Colorectal cancer (CRC) is a multi-factorial disease, the incidence of which is related in particular to a ‘Western’ diet and lifestyle but also to genetic and hormonal factors(Reference Chan and Giovannucci1, Reference Strate and Syngal2). It has been estimated that more than 40 % of CRC cases in Western countries could be prevented by appropriate food, nutrition, physical activity and body weight(3).
Emerging evidence of a probable protective role of the Mediterranean dietary pattern against cancer, especially in cohorts in the USA(Reference Verberne, Bach-Faig and Buckland4), has led to the suggestion that American and northern European populations should adapt to this diet. In the large National Institutes of Health-American Association of Retired Persons Diet and Health Study (NIH-AARP) Diet and Health Study in the USA, a cohort study of 3110 incident cases of CRC and 5 years of follow-up, compliance with a Mediterranean diet was associated with a 28 % lower incidence of CRC in men but not in women(Reference Reedy, Mitrou and Krebs-Smith5). In a more recent study in the USA, based on the Nurses' Health Study and the Health Professionals Follow-up Study of 1432 cases of CRC, no significant effect of the Mediterranean diet was found on the incidence of CRC(Reference Fung, Hu and Wu6). In a Danish intervention study, the dropout rate was much higher in the group assigned to the Mediterranean diet than in that assigned to a low-fat diet, suggesting that participants might more readily comply with a ‘traditional’ diet than with a foreign diet(Reference Astrup7, Reference Due, Larsen and Mu8). In countries outside the Mediterranean region, promotion of a healthy diet based on local items might be more relevant and feasible(Reference Bere and Brug9).
As the Nordic diet is in general rich in unhealthy foods, such as margarine and sugar, it would not be relevant to study the health effects of the overall Nordic diet(Reference Slimani, Fahey and Welch10). This diet does, however, also include a range of foods with anticipated health-promoting effects, such as whole-grain cereals and fish. In order to determine whether selected healthy food items in the Nordic diet have positive health effects, we evaluated a healthy Nordic food index consisting of six items that are part of traditional Nordic cuisine: fish, cabbage, rye bread, oatmeal, apples and pears, and root vegetables. In a previous study, adherence to a healthy Nordic food index was associated with lower total mortality(Reference Olsen, Egeberg and Halkjaer11). Moreover, a diet rich in whole-grain products, including rye bread and oatmeal, was associated with a lower incidence of colon cancer among men(Reference Egeberg, Olsen and Loft12). The aim of the study reported here was to elucidate whether adherence to a healthy Nordic food index was associated with a lower incidence of CRC in a cohort of Danish men and women.
Materials and methods
Study population
The Danish Diet, Cancer and Health prospective cohort study was initiated in 1993. During 1993–7, 80 996 men and 79 729 women aged 50–64 years were invited to participate in the study, representing 19 % of the Danish population in that age group. Those invited also had to have been born in Denmark, have no diagnosis of cancer registered in the Danish Cancer Registry and live in the municipality of Copenhagen, Frederiksberg, Aarhus, Hinnerup or Hørning at the time of invitation. The participation rate was 37 % for women and 34 % for men, resulting in a cohort of 57 053(Reference Tjonneland, Olsen and Boll13). The study was approved by the relevant scientific committees and the Danish Data Protection Agency, and all the participants gave written consent. All participants filled in a questionnaire including questions on social factors, health status, reproductive factors and lifestyle at the study centres; anthropometric measurements (height, weight and waist circumference) were made by a laboratory technician(Reference Tjonneland, Olsen and Boll13).
Of the 57 053 members of the Diet, Cancer and Health cohort, 572 were excluded because of a diagnosis of cancer before baseline. Another thirty-seven were excluded because they did not fill in the questionnaire, 564 were excluded because of missing information on variables of interest for this study: fish intake, rye bread intake, anthropometrics, education, smoking status, use of non-steroidal anti-inflammatory drugs and use of hormone replacement therapy (for women). The resulting cohort consisted of 55 880 participants, of whom 29 216 were women and 26 664 were men.
Case ascertainment and selection
All participants were followed-up from the date of their visit to the centre by the personal identification number assigned to all Danish inhabitants. They were followed-up until censoring, which was the date of diagnosis of any cancer (except non-melanoma skin cancer), date of death, date of emigration or end of follow-up (31 December 2009). Information on cancer was obtained by linkage with the Danish Cancer Registry, which holds information on all cancer cases in Denmark(Reference Gjerstorff14).
