Introduction
The creation of the Montreal Neurological Institute (MNI) can be traced to a proposal that Charles F. Martin, Professor of Medicine at McGill University, made in 1917. He proposed that the Departments of Medicine, Surgery, and Gynaecology each name a professor and two assistants whose practice would be limited to a clinical unit in one of the University’s hospitals. They would forego private practice and receive a salary from the University, for which they would limit their clinical activities and devote most of their time to teaching and research. Reference Lewis1,Reference Entin, Hanaway and Nimeh2 McGill’s faculty and governance rejected Martin’s plan because they feared that it would decrease the chosen hospital’s income. Martin visited William Osler in July 1918 to enlist his support. Osler then wrote to Herbert Stanley Birkett, the Dean of McGill’s Faculty of Medicine, and to the Rockefeller Foundation, in November 1919, in favor of Martin’s plan. Reference Osler3 The Rockefeller Foundation eventually funded a Chair of Medicine and a University Medical Clinic at McGill’s Royal Victoria Hospital (RVH) in 1923. A second University Clinic was created for Wilder Penfield in 1928 as head of McGill’s newly created Sub-department of Neurosurgery at the RVH. Penfield soon outgrew the facilities allotted to him and in 1933 he secured funding from the Rockefeller Foundation, from the governments of Canada, Québec, and Montréal, and from Montreal philanthropists in order to create the MNI. The MNI was unique in its structure and staff. Its faculty held full-time university appointments and their offices, clinics, and research laboratories were all housed in the Institute, facilitating interaction between clinicians and basic scientists who addressed the same problems from different vantage points. There were clinical and research laboratories in Neurophysiology, Neurochemistry, Neuroanatomy, and Clinical Psychology. Reference Leblanc4 Admission to the MNI’s training programs was predicated on an applicant’s willingness to perform independent research in one of its laboratories, which assured that its trainees foresaw an academic career. This paper shows that the MNI’s success in integrating clinical care, research, and teaching was the model for the National Institute of Neurological Diseases and Blindness (NINDB), and that the NINDB’s recruitment of MNI trainees at its inception assured that it would be at the forefront of neuroscience in the USA from its very beginning.
The National Institute of Neurological Diseases and Blindness
Donald Tower, who later headed the NINDB, described the state of neurology and neurosurgery in America after World War Two:
At a time when neurological and neurosurgical training was at its lowest ebb in North American and European centers, two facilities bridged the gaps. The MNI rapidly expanded its training programs, attracting a mature cadre of trainees and researchers worldwide. Later, the US Veterans Administration (VA) initiated a neurological training program at various of its medical-school-based VA hospitals. VA neurology was under the direction of Pearce Bailey, fresh from US Naval Service. Literally speaking, these two programs resurrected American neurology from its nadir and began the rebuilding. Reference Tower5
Pearce Bailey Jr. studied psychology at Columbia University and at La Sorbonne in Paris. He graduated in medicine from the University of South Carolina in 1941 and completed his residency in neurology at Columbia University in 1944. He then served in the American Armed Forces as Head of Neurology at the Philadelphia Naval Hospital. He was appointed head of the neurology program of the Division of Neuropsychiatry of the Veteran’s Administration (VA) in 1946, and then as the first Director of NINDB in 1950. Reference Bailey, Tower and Brady6–Reference Ferraras, Hannaway and Harden8
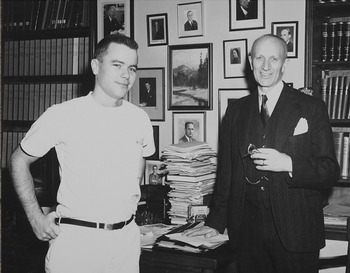
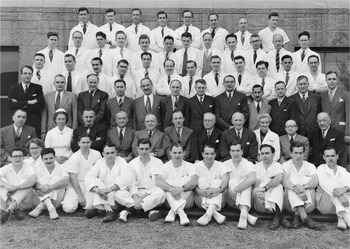
Bailey met with Maitland Baldwin and Milton Shy in Denver in 1951. Baldwin and Shy had trained at the MNI and both had been on staff as Demonstrators in Neurosurgery and Neurology, respectively, before relocating to the University of Colorado (Figures 1 and 2). As a result of this meeting, Baldwin, 33 years old, agreed to head the NINDB’s Surgical Neurology Branch, and Shy, 31, agreed to head Medical Neurology, effective the first of May 1953. They soon recruited six MNI fellows: Cosimo Ajmone-Marsan, Choh-Luh Li, and John Van Buren to the Surgical Branch, Donald Tower and Anatole Dekaban to the Neurology Branch, and Igor Klatzo as neuropathologist to both branches (Table 1, Figure 3).

