The consumption of certain types of food, especially highly palatable foods that are rich in sugar and fat, activates the mesolimbic pathway in the brain. This impairs decision-making processes, having an effect similar to that of drugs of abuse(Reference Ayaz, Nergiz-Unal and Dedebayraktar1–Reference Wiss, Avena and Rada3). An increasing number of studies have shown evidence regarding biological and behavioural changes in response to consumption that meet the criteria of food addiction (FA)(Reference Gordon, Ariel-Donges and Bauman4). FA can be diagnosed in individuals with different nutritional statuses, but the risks associated with and changes in the control of food consumption are greater in overweight individuals(Reference de Sousa Fernandes, Santos and dos Santos5). Preliminary investigations in overweight and obese children revealed eating behaviours consistent with FA(Reference Tompkins Connie and Laurent Jennifer6,Reference Filgueiras, de Almeida and Nogueira7) .
Increases in the production and consumption of ultra-processed foods that are cheap, palatable and ready for consumption are associated with the advancement of obesity(Reference Martins, Levy and Claro8,Reference Monteiro, Levy and Claro9) . These foods use salt, sugar, oils and fats. On top of that, ultra-processed foods are defined as including substances not used in culinary preparation as additives intended to imitate the sensory qualities of fresh foods(Reference Monteiro, Levy and Claro9,Reference Monteiro, Levy and Claro10) . Furthermore, there is evidence that increased consumption of ultra-processed foods increases one’s risk for developing obesity and chronic diseases. These chronic diseases include diabetes, hypertension and cancer(Reference Mendonça, Lopes and Pimenta11–Reference Srour, Fezeu and Kesse-Guyot13).
The Yale Food Addiction Scale for Children (YFAS-C) is currently the only validated psychometric assessment tool for assessing FA in life’s early stages(Reference Meule, Hermann and Kübler14,Reference Richmond, Roberto and Gearhardt15) . The YFAS-C has been cross-culturally adapted, translated into Portuguese and validated for overweight Brazilian children(Reference Gearhardt, Corbin and Brownell16,Reference Filgueiras, Sesso and Almeida17) . Cross-cultural adaptations of the YFAS-C were also successfully experienced in many countries. For example, a meta-analysis of twenty-two observational studies included data from the USA, the Netherlands, Egypt, Australia, Hungary, Brazil, Iran, Russia and Mexico. Among obese children, the prevalence of FA was 19 % (95 % CI 14 %, 26 %). The overall prevalence was 15 % (95 % CI 11 %, 19 %). Authors did not identify results from longitudinal studies in the search(Reference Yekaninejad, Badrooj and Vosoughi18). Only four studies investigated the correlation of FA with BMI z-score (0·30; 95 % CI 0·24, 0·36). Also noted is the fact that the higher FA prevalence observed in female adults in previous studies(Reference Pursey, Stanwell and Gearhardt19) was not observed in female children. This suggests that sex-related differences might not occur in children with FA. In adults, high YFAS scores have been associated with higher BMI, stronger cravings for certain foods and more frequent episodes of binge eating(Reference Richmond, Roberto and Gearhardt15).
It is important to note that FA can hamper weight loss efforts(Reference Burmeister, Hinman and Koball20). However, it is unclear whether this is a barrier to successful treatment for childhood obesity. Thus, a thorough assessment of the role that an addictive process can play in childhood is justified, especially for those monitored for weight control. This study aimed to assess whether FA was associated with changes in the BMI/age z-score as well as whether FA was associated with the consumption of ultra-processed foods by overweight students undergoing multicomponent interventions in the school environment.
Methods
Study participants and design
The study evaluated multicomponent interventions for low-income overweight students (BMI-for-age = weight in kg/height in square meters ≥ 1 z-score (BMIz)) in two public schools, each undergoing a set of interventions. The current study is part of a larger project. It aims to assess the association between FA measured at baseline and FA after the intervention with BMIz and food consumption changes. The schools were in a low-income area of the city of São Paulo, Brazil. The selection criterion was school proximity to the Centre for Nutritional Recovery and Education (CREN), from which the programme was managed and to which the overweight students were referred for individualised outpatient treatment. All students enrolled in grades 4 and 5 participated in school activities (workshops with teachers, parents, children and physical activity). The activities at school aimed to motivate students, teachers and parents/guardians to consume healthier food and undertake healthier lifestyles. As the study aimed to ameliorate excess weight through educational activities, all the changes towards better food intake or lifestyle that occurred in the school environment were considered a result of the intervention.
