Depression in schizophrenia recently has enjoyed a revival in research settings, although depression-like pathology has been acknowledged in the literature since the earliest observations (Reference BleulerBleuler, 1950). The major shift in this position has been the observation that depression may also occur independently of the symptoms of schizophrenia and several months after recovery from an acute episode, i.e. post-psychotic depression, in up to 30% of cases (Reference Siris, Hirsch and WeinbergerSiris, 1995); it is known to be both a precursor and a concomitant feature of hopelessness and suicidal thinking (Drake & Cotton, 1986). Several theories attempting to account for the onset of secondary depression have been postulated. The ‘intrinsic’ theory suggests that depression is an essential aspect of the schizophrenic process and as such should be discernible at one or more stages during the course of an acute psychotic episode (Reference Hirsch and JolleyHirsch & Jolley, 1989). ‘Pharmacogenic’ theories have suggested that the depression observed in psychosis may be simply a drug-induced akinetic dysphoria (Reference Van Putten and MayVan Putten & May, 1978). Results from Birchwood et al (Reference Birchwood, Mason and MacMillan1993) and Rooke & Birchwood (Reference Rooke and Birchwood1998) show that depression following acute psychosis may be a psychological response (demoralisation) to an apparently uncontrollable life event (the psychosis) and its attendant disabilities. Leff (Reference Leff and DeLisi1990) proposes three types of clinical course for secondary depression in schizophrenia: depressive symptoms at the acute stage that are ameliorated as psychotic pathology recedes and do not re-emerge after recovery; depressive symptoms that emerge at the point of remission of the acute psychosis; and depressive symptoms that emerge independently of the acute psychosis at a point several months after recovery (post-psychotic depression). In this study we investigate the ontogeny of depression from the acute episode onwards and put these models and course patterns to the test. We report the evolution of depression over a 12-month follow-up period and its link with positive and negative symptoms.
METHOD
Design
The course of psychotic and dysphoric symptoms was investigated by longitudinal assessment of symptoms during the acute stage, on recovery and at follow-up interviews 4, 8 and 12 months after recovery. Specific instruments were employed to assess the course of positive and negative symptoms, depression and suicidal ideation.
Case identification
The study commenced in 1994 and all patients were recruited from acute services in northern Birmingham (population 650 000). Inclusion required that patients fulfilled ICD-10 (World Health Organization, 1992) criteria for schizophrenia or a related disorder (F20, F22 and F23), in the absence of organic disorder or a current diagnosis of mania or bipolar disorder or mood-congruent delusions and hallucinations. All participants were aged between 18 and 65 years inclusive.
Daily contact with admission units ensured that all new admissions were screened within 3 days of their arrival by examining medical files for exclusion criteria and current symptoms/diagnosis and through discussion with ward nursing and psychiatric staff. Patients satisfying screening criteria were interviewed within the next 2 days; thus, no more than 5 days elapsed between admission and first interview. The timing of the recovery interview corresponded with each patient's discharge from the ward and employed recovery criteria described by Drury et al (Reference Drury, Birchwood and Cochrane1996). Patients were re-interviewed until recovery had occurred.
Assessments
Each interview was conducted using a battery of measures. Negative and positive symptoms were measured using the Scale for the Assessment of Negative Symptoms (SANS; Reference AndreasonAndreason, 1982) and the Scale for the Assessment of Positive Symptoms (SAPS; Reference AndreasonAndreason, 1986) respectively. Two measures were used to assess depressive pathology: the self-report Beck Depression Inventory (BDI; Reference BeckBeck, 1967) and the interview-based Calgary Depression Scale for Schizophrenia (CDSS; Reference Addington, Addington and Maticka-TyndaleAddington et al, 1993), which also provides sub-scales for hopelessness and suicidal ideation. The CDSS was developed specifically with the aim of avoiding phenomenological overlap between depression and negative symptoms. The presence and severity of pharmacogenic side-effects were assessed using the Abnormal Involuntary Movements Scale (AIMS; Reference Wojcik, Gelenberg and LaBrieWojcik et al, 1980) and the chlorpromazine equivalent dosages were calculated from the September 1996 British National Formulary (British Medical Association & Royal Pharmaceutical Society of Great Britain, 1996). Basic demographic and clinical data were collected on a standardised form.