Figure 1: Baldwin and Penfield in Penfield’’s office, Christmas, 1949. Montreal Neurological Institute archives. All rights reserved.

Figure 2: Milton Shy, 1949. Montreal Neurological Institute archives. All rights reserved.

Figure 3: MNI staff, residents, and fellows 1949–1950. Second row: Penfield (8). Fourth row: Baldwin (2), Ajmone-Marsan (3), Dekaban (7). Fifth row: Van Buren (2), Li (6), Shy (7). Top row: Klatzo (5). Montreal Neurological Institute archives. All rights reserved.
Table 1: MNI trainees and the NINDB

* National Institute of Neurological Disorders and Stroke. ** John Lord was in private practice but was a consultant to the Surgical Neurology Branch of the NINDB.
The Surgical Neurology Branch
Pearce Bailey’s plan for the NINDB prioritized the care of persons with epilepsy, most notably those with psychomotor seizures. “Temporal lobe epilepsy merits investigation,” he wrote, “because of its importance as a public health problem. All epilepsies constitute a social and vocational problem beyond their medical aspects and in this sphere the victims of temporal lobe seizures, with their diffuse and bizarre, psychomotor manifestations, carry the most severe handicap of all.” Reference Baldwin and Bailey9 Baldwin’s role in the discovery of mesial temporal sclerosis and of the technique for its resection Reference Leblanc4 were undoubtedly the reasons for his recruitment to head the NINDB.
Maitland Baldwin
Maitland Baldwin matriculated at Harvard College and attended medical school at Queen’s University, Kingston, Canada. An encounter with Wilder Penfield at Queen’s set Baldwin’s course towards neurosurgery. He graduated medical school in 1943 and interned at the Montreal General Hospital. Baldwin served in the United States Marine Corps following his internship and later came to the MNI to train in neurosurgery in 1947, after his discharge from the Navy. He moved to the University of Colorado in 1951, where he founded the Division of Neurosurgery, before moving to Bethesda.
As Cosimo Ajmone-Marsan observed, “Baldwin’s heading the Surgical Neurology Branch of the Institute [NIH] illustrated Bailey’s intentions to make epilepsy, with an emphasis on this special form of treatment [surgery], one of the major areas of research within the intramural program” Reference Ferraras, Hannaway and Harden8 (Figure 4). To do so, Baldwin turned to the MNI and recruited Ajmone-Marsan in electroencephalography and electrocorticography, Choh-Luh Li in experimental neurosurgery, Igor Klatzo in neuropathology, and John Van Buren as the NINDB’s second neurosurgeon. Baldwin’s wife, Shirley Lewis, who had been an operating room nurse at the MNI, was his scrub nurse.

Figure 4: Wilder Penfield and Maitland Baldwin on 4 October 1960 during Penfield’s visit at the NINDB, when he gave a lecture entitled Conscious Experience–What the Brain Records and Where. National Institutes of Health Archives. Public domain.