In one week, the students took part in nutrition education workshops. During the other week, they attended consecutive reflective meetings. The nutrition education workshops were playful and included a set of strategies to improve healthy eating. These strategies included lectures, videos about childhood obesity, magazine clippings, pictures, posters and slide shows, among other resources. The workshops occurred in groups of thirty-five students at a time, lasted 45 min, and were conducted by two experienced and trained professionals. The reflective meeting was a psycho-educational activity seeking solutions for significant problems in daily life. The theoretical basis of this practice is the existential phenomenology and dialogical group meetings proposed by Paulo Freire(Reference Szymanski and Szymanski21). A psychologist coordinated reflective meetings with another professional aid, who recorded key information during the sessions. In addition, supervised physical activity was performed every week. Once a week, the physical educator conducted physical activities in an adequate space at the school, with groups of about thirty-five to forty students for 45 min. The main objective was to encourage regular physical activity and teach practices that could be replicated at other times in daily life, focusing on youth autonomy and leadership. To favour free initiatives, new rules for the games were discussed and created after the debate to improve collaboration between teams and partners. Tournaments that involved all classes were also conducted. Monthly meetings with parents/guardians, teachers and students were conducted on weekends.
The weight and height of students aged 8–11 years were measured to identify overweight individuals students (BMI/age ≥ 1 z-score) in both schools. The intervention at school 1 consisted of weekly meetings conducted by a multidisciplinary team (nutritionists, a psychologist and a physical educator) during the first 6 months to motivate the adoption of a healthy lifestyle for the whole class. After this period, only overweight students were referred for outpatient treatment at the CREN. They proceeded to follow up there for 10 months. The intervention at school 2 was carried out by the whole class attending a nutritional education programme, counselling group meetings and weekly physical activity for 16 months; overweight students also received outpatient care at CREN. The study lasted 16 months following the school schedule and was registered in the Brazilian Clinical Trials Registry (primary identification number: RBR-9t2jr8). Individuals with neurological, cardiovascular, respiratory or metabolic disorders and known family problems that could affect participation in the programme and involvement in activities, such as answering questionnaires, were excluded from the study.
The sample size calculation was made for the primary study objective, which was the change in BMI z-score (post-intervention v. baseline measurements). A sample of ninety-eight participants aged 8–11-years-old was calculated considering a mean difference of 0·12 and a standard error of 0·30, with a probability of a type I error (α) of 0·05 and a desired power of 0·80(Reference Patriota, Filgueiras and de Almeida22).
All overweight students eligible for the study underwent blood collection and pubertal staging assessment and answered the YFAS-C questionnaire to identify the presence of FA and FFQ at baseline and after the intervention. Children aged 8 years were not included because of the difficulty in completing the questionnaires.
The students’ parents/guardians and students all signed the free and informed consent form, and the study was approved by the Research Ethics Committee of the Federal University of São Paulo (CAAE: 34.304. 714.40000.5505).
Assessment of food consumption
A semi-quantitative FFQ developed and validated for Brazilian adolescents(Reference Araujo, Yokoo and Pereira23) was applied by the same interviewer at the baseline and after 16 months of intervention. The subsequent adaptation standardised portion sizes and frequencies and excluded two items after a pre-test. To assist in the application of the FFQ, a photographic manual with images representing the portion sizes of each item was used(Reference Brito, Araujo and Guimarães24).
Food consumption data were processed using the Nutrition Data System for Research software database (NDS-R version 2014; University of Minnesota), according to the standard protocol recommended by Fisberg and Marchioni for Brazilian research(Reference Fisberg, Marchioni and Previdelli25). Portion sizes were converted to g with the support of a Brazilian table of domestic measures(Reference Pinheiro, Lacerda and Benzecry26). Thus, nutritional information was obtained regarding the energy and nutrient consumption of each participant. The variables of sugar and Na were chosen because of their high content and prevalence in ultra-processed foods and the association of these dietary factors with the development of obesity and other chronic, non-communicable diseases.