Patients' beliefs about their illness (Personal Beliefs about Illness Questionnaire, PBIQ; Reference Birchwood, Mason and MacMillanBirchwood et al, 1993), self-esteem (Crown Self-Esteem Scale; Reference Crown, Lucas and StringerCrown et al, 1977) and insight (Insight Scale; Reference Birchwood, Smith and DruryBirchwood et al, 1994) were also assessed. Additional ‘one-off’ measures were employed during the follow-up phase to evaluate cognitions pertaining to the self, namely the Possible Selves Questionnaire (PosSQ; Reference Marcus and NuriusMarcus & Nurius, 1986) and the Depressive Experiences Questionnaire (DEQ; Reference Blatt, D'Afflitti and QuinlanBlatt et al, 1976). The data from the PBIQ, Crown Self-Esteem Scale, Insight Scale, PosSQ and DEQ will be commented upon in our subsequent companion paper.
Each item pertaining to a symptom on either the SANS and SAPS is assessed on a six-point scale. A score of zero denotes the absence of the symptom whereas a rating of 1-5 denotes the presence of the target symptom in increasing severity. The SANS has five categories: affective blunting and flattening, alogia, avolition-apathy, anhedonia-associality and attention. The SAPS consists of four categories: hallucinations, delusions, bizarre behaviour and positive formal thought disorder. In addition to the symptom items, which comprise each SANS or SAPS category, an additional ‘global rating’ item for the category as a whole is included.
Reliability of SANS and SAPS ratings
Following a period of training in the instruments, mental state assessments carried out by the second author (Z.I.) were subject to a reliability check to prevent drift in accuracy of ratings across the study. A sample (n=6) from the present study was selected randomly at different points and re-interviewed by M.B. blind to the original assessment. Sufficient concordance between the two raters was established for both SANS (r=0.95, P<0.01) and SAPS (r=0.86, P<0.05) total scores.
Hypotheses
-
(a) Depression and positive symptoms will ‘follow the same course’ during recovery from the acute phase.
-
(b) Depressive symptoms that emerge at the post-psychotic stage will do so independently of the course of negative or positive symptoms or neuroleptic side-effects.
RESULTS
Of the 105 subjects recruited into the study, a subsample of 24 (22.8%) dropped out during follow-up: 87 (83%) completed two observations, 81 (77%) completed three or four observations and 78 (74.3%) completed all five interviews over the duration of the study. The subsample of subjects (n=27) who did not complete all assessments was found to differ significantly from the main sample in two respects: the subsample was significantly older at the first onset of psychosis and also in chronological age (see Table 1). Completion of all five follow-up assessments was not linked to use of the Mental Health Act during hospital admission (χ2=1.0, NS).
Table 1 Mean values for complete and incomplete data subgroups at onset and recovery interviews

| Variable | Onset | Recovery | ||||||
|---|---|---|---|---|---|---|---|---|
| Complete (n=78) | Incomplete (n=27) | t | P | Complete (n=78) | Incomplete (n=15) | t | P | |
| BDI score | 21.09 | 17.37 | 1.37 | NS | 12.99 | 17.07 | 1.48 | NS |
| CDSS score | 9.20 | 9.18 | 0.01 | NS | 5.87 | 6.00 | 0.11 | NS |
| Negative symptoms | 11.44 | 9.63 | 1.72 | NS | 7.86 | 8.33 | 0.41 | NS |
| Positive symptoms | 7.94 | 8.58 | 0.94 | NS | 3.37 | 3.33 | 0.44 | NS |
| Suicidal ideation | 0.77 | 0.59 | 0.81 | NS | 0.26 | 0.40 | 0.72 | NS |
| Hopelessness | 1.24 | 1.04 | 0.86 | NS | 0.87 | 0.80 | 0.36 | NS |
| Duration of admission | - | - | - | - | 72.47 | 62.85 | 0.58 | NS |
| Age at first onset | - | - | - | - | 25.29 | 32.07 | 2.96 | 0.004 |
| Total admissions | - | - | - | - | 5.17 | 6.67 | 0.98 | NS |
| Age | - | - | - | - | 33.52 | 39.85 | 2.33 | 0.022 |
Definition of post-psychotic depression
The ICD-10 definition of post-psychotic depression (PPD, F20.4) requires that, along with general criteria for schizophrenia during the previous 12 months, the patient must still exhibit persistent hallucinations, thought disorder or negative symptoms not due to depression or neuroleptic medication. These criteria make many of the assumptions embodied in the theories outlined in the introduction, whereas in this study we are making no such assumptions and indeed we are attempting to discern empirical support for them. Hence, our definition revolves around depressed mood per se.
