in the UK following children born in 2000–2002. In total, 19 519 children were recruited and have been followed up seven times to date at ages 9 months and 3, 5, 7, 11, 14 and 17 years. For information regarding the design of the MCS, see https://cls.ucl.ac.uk/cls-studies/millennium-cohort-study/.
We used data gathered at 9 months and 3 years of age on assigned sex. The outcomes and covariates in the analysis were assessed at 17 years of age (2018–2019), except ethnicity, which was only reported by young people at 14 years of age. In the sweep when cohort members were 17 years of age, 14 496 families were invited to participate. Of this number, 10 625 (73.2%) families and 10 345 (71.4%) adolescents provided informed written consent and were interviewed.
Ethics approval for the age-17 sweep was obtained from the National Research Ethics Service Research Ethics Committee North East – York (ref: 17/NE/0341). Collected data are anonymised and available to researchers via the UK Data Service. We adhered to the Strengthening the Reporting of Observational studies in Epidemiology guidelines in this work.Reference von Elm, Altman, Egger, Pocock, Gøtzsche and Vandenbroucke8
Measures
Mental health outcomes
Participants responded to the validated K6 measure of psychological distress.Reference Kessler, Green, Gruber, Sampson, Bromet and Cuitan9 This measure asks respondents how often in the past 30 days they felt, for instance, worthless, with five response options ranging from none to all of the time. Total scores range from 0 to 24, with higher scores indicating greater distress.
Parent/carers and young people completed the Strengths and Difficulties Questionnaire (SDQ),Reference Goodman10 a validated screening tool to measure child and adolescent behavioural and emotional difficulties.Reference Goodman and Goodman11 The SDQ consists of four subscales that rate areas of behavioural and emotional difficulties (conduct problems, hyperactivity, emotional symptoms and peer problems), with each consisting of five items on a three-point scale. Individual item scores were summed to produce a continuous total score.
Self-harm was reported as a binary response (never harmed = 0; harmed = 1) to the question ‘During the last year, have you hurt yourself on purpose in any of the following ways?’, with separate questions for the methods of: cut or stabbed; burned, bruised or pinched; overdose; pulled out hair; and other. This question has not been validated, but our analyses focused on self-harm in the previous year as this is more clinically relevant and less prone to recall bias than self-harm occurring more than a year ago.Reference Kidger, Heron, Lewis, Evans and Gunnell12
Attempted suicide was reported with the question ‘Have you ever hurt yourself on purpose in an attempt to end your life?’. This question has not been validated. We derived a binary measure of lifetime suicide attempt from responses (never attempted suicide = 0; made a suicide attempt = 1).
Gender identity
Gender identity was assessed using self-reports from participants at 17 years of age with the question ‘Which of the following describes how you think of yourself?’ and the response options of: ‘male’, ‘female’ and ‘in another way’. Those selecting ‘in another way’ then provided a description that was coded into: ‘androgenous (male and female)’, ‘gender fluid’, ‘non-binary’ and ‘other.’ We also compared the gender identification provided by young people at 17 years with the sex provided by parent/carers when they were 9 months and 3 years of age. Parent/ carers at 9 months and 3 years could only report whether a child was male or female. We derived participants’ gender minority status using both parents’ and young people's responses. If young people at 17 years identified with a gender that was: ‘other’, ‘androgenous (male and female)’, ‘gender fluid’ or ‘non-binary’, they were categorised as a gender minority. If the sex reported by the parent/carer at 9 months or 3 years did not match that reported by young people at 17 years of age (e.g. the parent response at 9 months was male and the young person's response at 17 years was female), the participant was also categorised as gender minority.
Preliminary analysis (before imputation) categorised 109 (1.1%) participants as a gender minority. Of these, 58 (53.2%) were categorised in this way based on young people's self-reports. The remaining 51 were categorised by from comparing participants’ reported male or female gender identity at 17 years of age with the gender identity of the participant reported by the parent/carer at 9 months or 3 years of age.
