Introduction
Bipolar disorder (BD) is associated with significant cognitive deficits present in a substantial proportion of patients (Burdick et al., Reference Burdick, Russo, Frangou, Mahon, Braga, Shanahan and Malhotra2014; Cullen et al., Reference Cullen, Ward, Graham, Deary, Pell, Smith and Evans2016). Strong evidence demonstrates the relevance of cognitive impairment for psychosocial and occupational functioning (Ehrminger et al., Reference Ehrminger, Brunet-Gouet, Cannavo, Aouizerate, Cussac, Azorin and Roux2019; Tse, Chan, Ng, & Yatham, Reference Tse, Chan, Ng and Yatham2014). This highlights the need for evidence-based interventions targeting cognitive dysfunction to improve functional recovery and the overall illness course (Miskowiak, Carvalho, Vieta, & Kessing, Reference Miskowiak, Carvalho, Vieta and Kessing2016). Cognitive remediation (CR) is a psychological intervention which was developed to tackle cognitive deficits and reduce the impact of cognitive impairment on functional recovery. Meta-analytic evidence demonstrates effectiveness of CR at improving cognitive and functional outcomes in people with a diagnosis of schizophrenia (Wykes, Huddy, Cellard, McGurk, & Czobor, Reference Wykes, Huddy, Cellard, McGurk and Czobor2011). For people with BD, evidence for the potential benefits of CR is still emerging and more high-quality randomized trials are required to establish these effects (Bellani et al., Reference Bellani, Biagianti, Zovetti, Rossetti, Bressi, Perlini and Brambilla2019; Tsapekos et al., Reference Tsapekos, Seccomandi, Mantingh, Cella, Wykes and Young2020a). Recent trials report promising findings for the effect of CR on functional outcomes (Bernabei et al., Reference Bernabei, Bersani, Pompili, Delle Chiaie, Valente, Corrado and Coccanari de'Fornari2020; Lengvenyte, Coppola, Jaussent, Courtet, & Olié, Reference Lengvenyte, Coppola, Jaussent, Courtet and Olié2020; Strawbridge et al., Reference Strawbridge, Tsapekos, Hodsoll, Mantingh, Yalin, McCrone and Young2021). According to a CR model, changes in functioning are not only explained by a direct effect of the therapy, but can also be attributed to the indirect effect that cognitive improvements have on functioning (Wykes & Spaulding, Reference Wykes and Spaulding2011). To date, this generalization of cognitive improvements to functioning has received limited attention and requires further empirical evidence.
Evidence of whether and how a transfer of cognitive skills to functional outcomes occurs for people with BD is limited. An uncontrolled study considering 18 participants suggested that changes in self-reported executive functioning partially accounted for the improvement in functional outcomes (Deckersbach et al., Reference Deckersbach, Nierenberg, Kessler, Lund, Ametrano, Sachs and Dougherty2010). More recently, a trial assessing CR effects in people with psychotic BD reported a significant correlation between post-treatment changes in cognition and community functioning, but that was not specific to the treatment group and so cannot be attributed to the effect of CR (Lewandowski et al., Reference Lewandowski, Sperry, Cohen, Norris, Fitzmaurice, Ongur and Keshavan2017). Findings from a follow-up study assessing the long-term effects of functional remediation, a psychological intervention similar to CR, suggested a significant correlation between verbal memory improvement and changes in psychosocial functioning for participants receiving the treatment (Bonnin et al., Reference Bonnin, Reinares, Martinez-Aran, Balanza-Martinez, Sole, Torrent and Vieta2016). However, the study used cross-sectional data which limits the scope for a causal interpretation of this association. Overall, available evidence is hampered by methodological limitations (e.g. uncontrolled design, no time sequencing) and choice of analytic methods (e.g. use of simple correlation).
