Ever since its conception, ‘schizophrenia’ has been an ‘essentially contested concept’ (Geekie & Read, Reference Geekie and Read2009). Debates at (European) mental health conferences invariably end with around 50% in favour of abandoning the term, and 50% in favour of the status quo. This divide has become the implicit hallmark of academic psychiatry: a science in search of solid data to back up its early 20th century nosological outlook on mental variation. For decades, biological approaches have been tested in an attempt to essentially ‘reverse-engineer’ the hypothesized disease entity, using the classical case–control comparison. However, despite many claims of success (‘genes for schizophrenia’, ‘cognitive illness’, ‘brain disease’), biological findings in psychiatry, whilst fascinating, are fuzzy and unreliable (Ioannidis, Reference Ioannidis2005), and do not suggest categorical distinctions (Kapur et al. Reference Kapur, Phillips and Insel2012).
Schizophrenia represents the 30% poor outcome of a much broader spectrum of psychotic disorders (Perala et al. Reference Perala, Suvisaari, Saarni, Kuoppasalmi, Isometsa, Pirkola, Partonen, Tuulio-Henriksson, Hintikka, Kieseppa, Harkanen, Koskinen and Lonnqvist2007). It is at least 10 times more researched than the other 70% of the clinical psychosis spectrum (van Os, Reference van Os2016) and basically has come to represent everything ‘psychotic’ – even those with subtle experiences of psychosis in the context of anxiety and depression, said to be at ‘Ultra High Risk’ (of schizophrenia) (Van Os & Guloksuz, Reference Van Os and Guloksuz2017).
The question that we – prudently and constructively – attempt to address in this article is: should psychiatry continue to look at human variation through the ‘schizo’-prism, as embedded in major classification systems, or can an alternative case be made that makes more sense, both in clinical practice and in research?
The devolution of the concept of schizophrenia
‘We stand atop a long tradition of clinical descriptive research and ‘authority-based’ diagnostic systems, in which, in the struggle for dominance of psychiatric nosologies, the most famous and articulate professor won.’ (Kendler, Reference Kendler2016b ).
The concept of schizophrenia has – not – evolved since Kraepelin coined the term ‘dementia praecox’ about a century ago. Kraepelin first conceptualized dementia praecox and manic-depressive psychosis as two distinct natural disease entities; Bleuler later introduced the term ‘schizophrenia’ for the first time in his monograph: ‘Dementia Praecox or the Group of Schizophrenias’ (Jablensky, Reference Jablensky2010). Based on his extensive clinical work with patients, Bleuler challenged the gloomy viewpoint of dementia praecox: Progressive deterioration to dementia and early onset were neither exclusive nor uniform to justify a discrete disease category. In contrast to Kraepelin's narrow perspective of dementia praecox, limited to the most severe clinical representation, he adopted a much broader approach that expanded the boundaries of schizophrenia to incorporate a continuum phenotype from latent schizotypy and schizophrenia (Jablensky, Reference Jablensky2010). Early efforts to classifying mental disorders in the USA – largely influenced by the mainstream psychoanalytical formulation – embraced Bleuler's broad and more psychologically-oriented concept of schizophrenia until the release of the third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III) (Andreasen, Reference Andreasen1989). The DSM-III, preceding endeavours to increase the reliability of psychiatric diagnoses in research, e.g. the Research Diagnostic Criteria and Feighner Criteria, introduced a ‘mutated’ Kraepelinian diagnostic practice that was substantially influenced by Langfeldt's poor outcome schizophrenia theory and Schneider's first rank symptoms. One of the main driving forces for the neo-Kraepelinian movement was the disappointment with low reliability hindering collaborative research efforts (Dutta et al. Reference Dutta, Greene, Addington, McKenzie, Phillips and Murray2007). The widespread use of antipsychotics with serious – sometimes irreversible and even life-threatening – side effects also necessitated this narrow diagnostic convention to improve the risk–benefit ratio of antipsychotics by limiting the treatment to the most severe and chronic manifestations of illness (Andreasen, Reference Andreasen1989). This progressive movement – cutting all ties with psychoanalysis and emphasizing the importance of psychiatric nosology akin to European practice – were welcomed across the pond (Murray, Reference Murray1979). However, this revolution in psychiatry, like other radical shifts in history, has subsequently evolved into a dogma per se that ignores all criticisms. Sailing before the wind of biological psychiatry, data of which are applied in attempts to reverse-engineer the narrow concept of schizophrenia, seeded first in the USA, has dominated the field over the last 40 years (Dutta et al. Reference Dutta, Greene, Addington, McKenzie, Phillips and Murray2007).
The outcome bias
‘Schizophrenia is heterogeneous. Some patients with the disorder do well at follow-up and should not, for this alone, be regarded as misdiagnosed.’ (McGlashan, Reference McGlashan1988)
Robins and Guze (pioneers of the DSM-III) concluded: ‘good prognosis “schizophrenia” is not mild schizophrenia, but a different illness’ (Robins & Guze, Reference Robins and Guze1970). However, evidence suggests that the schizophrenia construct is subject to Berkson's bias, which is a specific type of selection bias that occurs when the research sample is limited to help-seeking populations, particularly when the research is carried out at specialized tertiary centres. The restrictive construct of schizophrenia, particularly emphasizing chronicity and deterioration, filters out less severe cases with good prognosis and leads to morbidity concentration (Cohen & Cohen, Reference Cohen and Cohen1984) (Fig. 1). This ‘enriched’ sample of severely ill patients with poor outcome represents only a fraction of the broader phenotype that includes a variety of psychosis spectrum diagnostic categories such as schizophreniform disorder, delusional disorder, brief psychotic disorder and so on (Perala et al. Reference Perala, Suvisaari, Saarni, Kuoppasalmi, Isometsa, Pirkola, Partonen, Tuulio-Henriksson, Hintikka, Kieseppa, Harkanen, Koskinen and Lonnqvist2007). Prospective studies of patients with an initial diagnosis of schizophrenia indicate a vast amount of outcome heterogeneity within and between patients (Harding et al. Reference Harding, Zubin and Strauss1987; Allardyce & van Os, Reference Allardyce, van Os, Gattaz and Busatto2010). Patients with better outcome either never enter, or eventually drop out of mental health care: They either recover and do not necessitate mental health treatment or display a favourable illness course and thus no longer fit into the schizophrenia definition per current classification systems.
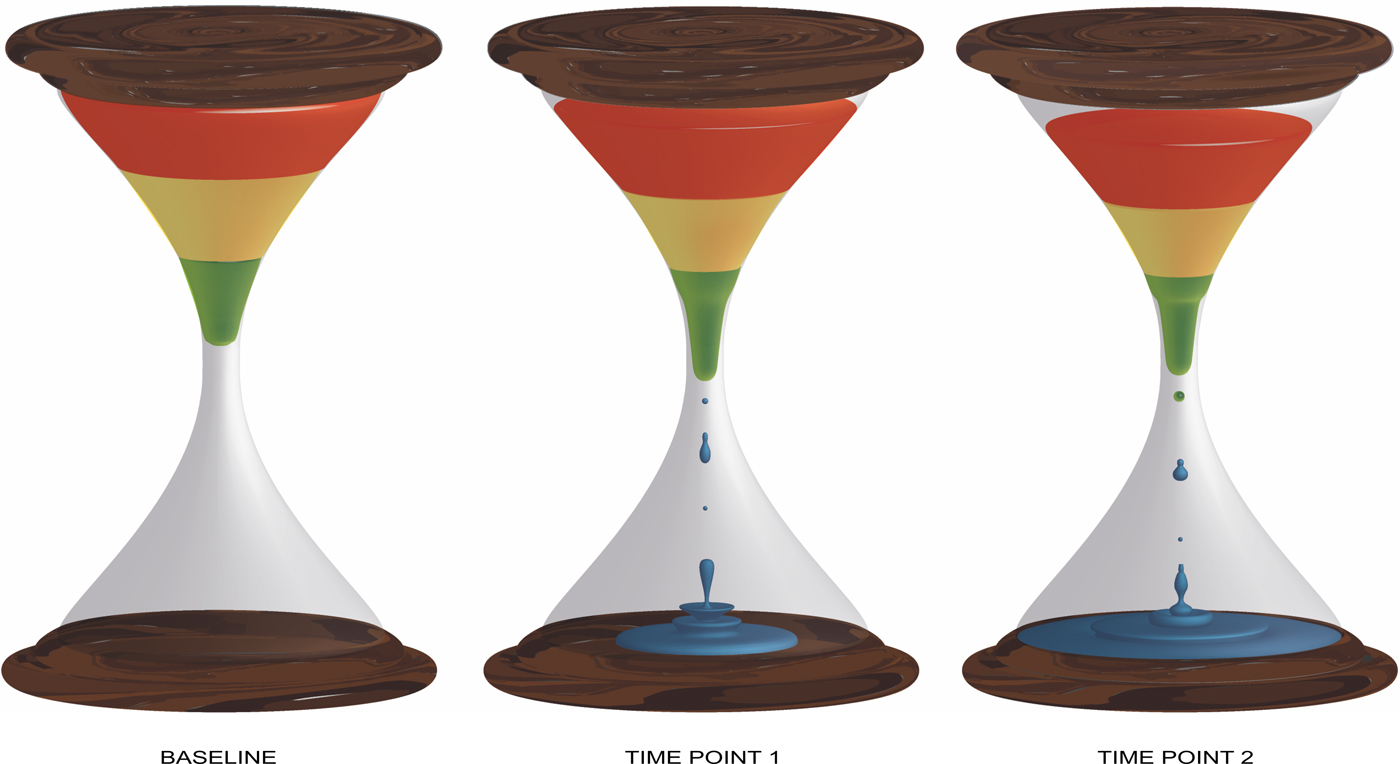
Fig. 1. Depicts the morbidity concentration in an inception cohort of first episode psychosis over a period. The relative balance between poor (red), intermediate (yellow) and favourable outcome (green) shifts towards poor outcome as a fraction of the patients with favourable outcome (green) either recover or no longer meet diagnostic criteria for schizophrenia (blue).