Baldwin’s approach to the surgical treatment of epilepsy at the NINDB mirrored Penfield’s at the MNI, as described by Ajmone-Marsan:
Baldwin transferred a very similar organizational approach to the field of surgical management of epilepsy from the MNI to the NIH [NINDB]. This approach emphasized a detailed analysis of epileptic seizures, mostly through a careful history and/or a detailed description by patients, their family, and hospital staff, and a close collaboration with electroencephalographers, neuropsychologists, and neuroradiologists. Radiographs consisted mainly of plain X-rays, pneumoencephalograms, and, occasionally, angiograms … Final discussion of a case with the presentation of specific findings from each of the various team members took place at weekly “EEG Conferences” in the presence of the patient. As was the case in Montreal, acute electrocorticography monitoring in the course of cortical exposure [at surgery] was routinely performed. This technique played an important role in the outline of the regions to be excised and, in particular, to check for completion or, if necessary, to extend the ablation of such regions after the main excision had been performed. The surgical procedure itself included a protracted period of cortical stimulation studies (with the patient awake and alert), not only to identify important functional areas but also to extend Penfield’s original investigations on cortical localization of secondary motor and sensory areas Reference Ferraras, Hannaway and Harden8
The NINDB’s epilepsy program attracted the attention of the International League Against Epilepsy, which held its second Colloquium on Temporal Lobe Epilepsy in Bethesda in 1957. The proceedings of the colloquium were published the following year and constitute the most comprehensive view of temporal lobe epilepsy and its treatment at the time Reference Baldwin and Bailey9 The major contributions came from the MNI and the NINDB. Of note were addressed by Jasper on the electrophysiology of the mesial temporal lobe, by Ajmone-Marsan and Van Buren on pre-operative depth electrode recordings, by Ajmone-Marsan and Baldwin on electrocorticography, and by Tower on the neurochemistry of epileptic seizures. Five groups reported their experience with the surgical treatment of temporal lobe seizures: Theodore Rasmussen and Jasper from Montreal, Francis Gibbs and Percival Bailey from Chicago, Henri Gastault from Marseille, Murray Falconer from London, and Paolo Niemeyer from Rio de Janeiro. It is striking to read that the patients operated upon for temporal lobe epilepsy in Marseille, Chicago, and London came from psychiatric institutions, in stark contrast to the MNI. It is also noteworthy that Paolo Niemeyer first described the technique of selective amygdalo-hippocampectomy during the Colloquium.
Cosimo Ajmone-Marsan
Ajmone-Marsan was to Baldwin as Herbert Jasper was to Penfield. He graduated in medicine from the University of Torino, Italy, in 1942, and worked at the university’s neurological and psychiatric clinic during the war. He received his accreditation in neuropsychiatry in 1947. Ajmone-Marsan came to the MNI in 1949, where Jasper took him under his wing, taught him to read EEGs and electrocorticograms, and soon appointed him assistant electroencephalographer and electrocorticographer. Together they studied the relationship of the cortex and thalamus and published the influential Stereotaxic Atlas of the Diencephalon of the Cat, which could be found in most neurophysiological laboratories. Reference Stoll, Ajmone-Marsan and Jasper10–Reference Jasper and Ajmone-Marsan12 Ajmone-Marsan was recruited to the NINDB in January 1954 as Chief of the Clinical Neurophysiology Branch, whose structure and function mirrored the MNI’s, as he confided in a letter to Penfield on February 3, 1955: Reference Ajmone-Marsan13
It took me a certain time to organize the department of EEG and to train the technicians: of big help in this regard was the opportunity offered to me by Dr Jasper who accepted one of my girls [sic] for a training period of three months at the MNI (Figure 5). Now I can say I have a copy (in a very small scale) of the basement of the MNI. The type of routine work is indeed very similar to that carried out in Montreal, and I try my best to help Mait Baldwin in the localization of epileptogenic foci, particularly in cases of temporal lobe seizures. …. In my free time I am working experimentally on cats, trying to get some more information about the nonspecific system [of the thalamus], and particularly about its relations with the specific system, with the idea of getting some experimental evidence on the hypothesis offered by you at the Ste. Marguerite Symposium. Footnote *

Figure 5: Staff of the NINDB’s Department of electroencephalography. Cosimo Ajmone-Marsan is standing, fourth from the left. Maureen Benson-DeLemos, the EEG department’s chief technician who was trained at the MNI is at center in the front row. National Institutes of Health Archives. Public domain.