Given that we are concerned with depressed mood and not necessarily formal major depression, the definition of caseness is arbitrary; however, for reasons outlined in the introduction, we used a definition of ‘at least moderate depression’ (BDI score ≥15). The correlation between the self-report BDI and the interview-based CDSS approached unity (r=0.91) and the thresholds proposed by Addington et al (Reference Addington, Addington and Maticka-Tyndale1993) conformed almost exactly with the subgroups defined below using the BDI. The BDI criteria will be used in this and our subsequent companion paper.
Using this definition, 70% of the sample were depressed at onset (n=55): of these, 48 (87%) dipped below the threshold for at least one post-recovery follow-up observation, 26 (54%) of whom became depressed once again and the remaining 22 (46%) stayed below threshold; 5 (9%) were depressed at all follow-up points; and 2 (4%) were depressed at all but the final follow-up point.
Twenty-three subjects were not depressed at onset: thirteen (56%) exceeded the threshold on at least one occasion (post-recovery), nine (39%) remained below threshold and one (4%) became depressed at the recovery observation but remained below threshold at all future follow-up points.
Course types
Using these criteria, all but eight patients were assigned to the following groups:
Post-psychotic depression (PPD, n=39)
Group I: Depressed at onset, improvement and return of depression (n=26)
Group II: No depression at onset; depressed at one or more follow-up points (n=13)
No post-psychotic depression (non-PPD, n=31)
Group III: Depressed at onset; no depression throughout the follow-up period (n=22)
Group IV: No depression at onset or throughout the follow-up period (n=9)
Five patients did not recover from their acute illness throughout this follow-up period and a further three patients could not be assigned to the above groups. Of the three patients unable to be assigned, two were above threshold for all but the final follow-up point and the third was depressed at the recovery observation.
The potential problem of observer bias was controlled by allocation of subjects to one of the four groups once the collection of data had been completed.