Thus, the biased cluster of diagnosed help-seeking patients shares similarities that are discretely associated with poor outcome but are not necessarily expressed across the whole phenotypic spectrum (van Os et al. Reference van Os, Wright and Murray1997; Zipursky et al. Reference Zipursky, Reilly and Murray2013). Researchers searching for indices of deterioration, akin to Kraepelin's dementia praecox, may have failed to demonstrate such neurodegeneration, but their remarks – albeit within a different context – were accurate: ‘The ‘true’ natural history of an illness cannot be determined from studies in treated populations’ (Waddington et al. Reference Waddington, Scully and Youssef1997).
Considering major advances in mental health care, a linear increase in good outcome would logically be anticipated. However, a meta-analysis of outcome studies of schizophrenia in the last century demonstrated that a biphasic pattern exists, not as a function of improvement in treatment but as a function of diagnostic trends (Hegarty et al. Reference Hegarty, Baldessarini, Tohen, Waternaux and Oepen1994). The steady rising trend in the proportion of patients with a favourable outcome, which saw a remarkable twofold increase to around 50% after the introduction of antipsychotics in the 1950s and 1960s, came to an end after the 1970s when the broad definition of schizophrenia was replaced with stringent diagnostic criteria, initiating a downward trend, with a drop of 15% by 1990 (Hegarty et al. Reference Hegarty, Baldessarini, Tohen, Waternaux and Oepen1994). Findings indicate that the narrow definition of schizophrenia is significantly associated with a decline in the rates of patients with a favourable outcome (McGlashan, Reference McGlashan1988). Studies using the Kraepelinian diagnostic systems also found lower but not statistically significant recovery estimates in comparison to non-Kraepelinian samples (median of 9% v. 12.5%) (Jaaskelainen et al. Reference Jaaskelainen, Juola, Hirvonen, McGrath, Saha, Isohanni, Veijola and Miettunen2013). Contrary to expectations, more recent findings from the 10-year follow-up of the Suffolk County Mental Health Project cohort showed no significant improvement in the rate of favourable outcome compared with those in previous samples (Bromet et al. Reference Bromet, Naz, Fochtmann, Carlson and Tanenberg-Karant2005). The investigators argued that the lack of progress might be attributed to the nosological switch from the broader schizophrenia concept in DSM-II to a narrowly defined chronic schizophrenia in DSM-III, as well as the influence of Berkson's bias.
Inclusiveness of diagnostic criteria appears to be a significant confounder in studies of predictors for outcome, such as in the case of the higher male/female ratio in patients with an unfavourable outcome as a function of more restrictive diagnostic systems (Castle et al. Reference Castle, Wessely and Murray1993). Similarly, enriched samples of poor outcome spuriously find a more co-occurrence of positive and negative symptom domains, thus creating a false conception of a distinct illness, when in fact an inflated rate of concurrence has been the individual contribution of each dimension to help-seeking behaviour (Maric et al. Reference Maric, Myin-Germeys, Delespaul, de Graaf, Vollebergh and Van Os2004).
Meta-analyses report that male sex is associated with a 1.3–1.5-fold increase in the risk of developing schizophrenia (Aleman et al. Reference Aleman, Kahn and Selten2003; McGrath et al. Reference McGrath, Saha, Welham, El Saadi, MacCauley and Chant2004). Similar to the outcome bias, the sex difference in incidence rates were significantly higher in studies with samples collected in the post-DSM-III era compared with those collected prior to 1980 (Aleman et al. Reference Aleman, Kahn and Selten2003) – apparently as a result of the use of more stringent diagnostic criteria (Lewine et al. Reference Lewine, Burbach and Meltzer1984; Castle et al. Reference Castle, Wessely and Murray1993; Beauchamp & Gagnon, Reference Beauchamp and Gagnon2004). Conversely, no statistically significant sex difference exists in prevalence estimates of schizophrenia (Saha et al. Reference Saha, Chant, Welham and McGrath2005; Perala et al. Reference Perala, Suvisaari, Saarni, Kuoppasalmi, Isometsa, Pirkola, Partonen, Tuulio-Henriksson, Hintikka, Kieseppa, Harkanen, Koskinen and Lonnqvist2007). Aside from methodological issues (Saha et al. Reference Saha, Chant and McGrath2008), the ebb of male preponderance in prevalence estimates, contrasting with comparable incidence rates, could be interpreted with two propositions: (i) Male sex predicts both development of schizophrenia and either better outcome or greater illness-related mortality during the course. However, evidence indicates no sex-difference in standardized mortality ratios (Saha et al. Reference Saha, Chant and McGrath2007) and better outcome in women diagnosed with schizophrenia (Abel et al. Reference Abel, Drake and Goldstein2010). (ii) Clinicians, guided by diagnostic manuals with rigid criteria, erroneously tend to overdiagnose schizophrenia in males at first contact. With this discussion, our aim was not to disentangle this paradox but to prompt researchers about how different definitions can dramatically influence even basic demographic and epidemiological parameters underlying a disease concept.
Psychosis continuum
Modern classification systems, embracing a polythetic approach, categorize schizophrenia and related disorders based on different combinations of a required number of symptom domains that exceed the operational threshold of severity. This taxonomy implies a point of rarity, a unique phenotype with precise boundaries. However, a systematic review of taxometric research on schizophrenia concluded that studies favouring a categorical construct over a single distribution model were heavily influenced by a variety of methodological issues endangering the external and the internal validity (Linscott et al. Reference Linscott, Allardyce and van Os2010).