Covariates
To describe the characteristics of gender minority young people compared with their cisgender peers, we analysed self-reported data collected on demographic characteristics including housing tenure (i.e. rented, owned), parent/carer composition in household (single parent or carer, or both parents or carers), responding parent/carer employment status, adolescent's ethnicity (i.e. White; ethnic minorities: mixed, Indian, Bangladeshi or Pakistani, Black or Black British, other ethnic groups) and sexual identity. Sexual identity was adjusted for given the link between gender and sexual identity and associations between sexual identity and mental health. Sexual identity was self-reported according to categories of completely heterosexual/straight, mainly heterosexual/straight, bisexual, mainly gay or lesbian, completely gay or lesbian, other, do not know and prefer not to say. In the unimputed data-set, 0.9% (n = 90) indicated they were mainly gay or lesbian, 1.6% (n = 160) completely gay or lesbian, 10.6% mainly heterosexual (n = 1101) and 6.3% (n = 656) bisexual. There is strong evidence that adolescents identifying as mainly heterosexual or not sure have an increased risk of mental health problems compared with those reporting they are completely heterosexual.Reference Plöderl and Tremblay13,Reference Lucassen, Stasiak, Samra, Frampton and Merry14 To be consistent with this literature, participants reporting they were mainly heterosexual were categorised as bisexual, and those indicating that they were mainly or completely gay or lesbian were collapsed into one category. We assessed two hypothetical mediators of associations between gender minority status and mental health outcomes: substance use and victimisation. Substance use comprised lifetime smoking experimentation (including those who had only had one puff of a cigarette), consumption of a whole alcoholic drink and illicit drug use. Victimisation assessments were self-reports of experience over the past 12 months of nine forms of harassment, abuse and violence.
Statistical analysis
A detailed description of attrition in the cohort has been provided elsewhere.15 Missing data per variable ranged from 2.3 to 12.9%. Participants who reported that they ‘do not know’, ‘prefer not to say’ or ‘do not want to provide’ their gender (n = 47), sexual identity (n = 51) or ethnic identity (n = 56) were removed from the sample. There were 7829 participants with no missing data on the variables used in our statistical models, making up the complete data sample. The imputed analytical sample had 10 247 participants. We assumed missingness was dependent on the observed data and imputed 20 data-sets by multiple imputation using chained equations. The imputation prediction model included all other analysis variables, along with combined sampling and attrition weightsReference Quartagno, Carpenter and Goldstein16 and an indictor variable denoting whether or not participants were the only cohort member in the household. Estimates were obtained by pooling results across 20 imputed data-sets, and the Monte Carlo errors suggested that this was a suitable number.Reference White, Royston and Wood17
The association between gender minority status and outcomes was analysed using multivariable modified Poisson regression with robust errors.Reference Yelland, Salter and Ryan18 Seven separate multivariable modified Poisson regressions were performed for the association between gender minority status and each binary outcome (model 1). Next, we used linear regression to estimate associations between gender minority status and the three continuous measures of reported psychological distress, behavioural and emotional difficulties (adolescent and parent/carer report). We adjusted estimates for sexual identity (model 2). To explore potential mechanisms, we then added to model 2 the hypothetical mediating substance use variables (model 3) and victimisation variables (model 4). Results for the binary outcomes are presented as relative risks (RRs) and continuous outcomes as coefficients, both with 95% confidence intervals. To examine the influence of missing data we re-ran the analysis on a complete data sample. All analyses were performed in Stata version 17.0 (Stata Corp.).
Results
Supplementary Fig. 1 (available at https://doi.org/10.1192/bjo.2023.534) shows how we derived the analytical sample. Of the 10 247 participants, 113 (1.1%) reported they were a gender minority. Table 1 shows the characteristics of young people according to gender minority status. Compared with their cisgender peers, young people who identified as a gender minority were more likely to be bisexual (33.0 v. 17.2%) or gay (28.5 v. 2.2%) or report an ‘other’ sexual identity (30.3% v. 1.1%), and to report all forms of victimisation, including sexual assault (12.2 v. 3.1%), an unwelcome sexual approach (31.0 v. 12.2%), and experience of physical violence (36.9 v. 17.3%), but they were less likely to identify as an ethnic minority (21.3 v. 12.2%). There were no other differences in participant characteristics according to gender minority status.
Table 1 Characteristics of young people by self-reported gender identity
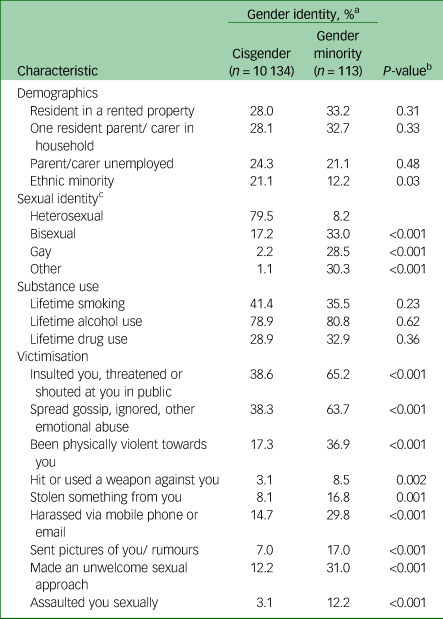
a. All numbers estimated from imputed proportions.
b. Determined by Poisson regression.
c. Bisexual comprised bisexual and mainly heterosexual/straight respondents; gay comprised mainly gay or lesbian and completely gay or lesbian.