For those patients with PPD, we defined the follow-up point immediately prior to its appearance as ‘pre-PPD’: in other words, the point in the follow-up period where the patient manifested no depression prior to the onset of PPD.
The individual subject variation in the timing of PPD, and therefore pre-PPD points, would make any attempt at analysing the data virtually impossible using the original temporal sequence. We therefore examined data at the pre-PPD and PPD stages by realigning individual subject data at the appropriate follow-up points. As the average number of days from the discharge interview to the pre-PPD observation was 167.5 (s.d.=124.9), the default ‘pre-PPD’ and PPD observations for those subjects who did not develop PPD (n=31) were those at 4 and 8 months after recovery, respectively.
The PPD groups
Figure 1 shows the evolution of PPD in each of the two PPD groups (groups I and II) juxtaposed with that for positive symptoms (SAPS total score) and negative symptoms (SANS total score).
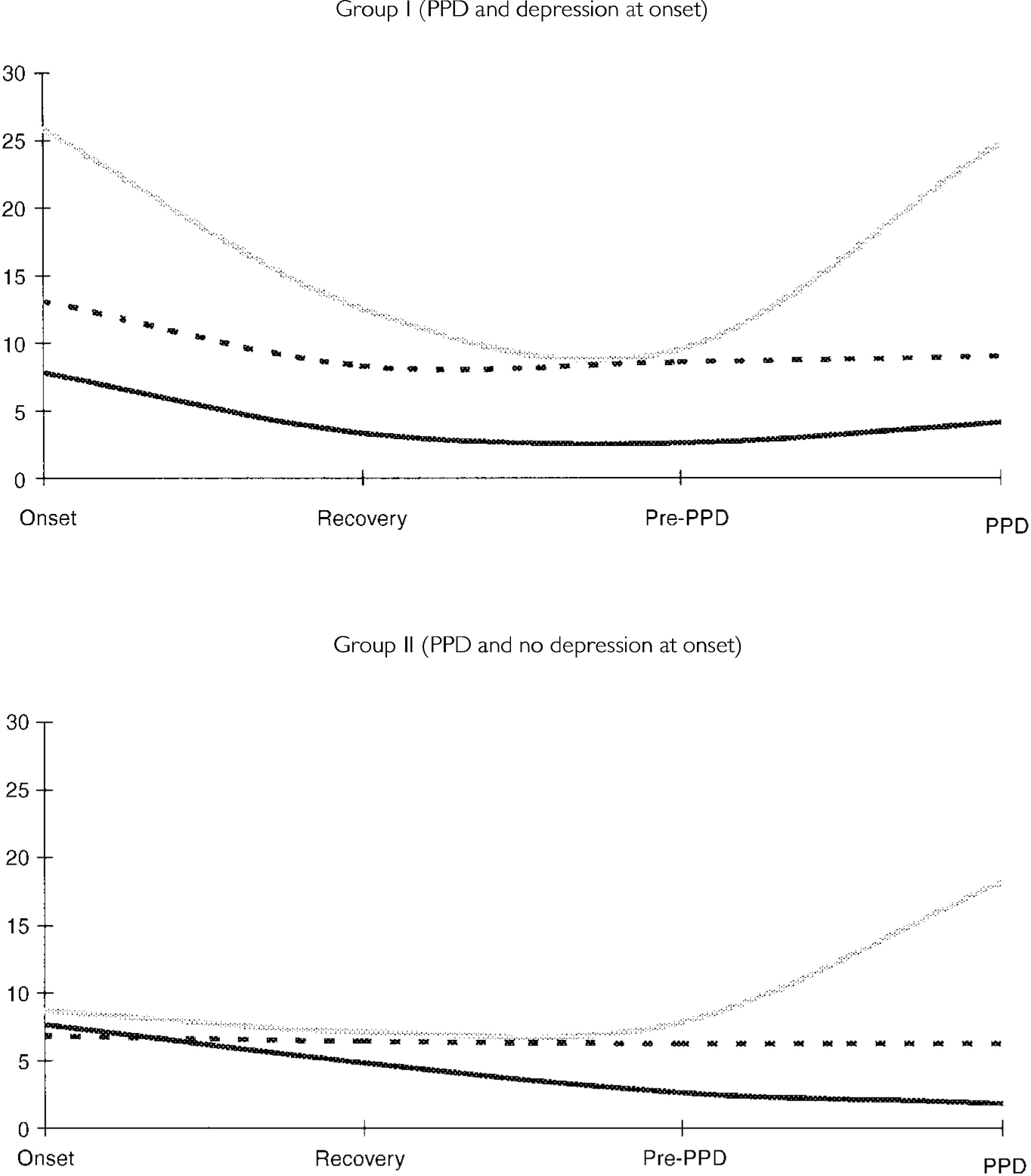
Fig. 1 Graphs depicting mean values for the course of depression and positive and negative symptoms for post-psychotic depression (PPD) groups I and II. [UNK], Scale for the Assessment of Positive Symptoms; [UNK], Scale for the Assessment of Negative Symptoms; [UNK], Beck Depression Inventory.
The SAPS scores remained unchanged during the PPD episode in both group I (pre-PPD v. PPD: t=1.84, P=0.08) and group II (t=1.34, NS). The SANS scores were also stable in group I (t<1, NS) and group II (t<1, NS).
Although the BDI score in group I reverted to that observed in the acute episode (BDI score=25), the SAPS score rose only slightly (but non-significantly). In group II the BDI score rose to 18.2, which is an unprecedented rise in this particular group, without a concomitant increase in SAPS. It should be noted that the mean level of depression during PPD was ‘moderate’ for the latter group and ‘severe’ for the former, using conventional criteria (see Reference WilliamsWilliams, 1992, for a review).
The non-PPD groups
Again, the evolution of depression in patients not manifesting PPD is juxtaposed with that for SAPS (Fig. 2). In the case of group III, SAPS declines in line with depression, whereas in group IV, by definition, the decline in SAPS does not coincide with that for depression.