Consecutive meta-analyses of modern epidemiological data further suggest that psychosis expression is not an all-or-none phenomenon, but, in fact, phenomenologically and temporally continuous across the general population, with prevalence rates of subthreshold states varying from around 5% (delimited to interview-based reporting) to 8% (including self-report estimates) and incidence rates of 2.5% (van Os et al. Reference van Os, Linscott, Myin-Germeys, Delespaul and Krabbendam2009; Linscott & van Os, Reference Linscott and van Os2013). With regard to temporal continuity, psychotic experiences at a subclinical level in adolescence and early adulthood have some predictive value for psychotic disorders and also, to a lesser degree, for non-psychotic disorders, but mainly for a more severe psychopathology: functional impairment, violence and suicide (Poulton et al. Reference Poulton, Caspi, Moffitt, Cannon, Murray and Harrington2000; Hanssen et al. Reference Hanssen, Bak, Bijl, Vollebergh and van Os2005; Rossler et al. Reference Rossler, Riecher-Rossler, Angst, Murray, Gamma, Eich, van Os and Gross2007; Dominguez et al. Reference Dominguez, Saka, Lieb, Wittchen and van Os2010, Reference Dominguez, Wichers, Lieb, Wittchen and van Os2011; Saha et al. Reference Saha, Scott, Varghese and McGrath2011; Kaymaz et al. Reference Kaymaz, Drukker, Lieb, Wittchen, Werbeloff, Weiser, Lataster and van Os2012; Kelleher et al. Reference Kelleher, Keeley, Corcoran, Lynch, Fitzpatrick, Devlin, Molloy, Roddy, Clarke, Harley, Arseneault, Wasserman, Carli, Sarchiapone, Hoven, Wasserman and Cannon2012; Werbeloff et al. Reference Werbeloff, Drukker, Dohrenwend, Levav, Yoffe, van Os, Davidson and Weiser2012; Sharifi et al. Reference Sharifi, Eaton, Wu, Roth, Burchett and Mojtabai2015; Honings et al. Reference Honings, Drukker, Groen and van Os2016a , Reference Honings, Drukker, van Nierop, van Winkel, Wittchen, Lieb, Ten Have, de Graaf, van Dorsselaer and van Os b ). Recent findings from World Health Organization World Mental Health Surveys showing bidirectional temporal associations between positive psychotic experiences and a broad spectrum of non-psychotic mental disorders concur with the notion that subtle psychosis expression is transdiagnostic (McGrath et al. Reference McGrath, Saha, Al-Hamzawi, Andrade, Benjet, Bromet, Browne, Caldas de Almeida, Chiu, Demyttenaere, Fayyad, Florescu, de Girolamo, Gureje, Haro, Ten Have, Hu, Kovess-Masfety, Lim, Navarro-Mateu, Sampson, Posada-Villa, Kendler and Kessler2016).
Psychotic experiences are generally (almost over three-fourths) transient (Hanssen et al. Reference Hanssen, Bak, Bijl, Vollebergh and van Os2005; Cougnard et al. Reference Cougnard, Marcelis, Myin-Germeys, De Graaf, Vollebergh, Krabbendam, Lieb, Wittchen, Henquet, Spauwen and Van Os2007). However, the likelihood of later psychopathology that requires professional care increases as a function of the additive interaction between subthreshold expression of multiple psychotic symptom domains – for example, the co-occurrence of hallucinations and delusions predicts higher psychopathology load and greater severity (Smeets et al. Reference Smeets, Lataster, Dominguez, Hommes, Lieb, Wittchen and van Os2012; Nuevo et al. Reference Nuevo, Van Os, Arango, Chatterji and Ayuso-Mateos2013; Smeets et al. Reference Smeets, Lataster, van Winkel, de Graaf, Ten Have and van Os2013). Similarly, the greater the admixture with affective disturbance (Hanssen et al. Reference Hanssen, Bak, Bijl, Vollebergh and van Os2005) or motivational impairments (Dominguez et al. Reference Dominguez, Saka, Lieb, Wittchen and van Os2010), the greater the risk of psychotic disorder in the future. The presence of psychosis can thus be considered as a marker for more severe psychopathology that negatively impacts outcome. To what degree psychosis itself, rather than the severity of the mixed psychopathological states it forms a part of, causally impacts outcome remains uncertain.
Evidence that environmental and genetic load are shared across clinical and subthreshold psychotic phenomena lend further support for aetiological continuity and provides us with a framework to dissect diverse paths from transitory psychotic experiences to persistent psychosis expression and subsequent need for care. Studies have shown that genetic liability and exposure to environmental risk factors (trauma, urban environment, cannabis, etc.) synergistically increase psychosis expression – as a function of the severity of comorbid psychopathology – in a dose–response fashion (Guloksuz et al. Reference Guloksuz, van Nierop, Lieb, van Winkel, Wittchen and van Os2015) and further predicts subsequent persistence and need for care in those with baseline subthreshold psychotic experience (Henquet et al. Reference Henquet, Krabbendam, Spauwen, Kaplan, Lieb, Wittchen and van Os2004; Spauwen et al. Reference Spauwen, Krabbendam, Lieb, Wittchen and van Os2004, Reference Spauwen, Krabbendam, Lieb, Wittchen and van Os2006a , Reference Spauwen, Krabbendam, Lieb, Wittchen and van Os b ).
Instead of a binary model, the liability-threshold model (Gottesman & Shields, Reference Gottesman and Shields1967), providing a basis to predict phenotypic outcome quantitatively by the cumulative risk load of genetic and environmental factors, might be advantageous in investigating psychosis expression lying on the same continuum with normality (Fig. 2).
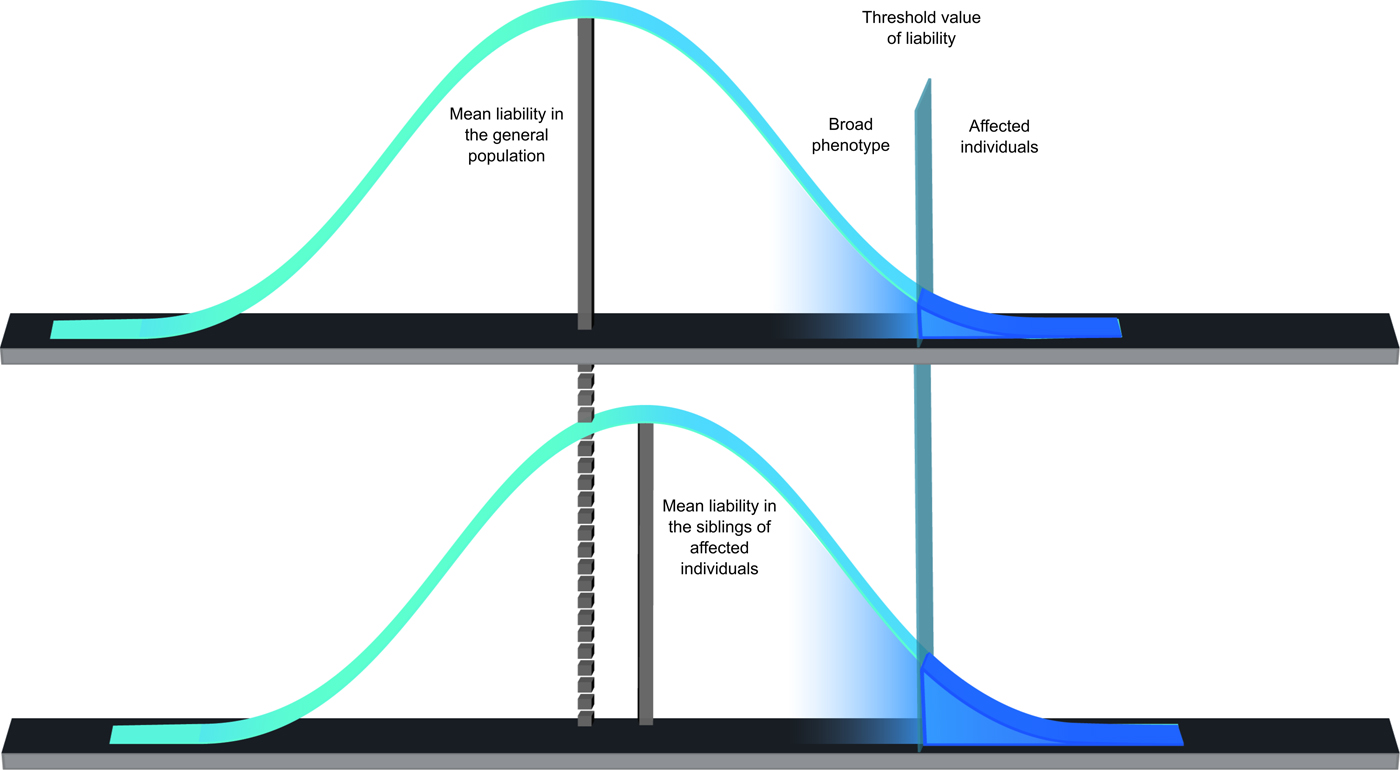
Fig. 2. The liability-threshold model, assuming a Gaussian distribution of a continuous liability in the general population, posits phenotypic outcome can be determined quantitatively by the combined effects of genetic load and environmental factors. If cumulative predisposition exceeds a certain threshold value, individual manifests the clinical syndrome.
