INTRODUCTION
Patients who present to an emergency department (ED) are assessed and treated according to a triage system that determines priority.Reference Khangura, Flodgren and Perera 1 This model often results in long waiting times, overcrowding, patient dissatisfaction, high walk-out or left-without-being-seen (LWBS) rates for those categorized as lower priority.Reference Khangura, Flodgren and Perera 1 Although LWBS rates are routinely tracked, monitored, and used as an indicator of ED performance, there is limited knowledge about why people leave or whether they seek alternate care.
The literature indicates that LWBS patients have conditions of lower urgency and lower acuity, are more likely to be male and younger, and are likely to identify prolonged waiting times as a central concern.Reference Fayyaz, Khursheed and Mir 2 , Reference Lucas, Batt and Soremekun 3 Although there are reports of low rates of adverse health effects in the LWBS population, including low-return ED visits and hospitalizations,Reference Ding, Jung and Kirsch 4 , Reference Guttman, Schul and Vermeulen 5 others report that LWBS patients often seek alternative medical attention and exhibit higher rates of ongoing symptoms at follow-up compared to those who wait.Reference Rowe, Channan and Bullard 6 , Reference Kennedy, MacBean and Brand 7
In 2009-2010, the ED of our tertiary referral centre averaged LWBS rates of 9%-10%; this number was more than three times the national average of 3%. 8 In this study, we wished to determine factors contributing to the local LWBS rate. We also wished to compare LWBS patients to a similar group of triaged patients who did not leave to determine whether factors associated with leaving were intrinsic or extrinsic to patient characteristics. Finally, we were interested in determining the proportion of LWBS patients who sought further medical attention.
METHODS
We performed a cross-sectional survey and follow-up telephone survey of ED patients using a matched case-control design to compare characteristics, factors associated with LWBS and subsequent events for ED LWBS patients, with a demographically matched control group of patients who waited to be seen.
We collected demographic data over a 6-month period on 1508 LWBS patients in two urban hospitals located in one city; one hospital was a tertiary referral centre, and the other was an urgent care centre. Both hospitals use a standard process of tracking all LWBS patients, which includes monitoring all patients who leave the ED without being assessed by a physician, regardless of their triage level or reason for ED visit.
A total of 467 sequential LWBS patients were contacted and surveyed by nursing staff using a standardized telephone survey (Table 1). Nursing staff were not blinded to LWBS and control groups. Two attempts were made to contact each patient. Data on a matched control group of 1504 patients who did not leave the ED were collected, and 437 control patients were also surveyed. Matching was attempted for the triage category, employment and education, distance from hospital to home, and having a family physician. Re-attendance and readmissions were screened at both centres. Categorical data were analysed using chi-square and Fisher exact tests. Participation was voluntary and confidential. The study was approved by the Horizon Health Network Research Ethics Board. Because of the nature of the study and in compliance with national research guidelines, a request to waiver written consent was obtained by the institutional research ethics board.
Table 1 Telephone survey questionnaire
RESULTS
Data from the cross-sectional survey confirmed that the LWBS group (n=1508) and the control group (n=1504) were adequately matched for sex, triage category, and recorded wait times. Patients in the LWBS group were younger (32.6 v. 36.0 years; p<0.0001) and more likely to present in the evening or at night (compared to daytime) than control patients (evening: LWBS 47.8% v. control 39.2%; day: LWBS 40.6% v. control 52.1%; night: LWBS 11.6% v. control 8.7%; chi-square test 40.37, p<0.0001; Table 2). There was no difference in the cumulative percentage (fractile) wait times between LWBS patients and patients from the control group for each hour time period beyond the first hour (Figure 1).