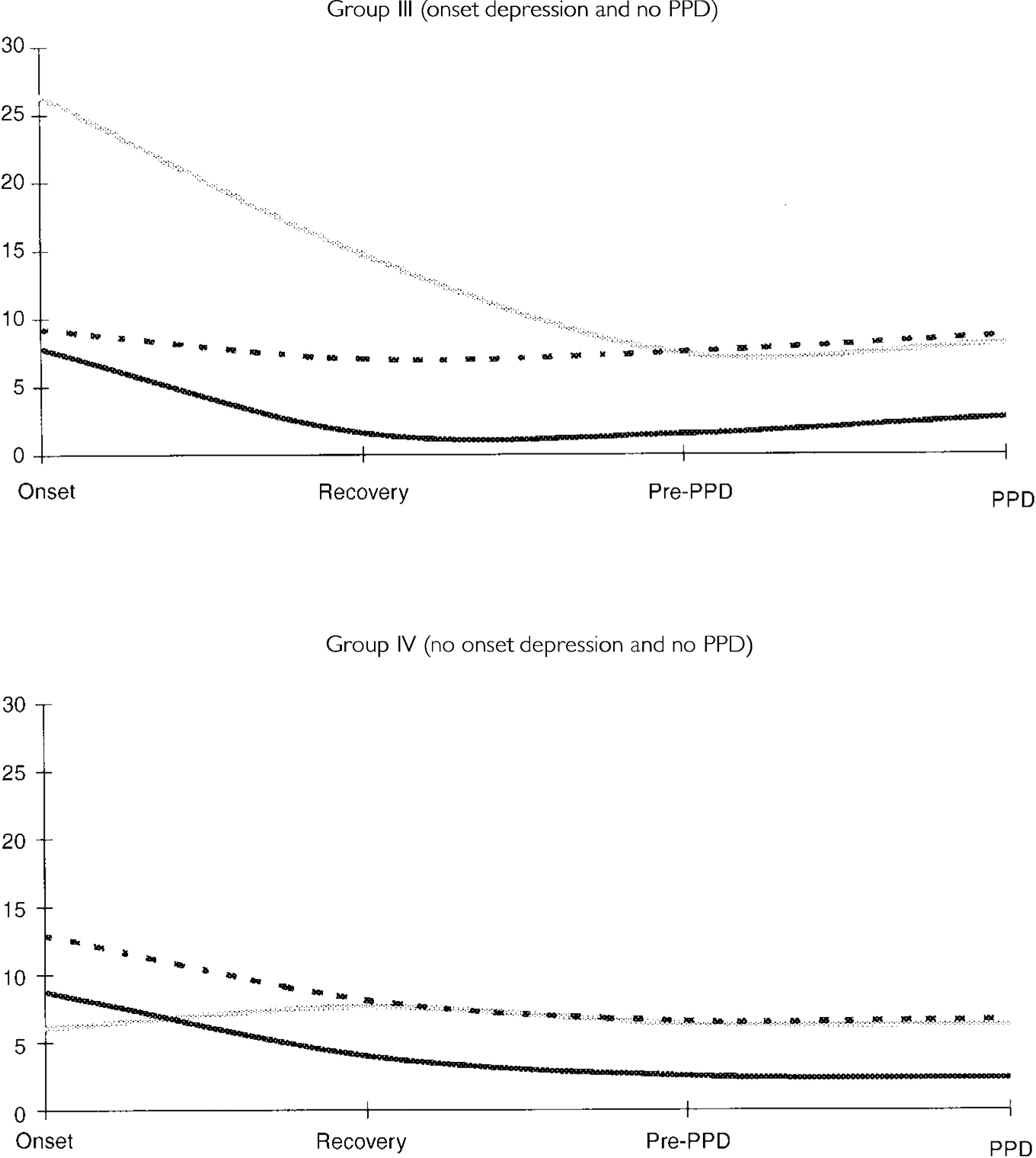
Fig. 2. Graphs depicting mean values for the course of depression and positive and negative symptoms for non-post-psychotic depression (PPD) groups III and IV. [UNK], Scale for the Assessment of Positive Symptoms; [UNK], Scale for the Assessment of Negative Symptoms; [UNK], Beck Depression Inventory.
Overall then, in groups I and III depression and positive symptoms follow the same course (combined n=48) during the acute episode, whereas in groups II and IV (n=22) depression and positive symptoms are not synchronous at the acute episode. However, on comparing patients with and without depression at onset (BDI score ≥15), there was no significant difference in SAPS score at onset, confirming that, in general terms, any link between positive symptoms and depression is confined to a subgroup.
Comparison of PPD with non-PPD groups
Positive symptoms
In order to determine whether the presence of PPD was the result of variation in positive symptoms, the groups were compared at each follow-up point. For this analysis groups I and II (PPD) and (III and IV) (non-PPD) were combined. Table 2 suggests a small mean rise in SAPS in each of the PPD groups; combining these groups into a single PPD group (n=39) revealed a modest significant rise in SAPS from 2.3 (2.6) to 3.6 (3.2) (t=2.3, P<0.05) during PPD; no overall change in SANS was apparent.