Transdiagnostic psychosis manifestation
‘If we were to accept that the affective and schizophrenic manifestations of insanity are not in themselves the external expression of certain disease processes, but merely reveal those areas of our personality in which such processes take place, … [t]heir significance would then only reside in the fact that the schizophrenic illnesses affect different parts of our emotional life from the manic-depressive insanity.’ (Kraepelin, Reference Kraepelin1992)
A spectrum model of psychosis has testable implications (e.g. across the psychosis spectrum there are no qualitative differences in psychopathology, aetiology, treatment and outcome; there is movement over the spectrum and across dimensions within individuals), many of which are supported by the existing literature. Thus, similarities between schizophrenia and bipolar disorder exceed their differences: phenomenological expression (van Os et al. Reference van Os, Gilvarry, Bale, van Horn, Tattan, White and Murray2000; Krabbendam et al. Reference Krabbendam, Myin-Germeys, De Graaf, Vollebergh, Nolen, Iedema and Van Os2004; Kaymaz et al. Reference Kaymaz, van Os, de Graaf, Ten Have, Nolen and Krabbendam2007), cognitive functioning (Bora et al. Reference Bora, Yucel and Pantelis2009; Hill et al. Reference Hill, Reilly, Keefe, Gold, Bishop, Gershon, Tamminga, Pearlson, Keshavan and Sweeney2013), genetic liability (Van Snellenberg & de Candia, Reference Van Snellenberg and de Candia2009; Ritsner & Gottesman, Reference Ritsner, Gottesman and Ritsner2011; Lee et al. Reference Lee, Ripke, Neale, Faraone, Purcell, Perlis, Mowry, Thapar, Goddard, Witte, Absher, Agartz, Akil, Amin, Andreassen, Anjorin, Anney, Anttila, Arking, Asherson, Azevedo, Backlund, Badner, Bailey, Banaschewski, Barchas, Barnes, Barrett, Bass, Battaglia, Bauer, Bayes, Bellivier, Bergen, Berrettini, Betancur, Bettecken, Biederman, Binder, Black, Blackwood, Bloss, Boehnke, Boomsma, Breen, Breuer, Bruggeman, Cormican, Buccola, Buitelaar, Bunney, Buxbaum, Byerley, Byrne, Caesar, Cahn, Cantor, Casas, Chakravarti, Chambert, Choudhury, Cichon, Cloninger, Collier, Cook, Coon, Cormand, Corvin, Coryell, Craig, Craig, Crosbie, Cuccaro, Curtis, Czamara, Datta, Dawson, Day, De Geus, Degenhardt, Djurovic, Donohoe, Doyle, Duan, Dudbridge, Duketis, Ebstein, Edenberg, Elia, Ennis, Etain, Fanous, Farmer, Ferrier, Flickinger, Fombonne, Foroud, Frank, Franke, Fraser, Freedman, Freimer, Freitag, Friedl, Frisen, Gallagher, Gejman, Georgieva, Gershon, Geschwind, Giegling, Gill, Gordon, Gordon-Smith, Green, Greenwood, Grice, Gross, Grozeva, Guan, Gurling, De Haan, Haines, Hakonarson, Hallmayer, Hamilton, Hamshere, Hansen, Hartmann, Hautzinger, Heath, Henders, Herms, Hickie, Hipolito, Hoefels, Holmans, Holsboer, Hoogendijk, Hottenga, Hultman, Hus, Ingason, Ising, Jamain, Jones, Jones, Jones, Tzeng, Kahler, Kahn, Kandaswamy, Keller, Kennedy, Kenny, Kent, Kim, Kirov, Klauck, Klei, Knowles, Kohli, Koller, Konte, Korszun, Krabbendam, Krasucki, Kuntsi, Kwan, Landen, Langstrom, Lathrop, Lawrence, Lawson, Leboyer, Ledbetter, Lee, Lencz, Lesch, Levinson, Lewis, Li, Lichtenstein, Lieberman, Lin, Linszen, Liu, Lohoff, Loo, Lord, Lowe, Lucae, MacIntyre, Madden, Maestrini, Magnusson, Mahon, Maier, Malhotra, Mane, Martin, Martin, Mattheisen, Matthews, Mattingsdal, McCarroll, McGhee, McGough, McGrath, McGuffin, McInnis, McIntosh, McKinney, McLean, McMahon, McMahon, McQuillin, Medeiros, Medland, Meier, Melle, Meng, Meyer, Middeldorp, Middleton, Milanova, Miranda, Monaco, Montgomery, Moran, Moreno-De-Luca, Morken, Morris, Morrow, Moskvina, Muglia, Muhleisen, Muir, Muller-Myhsok, Murtha, Myers, Myin-Germeys, Neale, Nelson, Nievergelt, Nikolov, Nimgaonkar, Nolen, Nothen, Nurnberger, Nwulia, Nyholt, O'Dushlaine, Oades, Olincy, Oliveira, Olsen, Ophoff, Osby, Owen, Palotie, Parr, Paterson, Pato, Pato, Penninx, Pergadia, Pericak-Vance, Pickard, Pimm, Piven, Posthuma, Potash, Poustka, Propping, Puri, Quested, Quinn, Ramos-Quiroga, Rasmussen, Raychaudhuri, Rehnstrom, Reif, Ribases, Rice, Rietschel, Roeder, Roeyers, Rossin, Rothenberger, Rouleau, Ruderfer, Rujescu, Sanders, Sanders, Santangelo, Sergeant, Schachar, Schalling, Schatzberg, Scheftner, Schellenberg, Scherer, Schork, Schulze, Schumacher, Schwarz, Scolnick, Scott, Shi, Shilling, Shyn, Silverman, Slager, Smalley, Smit, Smith, Sonuga-Barke, St Clair, State, Steffens, Steinhausen, Strauss, Strohmaier, Stroup, Sutcliffe, Szatmari, Szelinger, Thirumalai, Thompson, Todorov, Tozzi, Treutlein, Uhr, van den Oord, Van Grootheest, Van Os, Vicente, Vieland, Vincent, Visscher, Walsh, Wassink, Watson, Weissman, Werge, Wienker, Wijsman, Willemsen, Williams, Willsey, Witt, Xu, Young, Yu, Zammit, Zandi, Zhang, Zitman, Zollner, Devlin, Kelsoe, Sklar, Daly, O'Donovan, Craddock, Sullivan, Smoller, Kendler and Wray2013; van Os et al. Reference van Os, van der Steen, Islam, Guloksuz, Rutten, Simons and Investigators2017) and possible neuroanatomical correlates (Ivleva et al. Reference Ivleva, Bidesi, Keshavan, Pearlson, Meda, Dodig, Moates, Lu, Francis, Tandon, Schretlen, Sweeney, Clementz and Tamminga2013; Goodkind et al. Reference Goodkind, Eickhoff, Oathes, Jiang, Chang, Jones-Hagata, Ortega, Zaiko, Roach, Korgaonkar, Grieve, Galatzer-Levy, Fox and Etkin2015). Recent efforts to discriminate the DSM categories of bipolar disorder and schizophrenia using a multimodal set of biomarkers (cognition, evoked potentials, anti-saccadic eye movement and neuroimaging) failed to yield a desirable outcome (Tamminga et al. Reference Tamminga, Ivleva, Keshavan, Pearlson, Clementz, Witte, Morris, Bishop, Thaker and Sweeney2013). Clinical data suggest that bipolar disorder and schizophrenia lie at distant ends of a severity continuum, with schizoaffective being in the middle (Mancuso et al. Reference Mancuso, Morgan, Mitchell, Berk, Young and Castle2015). Also, in help-seeking samples said to show ‘Clinical High Risk’, mood and anxiety disorders commonly coexist with sub-threshold psychotic symptoms, anticipating relatively unfavourable prognosis (Perlis et al. Reference Perlis, Uher, Ostacher, Goldberg, Trivedi, Rush and Fava2011; Wigman et al. Reference Wigman, van Os, Abidi, Huibers, Roelofs, Arntz, Kelleher and Peeters2014), questionably framed as ‘clinical transition’ (Fusar-Poli et al. Reference Fusar-Poli, Yung, McGorry and van Os2014).