There were 1035 incident cases of CRC between baseline and the end of follow-up, but ten were excluded because of missing information on the questionnaire, leaving 1025 cases for the present study. CRC cases were identified as codes C18–C20 in the 10th revision of the International Statistical Classification of Diseases, Injury and Causes of Death (ICD-10), which include all first incident primary adenocarcinomas; proximal colon cancers, of the caecum, appendix, ascending colon, hepatic flexure, transverse colon and splenic flexure (C18:0–C18:5); and distal colon cancers, of the descending (C18:6) and sigmoid colon (C18:7). Overlapping (C18:8) and unspecified lesions (C18:9) of the colon and cancers of the rectosigmoid junction (C19) were grouped with all colon cancers only. Cancers of the rectum (C20) were assessed both separately and with all colon cancer as CRC (C18–C20).
Dietary assessment
Before their visit to the study centre, the participants were asked to fill in a 192-item FFQ, which has been validated(Reference Overvad, Tjonneland and Haraldsdottir15, Reference Tjonneland, Overvad and Haraldsdottir16). The participants were asked to report their habitual intake of food items within the past 12 months in twelve categories ranging from never to more than eight times a day. The intakes of specific foods were calculated with the software program FoodCalc(Reference Lauritzen17). At the study centre, the FFQ were scanned optically and checked for missing values and reading errors. Uncertainties were cleared up with the participants by the laboratory technician during the visit(Reference Tjonneland, Olsen and Boll13).
The healthy Nordic food index was based on traditional Nordic foods chosen a priori on the basis of expected health benefits. The food items had to be present naturally in the Nordic countries, to already be an essential part of the Nordic diet, and information on the food items should be available from the FFQ. The food items used as exposure variables in the study were fish, cabbage, rye bread, oatmeal, apples and pears, and root vegetables. Information on intake of fish, cabbage, apples and pears, and root vegetables was obtained from multiple questions in the FFQ, whereas intake of oatmeal and rye bread was derived from one question each. Intake of fish was based on answers to twenty-three questions on a variety of fish and fish products eaten as hot meals or in open sandwiches. Information on intake of the Brassicaceae cauliflower, brussels sprouts, broccoli, kale, white cabbage and red cabbage was derived from answers to six questions. Consumption of apples and pears was inferred from the answers to two questions. That of root vegetables was derived from several questions on the intake of raw and cooked vegetables separately and as part of a recipe; carrots were the main root vegetables consumed.
The healthy Nordic food index was scored in accordance with those for the Mediterranean diet constructed by Trichopoulou et al. (Reference Trichopoulou, Kouris-Blazos and Wahlqvist18, Reference Trichopoulou, Costacou and Bamia19). Here, 1 point was given for an intake equal to or greater than the sex-specific median for each food category. As information on oatmeal and rye bread intake was derived from only one question each, it could not be divided into equal groups; the cut-off values were therefore defined from sex-specific spline curves with boundaries at predefined questionnaire categories.
In the scoring, 1 point was given for intake as follows: for men, fish ≥ 42 g/d; cabbage ≥ 14 g/d; rye bread ≥ 113 g/d; oatmeal ≥ 50 g/d; apples and pears ≥ 56 g/d; root vegetables ≥ 16 g/d; for women, fish ≥ 35 g/d; cabbages ≥ 16 g/d; rye bread ≥ 63 g/d; oatmeal ≥ 50 g/d; apples and pears ≥ 71 g/d; root vegetables ≥ 29 g/d. A score of 0 or 1 was given to each participant for each of the six dietary components in the index, so that each participant could score between 0 (poorest adherence) and 6 points (best adherence). As few participants had 0 or 6 points, we pooled the groups with 0 or 1 point and the groups with 5 or 6 points.
Statistical analyses
Cox proportional hazard models were used to estimate incidence rate ratios (IRR), with age as the underlying time axis. All quantitative variables were entered linearly into the Cox model(Reference Greenland20). Linearity of the associations was evaluated graphically by linear splines with three boundaries placed at quartiles of cases(Reference Greenland21). Time under study was the time-dependent variable and modelled as a linear spline with boundaries at 1, 2 and 3 years after entry into the study to allow for different underlying hazards during the first years of follow-up.
