In the past the content of paranoid thoughts was not to be discussed with patients. In the influential textbook Clinical Psychiatry, the view was expressed throughout the three editions from 1954 to 1969 that
‘Although it is a waste of time to argue with a paranoid patient about his delusions, he may still be persuaded to keep them to himself, to repress them as far as possible and to forgo the aggressive action they might suggest, in general to conduct his life as if they did not exist’ (Reference Mayer-Gross, Slater and RothMayer-Gross et al, 1954: p. 280)
Such ideas were not confined to psychiatry. A number of psychologists applied reinforcement techniques to try to reduce the time that patients spoke about delusions (e.g. Reference Wincze, Leitenberg and AgrasWincze et al, 1972; Reference Liberman, Teigen and PattersonLiberman et al, 1973). However, there has been a remarkable transformation in how delusions are viewed. Together with medication, recommended treatment now encourages clinicians to give most patients time to talk about their experiences and to use particular cognitive–behavioural therapeutic techniques to reduce distress (National Institute for Clinical Excellence, 2002; Reference Lehman, Kreyenbuhl and BuchananLehman et al, 2004).
But how should the content of delusional ideas be discussed? There are clearly lingering uncertainties in the mental health professions about this, as illustrated by a study of psychiatrist–patient routine consultations (Reference McCabe, Heath and BurnsMcCabe et al, 2002). It was found that patients repeatedly tried to talk about the content of their psychotic symptoms and in response doctors hesitated, responded with a question rather than an answer and, when a carer was present, even smiled and laughed.
In this article we focus on paranoid and suspicious thoughts, drawing on developments in the cognitive understanding and treatment of such experiences to describe how best to talk with patients about them.
What is paranoia?
Paranoid or persecutory delusions are a subtype of delusional beliefs. In essence, a delusion is a fixed, false belief. In clinical settings the belief is likely to be distressing or disruptive for the individual. However, there has long been debate about such definitions, in that most proposed criteria do not apply to all delusions. A more sustainable position is that of Reference Oltmanns, Oltmanns and MaherOltmanns (1988). Assessing the presence of a delusion may best be accomplished by considering a list of characteristics or dimensions, none of which is necessary or sufficient, that with increasing endorsement produces greater agreement on the presence of a delusion. For instance, the more a belief is implausible, unfounded, strongly held, not shared by others, distressing and preoccupying, the more likely it is to be considered a delusion. The practical importance of the debate about defining delusions is that it informs us that there is individual variability in the characteristics of delusional experience (Table 1). Delusions are definitely not discrete discontinuous entities. They are complex, multidimensional phenomena (Reference Garety and HemsleyGarety & Hemsley, 1994). There can be no simple answer to the question ‘What causes a delusion?’ Instead, an understanding of each dimension of delusional experience is needed: What causes the content of a delusion? What causes the degree of belief conviction? What causes resistance to change? What causes the distress? And clinicians need to think with patients about the aspect of delusional experience that they are hoping will change during the course of an intervention.
Table 1 The multidimensional nature of delusions

| Characteristic of delusions | Variability in characteristic |
|---|---|
| Unfounded | Sometimes the delusions reflect a kernel of truth that has been exaggerated (e.g. the person had a dispute with a neighbour but now believes that the whole neighbourhood is monitoring them and will harm them). It can be difficult to determine whether the person is actually delusional. With others the ideas are fantastic, impossible and clearly unfounded (e.g. the person believes that they were present at the time of the Big Bang and are involved in battles across the universe and heavens) |
| Firmly held | Beliefs can vary from being held with 100% conviction to being believed only occasionally when the person is in a particular stressful situation |
| Resistant to change | Some individuals are certain that they could not be mistaken and will not countenance any alternative explanation for their experiences. Others feel very confused and uncertain about their ideas and readily want to consider alternative accounts of their experiences |
| Preoccupying | Some people report that they can do nothing but think about their delusional concerns. For other people, although they firmly believe the delusion, such thoughts rarely occur to them |
| Distressing | Many beliefs, especially those seen in clinical practice (e.g. persecutory delusions), are very distressing but others (e.g. grandiose delusions) can actually be experienced positively. Even some persecutory delusions can be associated with only low levels of distress (e.g. the individual believes that the persecutor does not have the power to harm them) |
| Interferes with social functioning | Delusions can stop people interacting with others and lead to great isolation and abandonment of activities. Some can have a delusion and still function at a high level, including maintaining relationships and employment |
| Involves personal reference | In many instances the patient is at the centre of the delusional system (e.g. ‘I’ve been singled out for persecution’). However, friends and relatives can also be involved (e.g. ‘They’re targeting my whole family’) and some people believe that everybody is affected equally (e.g. ‘Everybody is being experimented on’) |
In contrast to the debates about defining delusions, diagnostic criteria for subtypes of delusional beliefs based on content have not been a topic of comment. This is perhaps because the issue is thought to be self-evident, but it is more complex than might be considered at first sight. There is great variety in the content of thoughts of a persecutory nature, for instance, in the type and timing of threat, the target of the harm, and the identity and intention of the persecutor (Reference Freeman, Garety and KuipersFreeman et al, 2001). Furthermore, terms such as paranoia, delusions of persecution and delusions of reference have been used interchangeably and to refer to different concepts. Reference Freeman and GaretyFreeman & Garety (2000) clarify the definition of persecutory delusions: the individual believes that harm is occurring, or is going to occur, to him or her, and that the persecutor has the intention to cause harm (Box 1). The second element of this definition distinguishes persecutory from anxious thoughts.