Table 2 Mean BDI, SANS and SAPS scores for groups I-IV at onset, prior to and during post-psychotic depression (PPD)

| Group | Measure | Onset (s.d.) | Follow-up point pre-PPD (s.d.) | PPD (s.d.) |
|---|---|---|---|---|
| PPD | ||||
| I (n=26) | BDI | 25.9 (7.0) | 9.5 (4.1) | 24.7 (9.4) |
| SAPS | 7.8 (3.5) | 2.7 (2.7) | 4.1 (3.1) | |
| SANS | 13.1 (4.6) | 8.6 (4.8) | 9.0 (3.6) | |
| II (n=13) | BDI | 8.7 (4.7) | 7.7 (3.4) | 18.2 (3.3) |
| SAPS | 7.7 (2.8) | 1.5 (2.3) | 2.6 (3.3) | |
| SANS | 9.2 (4.0) | 6.2 (5.7) | 8.6 (4.4) | |
| Non-PPD | ||||
| III (n=22) | BDI | 26.4 (8.3) | 7.4 (4.9) | 8.1 (5.1) |
| SAPS | 8.7 (2.4) | 2.5 (3.0) | 2.3 (2.1) | |
| SANS | 13.0 (4.4) | 6.5 (3.7) | 6.6 (3.1) | |
| IV (n=9) | BDI | 6.0 (4.6) | 6.5 (3.8) | 6.2 (4.4) |
| SAPS | 7.6 (2.7) | 2.6 (3.0) | 1.8 (2.9) | |
| SANS | 6.7 (2.7) | 7.5 (3.6) | 6.2 (7.3) |
This result suggests the presence of a subgroup showing a rise in positive symptoms, beyond the chance level, ranging from a ‘mild’ increase through to a full relapse. Thus we defined the threshold for a rise in positive symptoms equivalent to at least a ‘mild’ increase in symptoms; our operational definition was a rise equivalent to at least the margin of measurement error in the SAPS scale. From the interrater reliability data, the maximum discrepancy in SAPS global score ratings by M.B. and Z.I. was 3, which is equivalent to a single standard deviation. By defining subgroups of the PPD subjects using this discrepancy as a cut-off, 28 out of 39 (72%) did not display an increase in positive symptoms (i.e. a change of <3 in the SAPS global score) whereas SAPS scores for 11 subjects (28%) increased at PPD by at least the maximum interrater discrepancy. The mean SAPS global score for these 11 subjects at PPD was not significantly different from their SAPS score at onset (t=2.03, NS), suggesting that the rise in depression and positive symptoms in this subgroup was concordant with symptoms indicative of a psychotic relapse, which indeed conformed with our clinical impression (e.g. some were hospitalised). We conclude, therefore, that the remaining 28 subjects (36% of the whole sample) developed PPD without any marked increase in positive symptoms and were hence not displaying signs of psychotic relapse. This now becomes the new ‘pure strain’ PPD sample.
Negative symptoms
A similar investigation of the depressed and non-depressed subjects' extent of negative symptoms during the pre-PPD and PPD stages was also conducted. No overall change in SANS was apparent (Table 2). These results clearly indicate the stability of negative symptoms during the pre-PPD and PPD stages as subjects become depressed, irrespective of changes in positive symptoms.
Drugs and side-effects
Information on prescribed neuroleptics was obtained at each of the follow-up points and converted to chlorpromazine equivalents (British National Formulary, 1996). In accordance with pharmacogenic theories of depression in schizophrenia, the two groups were compared at each follow-up point to determine whether the presence of PPD was the result of neuroleptic exposure. No differences were observed at any of the follow-up points (F<1 for all).
Similarly, the two groups were compared for side-effects using the AIMS scale. At no point in the follow-up period did the PPD group differ in severity of side-effects using either the global or composite item measures.
Is PPD just an early sign of relapse?
It can be argued that the rise in depression during the PPD phase may be an early sign of a further psychotic episode, because dysphoria is a known precursor of psychotic relapse (Reference Birchwood, Smith and MacMillanBirchwood et al, 1989), rather than PPD per se. One way of addressing this issue is to establish the presence of psychotic symptoms following PPD. A comparison of positive symptoms after the PPD stage could be investigated only for those subjects who developed PPD at the third or fourth observation points, where follow-up data would therefore be available (i.e. at the fourth or fifth observation, respectively). Hence, there would be no follow-up data for subjects developing PPD at the fifth (and final) observation. Sixty-four per cent of subjects (n=18) who developed PPD had follow-up data after the PPD stage. For these cases, the mean SAPS global score was not higher at the subsequent observation than that observed at PPD (2.52 (2.50) v. 2.76 (2.66); t=0.38, NS) and thus does not support the argument that the rise in depression at PPD is a precursor to the onset of relapse.