All the estimates are presented as both crude unadjusted and adjusted estimates. Overall, three adjustments were made. Of these, one adjustment was made for factors known to be associated with CRC: alcohol intake (any consumption, yes/no and g/d), smoking status (current, former, never), use of hormone replacement therapy (current, former, never), schooling (low: ≤ 7 years, medium: 8–10 years, and high: ≥ 10 years), participation in sports activities (yes/no), use of non-steroidal anti-inflammatory drugs (yes/no; yes: taken at least once a month within the past year), waist circumference (cm) and meat intake (g/d of red and processed meat). Another adjustment was made with the same factors and also energy (kJ/d, excluding alcohol). A final adjustment was made for Ca (dietary, dietary supplements), vitamin D (dietary, dietary supplements) and dietary fibre.
Exclusion of cases diagnosed within the first year and within the first 2 years after baseline did not change the results, and these were therefore included in the analysis.
Competing risk tests were performed to determine whether cases of colon and of rectum cancer and cases of distal and of proximal colon cancer could be merged(Reference Andersen, Borgan, Keiding and Andersen22). We used the likelihood test for interactions between the healthy Nordic food index and categories of BMI ( ≤ 25, 25–30 and >30 kg/m2) for men and women (P values >0·77).
SAS statistical software release 9.1 (SAS Institute, Inc.) on a TextPad platform was used for all statistical analyses. The PHREG procedure was used for the Cox proportional hazard models and the UNIVARIATE and FREQ procedures for the descriptive analyses.
Results
During a median of 13 years of follow-up, colon or rectal cancer was diagnosed in 567 men and 458 women.
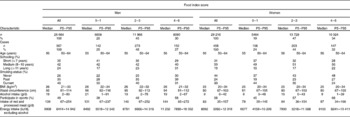
Table 1 shows the median intakes of the food groups of the healthy Nordic food index, with the 5th and 95th percentiles, for all participants and for cases stratified by sex. For men, no differences were observed. Women with CRC had slightly lower intakes of fish, cabbage, root vegetables, apples and pears than all participants.
Table 1 Intake of items in a healthy Nordic food index of colorectal cancer cases and all participants in the Danish Diet, Cancer and Health cohort (Medians and percentiles)

P5, 5th percentile; P95, 95th percentile.
* Information on intake from a single question; therefore, medians do not divide participants into equal groups.
The baseline distribution of possible confounders for the entire cohort and for people with 0–1 points (poor adherence), 2–3 points (medium adherence) and 4–6 points (good adherence) are shown in Table 2. Participants who scored high on the healthy Nordic food index had had longer schooling, were less likely to be smokers and had a smaller waist circumference than participants with lower scores. Furthermore, participants with high scores had a greater energy intake and more frequently participated in sports.
Table 2 Baseline characteristics of all participants in the Diet, Cancer and Health cohort and by healthy Nordic food index scores of 0–1 points (poorest adherence), 2–3 points and 4–6 points (best adherence) (Medians, number of participants, percentiles and percentages)

P5, 5th percentile; P95, 95th percentile.
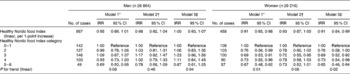
Adherence to the healthy Nordic food index was associated with a lower incidence of CRC for women, and the same tendency was found for men before adjustment for potential confounders (Table 3). When the index was assessed as a linear variable, a 1-point increase was associated with a non-significant, 5 % lower incidence of CRC for men (crude IRR, 0·95; 95 % CI 0·89, 1·01; P =0·08) and a statistically significant, 9 % lower incidence of CRC for women (crude IRR, 0·91; 95 % CI 0·85, 0·98; P= 0·01). Adjustment for potential confounding factors removed the association for men but not for women (adjusted IRR, 0·91; 95 % CI 0·84, 0·99; P =0·02). In the crude model, both men and women with 5–6 points had a considerably lower incidence of CRC than those with 0–1 points. For women, a 35 % lower incidence was found even after adjustment (adjusted IRR, 0·65; 95 % CI 0·46, 0·94). For men, a statistically significant, 31 % lower incidence was found in the crude model, but the association was no longer significant after adjustment for risk factors. Further adjustment for Ca, vitamin D and dietary fibre did not change the estimates (results not shown).