As previously suggested for other psychological interventions (Windgassen, Goldsmith, Moss-Morris, & Chalder, Reference Windgassen, Goldsmith, Moss-Morris and Chalder2016), establishing models of how CR affects functioning through cognition is essential not only to confirm the theoretical mechanism of action, but also to refine the way CR is delivered. Identifying transfer mechanisms related to cognition can help treatment paradigms emphasize those cognitive skills driving functional improvement which may result in more efficient and effective therapy delivery (Wykes et al., Reference Wykes, Reeder, Huddy, Taylor, Wood, Ghirasim and Landau2012). This is in line with the recommendations of International Society of Bipolar Disorders (ISBD) for cognitive intervention trials suggesting the use of long-term follow-up assessments to examine the translation of cognitive benefits into functional improvements (Miskowiak et al., Reference Miskowiak, Burdick, Martinez-Aran, Bonnin, Bowie, Carvalho and Vieta2017). Providing models of how this transfer occurs is important for establishing the clinical significance of CR for people with BD (Tsapekos, Strawbridge, Cella, Wykes, & Young, Reference Tsapekos, Strawbridge, Cella, Wykes and Young2020b).
This study will examine whether and how cognitive gains following CR transfer to prospective improvement in functional outcomes using data from a randomized controlled trial (CRiB). Two models will be explored: mediation and moderation. Mediation will examine whether post-treatment cognitive changes account for the effect of CR on functional outcomes at follow-up. Moderation will test if the level of cognitive performance achieved at post-treatment affects functional improvement at follow-up.
Methods
Study design
This is a secondary analysis of longitudinal data from the CRiB study comparing CR to treatment-as-usual (TAU) in euthymic patients with BD (Strawbridge et al., Reference Strawbridge, Tsapekos, Hodsoll, Mantingh, Yalin, McCrone and Young2021). Compared to main CRiB, this study includes an extended sample (plus 20 participants). These participants, recruited under the same criteria following a recruitment extension, were not included in the primary CRiB analysis which was conducted in accordance with the published protocol (N = 60) (Strawbridge et al., Reference Strawbridge, Fish, Halari, Hodsoll, Reeder, Macritchie and Young2016), before all 80 participants had completed trial participation. The additional 20 participants are included in this study to increase the power of secondary analyses. All participants provided written informed consent prior to study procedures. Cognitive and functional outcomes were assessed at three time points: baseline (week 0), post-treatment (week 13), and follow-up (week 25). After the baseline assessment, participants were randomly allocated to CR or TAU groups, with an intervention period of 12 weeks (weeks 1–12). The trial was approved by the City Road & Hampstead NHS Research Ethics Committee (reference 15/LO/1557).
Participants
CRiB included participants with a DSM-5 diagnosis of BD, from primary and secondary care services, online advertising, and mental health charities. Included participants had to be fluent in English and aged between 18 and 65 years. The Mini International Neuropsychiatric Interview (Sheehan et al., Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs, Weiller and Dunbar1998) was used to confirm the BD diagnosis and subtype. Participants had to be on stable psychiatric medication and free of acute mood symptoms for ⩾1 month prior to inclusion. Euthymia was defined as a score of ⩽7 on the Hamilton Depression Rating Scale 17-item (HAMD) (Hamilton, Reference Hamilton1960) and Young Mania Rating Scale (YMRS) (Young, Biggs, Ziegler, & Meyer, Reference Young, Biggs, Ziegler and Meyer1978) for one month. Exclusion criteria included a neurological disorder, personality disorder diagnosis, abuse or dependence on alcohol or illicit substances over the past six months.
Intervention
Cognitive remediation
CR was delivered for 12 weeks using the online software ‘Computerised Interactive Remediation of Cognition – Interactive Training for Schizophrenia’ (CIRCuiTS; https://www.circuitstherapyinfo.com). CIRCuiTS is a therapist-led, metacognition-informed, computerized CR approach, focusing on strategy use and transfer of cognitive skills to daily-life activities and individual goals. It has been previously validated for patients with schizophrenia (Reeder et al., Reference Reeder, Pile, Crawford, Cella, Rose, Wykes and Callard2016, Reference Reeder, Huddy, Cella, Taylor, Greenwood, Landau and Wykes2017).
