Grief is the price of love. It is the ‘cost of commitment’, as Colin Murray Parkes entitles the opening chapter of his seminal work Bereavement: Studies of Grief in Adult Life (Reference ParkesParkes, 1986). Just as close attachment relationships (which may not always be loving) are a near-universal human experience, so grief following the permanent loss of such a relationship is a normal part of being human. It is also one of the most intensely painful of all human experiences.
What is the role, if any, of professionals in contact with people who are going through an intensely painful but natural process? What are the indications that the process of bereavement is not pursuing a natural course, and what can mental health professionals offer in these circumstances? To address these questions, we need first to turn to what is known about the natural process of grief.
The anatomy of natural grief
We owe a great debt to John Bowlby and his colleague Colin Murray Parkes for their clarification of the key elements of natural grief (Reference BowlbyBowlby, 1980; Reference ParkesParkes, 1986). For both, grief was an extension of the natural human response to separation. Just as physical trauma to the body evokes the inflammatory response – redness, swelling, heat and pain – so the psychological trauma of loss leads to a sequence of natural experiences, as detailed in Box 1.
Box 1 Phases of normal grief reaction
| Phase I | Shock and protest – includes numbness, disbelief and acute dysphoria |
| Phase II | Preoccupation – includes yearning, searching and anger |
| Phase III | Disorganisation – includes despair and acceptance of loss |
| Phase IV | Resolution |
Bowlby was at pains to stress that these phases are not clear-cut and that bereaved individuals may for a time oscillate back and forth between any two phases. He was also reluctant to detail a precise timescale for progression through these phases, noting the impact of the culturally diverse rites and rituals of mourning. He also suggested that timescales can reflect more the wishes of those witnessing a person's grief rather than the individual's natural process. With these provisos, it is generally accepted within Western culture (e.g. Royal College of Psychiatrists, 1997) that the initial response is one of shock, emotional numbness and disbelief. Within a few days, this gives way to agitation and pining for the dead person. Agitation is at its worst at around 2 weeks, usually giving way to depressive symptoms, which peak at about 4–6 weeks after the death. Pangs of grief may occur at any time, sparked off by people, places or things that bring back memories of the dead person. As time passes, the intense pain of early bereavement begins to fade. The depression lessens and it is possible to think about other things and even to look again to the future. Most people recover from a major bereavement within 1–2 years.
Psychological theories of grief
In his classic paper Mourning and Melancholia(1917), Freud observed that although these two states of mind have a number of similarities, such as profound dejection and loss of interest, they are distinguished by the presence, in melancholia, of a marked lowering of self-regard. He explained this by proposing that in melancholia ‘the self-reproaches are reproaches against a loved object which have shifted away from it onto the patient's ego’ (Reference Freud and StracheyFreud, 1917: p. 248). Thus, the ego internalises the lost person, ‘the shadow of the object falls upon the ego’ (p. 249), and both ego and object fall under the harsh judgement of a critical agency, a concept later developed into the super-ego. By contrast, Freud suggested that in normal mourning there is no process of identification and internalisation, but rather a gradual withdrawal of libido from the lost person. Once this task is completed the libido is ‘free’ to be invested elsewhere. Mourning and Melancholia is such a seminal paper that Freud's subsequent thoughts about mourning are not always given the attention they deserve. By the time he wrote The Ego and the Id (1923), he recognised that the withdrawal of the libido that attaches one person to another can take place only when the lost person has been ‘reinstated’ within the ego.
Melanie Klein developed this notion further. Drawing on her own experience of mourning for her son, who died in a climbing accident, she suggested that in adult mourning we revisit early experiences of mourning for a lost other:
‘My contention is that the child goes through states of mind comparable to the mourning of the adult, or rather, that this early experience is revived whenever grief is experienced in later life’ (Reference KleinKlein, 1940: p. 344).
In ‘good enough’ early experiences, we repeatedly lose and refind our loved objects. Through the cumulative effects of many such experiences as a child, we internalise a sense of a present loved other. This cumulative process of internalisation will be hindered if the child experiences major separations from or loss of loved ones. Klein went on to say that when we are bereaved as adults we fear that we have lost not just this loved one, but also our internalised loved ones:
‘Through the work of mourning [the bereaved individual] is reinstating all his loved internal objects which he feels he has lost … Every advance in the process of mourning results in a deepening of the individual's relation to his inner objects, in the happiness of regaining them when they were felt to be lost’ (p. 362).