Ajmone-Marsan was expert in analyzing seizure patterns and the pathways by which epileptic activity spreads from a primary focus, such as the hippocampus, to other areas of the cortex, such the lateral temporal lobe. This experience was conveyed in an influential book, The Epileptic Seizure Its Functional Morphology and Diagnostic Significance – “bearing the hallmark of the Montreal School” as one reviewer put it – on the investigation of epileptic seizures. 14,Reference Ajmone-Marsan and Ralston15
As Ajmone-Marsan had discussed at the temporal epilepsy colloquium, depth electrode recordings were integral to the NINDB’s surgical epilepsy program. Reference Li and Baldwin16,Reference Ludwig, Ajmone-Marsan and Van Buren17 Basic electrophysiological research, however, was Choh-Luh Li’s area of expertise.
Choh-Luh Li
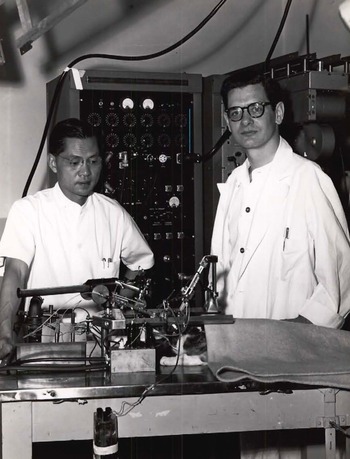
Li came to the MNI in 1946 from Shanghai’s National Medical College to train in neurosurgery, which he began by studying the anatomical connections of the temporal lobe with Jerzy Olszewski. Reference Li18 He then teamed with Jasper and, using microelectrodes that he made himself, shed new light on the electrophysiology of the cortex and thalamus Reference Li19–Reference Li, Cullen and Jasper22 (Figure 6). As Jasper acknowledged:

Figure 6: Choh-Luh li (left) and Chester Cullen (right) in the neurophysiology laboratory at the MNI, 1954. Li is performing single cell recordings from the cortex of a cat, with Cullen’s assistance. Cullen later became an authority on multiple sclerosis, a condition from which he suffered. Richard Leblanc MD. All rights reserved.
“The microelectrode studies with Dr Li have been most illuminating. It has been found that there is a veritable beehive of activity going on in the depths of the cortex… Gradually the true pattern of cortical activity is being revealed: it is organized in depth, and under the constant influence of to-and-fro currents from subcortical structures, the delicate balance of controlled function being lost in the explosive chain reaction of the epileptic discharge.” Reference Jasper23
Baldwin recruited Li in 1954 to head the Section of Experimental Neurosurgery at the NINDB where he studied the electrical activity of single neurons in cortical slices, in animals, and in humans. Tower, echoing Jasper, commented: “Li could make beautiful microelectrodes… All that was necessary was to drop the microelectrode into a neuron in that slice of brain in order to see what the effect of stimulation or change in the ionic environment might be.” Reference Ferraras, Hannaway and Harden8 Li’s work at the NINDB supported Jasper’s theory of synchronization of cortical neurons in an important paper published in Science and expanded his and Jasper’s work on the influence of the thalamus on cortical sensorimotor function. Reference Li, McLennan and Jasper24–Reference Li27 The latter became clinically relevant as the thalamus became a target in the treatment of Parkinson’s disease at the NINDB under John van Buren.