Who develops PPD?
Of the 28 patients developing PPD, 68% were also depressed at onset. A total of 22/48 (46%) with depression at onset did not develop PPD and conversely 9/28 (32%) with PPD were not depressed at onset. Overall, the presence of depression at onset did not raise the risk of PPD (χ2=0.63, NS). There were no differences between the groups with (n=28) and without PPD (n=31) for: age at onset, duration of illness or total number of admissions; gender, marital status or ethnicity; or being under a section of the Mental Health Act.
Depression during acute psychosis
Definition
The wide variation in depression during the acute episode was not anticipated and here we distinguish those individuals with and without depression at onset using the same criteria (BDI score ≥15). This yields a group of patients with acute psychosis who are not depressed: 39/105 (37%) for the whole cohort and 22/78 (28%) for the sample completing all follow-up points. The mean BDI score for the depressed group was 27.7 (8.5) and for the non-depressed was 7.4 (4.4), indicating that the depressed group were, on average, ‘severely’ depressed. Contrary to expectation, there was no difference in SAPS global score between these depression groups: depressed=8.2 (3.7); not depressed=7.8 (3.1). Similarly, there was no difference between these groups in SANS global score: depressed=11.8 (4.7); not depressed=11.2 (4.9).
Who develops depression at onset?
People with depression at onset were younger at their first episode (30 v. 25 years; F=6.1, P<0.01) and younger at inclusion to the study (40 v. 32; F=10.8, P<0.001). There were no differences between the groups in neuroleptic dose or drug side-effects.
Hopelessness and suicidal thinking
A total of 54% of non-relapsing depressed patients at the PPD stage also reported suicidal thinking or worse on the CDSS, including 18% who had made suicidal plans and 4% who had undertaken a suicide attempt designed to end in death. Similarly, 36% of those with PPD expressed a concurrent persistent sense of hopelessness about the future (P<0.01 for both).
One-year prevalence
In order to gauge the level of occurrence of these features using this unique longitudinal perspective, we calculated the prevalence of at least moderate severity levels of depression or hopelessness or suicidal thinking across the three follow-up points over the 12-month envelope. Excluding the acute psychotic and recovery points, the 12-month prevalence for subjects with moderate levels of depression and hopelessness amounted to one-third (33.3%) of the sample, whereas that for subjects who were moderately depressed and suicidal was 20.5%. Finally, 61% during the 12 months after discharge from hospital experienced at least moderate levels of depression or suicidal ideation or hopelessness at a follow-up observation.
DISCUSSION
To the best of our knowledge, this is the first study to investigate the course of depression in schizophrenia within a longitudinal framework using this density of follow-up observation, the nearest comparable study being that of Leff et al (Reference Leff, Tress and Edwards1988). Given the frequency of follow-up and the assessments required, the level of concordance with the research protocol was exceptional.
On the basis of our definition of PPD, 36% (28/78) of patients in the study developed depressive symptoms of at least moderate intensity during the 12 months following an acute psychotic episode. It is important to point out that at the follow-up point immediately preceding the onset of PPD (i.e. pre-PPD) all these subjects were not depressed. The average time to PPD after recovery was 248 days or about 8 months, whereas the average number of days to PPD from the onset of psychosis was 304. Earlier studies have observed prevalence rates for PPD at 38% (Reference Van Putten and MayVan Putten & May, 1978), 39% (Reference RoyRoy, 1981) and 45% (Reference Leff, Tress and EdwardsLeff et al, 1988). Our sample consists of a high proportion of chronic and multiple-relapse cases within a socio-economically depressed inner-city area, more so than in previous studies, although these similar rates of PPD suggest that chronicity or relapse history may not alone be predictive of PPD and its origin may lie elsewhere. This is underlined by recent observations of a high rate of depression in first-episode subjects (Reference Addington, Addington and PattenAddington et al, 1998), and in the present study 50% of first-episode subjects developed PPD compared with 32% for those with multiple relapses (t=3.1, P<0.01). Overall, then, the sample's bias towards youth and the differential rate of PPD in the first-episode group need to be kept in mind when considering the generalisability of the data.