The clinical significance of her theory is that, if individuals have not had the early experiences that enable them to internalise a good object, then mourning as adults will be complicated by significant depression.
Bowlby's thoughts on loss and grief were developed over a period of decades and are expressed most completely in his book Loss: Sadness and Depression(1980). His ethological attachment perspective allowed him to draw direct parallels between an infant's response to separation from its attachment figure and the phenomenology of grief. He proposed that the absence of an attachment figure activates an innate motivational system that compels the individual to search for the person and to do everything possible to regain that person's proximity and care. When these efforts fail, the bereaved individual experiences profound sorrow and despair. Through the work of mourning, the bereaved individual reorganises his or her representations of the world in a way that allows a return to normal activities and the seeking out or renewal of social relationships.
In summary, it seems that the natural process of grieving allows the bereaved eventually to reinstate or refind some aspect of the person they have lost. The beginning of this process is movingly described in C. S. Lewis's account of his personal grief following the death of his wife, whom he refers to as H.:
‘And suddenly at the very moment when so far I mourned H. least, I remembered her best. Indeed it was something (almost) better than memory; an instantaneous unanswerable impression. To say it was a meeting would be going too far. Yet there was that in it which tempts one to use those words. It was as if the lifting of sorrow removed a barrier … Why has no-one told me of these things? How easily I might have misjudged another man in the same situation? I might have said, “He's got over it. He's forgotten his wife,” when the truth was, “He remembers her better because he has partly got over it”’ (Reference LewisLewis, 1966: p. 37).