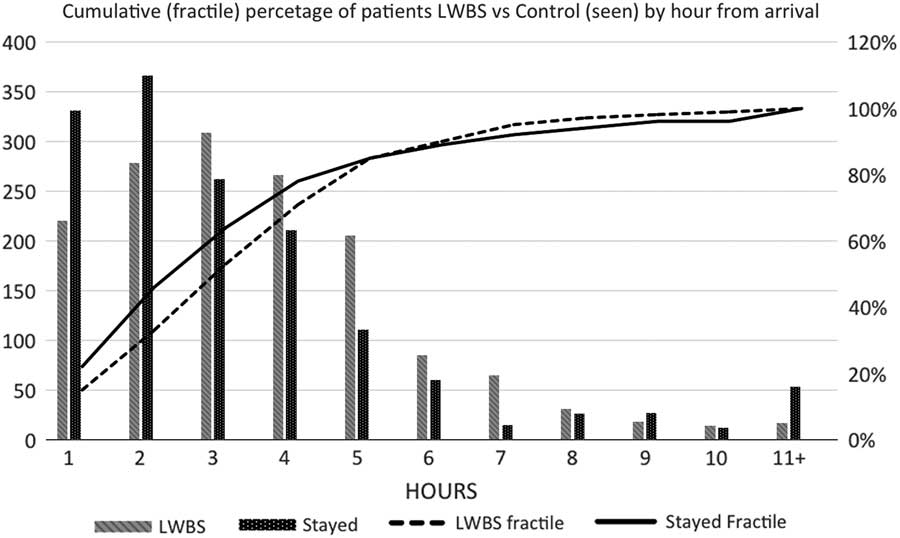
Figure 1 Cumulative (fractile) percentage of LWBS patients v. control patients (seen) by hour from arrival.
Table 2 Patient characteristics (cross-sectional survey)
CI=confidence interval; ED=emergency department; UCC=urgent care centre.
Out of 1508 LWBS patients, we attempted to contact 1424; contact information was not available for the remaining 84 people. Of the 1424 patients, we were unable to contact 890 due to incorrect contact info or because they did not answer the phone, leaving 534 patients; 67 patients refused to participate, which left a total of 467 respondents in the LWBS group. Out of 1504 control patients, we attempted to contact 1414. Of those 1414 patients, we were unable to contact 915 due to incorrect contact information or because they did not answer the phone, leaving 499 patients; 62 patients refused to participate, which left 437 respondents in the control group (Figure 2).
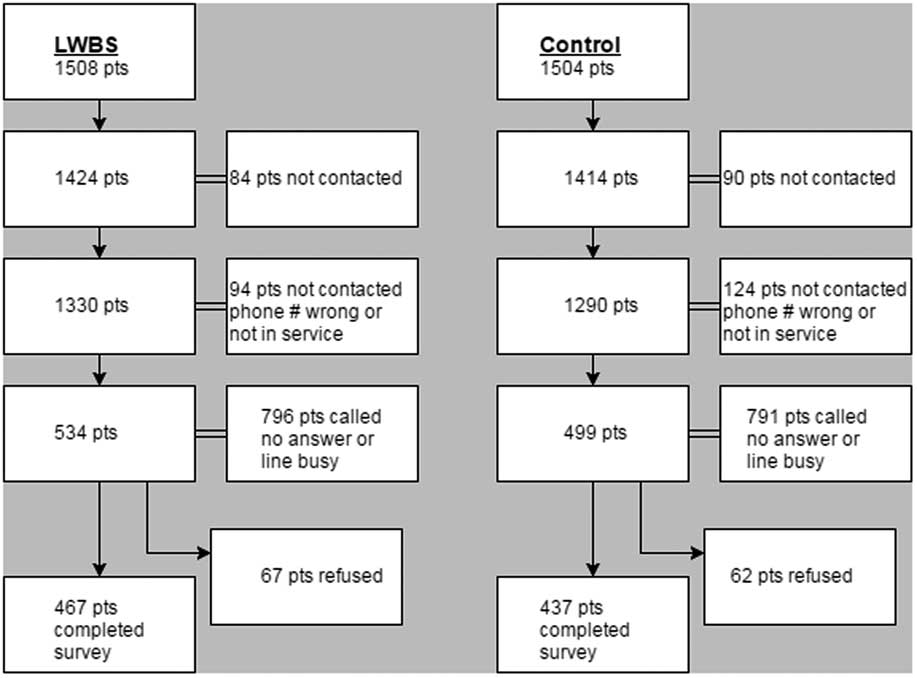
Figure 2 Study CONSORT diagram detailing the flow of left-without-being-seen (LWBS) patients and patients who stayed (control) through the study.
Results from the telephone survey confirmed that the LWBS and control groups were similar for self-reported employment and education status, and for having a family physician. Patients in the LWBS group were more likely to report living closer than 20 km from the hospital (Table 3: LWBS 65.2% v. control 54.3%; OR [odds ratio] 1.6; 1.2-2.1; p=0.001) and had a longer mode self-reported waiting time range of 2-3 hours, compared with 1-2 hours for control patients waiting to be seen, and were more likely to report having waited longer than 2 hours (LWBS 65.2% v. control 34.9%; OR 3.5; 2.7-4.6; p<0.0001; see Table 3; Figure 3, A).