Ultra-processed foods were identified according to the NOVA system(Reference Monteiro, Levy and Claro9) and are represented by items such as sweet and savoury cookies, snacks, instant noodles, sweets, sausages, soft drinks and beverages, and sugary dairy products. The complete description of the quantification, food classification and application of this questionnaire has been described in a previous study(Reference Filgueiras, de Almeida and Nogueira7).
The Yale Food Addiction Scale for Children
The YFAS-C scale includes twenty-five items based on Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV)(Reference Gearhardt, Roberto and Seamans27) to investigate seven diagnostic criteria that identify the presence of addiction and clinical impairment, or impairment related to specific eating behaviours. The YFAS characterises FA via the following items and criteria: Items 1–3 assess whether food is taken in larger amount and for longer period than intended (criterion 1); items 4, 17, 18 and 25 assess persistent desire or repeated unsuccessful attempts to stop one’s FA (criterion 2); items 5, 6 and 7 assess how much time is spent obtaining and eating food, or how much time was spent recovering from the food’s effects (criterion 3); items 8, 9, 10 and 11 assess which important social, occupational and/or recreational activities are given up or reduced due to FA (criterion 4); item 21 assesses if food is continuing to be used despite knowledge of adverse consequences (criterion 5); items 22 and 23 assess tolerance (criterion 6); items 12–14 assess the characteristics of withdrawal symptoms and whether food is used to relieve withdrawal (criterion 7); and items 15 and 16 assess clinically significant impairment or distress that is not listed in the inclusionary criteria for substance-use disorders but are instead mentioned prior to the specific inclusionary criteria. A 5-point Likert scale (0 = never; 4 = always) was applied to all eighteen YFAS items, and a dichotomous (yes/no) scale was used for the seven items. Following this, all the items were converted dichotomously (0 = no; 1 = yes) according to specific scoring thresholds for each item. Using the converted dichotomous scores, a symptom count score (ranging between 0 and 7) and a diagnostic score (having three or more criteria met plus having a clinically significant impairment or distress) can be generated(28). The questionnaire was simultaneously administered to two students using a single interviewer. The students were separated so that they could not see one another and were instructed not to read their answers aloud. The students received questionnaires and a pen to mark their responses. The lines were alternated with white and grey to make it easier for them to follow the line and not mark the answer to the wrong question. The interviewer read each question while the students followed the reading in their questionnaires. Each application lasted for approximately 15 min. The translation and validation of this questionnaire were carried out as previously described(Reference Filgueiras, Sesso and Almeida17). YFAS-C was applied at baseline and after 16 months of intervention.
Statistical analysis
Categorical variables were presented using a simple frequency distribution, while numerical variables were described by means and their respective standard deviations.
The associations with the intake of energy, carbohydrates, proteins, fats, sugar and Na from ultra-processed foods at baseline (dependent variables) with FA (at baseline) were explored using multiple linear regression models. We adjusted for sex, age and which school the participant attended. The best condition was adopted as the reference category for comparisons without FA at baseline.
The linear mixed-effects model was used to assess changes in the BMI/age z-score over time in relation to FA. The occurrence of FA at baseline, or at the final assessment in association with ultra-processed food consumption at baseline, was a pre-specified option in this analysis. This was used to fully capture the possibility of the occurrence of this risk factor in the studied individuals, even during the intervention. We assumed that the presence of FA at any measurement time (baseline or after the intervention) could be associated with BMI z and type of food consumption. In subsequent models, changes in the consumption of ultra-processed foods (sweet and savoury cookies, snacks, instant noodles, sweets, sausages, soft drinks and sugary milk-based drinks) in relation to FA were evaluated. In these models, sex, age, school, time, FA and time–FA interactions were considered variables with fixed effects. FA entered the models as a binary variable (yes/no type) at the time of study. The ‘individual’ was considered as a variable with random effects.
The data were processed using Stata 16.1 software (College Station), and a value of 5 % was adopted as a limit for rejecting the null hypothesis (P < 0·05).
Results
The sample consisted of 120 overweight students (mean BMI/age z-score = 1·96; sd 0·68) aged 9–11-years-old (64 girls, 53·4 %; 56 boys, 46·7 %) who completed the questionnaires both at baseline and after the study. The students had a mean age of 9·6 years (sd 0·7), meaning that most of them were in the prepubertal stage. Eighty students (66·6 %) did not exhibit food addiction in either assessment, whereas 40 (33·4 %) did in at least one of the assessments (n 29 in the initial assessment, n 15 in the final assessment, and four exhibited FA in the two measurements). This totalled forty-four occurrences of FA (Table 1).