Unnatural grief
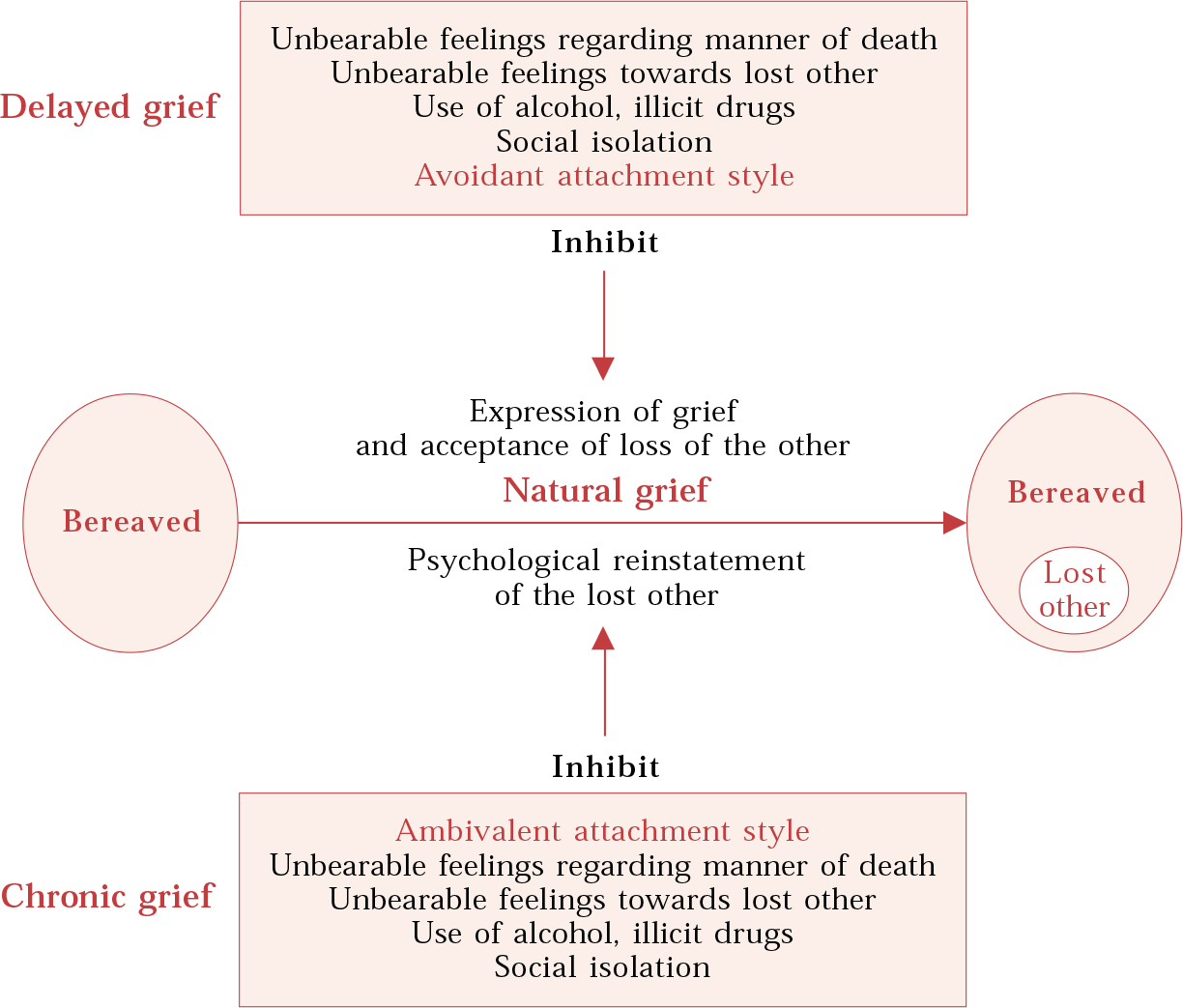
Following Bowlby, ‘pathological grief’ is usually subdivided into inhibited, delayed and chronic grief (Box 2). This can be thought of simply as ‘too little’ (inhibited or delayed) or ‘too much’ (chronic) grief. I find it useful to think of inhibited/delayed grief as being related to factors that get in the way of the expression of grief and acceptance of loss, whereas chronic grief is associated with factors that inhibit the process of reinstatement (Fig. 1).
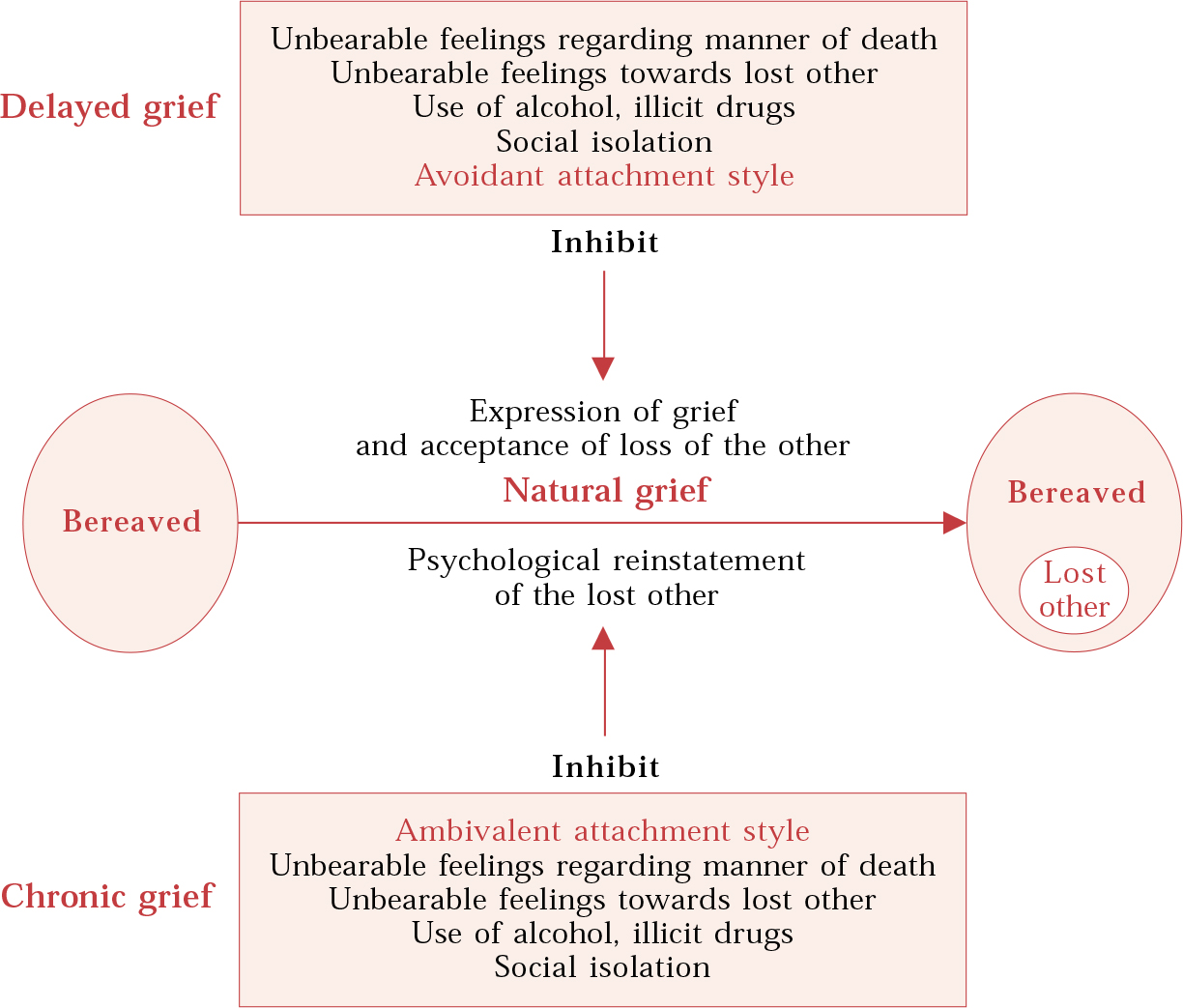
Fig. 1 Some factors that inhibit the natural grief process.
Box 2 Types of pathological grief
| Inhibited grief | Absence of expected grief symptoms at any stage |
| Delayed grief | Avoidance of painful symptoms within 2 weeks of loss |
| Chronic grief | Continued significant grief-related symptoms 6 months after loss |
Inhibited/delayed grief
Bowlby suggested that delayed grief is more common in people with avoidant attachment styles. They often see expression of feeling as a sign of weakness or as an invitation to ridicule. They usually have an early history in which expression of feeling was either actively discouraged or felt to be unsafe because of the unresponsiveness of caregivers. This leads to personality traits such as excessive self-reliance or compulsive caregiving. Such people find it hard to express any strong feeling, let alone one as intensely painful as grief.
Lack of family support and social isolation may also contribute to delayed grief reactions (Reference BowlbyBowlby, 1980). For example, Reference Maddison and ViolaMaddison & Viola (1968), in a study of 40 widows in Boston, USA, found that those who had a close ongoing relationship with their mother had better outcomes than those who had little contact with their mother.