Similar to data in clinical populations, a significant, albeit relatively weaker, association between dimensions of affective disturbance and psychotic expression has been shown in general population studies (Krabbendam et al. Reference Krabbendam, Myin-Germeys, De Graaf, Vollebergh, Nolen, Iedema and Van Os2004; van Rossum et al. Reference van Rossum, Dominguez, Lieb, Wittchen and van Os2011; Wigman et al. Reference Wigman, Lin, Vollebergh, van Os, Raaijmakers, Nelson, Baksheev and Yung2011). Epidemiological data further show that affective dysregulation and psychosis expression, with greater exposure to environmental risk factors, interact with each other, giving rise to a more severe outcome (Hanssen et al. Reference Hanssen, Bak, Bijl, Vollebergh and van Os2005; Kaymaz et al. Reference Kaymaz, van Os, de Graaf, Ten Have, Nolen and Krabbendam2007; Wigman et al. Reference Wigman, van Nierop, Vollebergh, Lieb, Beesdo-Baum, Wittchen and van Os2012; Guloksuz et al. Reference Guloksuz, van Nierop, Lieb, van Winkel, Wittchen and van Os2015; Isvoranu et al. Reference Isvoranu, Borsboom, van Os and Guloksuz2016).
These findings might be more suggestive of a unitary model of psychosis. Bipolar disorder and schizophrenia may well be different expressions (phenotypic presentations) of a substantially shared pathoaetiology, with varying outcomes due to disease modifiers (e.g. neurodevelopmental impairment), rather than two distinct entities with entirely diverse pathoaetiological processes (Murray et al. Reference Murray, Sham, Van Os, Zanelli, Cannon and McDonald2004). There are indeed various examples in medicine, such as multiple sclerosis, following distinct illness patterns (clinically isolated syndrome, relapsing-remitting, secondary progressive and primary progressive) with varying symptoms and outcomes but stemming from the same pathoaetiology (Confavreux & Vukusic, Reference Confavreux and Vukusic2006; Lublin et al. Reference Lublin, Reingold, Cohen, Cutter, Sorensen, Thompson, Wolinsky, Balcer, Banwell, Barkhof, Bebo, Calabresi, Clanet, Comi, Fox, Freedman, Goodman, Inglese, Kappos, Kieseier, Lincoln, Lubetzki, Miller, Montalban, O'Connor, Petkau, Pozzilli, Rudick, Sormani, Stuve, Waubant and Polman2014). Figure 3 illustrates illness course across different types of multiple sclerosis; in brackets, the DSM-IV diagnostic categories (Brief Psychotic Episode, Bipolar Disorder, Schizoaffective Disorder and Schizophrenia) were given on the basis of the resemblance of putative illness course. Similar to multiple sclerosis, these different psychiatric conditions may reasonably belong to the same spectrum of illness. Accordingly, a recent line of work suggests the existence of a general transdiagnostic psychosis phenotype at both subclinical and clinical levels – coinciding across the psychosis spectrum: schizophrenia, schizoaffective disorder and bipolar disorder – encompassing affective and non-affective symptoms, with five symptom dimensions (positive and negative symptoms, mania, depression and disorganization) disentangling the heterogeneity (Reininghaus et al. Reference Reininghaus, Priebe and Bentall2013, Reference Reininghaus, Bohnke, Hosang, Farmer, Burns, McGuffin and Bentall2016; Shevlin et al. Reference Shevlin, McElroy, Bentall, Reininghaus and Murphy2017). Originally, DSM5 was set up to encompass the model of psychotic disorders pertaining to a spectrum with transdiagnostic dimensions to allow for diagnosing heterogeneity; however, halfway the process, the idea of transdiagnostic dimensions was abandoned.
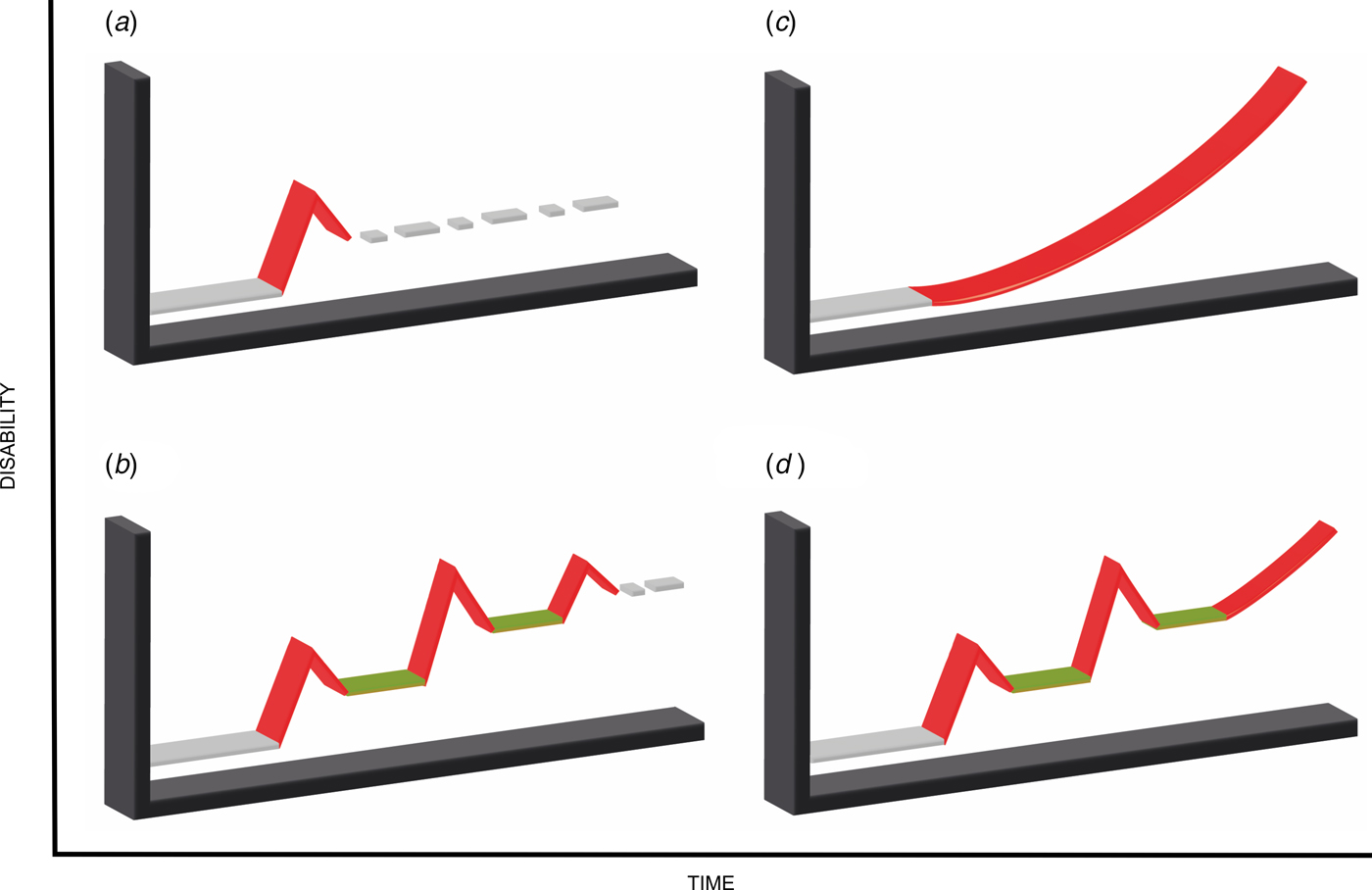
Fig. 3. Shows current multiple sclerosis classification based on disease progression. The colour red represents active disease; colour green represents remission. In brackets, the DSM-IV diagnostic categories were listed based on the resemblance of putative illness course. (a) Clinically Isolated Syndrome (Brief Psychotic Disorder), (b) Relapsing-remitting Multiple Sclerosis (Bipolar Disorder), (c) Primary Progressive Multiple Sclerosis (Schizophrenia), (d) Secondary Progressive Multiple Sclerosis (Schizoaffective Disorder).
From a researcher's standpoint, an artificial categorization leads to a considerable loss of power and precision (Kraemer, Reference Kraemer2007); from a clinician's standpoint, categories based on illness course – regardless if they are different types of the same illness or not – are pragmatically necessary to determine treatment strategy. The category of schizophrenia-type psychosis, confined to the most severely ill patients with poor outcome, may be beneficial in approximating need for care, outcome, course and treatment (Kendell & Jablensky, Reference Kendell and Jablensky2003). However, mounting evidence suggests that a transdiagnostic dimensional approach, complementary to the clinical utility of the categorical approach, may provide in-depth information that covers different aspects of psychopathology beyond the borders of the modern operationalized criteria (Demjaha et al. Reference Demjaha, Morgan, Morgan, Landau, Dean, Reichenberg, Sham, Fearon, Hutchinson, Jones, Murray and Dazzan2009; Russo et al. Reference Russo, Levine, Demjaha, Di Forti, Bonaccorso, Fearon, Dazzan, Pariante, David, Morgan, Murray and Reichenberg2014; van Os & Reininghaus, Reference van Os and Reininghaus2016).