John van Buren
Van Buren began training in neurosurgery at the MNI in 1949. Reference Jasper and Van Buren28 Baldwin recruited him to the NINDB in 1955, where his research on cortical-subcortical interaction, the semiology of psychomotor seizures, the hippocampal amnesic syndrome, perception, and speech mirrored the work of Penfield, Baldwin, Lamar Roberts, and Brenda Milner at the MNI. Reference Leblanc4
The MNI’s and the NINDB’s interests further converged in the 1960s with the development of stereotactic thalamotomy for Parkinson’s disease. While Jasper and Gilles Bertrand investigated the electrophysiology of the human thalamus as a preliminary procedure before thalamotomy, Van Buren was using similar methods to define the surgical anatomy of the thalamus. Reference Bertrand and Jasper29,Reference Van Buren and Maccubbin30 The latter led to Van Buren and Rosemary Borke’s publication of an influential atlas of the thalamus and its connections. Reference Van Buren and Borke31 Gilles Bertrand and Christopher Thompson, the MNI’s computer engineer, used Van Buren and Borke’s atlas to create the first computerized atlas of the thalamus, which they used as a guide during human thalamotomies. Reference Bertrand, Olivier and Thompson32
Igor Klatzo
Igor Klatzo arrived at the MNI as a neuropathology research fellow in 1948, where he worked with William Cone on the cytological characterization of malignant brain tumors. Reference Klatzo33 He had relocated to McGill’s Pathological Institute, situated adjacent to the MNI, before his recruitment to the NINDB in 1956. After his move to Bethesda Klatzo kept in close contact with the MNI’s Department of Neurochemistry in his work on cerebral edema, Reference Pappius, Klatzo and Elliott34 which led to its characterization as vasogenic or cytotoxic according to the electrolyte and protein constituents of the edema fluid. Reference Klatzo35 Having discovered the association of cytotoxic edema and cerebral ischemia, Klatzo turned his attention to stroke and shed new light on its pathophysiology and complications, which drew neurologists into a field that had been previously neglected. Reference Olsson, Crowell and Klatzo36–Reference Katzman, Clasen, Klatzo, Meyer, Pappius and Waltz38 Klatzo also holds the distinction of having described the cytopathology of transmissible spongiform encephalopathy. Reference Klatzo, Gajdusek and Zigas39
The Medical Neurology Branch
Milton Shy
Milton Shy graduated from the University of Oregon Medical School in 1943. Following his internship, he completed a year of residency in medicine at the RVH and a year of neurology at the MNI, subsequently joining the United States Army Medical Corps. Following his discharge from the Army he studied neurology at the National Hospital for the Paralyzed and Epileptics, Queen Square, London, England. He returned to the MNI in 1948 to complete his training in neurology. He studied the electrophysiology of peripheral nerves and muscles with Jasper, and the effects of cortisone on neuromuscular disorders with Donald MacEachern, the MNI’s Head of Neurochemistry. Reference Shy, Cone, Brendler, Rabinovitch and McEachern40–Reference McEachern and Shy42 Shy pursued his interest in the neurochemistry of neurological diseases at the NINDB, where he made significant contributions to the biochemistry of muscular dystrophy, and of myasthenia gravis. Reference Shy43–Reference Rowland, Korengold, Jaffe, Berg and Shy45 Shy was an early proponent of muscle biopsy in the investigation of neuromuscular diseases, which led to his discovery of central core disease, the elucidation of the floppy infant syndrome, and the characterization of the neuromyopathy that accompanies malignancy Reference Shy46–Reference Shy and Silverstein49 (Figure 7). Shy is best remembered for the discovery with Glen Drager of multiple system atrophy. Reference Shy and Drager50 As a result of his work with MacEachern and his own contributions to the understanding of neuromuscular diseases, Shy understood the importance of creating a section of neurochemistry at the NINDB, a task that he entrusted to Donald Tower.

Figure 7: Milton Shy (standing) and Godwin Greenfield at the NINDB, during their studies on the "floppy infant" syndrome. Reference Greenfield, Corman and Shy48 Image courtesy of the British Neuropathological Society archives. Reproduced with permission of the British Neuropathological Society.