Gender minority young people were three times more likely than their cisgender peers to report a suicide attempt (RR 3.42; 95% CI 2.45–4.78) (Table 2). There was evidence of an association of gender minority status with reporting self-harm in the previous year including cutting or stabbing (RR 4.38; 95% CI 3.55–5.40), burning (RR 3.81; 95% CI 2.49–5.82), bruising or pinching (RR 3.69; 95% CI 3.07–4.44), taking an overdose (RR 5.25; 95% CI 3.35–8.23), pulling out hair (RR 3.51; 95% CI 2.52–4.88), and harm in other ways (RR 6.39; 95% CI 4.63–8.83), as well as with scores on the Kessler K6 screening scale (coefficient 5.81; 95% CI 4.87–6.74) and SDQ total scores from study participants’ responses (coefficient 5.60; 95% CI 4.54–6.67) and parent/carers’ responses (coefficient 2.60; 95% CI 1.47–3.73). Associations were markedly reduced after the addition of sexual identity to models, but there was little evidence of further attenuation after substance use was added. After adjustment for reports of victimisation, the associations with gender minority status were weakened (Table 2).
Table 2 Self-reported suicide attempt, self-harm and psychological distress by gender minority status
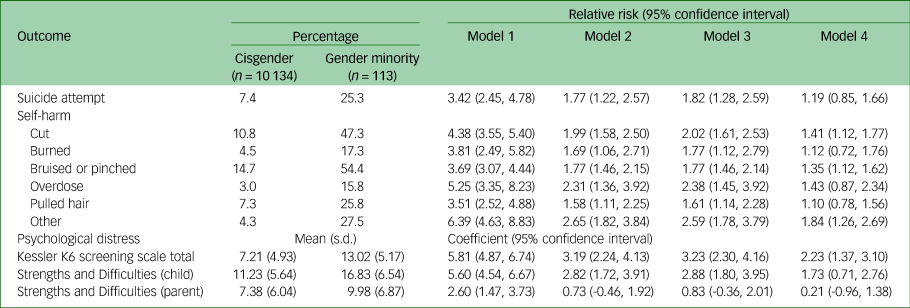
Model 1: gender identity; Model 2: model 1 plus sexual identity; Model 3: model 2 plus substance use; Model 4: model 2 plus victimisation.
In the subset with no missing data, the confidence intervals for estimates overlapped with those from the main results using imputed data (Supplementary Table 1).
Discussion
Main findings
Gender minority adolescents were more likely to report ever making a suicide attempt, self-harm in the previous year, psychological distress, and behavioural and emotional difficulties than their cisgender peers. These associations were markedly reduced after accounting for sexual identity and reports of victimisation, but adjustment for substance use had little impact on the strength on associations. To our knowledge, this is the first study to provide nationally generalisable estimates of inequities in UK adolescents’ mental health according to gender identity and indicate that these differences may be related to exposure to victimisation.
Interpretation of our findings and comparison with existing literature
The prevalence of young people identifying as a gender minority was small (1.2%) and comparable with estimates from community samples of young people in North America (2.1%, n = 65 231;Reference Lipson, Raifman, Abelson and Reisner19 1.9%, n = 908)Reference Almeida, Johnson, Corliss, Molnar and Azrael20 and the findings of the Youth’12 study, the only other nationally representative sample of high-school students conducted in New Zealand (1.2% transgender, n = 8,166).Reference Clark, Lucassen, Bullen, Denny, Fleming and Robinson6 In agreement with the results of that study,Reference Clark, Lucassen, Bullen, Denny, Fleming and Robinson6 we found gender minorities were around three times more likely to report having made a suicide attempt and were three to six times more likely to have self-harmed in the previous year than those who identified as cisgender. In two US studies, the online US Teen Health and Technology StudyReference Johns, Lowry, Andrzejewski, Barrios, Demissie and McManus4 and The Youth Risk Behavior SurveyReference Reisner, Greytak, Parsons and Ybarra7 conducted in ten US states, bullying and victimisation were reported more by transgender than cisgender young people. We replicated the findings of inequalities in mental health and victimisation according to gender identity but explicitly investigated whether victimisation explained associations between gender identity and mental health. Our analysis also extends the results of other studies by assessing six types of self-harm and a continuum of victimisation covering experiences ranging from insults to sexual assaults.