The expression of grief may also be inhibited by the sheer unbearable intensity of feeling towards the lost other or over the manner of the loss. Thus, if the bereaved person feels guilty about unresolved issues in relation to the lost other or feels especially angry towards them, they may be unable to express their grief, fearing that such feelings are unacceptable (‘Don't speak ill of the dead’). The manner of death may be associated with intense guilt (‘If only I had been there for him’) or anger (‘If only the doctors had diagnosed the condition sooner’). Death by murder or suicide is associated with such overwhelming feelings of helpless anger and guilt that bereaved individuals often feel that no one could bear the intensity of their feelings. Compared with other types of bereavement, bereavement by suicide is more commonly characterised by stigmatisation, shame, guilt and a sense of rejection (Reference Hawton and SimkinHawton & Simkin, 2003).
Chronic grief
This seems to be more common in people who have had an overly dependent relationship to the lost other. In attachment language, they usually have an ambivalent attachment style. These are the people that Parkes described as having a ‘grief-prone personality’ (Reference ParkesParkes, 1985). Their previous relationships are usually haunted by an overriding fear of losing the other. Bowlby thought that these expectations were based on early experiences of discontinuities in parenting and/or frequent rejection by parents. As a result of such experiences, these children struggled to internalise a good object and so their mourning as adults is complicated by protracted attempts to refind a good object and reinstate the lost other. The chronic grief is a chronic searching for something that cannot be found internally. The process of reinstatement may also be complicated by hateful or fearful feelings towards the lost other. For example, if the lost other was an abusive, frightening mother, then refinding aspects of her internally is inevitably disturbing.