Donald Tower
Donald aspired to become a neurosurgeon when he came to the MNI in 1947. Since he had studied chemistry as an undergraduate, Penfield suggested that he join McEachern and Allan Elliott in neurochemistry, with whom he investigated the cholinergic system in epilepsy and the role of sodium and potassium in cerebral edema. Reference Tower51–Reference Tower and Elliott54 After working with McEachern and Elliott, Tower decided to forego neurosurgery for a career in neurochemistry, although his experience as a neurosurgical resident still proved useful: “My year scrubbing with the Penfield team would stand me in good stead since I now knew the limitations under which the surgeon operated, and the criteria used to characterize the brain samples. It became my habit to sit in the OR gallery to observe the results of cortical stimulation and EEG recordings and to personally pick up the excised cortical samples for immediate processing and study in the lab.” Reference Tower5
Tower was appointed Associate Neurochemist at the MNI, a position that he held until 1953 when he joined the NINDB to head the Section of Clinical Neurochemistry, and where he continued his work on the biochemistry of excised epileptic foci. Reference Tower55 Shortly after his arrival at the NINDB, Elliot, Alva Bazemore, and Ernst Florey discovered that gamma amino butyric acid (GABA) is an inhibitory neurotransmitter. Reference Elliott, Bazemore and Florey56 GABA was the first of this class of neurotransmitters to be discovered, and Tower undertook to investigate its role in normal and epileptic cortex. Tower’s investigations of the cholinergic, GABAergic, and glutaminergic systems generated widespread interest in the biochemistry of epilepsy, which led to the publication of the influential text Neurochemistry of Epilepsy in 1960. Reference Tower and Kugelmass57
Tower was appointed acting director of intramural research at the NINDB in 1967-1968 and “spent a year learning how to conduct the $100+ million program in neuroscientific research and training.” Reference Tower5 He was appointed Director of the National Institute of Neurological Disorders and Stroke in 1973, a position that he held until his retirement in 1981.
Anatole Dekaban
Shy recruited Anatole Dekaban to head Developmental Neurology at the NINDB in 1955. Dekaban received his MD in 1944 from the University of Warsaw. He fled Poland in 1947 and gradually made his way to the MNI as a research fellow in 1949, where he studied the embryogenesis of the brain and malformations of the central nervous system. Reference Dekaban58,Reference Dekaban59 Dekaban left the MNI for the University of British Columbia in 1952, before later relocating to Bethesda. There he studied malformations of the central nervous system in children of diabetic mothers, and the teratogenic effects of X-irradiation during pregnancy, work that he had begun at the MNI. Reference Dekaban60,Reference Dekaban61 The latter was of immediate concern during the Cold War because malformations of the nervous system had been found in children born after the bombing of Hiroshima. Dekaban’s major contributions, however, were in the study of inherited nervous system malformations associated with disorders of lipid and glucose metabolism, which led to the first attempts at enzyme replacement therapy in these disorders. Reference Brady, Tallman and Johnson62,Reference Brady, Pentchev, Gal, Hibbert and Dekaban63
Discussion
The MNI’s success in integrating clinical care, basic research, and teaching drew Pearce Bailey’s attention, and he turned to MNI-trained clinician-scientists and basic researchers to staff the newly founded NINDB, where they continued the work that they had begun in Montreal. This assured that the NINDB hit the ground running, which brought it immediate credibility as a center for the care of neurological patients and research into the disorders that afflicted them.