Table 1. Descriptive values of the general characteristics of the students at baseline
(Numbers and percentages; mean values and standard deviations)
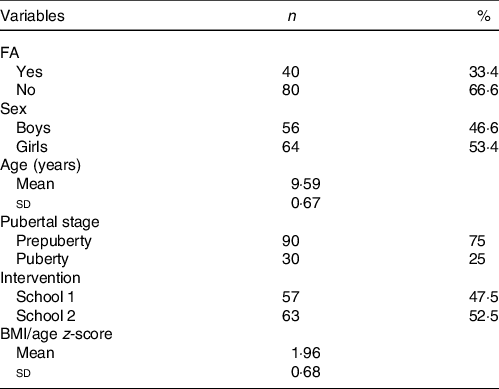
FA, food addiction.
Using multiple linear regression to measure the relationship between FA and dietary intake, it was observed that the occurrence of FA in the initial assessment was associated with a higher consumption of energy content, total carbohydrates, proteins, Na and sugar from ultra-processed foods at baseline (P < 0·05; Table 2).
Table 2. Consumption of food components from ultra-processed foods (energy, carbohydrates, proteins, fats, sugar and Na-dependent variables) at baseline, according to FA, adjusted for age, sex and
school (β-coefficients; 95 % confidence intervals)
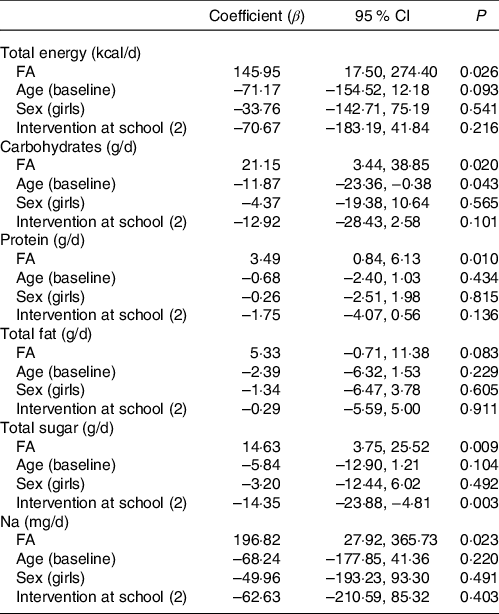
FA, food addiction.
We used the analysis of mixed-effects models to assess the effect of the intervention (represented by the time of the study) and the evolution of the BMI/age z-score between occurrences with and without FA. This showed that sex, age and school were not associated with BMI/age z-score (P > 0·05). However, FA proved to be a factor related to weight maintenance, showing significant interaction with time (P = 0·016) (Table 3). Weight loss was observed only in individuals non-food addiction (NFA) (BMI/age z-score = –0·3); however, individuals with FA showed a slight increase in the BMI/age z-score (Fig. 1).
Table 3. Linear mixed-effects model to assess the evolution of the BMI/age z-score over time in relation to FA
(95 % confidence intervals)

FA, food addiction.