One of the clinically-derived arguments for Kraepelinian dichotomy is that patients with bipolar disorder respond to lithium, whereas patients with non-affective psychosis do not. However, affective symptoms respond to lithium dimensionally, i.e. affective symptoms in the context of schizophrenia (i.e. schizo-affective disorder) also respond to lithium. In regard to this groundless notion of splitting and lumping of disorders on the basis of response to treatment, one may also declare the opposite, namely that these two phenotypes are identical based on the fact that they both respond to treatment with second-generation antipsychotics. In addition, cyclic illness course characterized by full remission between episodes predicts response far better than both categorical diagnoses (Tighe et al. Reference Tighe, Mahon and Potash2011). There is no doubt that this represents very useful information for treating clinicians, but it is a reductionist fallacy to propose these observations as the reasoning behind splitting or unifying the two conditions.
A lack of diagnostic markers in psychiatry impedes an objective classification. In this regard, current artificial boundaries drift the field to a paradox by hindering efforts to develop novel diagnostic tools, essential for a classification system grounded in theory. Research practice should resist the temptation of clinical pragmatism and better move away from the dichotomous approach to set sail for an evidence-based diagnostic practice replacing the century-old construct. Indeed, this was the reasoning behind the Research Domain Criteria (RDoC) system, introduced by the National Institute of Mental Health (NIMH) (Cuthbert & Insel, Reference Cuthbert and Insel2010).
Schizophrenia is an obstacle to aspirational work of early intervention
‘There is no dark side of the moon really. Matter of fact it's all dark. The only thing that makes it look light is the sun’ (in ‘Eclipse’, a song by Pink Floyd from the album: The Dark Side of the Moon)
Diagnostic manuals are like standard operating procedures: they simplify the decision-making process and guide clinicians to approximate diagnosis when valid and specific measures are not available or readily accessible to ascertain pathoaetiology. Therefore, objective diagnostic tools or lack thereof are critical for validating the diagnosis. At its best, check-listing diagnostic criteria improve reliability. Schizophrenia diagnosis has indeed ensured a high reliability, but as summarized above, its validity is debatable. Over the years, the weak validity and specificity of the schizophrenia construct have arisen as a critical methodological issue. As discussed previously, schizophrenia, along with other diagnostic categories, originally formulated to bring order to psychiatric taxonomy, has become reified over time and transformed into an impediment to research (Kendler, Reference Kendler2016a ).
Early intervention strategy became entangled in schizophrenia reification by hinging on the prototypic psychotic illness (schizophrenia) (Van Os & Delespaul, Reference Van Os and Delespaul2005; Fusar-Poli et al. Reference Fusar-Poli, Yung, McGorry and van Os2014). In keeping with classification manuals, operationalized criteria have been applied to conceptualize the binary model of clinical high-risk state – prodromal stage – as a proxy for schizophrenia. The target population has been identified as individuals with attenuated positive psychotic symptoms or a family history of psychotic disorder.
Adopting a pragmatic model, early intervention efforts have primarily aimed to reduce false discovery rate by implementing a narrow description of clinical high-risk state restricted only to subthreshold positive psychotic symptoms in help-seeking individuals (Miller et al. Reference Miller, McGlashan, Rosen, Cadenhead, Cannon, Ventura, McFarlane, Perkins, Pearlson and Woods2003; Yung et al. Reference Yung, Yuen, McGorry, Phillips, Kelly, Dell'Olio, Francey, Cosgrave, Killackey, Stanford, Godfrey and Buckby2005). The basic assumption of this indicated prevention, modelled after successful secondary prevention strategies in medicine, is that the detection of early warning symptoms of schizophrenia and subsequent intervention shall prevent subtle psychopathology from transitioning to a manifest clinical syndrome and ultimately reduce functional impairment (Van Os & Delespaul, Reference Van Os and Delespaul2005).
However, as discussed previously, epidemiological data from different populations have consistently demonstrated that a model based on psychosis expression per se – hallucinations and delusions at a sub-threshold level, which are not rare and often transient in the general population – overlooks the dynamic interplay between other elements of psychopathology and may, therefore, be insufficient to predict later psychopathology (Bentall & Beck, Reference Bentall and Beck2004; van Os, Reference van Os2013). In accordance, over three-fourths of the at-risk population enrolled in The North American Prodrome Longitudinal Study–2 had sought help for non-psychotic complaints prior to the onset of recognizable psychotic experiences (Woodberry et al. Reference Woodberry, Seidman, Bryant, Addington, Bearden, Cadenhead, Cannon, Cornblatt, McGlashan, Mathalon, Perkins, Tsuang, Walker and Woods2016). The initial intent of the prodromal psychosis concept, similar to its point of origin, schizophrenia, is to ascertain the group that benefits most from a therapeutic intervention, and thereby avoid unnecessary treatment (McGorry et al. Reference McGorry, Yung, Phillips, Yuen, Francey, Cosgrave, Germano, Bravin, McDonald, Blair, Adlard and Jackson2002; McGlashan et al. Reference McGlashan, Zipursky, Perkins, Addington, Miller, Woods, Hawkins, Hoffman, Lindborg, Tohen and Breier2003). However, this conceptualization possesses a danger of giving an implicit message to clinicians in the field that the at-risk population is the ‘pre-schizophrenia’ group and should be vigorously treated for that reason. Accordingly, a recent survey shows that clinicians follow a more conservative path than guidelines in deciding on dose reduction and discontinuation of antipsychotics after complete remission of the first psychotic episode (Thompson et al. Reference Thompson, Singh and Birchwood2016).
Emerging evidence from at-risk samples was a wake-up call to early intervention (Fusar-Poli et al. Reference Fusar-Poli, Yung, McGorry and van Os2014; McGorry & Nelson, Reference McGorry and Nelson2016): (i) The framework of ‘transition’ as an end result fails to explain the heterogeneity in clinical and functional outcome, (ii) Studies that control for ‘false transition’ representing natural fluctuation of an existing psychotic state find very low ‘transition’ rates (Morrison et al. Reference Morrison, French, Stewart, Birchwood, Fowler, Gumley, Jones, Bentall, Lewis, Murray, Patterson, Brunet, Conroy, Parker, Reilly, Byrne, Davies and Dunn2012), (iii) An over-reliance on positive psychotic symptoms sets a self-limiting barrier to capture early expression of non-specific psychopathology, the severity of which is ‘marked’ but not ‘caused’ by attenuated psychosis, (iv) ‘Clinical High Risk’ criteria majorly identify individuals with diagnosed states of anxiety/depression and/or drug use who also display subtle psychotic experiences, which research has shown is a marker for – but not necessarily the cause of – relatively poor outcome (Perlis et al. Reference Perlis, Uher, Ostacher, Goldberg, Trivedi, Rush and Fava2011; Wigman et al. Reference Wigman, van Os, Abidi, Huibers, Roelofs, Arntz, Kelleher and Peeters2014; McAusland et al. Reference McAusland, Buchy, Cadenhead, Cannon, Cornblatt, Heinssen, McGlashan, Perkins, Seidman, Tsuang, Walker, Woods, Bearden, Mathalon and Addington2015). Thus, early treatment of psychopathology (including treatment of subtle psychotic experiences), in states of anxiety/depression/drug use with a degree of psychosis admixture will naturally improve outcome; it does not seem necessary or valid, however, to claim that this effort represents ‘prevention of schizophrenia’ (Van Os & Guloksuz, Reference Van Os and Guloksuz2017).
Evidently, the aspirational work of early intervention shall evolve by abandoning confusing terminology based on the ill-defined concept of schizophrenia. A universal early intervention strategy in psychiatry, as embedded in the Headspace initiative (McGorry et al. Reference McGorry, Hamilton, Goldstone and Rickwood2016), should be the ultimate – and likely more effective – goal.
The term ‘schizophrenia’
‘The way a word is used this year is its phenotype, but it has a deeply seated, immutable meaning, often hidden, which is the genotype.’ (Thomas, Reference Thomas1973)
The origin of the term ‘schizophrenia’ is Greek, meaning ‘split mind’. The metamorphosis of the term ‘schizophrenia’ has been striking: Schizophrenia is now not only a medical term, but also a physics term to describe the split personality of electrons (Chase, Reference Chase2008) and a widely-used metaphor in economy for an unpredictable market.