Box 1 Criteria for a delusion to be classified as persecutory (Reference Freeman and GaretyFreeman & Garety, 2000)
Criteria A and B must be met:
-
A the individual believes that harm is occurring, or is going to occur, to him or her
-
B the individual believes that the persecutor has the intention to cause harm
There are a number of points of clarification:
-
• harm concerns any action that causes the individual to experience distress
-
• harm only to friends or relatives does not count as a persecutory belief, unless the persecutor also intends this to have a negative effect on the individual
-
• the individual must believe that the persecutor at present or in the future will attempt to harm him or her
-
• lusions of reference do not count within the category of persecutory beliefs
How common is persecutory thinking?
Paranoid thoughts have traditionally been viewed as a symptom of severe mental illness. Reference Sartorius, Jablensky and KortenSartorius et al(1986) present findings from a World Health Organization prospective study in ten countries of 1379 individuals with signs of schizophrenia making first contact with services. Persecutory delusions were the second most common symptom of psychosis, after delusions of reference, occurring in almost 50% of cases. Persecutory beliefs are the most likely type of delusion to be acted on (Reference Wessely, Buchanan and ReedWessely et al, 1993) and are a predictor of admission to hospital (Reference Castle, Phelan and WesselyCastle et al, 1994).
There are many other psychiatric and neurological diagnoses in which persecutory delusions occur in a substantial minority of patients. These include depression, mania, post-traumatic stress disorder, dementia and epilepsy (Reference Manschreck and PetriManschreck & Petri, 1978).
Increasingly, however, paranoid thoughts are considered not just as a symptom of a disorder but as an experience of interest in its own right, which occurs outside clinical groups and is frequently a cause of distress. The focus is on understanding and treating the distressing experience rather than on the diagnosis. Many have argued that psychotic symptoms such as delusions might be better understood on a continuum with normal experience (e.g. Reference StraussStrauss, 1969). Delusions in psychosis represent the severe end of a continuum, although such experiences are present, often to a lesser degree, in the general population. Thus, a relationship of degree is suggested between, for example, a clinical persecutory delusion about government attempts to kill the person, non-clinical delusions about neighbours trying to get at the person and everyday suspicions about the intentions of others. However, it should be emphasised that there are different forms of the continuum view (Reference ClaridgeClaridge, 1994). The distribution of symptoms may well be quasi-continuous, lying between dichotomous (i.e. most people have no paranoid thoughts and a small proportion have many) and continuous (i.e. there is a normal distribution of paranoid thoughts in the general population similar to, for example, blood pressure), which will depend on the number, prevalence and interaction of causal factors (Reference Van Os, Verdoux, Murray, Jones and Susservan Os & Verdoux, 2003).