Psychiatric sequelae of pathological grief
In pathological grief, the mental health professional will need to make an assessment of the nature of any psychiatric disorder and associated risk. Community studies show that 50% of bereaved spouses meet the criteria for a major depressive episode at some point in the first year following their loss, but this will usually have resolved by 6 months; 10% suffer from depression for the entire year (Reference Mitchell, House, Gelder, Lopez-Ibor and AndreassenMitchell & House, 2000). The features that distinguish major depression from a normal grief response are listed in Box 3. In a small US study of bereaved spouses (n=54), Reference Jacobs, Hansen and KaslJacobs et al(1990) found that 24 (44%) developed an anxiety disorder during the first year of their loss and 5 (9%) developed the symptoms of post-traumatic stress disorder. If pharmacological treatment is indicated, then this should be prescribed as for non-bereaved individuals, bearing in mind that certain medication, particularly anxiolytics, can inhibit the natural grief process.
Box 3 Clinical features suggesting a major depressive episode rather than normal grief
-
• Guilt about things other than actions taken or not taken by the survivor at the time of the death
-
• Thoughts of death except in relation to the deceased
-
• Feelings of worthlessness
-
• Psychomotor retardation
-
• Prolonged and marked functional impairment
-
• Hallucinations except in relation to the deceased
Evidence base for grief work
As far as psychological treatments are concerned, there is a dearth of literature about effective treatments. Reference RaphaelRaphael (1977) found that preventive interventions in the early bereavement period were effective for widows at high risk of pathological grief. The risk factors selected were lack of support from social networks, previous highly ambivalent relationship with the deceased and the presence of at least three concurrent stressful life events.
The treatment group in Raphael's study received an average of four 2-hour sessions of counselling. Of 200 high-risk widows, 77% in the treatment group were improved 13 months after their husband's death and 23% were unimproved, compared with 41% improved and 59% unimproved in the untreated group. Reference Marmar, Horowitz and WeissMarmar et al(1988), also in the USA, reported a randomised controlled trial of brief psychodynamic psychotherapy v. mutual-help group treatment for widows who had sought treatment for unresolved grief reactions between 4 months and 3 years after the death of their husband. Women in both groups experienced a reduction in stress-specific and general psychiatric symptoms as well as improvement in social and work functioning. The two treatments were equally effective, although there was greater attrition of numbers in the group treatment condition.
Principles of grief work
For professionals meeting newly bereaved individuals, Reference ParkesParkes (1986) gives some helpful words of wisdom:
‘Do nothing that will inhibit the expression of appropriate grief … The bereaved person has a painful and difficult task to perform which cannot be avoided or rushed. True help consists in recognising this fact and in helping the bereaved to arrange things in whatever way is necessary to set him or her free for the task of grieving’ (p. 174).
Support from family and friends is crucial at this stage. Voluntary organisations such as CRUSE and Compassionate Friends (in the UK) are also able to offer significant support, especially through opportunities to meet with other bereaved individuals.
Mental health professionals will work with grief in many different settings, for example on hospital wards or in the community, and in many different roles, perhaps as part of a treating team or as a single therapist. However, whatever the setting or role, the following principles are important.
Providing a secure base
The ‘secure base’ is a term coined by Bowlby to describe the role of the caregiver to whom a child turns when distressed. The concept has been usefully extended to psychotherapeutic work with adults (Reference HolmesHolmes, 2001). As well as referring to an actual person who provides a sense of security, the concept also refers to a representation of security within the individual's mind. Attention to the physical and psychological setting of grief work can allow the grieving patient to feel safe to explore painful feelings. Consistency of venue, personnel and timing (including protection from interruptions) will all help to create the experience of a secure base.
Facilitating the expression of grief
In Shakespeare's Macbeth, after MacDuff learns that his family have been killed, Malcolm comforts him:
‘Ne'er pull your hat upon your brows;
Give sorrow words. The grief that does not speak
Whispers the o'erfraught heart and bids it break’
(Macbeth, Act IV, Scene iii, line 208).