The dark view of the current concept of schizophrenia – a distinct, genetic brain disease with a poor course – is also a key factor that further increases stigma and discrimination. Of all diagnostic categories, schizophrenia has been by far the most stigmatized mental condition that generates negative emotions: desperation, pity and fear (Lasalvia et al. Reference Lasalvia, Penta, Sartorius and Henderson2015). Social media research has shown that ‘schizophrenia’ has been used inappropriately and non-medically with, as expected, the adjective form ‘schizophrenic’ being even more often negative (Joseph et al. Reference Joseph, Tandon, Yang, Duckworth, Torous, Seidman and Keshavan2015). Until the recent renaming of schizophrenia in Japan, these negative connotations had made clinicians largely reluctant to use the term in their communication with patients and their families (Takahashi et al. Reference Takahashi, Ideno, Okubo, Matsui, Takemura, Matsuura, Kato and Okubo2009). A similar pattern was also observed in other countries, such as Scotland (Allardyce et al. Reference Allardyce, Morrison, Van Os, Kelly, Murray and McCreadie2000). Although a simple renaming of schizophrenia may forestall its metaphorical use, a semantic revision without a reconceptualization may not be adequate to decrease stigma immediately (Lieberman & First, Reference Lieberman and First2007; Koike et al. Reference Koike, Yamaguchi, Ojio, Ohta and Ando2016). However, even more important than stigma may be internalised negative expectations associated with schizophrenia (Sullivan et al. Reference Sullivan, Mittal, Reaves, Haynes, Han, Mukherjee, Morris, Marsh and Corrigan2015) and its pessimistic and unproven ‘devastating genetic brain disease’ description in the scientific literature (Sawa & Snyder, Reference Sawa and Snyder2002). The recently formulated CHIME framework identifies ‘hope and optimism’ as one of the core conditions for personal recovery (Leamy et al. Reference Leamy, Bird, Le Boutillier, Williams and Slade2011). The question is to what degree mental health professionals, influenced by a long tradition of pessimistic and mystifying ‘schizo’ formulations of psychotic illness, provide an environment where patients are met with hope and optimism. More hopeful, and arguably scientifically more valid, alternatives, in the direction of a broad underlying susceptibility, have recently been proposed by those with lived experience of psychosis (George & Klijn, Reference George and Klijn2013). The CHIME framework shows a clear need to diagnose not only on the basis of symptoms, but also on the basis of where the person is in the process of personal recovery, starting with the phase of being completely overwhelmed by the illness, to living a meaningful life despite continuing mental challenges.
From rare mental disorder (schizophrenia) to psychosis spectrum disorders: dimensional assessment and multifactorial staging system
‘I expect to see the end of the concept of schizophrenia soon. Already the evidence that it is a discrete entity rather than just the severe end of psychosis has been fatally undermined.’ (Murray, Reference Murray2017)
Like all other things, the way we think about mental illness is subject to a set of shared beliefs that can show change over time as a result of, for example, novel scientific insights or persistent calls for change from subgroups with deviant beliefs. In the area of mental health, the shared belief that mental distress comes as diagnosable discrete disease entities increasingly is co-existing with the view that mental suffering in reality represents a series of spectrum phenotypes. The coexistence of beliefs has found its way to the DSM5, in which the idea of mental illness as a spectrum phenotype was emphatically introduced in the areas of autism, substance use and – nearly – personality disorder, but, remarkably, not for psychotic disorder. Thus, in the DSM5 fact sheet of the American Psychiatric Association (2013), it is stated that ‘The symptoms of people with Autism Spectrum Disorder will fall on a continuum, with some individuals showing mild symptoms and others having much more severe symptoms. This spectrum will allow clinicians to account for the variations in symptoms and behaviours from person to person’. The introduction of this type of spectrum thinking is remarkable, given that until relatively recently, autism was considered a rare and uniformly severe, poor prognosis mental disorder.
Psychotic phenomena might well be conceptualized as a broad spectrum ranging from mild but persistent schizotypy to severe and recurrent schizophrenia. Indeed, the DSM5 psychosis workgroup attempted to introduce the idea of a spectrum in the structure and the ordering of the chapter, using the level, number and the duration of psychotic signs and symptoms to demarcate psychotic disorders from each other, ‘as a stepping-stone towards a more valid classification system’ (Heckers et al. Reference Heckers, Barch, Bustillo, Gaebel, Gur, Malaspina, Owen, Schultz, Tandon, Tsuang, Van Os and Carpenter2013). A multimodal investigation of genetic susceptibility at different layers of environmental exposure using the unbiased multidimensional assessment of the psychosis spectrum, not confounded by current diagnostic categories, would contribute to a better understanding of psychotic phenomena. This ‘liberated’ strategy (Moncrieff & Middleton, Reference Moncrieff and Middleton2015) has a greater probability of generating novel findings and discerning distinct pathological processes that will pave the way for a coherent theory-based classification. For example, if a neurodevelopmental factor predisposes to poor outcome in the psychosis spectrum, this association may not be detectable if the research population is limited to those with poor outcome who may be universally exposed to the neurodevelopmental factor in question. A thorough assessment of symptom dimensions stratified by risk (genetic and environmental) and resilience tiers allows for a true precision medicine in clinical practice. In fact, this is no different than what mental health professionals exercise routinely when they formulate a case.
Current health care practice demands clinicians to make quick decisions under pressure. Therefore, the primary concern with the multidimensional psychosis spectrum approach is whether it will be beneficial or burdensome in the hectic routine of clinical practice involving ever-increasing administrative demands and chronic imbalance between clinical load and mental health workforce across the world. Another argument against the utility of this approach is that clinical decisions are often binary not dimensional: admission v. discharge or treatment v. no treatment.
An additional obstacle stalling the implementation of the dimensional approach in routine practice is the general lack of data verifying its applicability in clinical settings. Therefore, the next step should be to design pragmatic clinical trials testing the utility of the dimensional spectrum approach. These studies may yield data to construct an empirical clinical course staging system that is established on a dimensional formulation of psychopathology across the psychosis spectrum. Clinicians in the field might find this system more familiar and handy in their daily operations: abstract, categorical and more importantly allowing for a bidirectional (up and down) shift between stages/types as opposed to the supposedly static diagnostic categories. The diagnostic stability and consistency of psychotic conditions identified based on current classifications are insufficient, mediocre even for the chronic, poor outcome fraction diagnosed as schizophrenia. Diagnostic switches are common because diagnostic classification often relies on a snapshot of psychopathology, which in reality varies over time. Nevertheless, there are other important longitudinal elements that carry a lot of weight with the clinician's decision, such as the episodic nature – Kraepelin indeed prioritized cyclicity above other factors for discriminating manic-depressive insanity and dementia praecox.
The DSM schizophrenia concept has been criticized for: (i) overreliance on positive symptoms; (ii) negligence of affective, negative and cognitive dimensions; (iii) extraneous emphasis on Schneiderian first-rank symptoms and subtyping, which were both removed in the DSM5; and (iv) incompetency in overcoming heterogeneity (the polythetic structure of the operational criteria further complicating the matter). The value of the negative symptom domain for diagnosis has been consistently demonstrated in empirical studies, long before the release of DSM-III (Carpenter et al. Reference Carpenter, Strauss and Bartko1973) – largely by means of predicting (albeit with relatively low predictive value) poor outcome, poor treatment response, and functional and cognitive impairment (Milev et al. Reference Milev, Ho, Arndt and Andreasen2005; Ventura et al. Reference Ventura, Hellemann, Thames, Koellner and Nuechterlein2009). Over the years, the negative symptom domain has become an active area of investigation in psychosis research with hopes of reducing heterogeneity and developing targeted treatment (Kirkpatrick et al. Reference Kirkpatrick, Fenton, Carpenter and Marder2006).
Taking the debate on negative symptoms further, the Maryland group conceived an appealing concept to reduce heterogeneity: the deficit subtype of schizophrenia, characterized by persistent primary negative symptoms that are not secondary to depression, mental retardation, positive psychotic symptoms and medication use (Carpenter et al. Reference Carpenter, Heinrichs and Wagman1988). There exist some data – mainly from studies conducted by the same group that coined the deficit syndrome – suggesting a distinct disease entity: differences in clinical outcome, risk factors and biological parameters between deficit and non-deficit types of schizophrenia (Kirkpatrick & Galderisi, Reference Kirkpatrick and Galderisi2008).