A review of 15 studies shows clear evidence that the rate of delusional beliefs in the general population is higher than that of psychotic disorders and that delusions occur in individuals without psychosis (Reference FreemanFreeman, 2006). The frequency of delusional beliefs in non-clinical populations varies according to the content of the delusion studied and the characteristics of the sample population (e.g. age structure, level of urbanicity). About 1–3% of the non-clinical population have delusions of a level of severity comparable to clinical psychosis. A further 5–6% have a delusion but not of such a severity. Although less severe, these beliefs are still associated with a range of social and emotional difficulties. A further 10–15% of the non-clinical population have fairly regular delusional ideation. For example, Jim van Os and colleagues (2000) studied delusions in the large epidemiological Netherlands Mental Health Survey and Incidence Study (NEMESIS). In the sample, 2.1% received a DSM–III–R diagnosis of non-affective psychosis. However, a greater proportion had a ‘true’ psychiatrist-rated delusion (3.3%) or had a ‘clinically not relevant delusion’ (8.7%), defined as the person not being bothered by the belief and not seeking help for it. A separate group of people (3.8%) had endorsed a delusion item, but these beliefs were considered plausible or founded.
Many studies do not differentiate between delusion subtypes, and therefore it is harder to estimate the prevalence of persecutory thinking in particular. A conservative estimate is that 10–15% of the general population regularly experience paranoid thoughts, although such figures hide marked differences in content and severity (Table 2). It is also likely that the studies underestimate the true frequency of paranoid thoughts since large epidemiological studies from a psychiatric perspective are unlikely to record more plausible fleeting everyday instances of paranoid thinking. Reference Johns, Cannon and SingletonJohns et al(2004) report findings from a British survey of over 8000 people. The results of individuals with probable psychosis were removed from the analysis. The assessment of delusions was fairly rudimentary but the results are still striking: 20% had thought in the preceding year that people were against them at times, and 10% felt that people had deliberately acted to harm them. The least plausible paranoid item, fears of a plot, was endorsed by 1.5% of this non-clinical population. Interestingly, there is evidence from more elaborate epidemiological research that odder, less plausible paranoid thoughts build on commoner, more plausible ones, indicating a hierarchical structure to paranoia (Fig. 1).
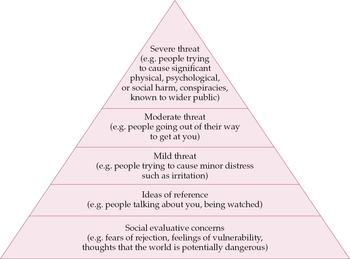
Fig. 1 The paranoia hierarchy (Reference Freeman, Garety and BebbingtonFreeman et al, 2005).
Table 2 Frequency of paranoid thoughts in a student sample (n = 1202)
| Rarely, % | Once a month, % | Once a week, % | Several times a week, % | At least once a day, % | Weekly, % | |
|---|---|---|---|---|---|---|
| I need to be on my guard against others | 31 | 17 | 21 | 21 | 10 | 52 |
| There might be negative comments being circulated about me | 35 | 24 | 21 | 14 | 7 | 42 |
| People deliberately try to irritate me | 57 | 17 | 15 | 8 | 4 | 27 |
| I might be being observed or followed | 67 | 14 | 8 | 7 | 4 | 19 |
| People are trying to make me upset | 72 | 16 | 7 | 4 | 1 | 12 |
| People communicate about me in subtle ways | 52 | 22 | 14 | 9 | 3 | 26 |
| Strangers and friends look at me critically | 29 | 23 | 21 | 18 | 9 | 48 |
| People might be hostile towards me | 45 | 27 | 16 | 9 | 4 | 29 |
| Bad things are being said about me behind my back | 45 | 25 | 15 | 11 | 4 | 30 |
| Someone I know has bad intentions towards me | 71 | 16 | 6 | 4 | 2 | 12 |
| I have a suspicion that someone has it in for me | 83 | 9 | 4 | 2 | 2 | 8 |
| People would harm me if given an opportunity | 83 | 9 | 4 | 2 | 2 | 8 |
| Someone I don’t know has bad intentions towards me | 82 | 10 | 3 | 3 | 2 | 8 |
| There is a possibility of a conspiracy against me | 90 | 5 | 2 | 1 | 2 | 5 |
| People are laughing at me | 41 | 26 | 19 | 9 | 6 | 34 |
| I am under threat from others | 76 | 13 | 5 | 3 | 2 | 10 |
| I can detect coded messages about me in the press/TV/radio | 96 | 2 | 1 | 1 | 1 | 3 |
| My actions and thoughts might be controlled by others | 81 | 10 | 3 | 3 | 2 | 8 |
How is paranoia understood psychologically?