Therapy was delivered individually by trained postgraduate psychologists with supervision from an experienced clinical psychologist. CR delivery comprised one-on-one sessions, either in person or remotely (e.g. video call), and supplementary independent homework sessions, flexibly adjusting to participant needs. The target for therapy engagement was 2–3 hourly sessions per week, aiming for a total of 30–40 sessions. A threshold of 20 h of CIRCuiTS training was predefined as the minimum for treatment completion. See further details in online Supplementary Methods.
Treatment-as-usual
Throughout the trial, participants in both groups continued their usual treatments, including medications and psychosocial interventions not explicitly targeting cognition, without any interference from the study team.
Measures
Data collection for clinical measures, cognitive and functional outcomes was blinded to group allocation. Information on sociodemographic characteristics (e.g. age, education) and clinical variables (BD subtype, age of onset, illness duration) was collected at baseline using a structured interview. Clinical symptoms were assessed using the HAMD and the YMRS. Psychotropic medication use (number of medications, medication classes) was recorded at baseline and changes were monitored throughout the study.
Cognitive assessments
We used four cognitive tests showing significant between-group improvement in CRiB for this analysis. These tests assessed four cognitive domains:
• Processing speed, with the Digit-symbol coding from the Wechsler Adult Intelligence Scale 4th edition (Wechsler, Reference Wechsler2014)
• Attention and working memory, using the Digit span (forward, backward and sequencing) from the Wechsler Adult Intelligence Scale 4th edition (Wechsler, Reference Wechsler2014)
• Verbal memory, using the Verbal paired associates II (VPA2; delayed free recall) from the Wechsler Memory Scale 4th edition (Wechsler, Reference Wechsler2009)
• Executive functioning, using the Hotel test (Manly, Hawkins, Evans, Woldt, & Robertson, Reference Manly, Hawkins, Evans, Woldt and Robertson2002)
Raw scores from each of the four individual cognitive tests were transformed to age- and education-corrected standardized scores (z scores; Mean = 0, s.d. = 1) according to the test manuals. Higher scores reflected better performance for all cognitive tests. A composite score for global cognition was computed by averaging individual domain z scores.
Functional outcomes
Psychosocial functioning was assessed using the Functional Assessment Short Test (FAST) (Rosa et al., Reference Rosa, Sánchez-Moreno, Martínez-Aran, Salamero, Torrent, Reinares and Ayuso-Mateos2007), a validated scale designed to measure functional difficulties commonly reported by people with BD. FAST evaluated six different domains of functioning (i.e. autonomy, occupation, cognition, financial issues, interpersonal relationships, leisure time) with higher scores representing greater levels of functional impairment. FAST was recommended by the International Society for Bipolar Disorders as a measure to detect changes in functioning associated with cognitive improvement (Miskowiak et al., Reference Miskowiak, Burdick, Martinez-Aran, Bonnin, Bowie, Carvalho and Vieta2017).
Attainment of personal goals was assessed using the Goal Attainment Scale (GAS) (Turner-Stokes, Reference Turner-Stokes2009). GAS provided a standardized way of quantifying the extent to which participants achieved their individual goals following the intervention period, with higher scores indicating greater goal achievement. Goals were set at baseline to suit the participant's daily-life needs and personal priorities. For each time-point, progress in goal attainment was evaluated considering the baseline and expected level of performance. The GAS has been previously used as an outcome in CR (Wykes et al., Reference Wykes, Joyce, Velikonja, Watson, Aarons, Birchwood and Upthegrove2018) and other cognitive rehabilitation studies (Hurn, Kneebone, & Cropley, Reference Hurn, Kneebone and Cropley2006).
Statistical analysis
Analyses were conducted using SPSS (version 26; IBM, New York). All continuous variables were checked for normality of distributions using the Shapiro−Wilk test and log transformation was applied for non-normally distributed variables; this successfully normalized the distribution.
Estimating treatment outcomes
Although treatment effects on cognition and functioning were previously estimated (Strawbridge et al., Reference Strawbridge, Tsapekos, Hodsoll, Mantingh, Yalin, McCrone and Young2021), this analysis was repeated since we considered an extended sample for this study. Repeated measures ANOVAs were conducted to assess the main effects of treatment group, time and a group × time interaction effect on cognitive and functional outcomes. These models were repeated to provide treatment effect estimates for post-treatment (week 13) and follow-up (week 25). This analysis tested whether changes over time were significant between groups for cognitive and functional outcomes considered in subsequent transfer models.