However, several methodological issues require further deliberation before drawing a conclusion. First, it is extremely difficult to make a valid and reliable distinction between primary and secondary negative symptoms, particularly in the context of enduring symptoms. Second, although the presence of persistent primary negative symptoms has been defined as the core inclusion criterion for deficit syndrome, the influence of exclusion criteria to rule out secondary negative symptoms should also be taken into account while interpreting findings. As a matter of fact, some of the distinct clinical features observed in deficit syndrome might have resulted from the exclusion criteria: lower rates of substance abuse, depressive symptoms, suicidal ideation and severe suspiciousness (Kirkpatrick et al. Reference Kirkpatrick, Buchanan, Ross and Carpenter2001). Therefore, even if deficit syndrome constitutes a distinct disease entity within schizophrenia; it is difficult to attribute biological and aetiological differences to enduring primary negative symptoms exclusively. If cognitive dysfunction and negative symptoms are associated with the level of functional impairment, this lends further support to the suggestion that the staging strategy and multidimensional approach would work better than the current taxonomy with a fuzzy algorithm. In this regard, the flexible and integrated spectrum approach, employing a staging system for clinical practice and a multidimensional structure for research use, may provide us with the essential framework to elucidate these enmeshed issues giving rise to often frustrating heterogeneity.
The introduction of a staging system across the spectrum of psychosis would produce a durable strategy (McGorry & van Os, Reference McGorry and van Os2013). In modern medicine, staging systems are frequently revised in the light of accumulating evidence about pathoaetiology, technological advancements and progress in treatment. Until a true discovery, these modifications, taking place within the illness spectrum, will not lead to a synthetic reclassification of diagnosis with each revision – the diagnostic category of a patient may artificially change over time with each new release of the current classification systems, e.g. the rise and fall of schizoaffective disorder.
Given apparent flaws of schizophrenia, both complementary and alternative paradigms, bearing a resemblance to our speculations in the current article, have been debated for a long time (Strauss & Gift, Reference Strauss and Gift1977; Bentall et al. Reference Bentall, Jackson and Pilgrim1988; Brockington, Reference Brockington1992; Boteva & Lieberman, Reference Boteva and Lieberman2003; van Os, Reference van Os2009; Keshavan et al. Reference Keshavan, Nasrallah and Tandon2011). Despite a series of demands for reconceptualization, these scholarly communications (in particular, strategies for clinical implementation) have been stuck at the theoretical level. Given the call for a change coming from highly influential scholars, one might ask why these discussions failed to go beyond ‘Monday morning quarterbacking’.
There are likely various reasons for this lack of progress, but the most obvious and influential ones in order of importance may be: (i) the influence of the DSM stronghold with a monopoly mentality, killing the competition in advance by not giving them a foothold; (ii) the sunk cost fallacy or, despite clear lack of progress, to continue to cling to the concept, because an enormous amount of funding and time have been invested in understanding schizophrenia over a century.
The idea of schizophrenia as a distinct categorical entity has recently been contested by the release of the NIMH research initiative, the RDoC (Cuthbert & Insel, Reference Cuthbert and Insel2010); and the multidimensional approach slowly gaining a foothold in the DSM (Heckers et al. Reference Heckers, Barch, Bustillo, Gaebel, Gur, Malaspina, Owen, Schultz, Tandon, Tsuang, Van Os and Carpenter2013). At last, these advances would generate most-needed funding to foster more research incorporating multidimensional assessment of transdiagnostic samples that would hopefully provide us with essential data for a reconceptualization along spectrum lines.
However, the current construct of schizophrenia still dominates the field as if there is no other reality without its borders, and therefore remains to be an obstruction, which stagnate the efforts to prudent and feasible solutions. Accordingly, limited data exist about how we may feed dimensional assessment into a staging system. For now, instead of repeating the mistake by proposing a radical shift towards a new framework offering unwarranted promises, we can modestly start with following the footsteps of the reconceptualization of autism spectrum disorder: a single umbrella disorder – psychosis spectrum disorder (PSD) – with specifiers. Even this subtle revision will help the field to rethink psychosis without the borders of schizophrenia and therefore clear the way for a better conceptualization in the future.
This unifying approach, however, should not be interpreted as a refutation of likelihood existence of distinct diseases in the broad PSD – deconstruction will eventually lead to a more stable reconstruction. For now, the reconceptualization is merely acknowledging the limits of our knowledge about PSD. Also, the reconceptualization of PSD cannot be complete without a semantic revision – the term ‘schizophrenia’ should be abolished.
In his self-reflection, looking back at his prolific career spanning over 50 years, Carpenter states that his major regret is his failure to be bold enough in pressing the field for reconstructing schizophrenia (Carpenter, Reference Carpenter2017). We can learn from the past and finally show some collective courage to open up the discussion of how we could replace the slowly dying schizophrenia concept.
Conclusion
Psychosis remains an enigma; despite intensive research, much remains to be elucidated in terms of aetiology, diagnosis and treatment. Given this state of affairs, perpetuating the diagnostic status quo has been the default to date. Furthermore, schizophrenia is a psychiatric tradition as much as a diagnosis, contributing to the identity of diagnosing professionals. In Japan and South Korea, change was perhaps easier as the concept of ‘splitting mind disease’ was imported from another part of the world, making replacement with a culturally more acceptable concept a viable option. In Europe, the concept of schizophrenia is associated with the origins of scientific psychiatry, something to be proud of, a symbol of progression. However, with the introduction of spectrum phenotypes in DSM5, and an increasingly vocal movement for change (George & Klijn, Reference George and Klijn2013; Henderson & Malhi, Reference Henderson and Malhi2014; Lasalvia et al. Reference Lasalvia, Penta, Sartorius and Henderson2015; Moncrieff & Middleton, Reference Moncrieff and Middleton2015) the tipping point may have been reached. Just as schizophrenia was the last diagnosis to benefit from research linking to childhood adversity to adult mental health outcomes (Read & Bentall, Reference Read and Bentall2012), so may it be the last to benefit from the advantages of a modern spectrum diagnostic approach. There is hope for schizophrenia.
Acknowledgements
SG and JvO would like to acknowledge the European Community's Seventh Framework Program under grant agreement No. HEALTH-F2-2009-241909 (Project EU-GEI). Authors would like to thank Lotta-Katrin Pries and Ilgin Guloksuz for their help with designing the figures.
Declaration of Interest
None.
Summary box
-
• With the introduction of spectrum phenotypes in DSM5, and an increasingly vocal movement for change, the tipping point may have been reached. Just as schizophrenia was the last diagnosis to benefit from research linking childhood adversity to adult mental health outcomes, so may it be the last to benefit from the advantages of a modern spectrum diagnostic approach.
-
• The current concept of schizophrenia, described by diagnostic guidelines and later reified, has become detrimental to progress in mental health by confining research efforts to a constantly changing construct that does not exist in Nature.
-
• The current concept of schizophrenia, subject to Berkson's bias, represents only a minor fraction with the worst outcome of a much broader and under-researched spectrum phenotype, yet has come to represent everything ‘psychotic’ – even psychotic experiences in non-psychotic disorders (‘Ultra-High Risk’).
-
• The current concept of schizophrenia overlooks evidence indicating that psychosis expression is continuous across the general population and can, therefore, be better explored using a quantitative dimensional approach than a dichotomous distinction between ill and healthy on the basis of arbitrary set points.
-
• The current concept of schizophrenia is far from being specific, as evidenced by the significant overlap between schizophrenia and other diagnostic constructs, concerning treatment, phenomenological expression, genetic liability, molecular mediation and anatomical representation.
-
• The current concept of schizophrenia, dictated by recent diagnostic manuals, is inadequate – even misleading at times – to convey an in-depth information to guide clinicians and patients in the decision-making process.
-
• The current concept of schizophrenia, as the prototypic psychotic illness, sets a self-limiting barrier to aspirational work of early intervention.
-
• The current concept of schizophrenia has led to the transformation of a medical term to a loaded layman's term with various negative connotations.
-
• The current concept of schizophrenia represents iatrogenic hopelessness (‘devastating genetic brain disease’), resulting in internalized negative expectations and undermining the CHIME framework guiding mental health services development.