It is interesting to note that Penfield had misgivings about Baldwin and Shy taking on so much responsibility so early in their careers, especially without the support of university appointments. He shared his misgivings in a letter to Baldwin dated December 7, 1952, in which Penfield advises that he and Shy delay taking up the positions offered by Bailey:
Dear Mait:
Congratulations to you and to Milton Shy for this early recognition of your combined work. The constructive teaching and neurological thinking of Milton has attracted a good deal of attention in various areas. It is quite obvious that the two projects, one in Denver and the other in Washington, are altogether different. The first is primarily a splendid clinical opportunity and the second an opportunity in neurological research. It is not for me to presume to know what the right answer is, but I am fairly well acquainted with both of you. It seems to me that if at the end of five years in Denver this offer had come to you, and if at that time you were dissatisfied with what could be done there, I would have no hesitation in advising you to go to Washington. On the other hand, as things are my initial immediate reaction is that you would both do better to remain in Denver where you are beginning to be established. You have a university set up, which is usually the best in the long run, instead of a set up in a research institution with little support from general medicine and general surgery and all the important academic departments of a university. I believe you need, both of you, a period of at least five years of steady clinical work with gradually increasing laboratory development. I think you will be happy there [Denver]. The large number of neurosurgeons who seem to be competitors may be converted into associates by means of a neurological and neurosurgical, and perhaps neuropsychiatric, club or society which will raise the level of everyone’s performance. Even if you have to wait a few years before securing what you consider to be ideal, namely a neurological and neurosurgical separateness, I should be patient and thankful for the opportunity to work straight ahead with maximum contacts with surgery and medicine. It seems to me actually that you, Mait, need to be close to surgery for the time being. You need to be in contact with abdominal, urological, gynecological, and thoracic surgical complications and problems. You need that just as much as you need contact with the rarified atmosphere of neurology! I can visualize some of the great opportunities and the certain disappointments that await the Chiefs in Washington. In a sense this is what Harvey Cushing visualized and hoped to organize, namely a National Institute. The time for you two fellows to tackle it is 10 years hence, if ever. Please accept this snap judgement as a snap judgement… Reference Penfield64
Penfield’s advice should not be surprising, as it is the path that he trod before assuming the Directorship of the MNI, Reference Leblanc4 the same path that Theodore Rasmussen followed as he left the MNI to head Neurosurgery at the University of Chicago before eventually succeeding Penfield as Director of the MNI. So did William Feindel, the MNI’s third director, who left Montreal to create a Department of Neurosciences at the University of Saskatoon before returning as Rasmussen’s successor. This is clearly the path that Penfield favored for Baldwin and Shy. Fortunately for American neuroscience, they disregarded his advice.
Milton Shy left the NINDB in 1965 to chair the Department of Neurology at the University of Pennsylvania. He died two years later, aged 47, a few weeks after his appointment as Director of the New York Neurological Institute.
Maitland Baldwin enjoyed a full life, in which athletics and service to the United States Navy and Marine Corps Reserves played an important part. He succeeded Shy as Clinical Director of the NINDB when Shy was appointed Associate Director for Research in 1960, a position that Baldwin held until 1970 when he suddenly died at the age of 52. Francis O'Brien, who had trained with Baldwin at the MNI, and Anatole Dekaban, wrote his eulogy. They praised his meticulous surgical technique, administrative skills, and broad scientific interests, and praised “his charm, kindness, and goodwill.” Reference O'Brien and Dekaban65
Penfield inspired loyalty in those who believed in the MNI’s mission, which is carved in stone on the corner of the building. It reads: “Dedicated to the Relief of Sickness and Pain and to the Study of Neurology.” Those who left the MNI for the NINDB were true to this mission. As Tower wrote, “I do not think we could have started on such a high note, such a golden-age approach, if we had not had this opportunity to bring top-flight people to Bethesda.” Reference Ferraras, Hannaway and Harden8
Acknowledgements
I am grateful to Andreas Killen PhD, Department of History, the Graduate Center, City University of New York, for sharing his insights on Maitland Baldwin and to Yvan Prkachin PhD, Department of the History of Science, Harvard University, for sharing his knowledge of the Penfield archives of the Osler Library of the History of Medicine.
Disclosures
None.