Testing transfer models
Transfer between cognition and functioning was examined using the PROCESS macro for SPSS (version 3.5), a regression-based tool designed for mediation and moderation analysis (Hayes, Reference Hayes2017). PROCESS uses a resampling method, percentile bootstrapping, to estimate coefficients and confidence intervals for indirect effects in mediator models and interaction effects in moderation models. Resampling approaches minimize confidence interval estimation bias for model parameters and provide greater power to detect an indirect effect compared to other methods (Mackinnon, Lockwood, & Williams, Reference Mackinnon, Lockwood and Williams2004; Williams & Mackinnon, Reference Williams and Mackinnon2008). Significance for indirect and interaction effects was determined based on bootstrap confidence intervals.
Mediation models tested whether cognitive gains after CR (week 13) are associated with functional improvement at follow-up (week 25). Models were fitted separately for the two functional outcomes and included the treatment group and the putative mediator (Fig. 1a). For each model, the direct effect of treatment group on functional outcome in the presence of the mediator (path c’) was estimated. Mediation effects were calculated by multiplying the intervention coefficient (path a) with the mediator coefficient (path b), with corresponding 95% confidence intervals for the path coefficients and the indirect effect obtained by bootstrapping (5000 repetitions). We also estimated the proportion (%) of the total treatment effect on the functional outcome accounted by the examined mediator.

Fig. 1. Path diagram examples of mediation (a) and moderation (b) models. Tx, treatment group (CR/TAU); M, cognition as putative mediator; UC, unmeasured confounding; W, cognition as putative moderator; Y, functioning as outcome.
All mediation models controlled for the baseline measure of the mediator and the outcome to account for potential unmeasured confounding in the non-randomized relationship between the mediator and the outcome (Emsley, Dunn, & White, Reference Emsley, Dunn and White2009). Baseline measures of the mediator and outcome are considered among the most important confounders for this relationship (Dunn, Emsley, Liu, & Landau, Reference Dunn, Emsley, Liu and Landau2013; Dunn et al., Reference Dunn, Emsley, Liu, Landau, Green, White and Pickles2015). We also included age, education years and depressive symptoms as covariates due to their known associations with cognition and/or functioning.
Moderation models examined whether changes in functional outcomes (week 25) depend on the level of normative cognitive performance achieved at the end of the intervention period (week 13). Normative cognitive performance is defined as the participant's performance compared to the general population norms and is measured in standard deviation (s.d.) units, both for individual tests and the composite score. For each functional outcome, the model included the treatment group, the putative moderator and their two-way interaction term as predictors, while also controlling for the baseline score of the examined outcome, age, education years, and depressive symptoms (Fig. 1b).
This was a complete case analysis, including only participants with full follow-up data, regardless of whether they completed therapy or not. We tested for observed variables predicting a pattern of missingness in outcomes under the assumption that data were missing at random (MAR) and included any predictors in the analysis as covariates. To examine potential bias of a complete case analysis, we tested baseline values of cognitive and functional outcomes as predictors of missingness (Hughes, Heron, Sterne, & Tilling, Reference Hughes, Heron, Sterne and Tilling2019). For all models, continuous variables were standardized to facilitate findings interpretation (i.e. predictor coefficients representing changes in s.d. units of the outcome). Although CRiB was not designed as a mechanistic study, mediation and moderation models tested in this study were designed to maintain temporal precedence, with cognitive and functional outcomes measured at sequential time points according to the theoretical treatment model of CR. This may assist with the interpretation of the relationship between cognition and functioning.