The bereaved need to feel that their grief is speakable and hearable. They may use a variety of avoidance strategies to protect themselves from the pain of grief. These will need to be explored with due respect for their defensive function. If alcohol, illicit drugs or anxiolytic medication are being used to dampen down distress, this needs to be addressed at an early stage in the grief work. Considerable time may be needed to explore a patient's fear of expressing grief. For example, they may fear that if they start crying they will never stop, that no one will be able to bear their pain. This links with Bion's helpful concept of containment (Reference Symington and SymingtonSymington & Symington, 1996). If the professional can contain the pain of grief, then this can help the patient internalise a sense that their pain can be borne and thought about. Patients can also fear being be severely judged if they express their grief (‘They all say I should be over it by now’). Professionals, like Malcolm, need to indicate by their words and non-verbal communication that they are prepared to listen in an accepting, non-judgemental manner.
Clinical example 1
Mr A was a 30-year-old single man who worked as a nurse. His mother had died a year ago from breast cancer. He developed a depressive episode characterised by intense feelings of guilt for not having been present when she died. He had nursed her during her final illness but on the night of her death had been out with a friend. He was unable to visit his mother's grave or sort out her belongings. He was unable to function at work. His guilt eventually drove him to take an overdose, which led to his psychiatric referral.
Grief work involved exploring his relationship with his mother. He had always felt that his older brother was the favoured child and that he could not do anything right in his mother's eyes. He recalled that she had been very busy running a centre for homeless adults and so had had very little time for her two sons. Initially, Mr A was reluctant to voice any difficult feelings towards his mother, fearing this would be disloyal. Instead, he spoke admiringly of her devotion to her work. As the therapy progressed, Mr A was able to acknowledge angry feelings towards his mother and that these might have been stirred up while he was nursing her before she died. Eventually, he was able to understand some of the difficulties that his mother must have faced in her life, which allowed him to be more accepting of her tendency to put her work before child care. He became able to visit his mother's grave, sort out her belongings and return to work.
Some patients may need encouragement to face reminders of their grief so that their feelings can be brought to the fore. This might involve addressing issues such as sorting out belongings or visiting the grave. Some authors advocate a behavioural approach to this, known as guided mourning. This approach ‘likens unresolved grief to other forms of phobic avoidance, which have been treated successfully by exposure to the avoided situation’ (Reference Mawson, Marks and RammMawson et al, 1981). Mawson et al summarise guided mourning as involving an ‘intense reliving of avoided painful memories and feelings associated with bereavement’. During treatment, patients are exposed both in imagination and in real life to avoided or painful memories or situations related to the loss of their loved one. This might include visiting the cemetery, looking at photographs or handling possessions of the deceased.
Revealing feelings that block natural grieving
The professional needs to help the bereaved person to recognise and name the difficult feelings that are blocking the natural grief process. These may include anger, guilt, shame, hatred or fear. Again, recognising these feelings may require groundwork exploring why the feelings may not be acceptable to the individual.
Making sense of these feelings
Helping a grieving person to make sense of and understand these feelings will require discussion of the individual's relationship to the lost other and how this relationship might follow a particular pattern of relating to others.
Clinical example 2
Mrs B was a 50-year-old woman married to a 35-year-old man. She had two daughters, aged 19 and 20, from a previous marriage. She became depressed following the collapse of her catering business and increasing estrangement from her second husband. Her daughters had recently left home and she no longer felt she had a role in the family. She presented to psychiatric services in a highly suicidal state and was admitted to a psychiatric ward. On detailed exploration of her suicidal thoughts and fantasies it emerged that she longed to reunite with her first boyfriend, a young Italian, whom she had known 30 years previously. They had known each other for a year before he was killed in a car accident at the age of 20. The accident happened following an argument with Mrs B, which she felt caused him to lose concentration while driving – with fatal consequences. In many of her subsequent relationships she had sought to recreate this first relationship. Significantly, she had married her second husband when he was 20. When this relationship faltered and other roles changed, her only hope of recreating her first love relationship as an adult was to ‘join him in death’.
Grief work involved exploring her chronic grief for her Italian boyfriend. In her early history, it emerged that she was the oldest of four children to an Italian father and English mother. Her father had been an alcoholic and her mother had struggled coping with four children, marital disharmony and poverty. As the oldest child, Mrs B had helped her mother look after younger siblings, but felt unable to express her own emotional needs, becoming a highly independent girl. She longed for her father's loving attention, but he was rarely able to provide this. During the course of grief work she was able to reflect on how her Italian boyfriend had provided her with an experience of being loved and cared for that she had longed for from her own father. Her grief at her boyfriend's death could then be seen as an extension of her more hidden grief for her father's love. These issues were explored over eight sessions and this enabled her to leave hospital with some hope of finding a renewed purpose in her life through voluntary work.