The prevalence figures are consistent with the idea that paranoid thoughts are an appropriate strategy that can, in particular circumstances, become excessive, just like anxious thoughts. Consideration of the potentially hostile intentions of others can be a highly intelligent and appropriate strategy to adopt. Walking down certain streets can be dangerous. Friends are not always good ones. Whether to trust or mistrust is a judgement that lies at the heart of social interactions, and since it is not always an easy decision to make it can be prone to errors. Most people can think of instances where they have misread the intentions of others. Most obviously, this is particularly likely to be the case immediately after negative events that question our trust in others. For example, for several months after being mugged, people can understandably be very wary, vigilant and suspicious when walking in the street.
Persecutory delusions are explicable in terms of normal psychological processes. However, there is an important caveat: no single factor is likely to account for paranoia. With colleagues, we have detailed a multi-factorial account of the formation and maintenance of persecutory delusions that addresses the complexity of the causal picture (Fig. 2) (Reference Garety, Kuipers and FowlerGarety et al, 2001; Reference Freeman and GaretyFreeman & Garety, 2004).
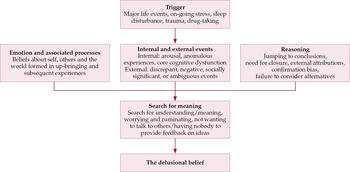
Fig. 2 Outline of factors involved in the development of delusions.
Making sense of events
The key opening for the psychological understanding of paranoia is that such thoughts are individuals’ attempts to explain their experiences, that is, to make sense of events (Reference Maher, Oltmanns and MaherMaher, 1988). The sorts of experiences that are the proximal source of evidence for persecutory delusions are external events and internal feelings.
Clinical experience indicates that ambiguous social information is a particularly important external factor. Such information is likely to be both non-verbal (e.g. facial expressions, people’s eyes, hand gestures, laughter/smiling) and verbal (e.g. snatches of conversation, shouting). Coincidences and negative or irritating events also feature in persecutory ideation.
Unusual or anomalous internal feelings often lead to delusional ideation. For example, the individual might be in a heightened state or aroused; feel that certain events are significant; experience perceptual anomalies (e.g. things may seem vivid or bright or piercing, sounds may feel very intrusive); feel that they are not really ‘there’ (depersonalisation); and might have illusions and hallucinations (e.g. hear voices). Experiences of this sort can also be caused by use of illicit drugs or sleep deprivation.
Typically, individuals who exhibit paranoid thinking are trying to make sense of their internal unusual experiences, often by drawing in negative, discrepant or ambiguous external information (e.g. others’ facial expressions). For example, a person may go outside feeling in an unusual state and rather than thinking ‘I’m feeling a little odd and anxious, probably because I’ve not been sleeping well’, interprets their feelings, together with the facial expressions of strangers in the street, as evidence of a threat (e.g. ‘People don’t like me and may harm me’). But why a persecutory interpretation? We interpret internal and external events in line with our previous experiences, knowledge, emotional state, memories, personality and decision-making processes and therefore the origin of persecutory explanations lies in such psychological processes.
Emotions
Suspicious thoughts often occur in the context of emotional distress. They are often preceded by stressful events such as difficult interpersonal relationships, bullying and isolation. Further, the stresses may happen against a background of previous experiences that have led to beliefs about the self (e.g. as vulnerable), others (e.g. as potentially dangerous) and the world (e.g. as bad) that make suspicious thoughts more likely (Reference Fowler, Freeman and SmithFowler et al, 2006).
Anxiety may be especially important in the generation of persecutory ideation. This is because anxiety and suspiciousness have the same cognitive theme of the anticipation of danger. In our model we hypothesise that anxiety is central in the interpretation of internal and external events and provides the threat theme of paranoia. Hence, we argue that emotion has a direct role in delusion formation (for a review see Reference Freeman and GaretyFreeman & Garety, 2003); this is in contrast to a popular view that delusions conceal emotional distress or low self-esteem (e.g. Reference ColbyColby, 1975; Reference Bentall, Kinderman and KaneyBentall et al, 1994). Typically, therefore, in paranoid thinking a person having unusual experiences that they find it hard to identify and correctly label interprets them in line with their emotional state. If they are anxious it is more likely that the interpretation will be of threat.
Anxious thoughts are truly persecutory when they contain the idea that harm is actually intended by the perpetrator. The cause of this idea of intent is underresearched. We think that most often ideas of threat contain an implicit attribution of intent. Irritation, resentment or anger – often not expressed because of fears of others’ reactions (‘timidity’) – may perhaps contribute to this idea of hostile intent, since judgements of blame and attributions of intent are central to anger. A lack of trust in others, an unwillingness to discuss emotions, or social isolation mean that the feelings of threat and intent are not shared with others but are ruminated on alone, preventing disconfirmation of their persecutory nature.