Power considerations
Using Monte Carlo simulation, Pan, Liu, Miao, & Yuan (Reference Pan, Liu, Miao and Yuan2018) estimated sample sizes required to achieve 80% power in longitudinal mediation models using the bootstrap method based on three factors: the strength of the mediation effect (i.e. coefficient values in the indirect path), the number of repeated measures (i.e. time points), and the intraclass correlation coefficient (ICC) of the model measures (i.e. with higher ICC values requiring a larger sample size). In our study, the ICC was 0.93 for the FAST, 0.56 for the GAS and higher than 0.8 for all cognitive outcomes, with measures repeated at three time points. Using these estimates, our mediation models were 80% powered to detect medium (0.39) or higher effect sizes for the mediator (path a) and intermediate (0.26) or higher for the outcome [path b; (Pan et al., Reference Pan, Liu, Miao and Yuan2018)]. For significant indirect effects, we conducted a post-hoc Monte Carlo power analysis to estimate the actual power achieved in the model (Schoemann, Boulton, & Short, Reference Schoemann, Boulton and Short2017). For interaction effects, a power analysis indicated that our moderation models were 80% powered to detect small-to-medium (f 2 ⩾ 0.08) or higher effect sizes for the interaction term coefficient.
Results
Eighty participants were equally randomized to CR (n = 40) and TAU (n = 40). Baseline sample characteristics are presented in Table 1. There were no missing data for participant characteristics and baseline variables, which were comparable between the two groups. For outcome measures, only the GAS was missing for two participants at baseline (one per group). Post-treatment and follow-up data were obtained for 90% and 88% of the participants, respectively. Missingness was balanced between groups (CR: 8%, TAU: 12%) and no baseline predictors of missingness were identified for any outcomes.
Table 1. Sample characteristics at baseline

BD, bipolar disorder; CR, cognitive remediation; HAMD, Hamilton Depression Rating Scale 17 items; TAU, treatment-as-usual; YMRS, Young Mania Rating Scale.
Outcome changes
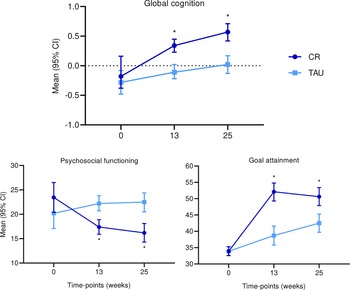
Participants receiving CR showed significant post-treatment improvements (week 13) compared to TAU participants (all p < 0.01) in individual cognitive tests and the global cognition composite score, which were maintained at follow-up (week 25; online Supplementary Table S1). This was also the case for the functional outcomes (FAST and GAS). Figure 2 illustrates the change trajectory from baseline to follow-up for global cognition and the two functional outcomes (for the FAST, score reduction indicates improvement). Change trajectories for cognitive domains are presented in online Supplementary Fig. S1.

Fig. 2. Unadjusted means (95% CI) of cognitive composite score and functional outcomes across time points per treatment group (*p < 0.01). CR, cognitive remediation; TAU, treatment as usual.
Mediation models
Post-treatment performance in global cognition partially mediated the effect of CR on the FAST at follow-up (indirect effect β = −0.23, 95% CI −0.51 to −0.04; online Supplementary Fig. 2), indicating that approximately 35% of the improvement in psychosocial functioning for the CR group was explained by cognitive gains (path a*b). The direct effect of CR on the FAST (path c′) also remained significant. A post-hoc power analysis for the indirect effect showed that this model achieved 0.89 power.
Indirect effects for individual cognitive domains as mediators of the CR effect on psychosocial functioning did not reach significance. Likewise, no cognitive variables mediated the treatment effect on goal attainment. For these models, the effects of putative mediators on the outcome were smaller than our sample size was powered for (all path b coefficients <0.25). Indirect, direct, and total effects for all mediation models are reported in online Supplementary Table 2.
Figure 3 illustrates the standardized indirect effects (95% CI) across cognitive variables tested as mediators for the FAST and the GAS. All mediated effects were negative for the FAST since these were the products of the positive effect of treatment on the mediator (path a) and the negative effect of the mediator on the outcome (path b). The opposite was observed for the GAS, where both the treatment-mediator and the mediator-outcome relationships were positive. There was no evidence of suppression (i.e. the direct and the indirect effect showing opposite directions).