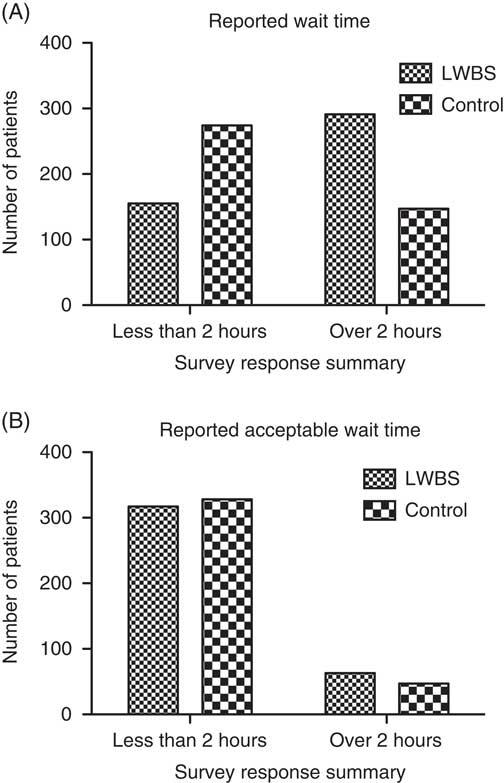
Figure 3, A and B Comparison responses for A: How long did you wait before being seen (or leaving)? and B: What is the length of time you feel you should have waited with your condition?
Table 3 Patient characteristics (telephone survey)
ED=emergency department; UCC=urgent care centre.
The most common reason reported (mode) for leaving was “long wait time” (79%), and the reason for staying was “concern about medical condition” (96%). The top response in both groups for how long patients considered to be an appropriate waiting time was “1-2 hours” (LWBS group 49% v. control 35%; see Table 3 and Figure 3, B), with no difference in the proportion of which patients felt that they should be seen in less than 2 hours (LWBS 83.4% v. control 87.5%; OR 0.72; 0.48-1.1; p=0.12). The top responses given for what would have improved the likelihood of waiting, or what would have improved waiting conditions, were “shorter wait times” (LWBS 66% v. control 31%) and “more information on wait times” (LWBS 41% v. control 23%; Figure 4).
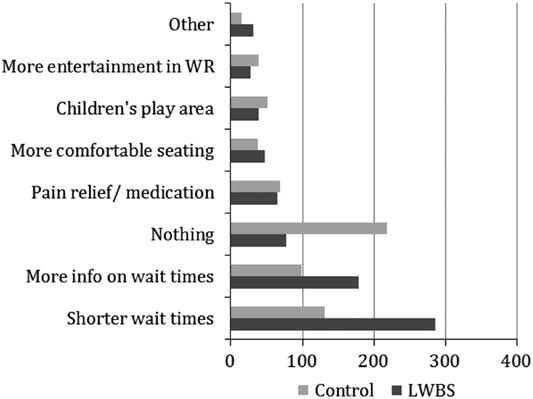
Figure 4 Responses for “What could we have done to make your wait easier and more pleasant?” and “What could we have done to make you wait longer to see a doctor?”
The majority in both groups felt that their condition was a true emergency (LWBS 63% v. control 72%). LWBS patients were more likely to seek further health care (LWBS 63% v. control 28%; p<0.001) and were more likely to do so sooner (Median time 1 v. 2-4 days; p=0.002). Of those who sought further health care, 44% followed up with a family doctor, 20% returned to the ED at a later time, 16% went to another ED, 16% went to an after-hours clinic, and the remaining 4% sought health care from “another allied health professional.” The majority of these contacts were made the same day (20%), the next day (40%), or 2-4 days after LWBS (27%); the remaining patients (13%) waited 4 days or more to contact a health care provider.
Of those patients who did not feel that their presentation was a true emergency (LWBS 37%; control 28%), the top reason given for ED attendance in both groups was the inability to see their family doctor (62% and 62%, respectively).
Fewer LWBS patients (7 [3%]) later returned to the ED with the same problem and were admitted to the hospital compared to patients who stayed and were admitted during their initial ED visit (30 [7%]; p<0.0001).