Reasoning
The final piece of the puzzle is reasoning. It needs to be remembered that persecutory delusions are inherently a judgement and therefore reasoning processes are of central importance. Persecutory ideas are more likely to reach a delusional intensity if there are accompanying biases in reasoning such as reduced data gathering (jumping to conclusions) (Reference Garety and FreemanGarety & Freeman, 1999), failure to consider alternative explanations (Reference Freeman, Garety and FowlerFreeman et al, 2004) and a strong belief confirmation bias (Reference WasonWason, 1960). When reasoning biases are present, suspicions become near certainties; ideas of threat are held with a conviction unwarranted by the evidence and may then be considered delusional.
Our model contains further hypotheses concerning the maintenance and emotional reaction associated with persecutory delusions. For example, since the explanations contain threat beliefs, the fears will be maintained by processes similar to those outlined in the anxiety disorders literature, such as the use of safety behaviours (e.g. avoiding other people) which prevent the processing of disconfirmatory evidence (Reference ClarkClark, 1999). Furthermore, the individual’s relationship with the persecutor may be important in determining emotional reactions; the belief that the persecutor is powerful has been associated with higher levels of depression (Reference Birchwood, Meaden and TrowerBirchwood et al, 2000b ; Reference Freeman, Garety and KuipersFreeman et al, 2001). Thus, we conceptualise paranoia as resulting from individuals’ attempts to understand their experiences, particularly unusual internal states, while under the influence of emotional states such as anxiety and biases of reasoning. Careful assessment is needed to determine the relevant factors in each individual case.
The cognitive–behavioural way of talking to people with paranoid thoughts
Therapeutic style
Therapeutic style is, of course, important for any type of intervention. For instance, the quality of the therapeutic alliance has been found to be a predictor of patients’ adherence to antipsychotic medication regimens (Reference Day, Bentall and RobertsDay et al, 2005). The cognitive–behavioural approach to reducing the distress of people with paranoid thoughts follows directly from the theoretical understanding outlined above. As we have said, there is a consensus that delusions are explanatory accounts of experiences. Delusions are the most compelling explanation that the person has arrived at on the basis of previous childhood and adult events, knowledge, emotional state, memories, personality and reasoning processes. It can be helpful for clinicians to keep in mind Maher’s idea that ‘the delusional belief is not being held “in the face of evidence normally sufficient to destroy it,” but is being held because of evidence powerful enough to support it’ (1974: p: 99). Therefore the clinician will want to learn more about the chain of events, experiences, feelings and judgements that has led to suspicious thoughts. Thus, the style of engagement is based on what Reference Kingdon and TurkingtonKingdon & Turkington (2002: p. 3) have called ‘a journey of exploration into patients’ beliefs’, which should be undertaken with an open mind and a willingness to understand the individual and find out about them.
This ‘voyage of discovery’ attitude will be more helpful in engaging the patient than any simple implementation of a set of techniques. The exploratory approach must be combined with an empathic, collaborative style. The patient needs to feel that their problems are being taken seriously. The therapist should listen empathically and regularly give brief summaries of what the patient has been saying. This will ensure that the clinician has understood and will help structure the discussion. The therapist should comment on the distress caused by the experiences, but without agreeing that the perceived threat is real, for example ‘It must make you very anxious’ or ‘Believing that the neighbours are trying to harm you must feel very intrusive and be upsetting’. The clinician should be collaborative, drawing up a list of goals with the patient, discussing what will happen in the meetings and regularly asking the patient for both positive and negative feedback on the meetings. Providing written information on paranoid thoughts can be helpful (Reference Freeman, Freeman and GaretyFreeman et al, 2006). Any immediate concerns (e.g. thoughts of suicide, difficulties getting to therapy sessions) should be dealt with before a full assessment is carried out. The clinician needs to be flexible in both the length of sessions and the degree to which key material is focused on. They must also keep a close eye on whether there are aspects of the sessions that the patient finds upsetting. In the early sessions, the therapist should not start challenging delusions, but perform the more difficult task of listening and trying to understand the patient’s perspective: challenging delusions in an inexpert way is equivalent to not listening to the patient’s experiences. It can also be extremely helpful not always to focus on problems but to find out about the positive aspects and achievements of the individual and show that you have noticed them. Patients with suspicious thoughts often present with low self-esteem, difficulties with trust and fears that others think they are ‘mad’. A clinician who shows positive regard can help circumvent these negative self-views, which sometimes hinder engagement.