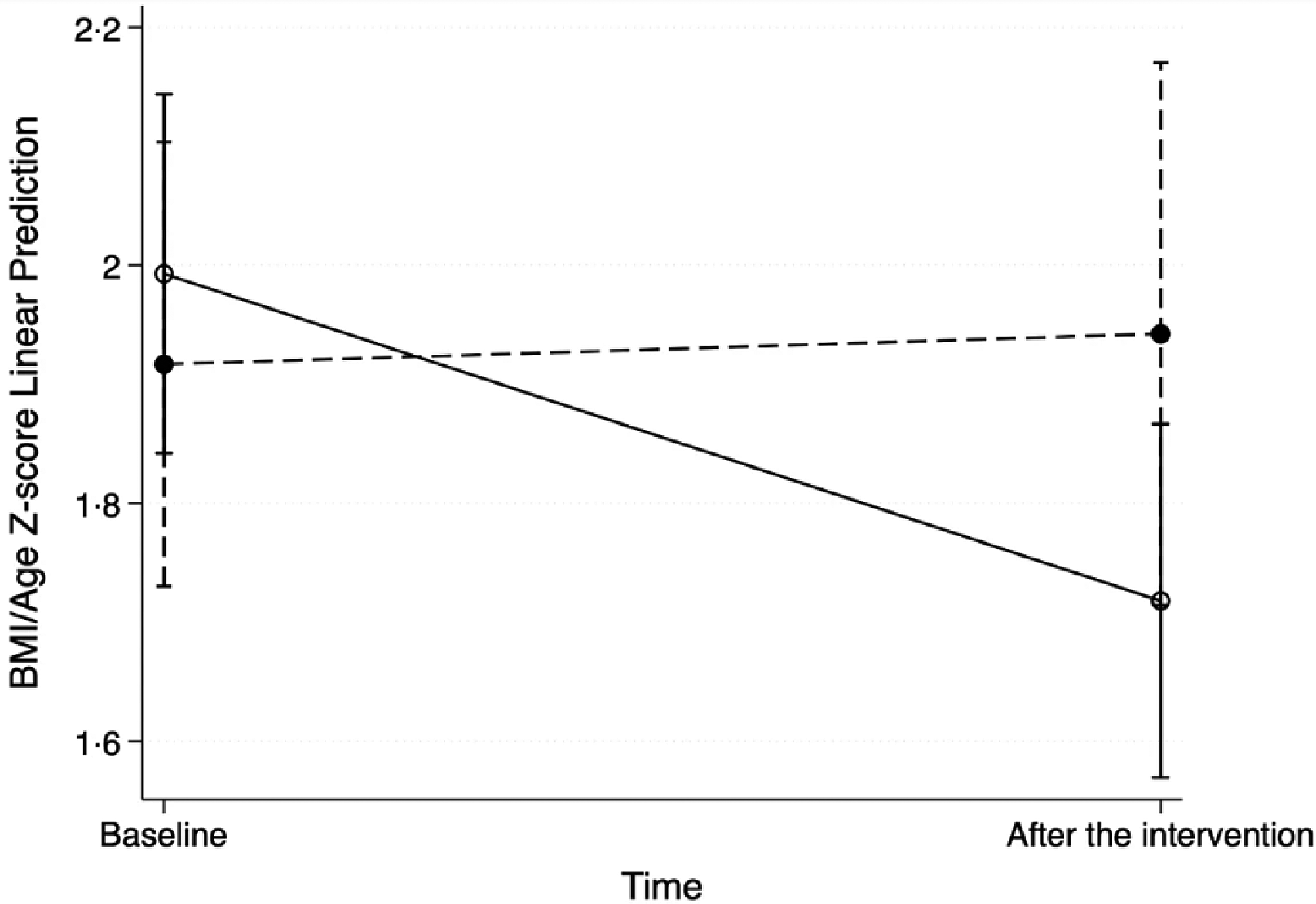
Fig. 1. Effect of the intervention time on the BMI/age z-score among students with and without FA. ![]() , NFA;
, NFA; ![]() , FA. NFA, non-food addiction; FA, food addiction.
, FA. NFA, non-food addiction; FA, food addiction.
Among the dietary variables, when evaluating the effects of the intervention and the measured consumption of sugary milk-based beverages, it was possible to verify an effect. We noted a significant reduction in consumption of the sugary milk-based beverages –71·13 kJ (–17 kcal), P = 0·04 in non-food addiction students, and a non-significant, slightly increased consumption at the end of the study in the FA students +50·21 kJ (+12 kcal), P = 0·41 (Table 4; Fig. 2). Similar models were made for the consumption of other ultra-processed foods, such as sweet and savoury cookies, snacks, instant noodles, sweets, sausages and soft drinks, but they did not reveal significant associations with FA.
Table 4. Linear mixed-effects model to assess the consumption of sugary milk-based drinks over time in relation to FA
(95 % confidence intervals)

FA, food addiction.

Fig. 2. Effect of the intervention time on the consumption of sugary milk-based drinks among students with and without FA. ![]() , NFA;
, NFA; ![]() , FA. NFA, non-food addiction; FA, food addiction.
, FA. NFA, non-food addiction; FA, food addiction.