Table 3 Incidence rate ratios (IRR) and number of colorectal cancer cases according to healthy Nordic food index (0–1 and 5–6 merged) (Number of cases and 95 % confidence intervals)

* Crude.
† Adjusted for covariates: alcohol intake, smoking status, use of hormone replacement therapy (women only), schooling, sports, use of non-steroidal anti-inflammatory drugs, waist circumference and meat intake (processed and red).
‡ Model 2 plus energy.
Even though competing risk tests showed that it was acceptable to merge colon and rectum cancer (women, P =0·15; men, P =0·22) and proximal and distal colon cancer (women, P =0·62; men, P =0·40), the subtypes were also evaluated separately (Table 4). In the crude analyses, a lower incidence of distal colon cancer was found for men, but the association was no longer significant after adjustment for total energy. For women, a lower incidence of rectum cancer was found (adjusted IRR, 0·83; 95 % CI 0·71, 0·96).
Table 4 Incidence rate ratios (IRR, linear, per 1-point increase) and numbers of cases of colon and rectum cancer according to healthy Nordic food index (Number of cases and 95 % confidence intervals)

* Crude.
† Adjusted for covariates: alcohol intake, smoking status, use of hormone replacement therapy (women only), schooling, sports, use of non-steroidal anti-inflammatory drugs, waist circumference and meat intake (processed and red).
‡ Model 2 plus energy.
None of the individual food items of the healthy Nordic diet was found to be solely responsible for the protective effect of the food index (results not shown), although consumption of rye bread tended to be associated with a lower incidence among men. For women, an intake of cabbage above or equal to the median was associated with a lower incidence of CRC (crude IRR, 0·80; 95 % CI 0·66, 0·96), but this statistically significant association disappeared after inclusion of the other dietary items in the model (mutual adjustment).
Discussion
In this prospective cohort study, adherence to a healthy Nordic food index was associated with a lower incidence of CRC among women. The magnitude of the protective effect was in the same range as that found for the Mediterranean diet(Reference Reedy, Mitrou and Krebs-Smith5, Reference Fung, Hu and Wu6). A score of 5–6 points (best adherence) to the diet was associated with a 35 % lower incidence of CRC for women; a similar tendency was found for men but was no longer significant after adjustment for potential confounders.
The strengths of this study include the sample size (>1000 cases) and the long follow-up (median, 13 years). Further, a validated FFQ was used to assess intake(Reference Overvad, Tjonneland and Haraldsdottir15, Reference Tjonneland, Overvad and Haraldsdottir16), and detailed information on potential confounding factors was obtained from an additional questionnaire. The prospective follow-up and minimal loss to follow-up because of linkage to the Danish Cancer Registry are further strengths(Reference Gjerstorff14). The potential limitations of the study include the assessment of diets from a single FFQ administered at baseline; therefore, any changes in diet during the long follow-up were not captured. Residual confounding due to incomplete adjustment for the potential confounding factors or the effects of unknown confounders cannot be ruled out. An additional limitation is that the FFQ was not designed to capture intake of other traditional Nordic food items, such as rapeseed oil and berries, and these items could not be included in the index. If they had been added to the index, an even stronger association might have been found.