Fig. 3. Standardized mediation effects of cognitive measures on psychosocial functioning and goal attainment. Indirect effects are standardized in s.d. units of the respective outcome. CR, cognitive remediation; ExF, executive functioning; FAST, functioning assessment short test; GAS, goal attainment scale; PrSp, processing speed; TAU, treatment-as-usual; VM, verbal memory; WM, working memory.
Moderation models
The effect of treatment on the GAS at follow-up was moderated by normative cognitive performance post therapy (interaction β = 0.78, 95% CI 0.08–1.55, p = 0.03). This corresponded to a small-to-medium moderating effect (f 2 = 0.09). As illustrated in Fig. 4, the effect of CR relative to TAU was not significant at week 25 for participants with a low cognitive level following therapy at week 13 (t = 0.98, p = 0.33), but it was significant for those achieving an average (t = 3.57, p = 0.001) or higher cognitive level (t = 4.08, p < 0.001). For our sample, the low level of normative cognitive performance corresponded to 0.5 s.d. below the population mean, with treatment effect on goal attainment not being significant for participants scoring at this level or lower. A similar pattern was observed for verbal memory, processing speed, and working memory (but not executive functioning), although these moderation effects did not reach significance (online Supplementary Table S3/Fig. S3).

Fig. 4. Treatment effect on goal attainment at study end moderated by the level of post-treatment global cognitive performance (*p < 0.01). CR, cognitive remediation; GAS, goal attainment scale; TAU, treatment-as-usual.
CR effect on the FAST at follow-up was not moderated by the post-treatment level of cognitive performance in the global cognition composite or the individual domains.
Discussion
To the best of our knowledge, this is the first study examining models of whether and how cognitive gains following CR translate into long-term functional improvements in euthymic people with BD. We considered two types of functional outcomes, a clinician-rated measure of psychosocial functioning and an idiosyncratic measure of recovery goals. Changes in global cognition were found to mediate the effect of CR on psychosocial functioning, but not goal attainment. However, the strength of the CR effect on goal attainment was moderated by cognition, with greater improvement for those with better cognitive performance following therapy. These findings support the theoretical assumption that cognitive changes are associated with functional improvement and provide initial evidence for this transfer in people with BD.
Does cognitive improvement transfer to functioning?
Mediation analysis indicates that improvement in global cognition accounts for more than one third (35%) of the CR effect on psychosocial functioning. This provides support for the theoretical model of CR, suggesting that functional difficulties can be reduced through improvements in cognition (Wykes & Spaulding, Reference Wykes and Spaulding2011), and is consistent with previous evidence of an indirect effect of cognition on functional outcomes in people with a diagnosis of schizophrenia (Reeder et al., Reference Reeder, Huddy, Cella, Taylor, Greenwood, Landau and Wykes2017; Wykes et al., Reference Wykes, Reeder, Huddy, Taylor, Wood, Ghirasim and Landau2012). Unlike these studies, which found executive functioning to be associated with functional changes, we detected a significant indirect effect only for global cognition (composite score), while individual domains accounted only for smaller proportions of the total CR effect (3–14%; online Supplementary Table 2). This was despite observing significant moderate-size improvements in every domain. A possible explanation may be that the variance of the composite score reflects the common features of all individual tests used to compute the composite which increases the likelihood of detecting significant associations with other outcomes (Song, Lin, Ward, & Fine, Reference Song, Lin, Ward and Fine2013).
The characteristics of the CR paradigm we used for CRiB may explain how cognitive changes exert an effect on psychosocial functioning (Strawbridge et al., Reference Strawbridge, Tsapekos, Hodsoll, Mantingh, Yalin, McCrone and Young2021). CIRCuiTS prompts the development and use of strategies to compensate for potential cognitive shortcomings, while a substantial part of therapy time is devoted to how participants can transfer newly acquired strategies and cognitive skills to daily-life activities and personal goals (Reeder et al., Reference Reeder, Pile, Crawford, Cella, Rose, Wykes and Callard2016). Conversely, a recently published randomized trial, assessing the effects of action-based CR on cognition and functioning in remitted patients with BD, did not detect a transfer of post-treatment cognitive changes to improved functioning at follow-up (Ott et al., Reference Ott, Vinberg, Kessing, Bowie, Forman and Miskowiak2020). This was despite employing strategy use to guide task practicing and bridging techniques to translate cognitive skills into everyday activities. However, CR recipients in this study attended fewer hours of therapy and showed smaller improvements in cognitive outcomes examined as putative mediators compared to CRiB, which might explain the absence of a significant transfer effect.