Among the mechanisms linking gender minority status with mental health problems, victimisation is likely to form part of an indirect mechanism. The marked attenuation of the association between gender minority status and outcomes we observed after adjustment for victimisation is consistent with it acting as a mediator. This hypothesis is consistent with the predictions of minority stress theory that mental health problems are more likely in gender minority compared with cisgender youth owing to the added stressors that accompany membership of this stigmatised group.Reference Meyer21,Reference Hendricks and Testa22 Other studies with cisgender comparator groups have found that gender minority adolescents report more victimisation than their cisgender peers,Reference Clark, Lucassen, Bullen, Denny, Fleming and Robinson6,Reference Reisner, Greytak, Parsons and Ybarra7 providing support for this hypothesis. In contrast to previous studies,Reference Johns, Lowry, Andrzejewski, Barrios, Demissie and McManus4,Reference Reisner, Greytak, Parsons and Ybarra7 we found little difference in substance use by gender minority status. If these substances were being used to cope with victimisation, they may be better characterised as a downstream outcome of victimisation than a mediator of the association between gender identity and mental health problems.
Limitations and strengths
One limitation of the present study is that its use of a single combined gender minority group meant that we did not further disaggregate analyses by gender identity (e.g. transmasculine, transfeminine, androgenous, gender fluid or non-binary) and did not include a ‘not sure about gender’ category. A related limitation is that we did not have enough young people to model all combinations of gender and sexual identity. There is likely to be variability in the lived experiences of different gender and sexual minority groups, and larger studies should investigate these differences. Some misclassifications could also have occurred if gender minority identities were underreported because of perceived stigma. This would lead to a misclassification which would probably attenuate associations to the null rather than introduce a spurious effect. Attrition and missing data are a concern in birth cohorts and can introduce selection biases. We used multiple imputation to maximise the plausibility of the missing-at-random assumption. Results were comparable when using the data-sets with no missing and imputed data. Our assessment of suicide attempts was a lifetime measure and so may reflect events that occurred before young people became aware of or identified as a gender minority. However, reverse cause, where a suicide attempt leads to a change in identity, seems a less plausible explanation for the associations reported than gender minority status acting as a putative causal factor.
The main strength of our study lies in the use of a large, contemporary, nationally representative sample of adolescents. Our findings are therefore likely to be generalisable across the UK. The use of a birth cohort with sex recorded by parents at a young age meant we doubled the number of people identified as a gender minority through a comparison of parent/carer reports of gender identity as a child with adolescent reports. This probably increased the power of the analysis and the precision of our estimates. Another strength was the assessment of self-harm that occurred in the past year, which is more clinically relevant and less prone to recall bias than assessments of self-harm occurring more than a year ago.Reference Kidger, Heron, Lewis, Evans and Gunnell12
Implications
In conclusion, we found that gender minority adolescents were more likely to report symptoms of psychological distress, emotional and behavioural difficulties, and self-harm and to have made a suicide attempt than their cisgender peers. We extend the findings from previous studies by showing that adjusting for victimisation explains variation in the association between gender minority status and outcomes. The implication of this finding is that reducing victimisation may be helpful in narrowing the gap in mental health problems between gender minority and cisgender adolescents. The unquestioning acceptance of rigid concepts of gendered behaviour should be challenged by wider society, including young people's families and communities. Clinicians need to consider discussing self-harm and suicide with gender minority young people and help them find safer ways of coping. Policies, organisational practices, and school-based interventions should seek to reduce victimisation of gender minority young people.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2023.534.
Data availability
The MCS data are available to all researchers, free of cost, from the UK Data Service (https://www.ukdataservice.ac.uk).
Acknowledgements
We are grateful for the cooperation of the MCS families who voluntarily participated in the study.
Author contributions
J.W. conceptualised the study, conducted the statistical analysis and wrote the first draft of the manuscript. J.W., C.A.R. and M.-H.T. interpreted the analysis. C.A.R. and M.-H.T. provided critical input into the manuscript.
Funding
The study did not receive any specific funding. The MCS is supported by the Economic and Social Research Council and a consortium of UK Government departments. J.W. was supported by The Centre for the Development and Evaluation of Complex Interventions for Public Health Improvement (DECIPHer), a UKCRC Public Health Research Centre of Excellence. Joint funding was received from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the Welsh Government and the Wellcome Trust, under the auspices of the UK Clinical Research Collaboration and the Welsh Government through Health and Care Research Wales (MR/KO232331/1); the Medical Research Council (MC_UU_00022/1) and the Chief Scientist Office (SPHSU16). The funders had no role in the design or conduct of the study; the collection, management, analysis or interpretation of the data; the preparation, review or approval of the manuscript; or the decision to submit the manuscript for publication.
Declaration of interest
None.






eLetters
No eLetters have been published for this article.