Adherence to the healthy Nordic food index was associated with a lower incidence of CRC, in accordance with our expectation, which was based on the hypothetical relationships of all the food items in the index to decreased cancer incidence. In the large European Prospective Investigation into Cancer and Nutrition study, fish intake was associated with a lower incidence of CRC (per 100 g increase, hazard ratio = 0·46; 95 % CI 0·27, 0·77)(Reference Norat, Bingham and Ferrari23). Isothiocyanate, which is found in cruciferous vegetables such as cabbage, is probably protective against CRC(Reference Yang, Gao and Shu24). Rye bread contains large quantities of whole-grain rye, which has a high fibre content; the evidence for a protective effect of fibre against cancer was classified as ‘convincing’ in the Continuous Update Project of the World Cancer Research Fund/American Institute for Cancer Research(25). Furthermore, cereal fibre in particular has been associated with a lower incidence of CRC(Reference Aune, Chan and Lau26). In line with our earlier study of whole-grain products in a smaller set of CRC cases, we did not find a lower incidence of CRC associated with rye bread or oatmeal intake for women(Reference Egeberg, Olsen and Loft12), whereas women with high intake of rye bread in a Swedish cohort had a lower incidence of colon cancer(Reference Larsson, Giovannucci and Bergkvist27). We did find a tendency for a protective effect of rye bread in men, which concurs with earlier findings(Reference Egeberg, Olsen and Loft12). Rye might have a greater protective effect against CRC than other types of whole grain. In a randomised crossover trial, rye bread increased the concentration of butyrate to a greater extent than white wheat bread in men(Reference Grasten, Juntunen and Poutanen28). Butyrate, which is a fermentation product of the colonic bacteria, may be one of the compounds responsible for the protective effect of whole grain against CRC(Reference Scharlau, Borowicki and Habermann29). Other studies suggest that intake of oats reduces the risk for CRC because of their high content of fibre and the content of the polyphenols avenanthramides, which attenuate the proliferation of colon cancer cells in vitro (Reference Guo, Nie and Wu30). Most of the intake of root vegetables in the present study was from carrots, a rich source of β-carotene, which has been associated with a lower incidence of CRC(Reference Chaiter, Gruber and Ben-Amotz31), even though the evidence is not consistent(Reference Flood, Velie and Chaterjee32). Proanthocyanidins, present in apples and pears, have been suggested to be chemopreventive(Reference Santos-Buelga and Scalbert33). Furthermore, the healthy Nordic food index might be associated with an overall healthy lifestyle and with other healthy dietary patterns.
Although a traditional Nordic food index has not previously been related to the incidence of CRC, two large cohort studies have been conducted in the USA on the Mediterranean diet, one of which found a moderate decrease in the incidence of CRC among participants with strong adherence to the Mediterranean diet(Reference Reedy, Mitrou and Krebs-Smith5, Reference Fung, Hu and Wu6). The size of the effect seen is comparable to that found in the present study, where a healthy Nordic food index is used.
We found a reduced incidence of CRC among women but only a tendency to a lower incidence among men. The reason for this sex difference is difficult to identify. The well-known protective effect of oestrogens against CRC may play a role(Reference Kennelly, Kavanagh and Hogan34), and there may be sex differences in the aetiology of this cancer(Reference Reedy, Mitrou and Krebs-Smith5). There might have been misclassification by sex; however, this is unlikely to have influenced the results, because in the validation study of the FFQ, the validity was better for men than for women(Reference Tjonneland, Overvad and Haraldsdottir16). Furthermore, sex differences in the estimated risks for CRC were also found in studies of the Mediterranean diet(Reference Reedy, Mitrou and Krebs-Smith5, Reference Cottet, Bonithon-Kopp and Kronborg35). In terms of generalisability, this study included only people aged 50–64 years at baseline and only people living in the Copenhagen and Aarhus areas. Additionally, the cohort underrepresented people of low socio-economic status(Reference Tjonneland, Olsen and Boll13). Therefore, caution should be used in extrapolating the results.
CRC has been associated with lower socio-economic status in Denmark(Reference Egeberg, Halkjaer and Rottmann36). As people find it easier to comply with a diet that is familiar to them than with the Mediterranean diet(Reference Astrup7, Reference Due, Larsen and Mu8), adherence to a healthy Nordic diet might be better for lower socio-economic groups, which are usually difficult to reach. As CRC is one of the commonest cancers in the Western world, with a 5-year survival of approximately 60 %(Reference Haggar and Boushey37), advocating local traditional diets could have a great impact on public health. The results of this study suggest that it would be useful to evaluate the health benefits of other regional diets, instead of promoting a Mediterranean diet worldwide.
In conclusion, we found that female participants with high scores on intake of a regional diet based on healthy Nordic food items had a lower incidence of CRC. Attempts should be made to promote a healthy regional diet, instead of promoting a Mediterranean diet worldwide; this might ensure the compliance of people of lower socio-economic status and also ensure cultural diversity, respect for heritage and protection of the environment.
Acknowledgements
The present study was funded by NordForsk (Centre of Excellence programme HELGA (070015)) and the Danish Cancer Society. A. T., K. O., A. O. and C. K. designed and conducted the research; J. C. and C. K. analysed the data; C. K., G. S. and A. O. wrote the paper under the supervision of S. L.; C. K. and A. O. bear the primary responsibility for the content. All the authors read and approved the final manuscript. The authors have no conflicts of interest to report.