Only 4% of patients believed patients should be seen in the order that they arrive, irrespective of their condition, whereas 82% believed that the sickest people should be seen first, regardless of wait times. Ten percent believed that each condition should be seen within a certain amount of time.
DISCUSSION
The objective fractile and median (control 244, minutes; LWBS, 210 minutes) wait time for LWBS and patients who were seen were similar, despite the difference in perceived wait time (median: control, 1-2 hours; LWBS, 2-3 hours). This is consistent with previous studies where objective and perceived wait times are not the same. The most commonly reported “reasonable” wait time for both groups was 1-2 hours, and the most common reason cited by patients as to the reason they left before assessment was a perceived long wait time. We demonstrated that LWBS patients leave when their perceived wait time exceeds their intrinsic wait time tolerance, because there was little difference in the extrinsic environment.
Although the most common change that patients stated that they would prefer was shorter waiting times, the next most popular suggested improvement was more information on waiting times. Published literature on consumer preferences indicates that improved communications and expectation setting are important for improved customer satisfaction.Reference Innes, Jackson and Plummer 9 , Reference Zeithaml, Berry and Parasuraman 10 Providing accurate information on the estimated wait may be one way to alter patients’ expectations of and tolerance for wait time, and thus change the rate of patients leaving.
The commonly cited reason of waiting too long to be seen is consistent with previously published reports on LWBS.Reference Blake, Dissanayake and Hay 11 Although the majority of our patients were triaged at a lower level, some were not, and 3% ultimately required an inpatient hospital admission for the same issue. Particularly concerning is the large number of our LWBS patients who could not be located. It cannot be assumed that these patients’ conditions improved and/or that they did not experience a significant health event as a result of not being seen in the ED. This fact underscores the continued importance of LWBS, despite years of research in the issueReference Kennedy, MacBean and Brand 7 and a need to address ED wait times.
Fewer LWBS patients were eventually admitted for their presenting problem compared to controls (3% v. 7%, respectively), suggesting that some patients may be able to self-triage. Our rate of ED return and subsequent hospital admission among LWBS patients is considerably lower than the 11% previously reported.Reference Rowe, Channan and Bullard 6 It is possible that our ED is able to appropriately discern those who require immediate ED care from those who can wait.
A high percentage of all patients attended the ED because they were unable to see their primary care provider. Although limited access to primary care may be an important determinant of ED utilization, the fact that almost three-quarters of our LWBS patients perceived their condition as being a true emergency is particularly concerning. This finding suggests that LWBS is a high-risk group that deserves further attention. More important, it highlights that access to health care services in general can be problematic for many. LWBS is a complex issue that transcends multiple levels of the health care system and demands a multilevel response.
LIMITATIONS
Investigators conducting the telephone surveys were not blinded to a study group; however, because the structured survey tool was designed in advance, the major limitation is the reliability of the tool. The telephone surveys were completed with only one-third of all patients in each group. It is possible that the experiences of those who did participate were not representative of the entire study sample; however, each group was satisfactorily matched. Telephone surveys were collected retrospectively, which may have led to recall bias. Estimates of perceived wait times were given in ranges, which may lead to data accuracy problems; however, the use of ranges are pragmatic and easily understood by the participants.
CONCLUSIONS
ED LWBS patients had similar opinions, experiences, and expectations as controls. Despite otherwise closely matched patients’ characteristics, LWBS patients believed that the wait times were longer than expected. Suggested improvements included shorter wait times and provision of more information on wait times. LWBS patients may be more likely to self-triage to alternate care: they do so sooner and in higher proportion but were less likely to be admitted to the hospital for the presenting problem. Both study groups contained patients requiring admission, demonstrating that LWBS patients do carry risk. Further study should explore relationships between LWBS patients, ED boarding rates, and physician initial assessment times.
Author contributions: PA and J Fraser contributed to project design, ethics application, data acquisition and analysis, and final project composition. AG contributed to project design, ethics application, and data acquisition and analysis. J French, RM, and MH contributed to project design and final project composition.
Acknowledgements: We wish to acknowledge the assistance of Kerry Betts, Debra Pitts, Tammy Lawson, and Kim David, who helped perform the telephone surveys and reviewed the manuscript.
Competing interests: None declared.