Discussion
The hypothesis that gave rise to this study was that an addictive eating behaviours could play a role in students monitored for weight control. Two models of school intervention were employed in this project. In the first one, the school activities lasted for the initial 6 months. Then, overweight students received individual treatment at CREN for the following 10 months (intervention 1). The second model performed activities and monitored overweight students using well-trained health professionals at school and offered individual treatment at CREN throughout the intervention period of 16 months (intervention 2). The primary intention was not to compare the two models by controlling the variables, as the actions taken during the interventions were many and varied. In fact, it was decided to carry out all possible educational actions to improve nutritional status and verify whether there was an association between FA, the change in the BMI/age z-score and the consumption of ultra-processed foods in overweight students.
Food addiction among overweight students
The presence of FA was reported in prepubertal adolescents from 9 years of age(Reference Laurent and Sibold29). The prevalence of FA among overweight students in this study was 33 %. Comparatively, in a study using participants from an outpatient weight control programme, FA’s prevalence was 30·7 % among obese Caucasian adolescents(Reference Tompkins Connie and Laurent Jennifer6) and 10 % among obese African adolescents(Reference Schulte, Jacques-Tiura and Gearhardt30).
Effect of food addiction on the intervention to improve BMI
We observed that with the intervention, the BMIz score decreased overtime in students did not exhibit FA. However, we did not observe this reduction in individuals who experienced FA during the study. These data reveal that FA can be a barrier to maintaining a healthy weight.
Research in this area suggests that FA may contribute to weight gain. However, it is not clear whether FA interferes with the success of a weight loss programme(Reference Meule, Hermann and Kübler14). Relatedly, however, studies of obese adult populations have shown that individuals with FA have worse results than their NFA counterparts when participating in these programmes(Reference Burmeister, Hinman and Koball20). These studies also show that adolescents experiencing FA, or a greater number of symptoms, may justify requiring additional resources for better adherence to the treatment for weight control(Reference Tompkins Connie and Laurent Jennifer6). Moreover, overweight children have been shown to be more likely to develop metabolic disorders such as insulin resistance, hypertension, CVD, psychological disorders and impaired social life(Reference Sahoo, Sahoo and Choudhury31).
Food addiction and food consumption
This study revealed an association between ultra-processed food consumption at baseline and FA. Greater consumption of energy content, carbohydrates, Na, sugar and proteins from ultra-processed foods was observed in individuals with FA. This result is consistent with findings in both animals and humans, which suggests that highly processed foods with additional amounts of refined carbohydrates and/or salt are closely associated as an indicator of FA(Reference Schulte, Avena and Gearhardt32–Reference Frank, Linder and Kullmann34). Increased consumption of foods rich in sugars and salt causes changes in metabolism, insulin sensitivity and appetite hormone function(Reference Leigh, Lee and Morris35,Reference Wahlqvist36) . These changes can generate changes over neural control of reward, increase dopamine release (as well as other hormones) and, consequently, reinforce the importance and motivation for ingestion of ultra-processed foods(Reference Sinha and Jastreboff37–Reference Dossat, Lilly and Kay39).
The consumption of sugar and sugary milk-based beverages was proven to be related to the presence of FA. These results are consistent with other findings demonstrating that individuals with FA reported having more problems with certain food items that are high in fat and sugar, dense in energy and highly palatable(Reference Ayaz, Nergiz-Unal and Dedebayraktar1,Reference Schulte, Jacques-Tiura and Gearhardt30) .
There are methodological difficulties in studying the effect of a food component separately, such as sugar or fat, since dietary surveys hardly identify ingredients or culinary recipes. Most of the results supporting the hypothesis that sugar consumption is associated with FA stem from animal studies(Reference Westwater, Fletche and Ziauddeen40). However, it has been shown that a combination of sugar and fat results in increased consumption volumes. Systematic reviews of the literature on FA have concluded that the foods commonly associated with symptoms like FA in humans are highly processed, have a high glycaemic index and contain large amounts of added fats and sugar(Reference Gordon, Ariel-Donges and Bauman4,Reference Pursey, Davis and Burrows41) .
Several studies have indicated that continual access to diets and an eating pattern based on foods rich in sugar, fat and salt causes signs of addiction. These signs include increased food craving, desire and motivation to eat and are associated with neurochemical adaptations in reward systems, like other chemical dependencies(Reference Schulte, Avena and Gearhardt32,Reference Rogers and Brunstrom42,Reference Mattes and Foster43) . Children are exposed to these early in their developmental period when their neural and psychological systems are the most vulnerable(Reference Richmond, Roberto and Gearhardt15). Data from the Brazilian Consumer Expenditure Survey, conducted in 2017 and 2018, revealed that the estimated frequency of consumption of fruits and vegetables was lower among adolescents than among adults and the elderly. On the other hand, the consumption of unhealthy foods, such as instant noodles, cookies, chips, sausages, chocolate, ice cream, soft drinks/processed juices, soft drinks, sugary milk-based drinks and sandwiches was higher among adolescents than among adults and seniors(44).