Analyses reveal that, for the patients developing ‘pure strain’ PPD, no significant changes are observed in positive symptoms, negative symptoms, the severity of side-effects or drug dose during the follow-up period.
The results clearly indicate the stability of negative and positive symptoms during the pre-PPD and PPD stages as subjects become depressed. To our surprise, correlational analyses between SANS global score and sub-scales and BDI for depressed subjects at the PPD phase indicate no significant associations between PPD and negative symptoms (all r<0.16, NS). We support Siris's (Reference Siris, Hirsch and Weinberger1995) position that the major difference between depression and negative symptoms is ‘blue mood’, a valuable indicator of depression that differentiates it from symptoms such as anhedonia, alogia, affective flattening and apathy, providing a clear rationale for distinguishing negative symptoms from depression. Finally, the risk of PPD was unaffected by the presence of depression during the acute psychotic stage. This suggests that the processes underlying PPD and depression at onset are different, and in line with the theories outlined in the introduction.
An unexpected finding was that about one-third of patients in acute psychosis were not depressed and the remaining two-thirds displayed mostly severe depression. Furthermore, there were no significant differences between the positive symptoms, drug dosage or severity of side-effects between these two groups at onset. Finally, there is substantial evidence that suicidal thinking and hopelessness accompany depressive pathology in the period following remission of acute psychosis. In the context of our 1-year prevalence rates for suicidal ideation, parasuicide and suicide of 23%, which are in line with previous results of 25% (Reference Roy and RoyRoy, 1986) and 10% (Reference Mortensen and JuelMortensen & Juel, 1993), there is a considerable need to establish a theoretical framework and preventive therapy for this most serious of problems, which shows a clear linkage with PPD.
The course patterns
We find evidence to support two of the course patterns outlined by Leff (Reference Leff and DeLisi1990). Depression can follow the same course as positive symptoms (during acute psychosis and relapse) and present de novo during follow-up without a change in positive symptoms (i.e. PPD). We found no evidence that depression emerged immediately following the remission of positive symptoms. Pharmacogenic theories are not supported either during acute psychosis or in the following 12 months. Similarly, negative symptoms remained stable whether PPD was observed or not. In addition, the study attempted to employ stringent criteria at recruitment and to define clearly the nature of PPD, and therefore we do not believe that diagnostic variation provides an explanation for these results.
Methodological considerations
In order to control for interviewer bias the BDI (self-report) and CDSS (observerrated), two highly correlated and virtually interchangeable depression inventories (Reference Addington, Addington and Maticka-TyndaleAddington et al, 1993), were utilised. These measures were highly intercorrelated (r=0.91). Interrater reliability for the SANS and SAPS was also established at various junctures throughout the study, and shown to be satisfactory.
We conclude that the experiment embodied little measurement error, and that insufficient to distort the main results.
What is PPD ?
The ICD-10 definition of PPD (F20.4) requires that, alongside a general criterion for schizophrenia during the previous 12 months, the patient must still exhibit persistent hallucinations in any modality, symptoms of thought disorder or certain negative symptoms that are not due to depression or neuroleptic medication. Based upon these criteria, none of our PPD subjects would conform to ICD PPD but would be simply depressed. We suggest that there is a strong case for further investigation of the diagnostic criteria for PPD. The ICD-10 criteria seem to be rooted in the assumption that depression in schizophrenia is an endemic feature of the psychotic process.
We have argued that although PPD is embedded in the realities of a psychotic illness, it is the beliefs or appraisals about psychosis made by those who experience it that are important (Reference Birchwood, Iqbal, Wykes, Tarrier and LewisBirchwood & Iqbal, 1998; Reference Rooke and BirchwoodRooke & Birchwood, 1998). In our subsequent companion paper this hypothesis is put to the test.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Patients, particularly those experiencing first-episode psychosis, need to be monitored for post-psychotic depression (PPD)/hopelessness/suicide risk some weeks after the acute episode.
-
▪ Patients' aspirations and perceived losses need to be assessed and subject to therapy.
-
▪ Developing a sense of control over psychosis may prevent feelings of entrapment and later PPD.
LIMITATIONS
-
▪ The study is a prospective snapshot of PPD following an acute episode.
-
▪ It is difficult to be certain whether the vulnerabilities were markers or risk factors.
-
▪ The inner-city provides the context for study.
ACKNOWLEDGEMENTS
We thank Professor Paul Gilbert for reviewing earlier drafts of the papers.







eLetters
No eLetters have been published for this article.