Addressing social isolation
It is easy for the bereaved to feel that others have not experienced pain like theirs and do not understand. Encouraging ongoing contact with family and friends or with others who have been bereaved (e.g. using organisations such as CRUSE) is important.
Showing the universality of grief
Ultimately, one of the most helpful realisations for the bereaved is recognition that what they are experiencing is known the world over and has been known since time immemorial. This is where literature, poetry, music and art can offer so much solace. In her first novel, Our Father Who Art in a Tree, Judy Reference PascoePascoe (2002) gives a powerful description of a family grieving for their father. The 20th-century English composer Herbert Howells composed his choral masterpiece Hymnus Paradisi in memory of his son, Michael, who died as a boy. Both works are less familiar examples of the many works of art that express grief in a deeply moving way.
Addressing spiritual beliefs
Grief can only be fully worked with if the professional has some understanding of the bereaved person's perspective on what lies on the other side of death. It is so easy to neglect this or assume that the bereaved person shares one's own perspective. It surely matters whether the bereaved believes that death is a final and complete end or a gateway to a different state of being.
Supervision
Clinical example 3
In the supervision of a psychotherapist's work with Mr C, a depressed father who had lost his daughter 2 years earlier from a brain tumour at the age of 10, a number of important issues emerged. When the therapist first reported the case he made a slip of the tongue, referring to the lost daughter as Mr C's wife. Reflecting on this we were able to discern the degree to which Mr C's relationship with his daughter, in particular their mutual love of football, had become a substitute for his hollow and unsustaining relationship with his grieving wife. Thus, grief for his daughter was mixed with grief for the relationship he did not have with his wife and had not had with his depressed mother. This became an important part of the therapy. As the work proceeded, the pain of Mr C's grief became difficult to listen to for the therapist who, as a father of a young daughter himself, imagined what it might be like to lose her. Supervision was important to enable the therapist to bear the patient's distress. After 20 sessions the therapy ended with signs that Mr C's marital relationship was beginning to improve. He was also able to take up his love of football again with the poignant associated memories of his daughter's enjoyment of the game. Working with grief can be challenging for professionals. Overzealous attempts to make things better or an unwillingness to hear and think about the pain of grief are commonplace. Many professionals will be confronted with reminders of their own experiences of grief and this can either interfere with or enhance their capacity to help. Self-reflection and supervision are crucial if professionals are to make best use of their humanity.
Multiple choice questions
-
1 The following features are consistent with a normal grief reaction:
-
a disbelief 1 month after loss
-
b depressive symptoms 6 weeks after loss
-
c hearing the voice of the deceased
-
d significant functional impairment at 6 months
-
e pangs of grief on the anniversary of the loss.
-
-
2 After a bereavement, the following features are strongly suggestive of a major depressive episode:
-
a a profound sense of worthlessness
-
b a transient wish to join the deceased in death
-
c guilt over not having been present at the time of death
-
d transient visual hallucinations of the deceased
-
e psychomotor retardation.
-
-
3 Factors contributing to delayed grief include:
-
a a secure attachment style
-
b excessive alcohol consumption
-
c lack of social support
-
d the lost other's death by suicide
-
e a close relationship with surviving family.
-
-
4 In grief work:
-
a medication is never appropriate
-
b Bowlby's concept of the ‘secure base’ is important
-
c grief avoidance may be treated by exposure therapy
-
d poetry can play a useful role
-
e a person's spiritual beliefs are irrelevant.
-
-
5 Supervision of grief work:
-
a can help professionals to distinguish between the patient's grief and their own
-
b can prevent overzealous attempts to cure grief
-
c can enhance a professional's capacity for self-reflection
-
d can help a therapist bear the pain of the patient's grief
-
e should discourage ordinary human responses to a patient's grief.
-
MCQ answers

| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | F | a | T | a | F | a | F | a | T |
| b | T | b | F | b | T | b | T | b | T |
| c | T | c | F | c | T | c | T | c | T |
| d | F | d | F | d | T | d | T | d | T |
| e | T | e | T | e | F | e | F | e | F |



eLetters
No eLetters have been published for this article.