Food addiction and intervention strategies
Ultra-processed foods facilitate overeating and the development of obesity because they are rich in energy content, salt, sugar and fat. They also cause changes in appetite control mechanisms. Moreover, they are used in highly palatable products which can generate pathological eating behaviours(Reference Hall, Ayuketah and Brychta45).
The success of treating obesity remains low. Not only that, but FA has been identified as an underlying factor with therapeutic relevance. In this study, the 16-month intervention for promoting healthy eating was carried out through multicomponent interventions. BMIz decreased over time in overweight students who did not exhibit FA. The hypothesis that FA has been implicated as a risk factor for overweight is plausible. Our results indicate that FA can adversely affect the efficacy of interventions for reducing overweight among students. This was previously reported for adults. The Diet Intervention Examining the Factors Interacting with Treatment Success trial followed 609 overweight or obese women (57 %) and men for 12 months. In that study, the authors observed that experiencing FA at baseline was the main factor correlated with treatment failure(Reference Fielding-Singh and Patel46).
Understanding the concept of FA can open new paths for the prevention and treatment of obesity. This understanding also allows for the proposing of new and improved public health policies, although it may not be suitable for the various disorders associated with overeating(Reference Adams, Sedgmond and Maizey47). The negative effects of food restriction are known(Reference Mairs and Nicholls48); however, at least in a subset of vulnerable individuals, some ultra-processed foods appear to be a specific trigger for eating disorders. These specific ultra-processed foods can be reduced or avoided. Other successful strategies used to combat FA include environmental interventions, such as restrictions on advertising and/or taxing sugary drinks(Reference Lennerz and Lennerz49).
Our study has some limitations, such as the relatively small number of individuals studied. In this sense, prospective studies with larger samples and that examine people at other stages of life are required to better establish the relationship between weight loss, ultra-processed food consumption and FA. We adopted a within-subjects design since all students should have the same opportunity to be informed about dietary recommendations and receive treatment for their overweight status. Another limitation is the use of an FFQ to determine the food intake of students. Although the methods of assessing food consumption are imprecise and limit the impact of the result, the choice of this method relied on the fact that it was the most practical and validated to achieve the objectives of the study. In addition, it was not possible for parents/guardians to answer the FFQ, since the students ate a large part of their meals outside the home and without the guardians present. Due to the small sample size and the study design, we could not establish a causal relationship between FA and BMI or food consumption changes. Additionally, we did not look for a causal relationship between FA and outcomes (BMI and food consumption), but rather an association between that behaviour (baseline or during the intervention) and outcomes. We could not address changes in FA classification from pre- to post-intervention.
However, some strengths of the study are the longitudinal character of 16 months of follow-up, with FA being assessed at baseline and after multicomponent interventions in students.
Conclusion
Clarification of the relevance of FA in childhood is essential for formulating nutritional policies aimed at this stage of life. This study showed that FA is associated with maintenance of excess weight in students undergoing a nutritional intervention. Specifically, the consumption of foods rich in sugar, especially sugary milk-based drinks, was associated with this condition. The limited literature on FA in childhood reinforces the need for further studies to develop new approaches to map, prevent and treat FA in this age group.
Acknowledgements
This work was supported by FAPESP – Foundation for Research Support of the State of São Paulo and CNPq – National Council for Scientific and Technological Development. Both institutes had no role in the design, analysis or writing of this manuscript.
V. B. P. A. and A. R. F. contributed to formulating the research questions, the study design, analysing the data and writing the manuscript; P. C. K. N. and R. C. S. contributed to data analysis, discussion of the results and article revision; A. L. S. is the professor responsible for the research funding, the formulation of the research questions, study design and revising the manuscript and S. M. A. D. is the professor responsible for the supervision of food consumption analysis, design of the study and manuscript revision.
None of the authors has any conflicts of interest to declare.