Although global cognitive improvement accounts for a substantial proportion of the total CR effect on psychosocial functioning, this leaves 65% of the total effect not explained by cognition; thus, changes in other factors may account for it. Improvement in metacognitive skills achieved following CR may be one of these factors. Metacognition refers to one's ability to understand, monitor, and manipulate their own cognitive processes (Flavell, Reference Flavell1979). In the context of CR, metacognitive skills are integral for regulating cognition and effective strategy use which enable acquiring new skills (Cella, Reeder, & Wykes, Reference Cella, Reeder and Wykes2015; Wykes & Reeder, Reference Wykes and Reeder2005). According to this model, metacognition contributes to the improvement of cognitive outcomes and primarily drives the CR effect on functioning. An improvement in metacognitive skills has previously been reported for people with schizophrenia after receiving CR with CIRCuiTS (Cella et al., Reference Cella, Edwards, Swan, Elliot, Reeder and Wykes2019). People with BD also present with maladaptive metacognitive skills which correlate with deficits across cognitive domains and may benefit from CR programmes emphasizing metacognitive training and transfer to daily-life skills, such as CIRCuiTS (Torres, Mackala, Kozicky, & Yatham, Reference Torres, Mackala, Kozicky and Yatham2016; Van Camp, Sabbe, & Oldenburg, Reference Van Camp, Sabbe and Oldenburg2019). Functional competence is another factor potentially accounting for psychosocial functioning improvements following CR. According to cross-sectional findings, functional competence partially mediates the relationship between cognition and daily-life functioning (e.g. community activities, work skills) in people with BD (Bowie et al., Reference Bowie, Depp, McGrath, Wolyniec, Mausbach, Thornquist and Pulver2010). This sequential transfer model considering both cognition and functional competence as factors driving CR effects is an interesting perspective for future research.
Mediation models for the GAS suggest that therapy derived cognitive improvements did not account for changes in goal attainment. However, we found that the cognitive level achieved following therapy accounts for differences in goal attainment between CR recipients since only those performing above a certain level (−0.5 s.d.) showed significant functional gains compared to the TAU group. Indeed, cognitive level even before the therapy may affect subsequent functional improvement, although the direction of this moderation effect is inconsistent across the literature, as recently shown by a systematic review of CR studies for people with schizophrenia (Seccomandi, Tsapekos, Newbery, Wykes, & Cella, Reference Seccomandi, Tsapekos, Newbery, Wykes and Cella2020). A possible explanation for our findings is that a minimum level of cognitive competence is necessary to implement skills and strategies to achieve personal goals. We did not observe a similar pattern for TAU participants achieving high levels of cognitive performance which suggests the importance of CR (and not only pre-existing high cognitive skills) for attaining such goals. Unlike goal attainment, there was no evidence of moderation for psychosocial functioning, suggesting that improvement did not depend on the normative level of cognitive performance following therapy.
This study offers initial evidence on CR transfer mechanisms between cognition and functioning for people with BD. Our analysis provides a framework for future mechanism evaluation trials. An examination of different mechanisms leading to functional improvement in the trial design is crucial for establishing the importance of CR for long-term functional recovery. Our findings primarily support the role of global cognition for the transfer of CR effects to functioning. Although composite scores are recommended by the ISBD as more sensitive and robust cognitive measures (Miskowiak et al., Reference Miskowiak, Burdick, Martinez-Aran, Bonnin, Bowie, Carvalho and Vieta2017), more comprehensive studies will need to parse out the role of different cognitive domains, as well as examine other factors (e.g. metacognition) putatively exerting an effect on functioning.
Strengths and limitations
Unlike previous research in BD, this study relied on a robust methodological approach to examine the transfer of improved cognitive skills to functional outcomes, using bootstrapping to estimate confidence intervals for indirect and interaction effects. Examined models of transfer were informed by theory of CR and previous research in people with schizophrenia (Wykes & Reeder, Reference Wykes and Reeder2005, Wykes et al., Reference Wykes, Reeder, Huddy, Taylor, Wood, Ghirasim and Landau2012). In addition, our models adhered to a temporal precedence of cognitive over functional outcomes, increasing our ability to interpret the mediating and moderating effects as transfer mechanisms. Finally, we used data from a high-quality randomized trial with few dropouts, and high levels of treatment adherence. Random group allocation and a high retention rate reduce the potential influence of confounding factors.
Relatively small sample size and complete case analysis might introduce bias and limit the study conclusions but a post-hoc power analysis indicated that we had sufficient power to detect an indirect effect of cognition on functioning and no patterns of missingness were identified, suggesting that biased estimations due to missing data were unlikely. A further limitation might be unmeasured or hidden confounding in the non-randomized relationship between mediator and outcome. However, we controlled for plausible confounding factors and baseline scores to minimize residual confounding in this relationship and reduce bias in the indirect effect estimates. We did not consider models of transfer using perceived cognitive performance as a mediator/moderator because CR did not have a significant post-treatment impact on subjective cognitive complaints and any associations with functioning could therefore not be attributed to the effects of the therapy. However, this should be explored by future studies given the relationship between subjective complaints and functioning (Samalin et al., Reference Samalin, Boyer, Murru, Pacchiarotti, Reinares, Bonnin and Vieta2017). Finally, variables analyzed as mediators/moderators and outcomes were potentially subject to measurement error. However, this is unlikely to cause type I errors (i.e. false positives), and we also used validated measures and trained assessors to reduce measurement error as much as possible.
Conclusions
Our findings suggest that enhancing cognition may lead to improvements in functioning, initially supporting the theoretical model for the mechanism of action of CR. Gaining cognitive skills might account for a substantial proportion of the CR effect on psychosocial functioning, while achieving a minimum level of cognitive performance following CR might be necessary for a significant therapeutic effect on goal attainment. Mechanism evaluation trials are warranted to ratify the putative transfer mechanisms following CR.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291721002336
Acknowledgements
We are grateful to all CRiB study participants, service user representatives, and all students and researchers from Centre for Affective Disorders who contributed to the CRiB study. We also thank King's College Hospital Clinical Research Facility and King's College Clinical Trials Unit, OPTIMA mood disorders service and SLaM Affective Disorders Service.
Author contributions
DT, AHY and TW conceived the study idea and planned this study. DT and RS were involved in data collection. DT carried out the analysis and prepared the first manuscript with support from RS. MC, AHY and TW supervised the project. All authors provided feedback, contributed to the final draft of the paper and approved the manuscript.
Financial support
This paper represents independent research part-funded by the National Institute for Health Research (NIHR) Maudsley Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King's College London. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. DT would like to acknowledge that this scientific paper was supported by the Onassis Foundation – Scholarship ID: F ZO077-1/2018-2019. AHY and TW would like to acknowledge their NIHR Senior Investigator award.
Conflict of interest
AHY reports paid lectures and advisory boards for the following companies with drugs used in affective and related disorders: AstraZeneca (AZ), Eli Lilly, Lundbeck, Sunovion, Servier, LivaNova, Allegan, Bionomics, Sumitomo, Dainippon Pharma and Janssen; consultant to Johnson & Johnson and LivaNova; principal investigator on the Restore-Life VNS registry study funded by LivaNova, on ESKETINTRD3004 trial funded by Janssen, and the p-TRD trial funded by Compass; no shareholdings in pharmaceutical companies. RS reports a paid lecture from Lundbeck. TW is the creator of CIRCuiTS cognitive remediation software. DT and MC report no conflict of interest for this work.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human patients were approved by the City Road & Hampstead NHS Research Ethics Committee (reference 15/LO/1557).