Obstacles to good engagement
There are, of course, obstacles to forming a good collaborative relationship with an individual who has paranoid thoughts. Elements of the role of a psychiatrist bring problems. Two key issues are hospitalisation and medication. An individual with paranoid thoughts may be worried about revealing these and being admitted compulsorily to hospital (or not discharged, if already an in-patient). The psychiatrist will often be keen to prescribe medication, which the patient may take as an indication that the clinician’s mind is already made up or which might conflict with the wishes of the patient. Such difficulties need to be acknowledged, discussed openly and resolved by negotiation. Specific techniques for developing appropriate medication adherence, including forming a collaborative relationship, using motivational interviewing, provision of information, and monitoring symptoms and side-effects, are described elsewhere (e.g. Reference Randall, Wood, Day and MorrisonRandall et al, 2002).
There is also the issue of the use of language. Mental health professionals may use diagnostic terms such as schizophrenia and give only biological explanations for experiences. Illness accounts of experiences can be helpful to some patients but there are two main difficulties with them. The first is that they contain within them a number of potential further or other meanings. For example, for some patients ‘schizophrenia’ carries connotations of madness and violence, they believe it to be an uncontrollable organic condition that will not improve and they fear that they will be shunned by others. There is an emerging and important literature indicating that careful attention should be given to appraisals of illness – concerning, for example, cause, course, outcome, loss, entrapment and humiliation – because they can lead to distress (Reference Birchwood, Iqbal and ChadwickBirchwood et al, 2000a ; Reference Lobban, Barrowclough and JonesLobban et al, 2003).
The second difficulty with illness models is that they mostly provide a poor causal description of a person’s subjective experiences. For example, telling Mr Smith that he is ‘ill’ does not necessarily provide a compelling account of why, when he goes outside, he feels very anxious, senses that something odd is going on and notices that people in the street are looking at him. A delusional explanation that people seem to recognise and know about him, are aware of bad things about his past and, as a consequence, are hostile may provide a richer account for Mr Smith of his subjective experience and draws on his own knowledge. Patients may favour the delusional account, being richer, over the illness account.
In psychological therapies, as shall be seen, an elaborated alternative account that draws on both the patient’s and the therapist’s knowledge is made: for example, that the patient has had previous adverse experiences with others (e.g. has been bullied) and therefore expects threat, may be more prone to notice it in ambiguous social information and to jump to the conclusion that they are to be harmed whenever there is any sign of danger. The therapist also tries to ensure that there is a simple, non-stigmatising label for such an account (e.g. that the person is ‘alert’ or ‘sensitive’ to threat). These accounts developed in therapy, similar in explanatory power to the delusional accounts, may make a more plausible alternative than either the ‘illness’ or the ‘delusional’ accounts.
Another obstacle to engagement can be that the clinician becomes incorporated into the delusional system. If the clinician’s approach is empathic and based on understanding, this happens less often than they fear it might. However, the clinician should anticipate the problem by checking at the end of initial meetings whether the patient has any concerns about them (e.g. ‘You have described mistrusting people. I therefore wondered whether you’ve had any such worries about me?’). If the patient does have such concerns the clinician should first explain their role very clearly. If the patient does not respond to simple reassurance the clinician should use problem-solving techniques to address the difficulty in the therapeutic relationship. For example, the clinician might suggest that the patient does not talk about the most private aspects of their experiences until they feel greater trust or may ask whether there is anything that they could do to ease the patient’s worries about them. It can be helpful for the clinician to show the patient the notes being taken in the meeting. It can bring down the emotional impact of paranoid thoughts in meetings if the clinician points out that it is not surprising that the patient is suspicious about the clinician, given the delusional system, and that it is simply a problem that can be discussed like any other and compromises and solutions can be found.
The techniques of cognitive–behavioural therapy for paranoia
The general strategy of trying to understand, in the context of an empathic and collaborative approach, are key whatever treatment is adopted. But for a cognitive–behavioural intervention there are many additional elements, and these are outlined here. There have been repeated demonstrations of the efficacy of cognitive–behavioural therapy (CBT) for delusions and hallucinations (e.g. see review by Reference Zimmermann, Favrod and TrieuZimmermann et al, 2005). The evidence base is strongest concerning CBT for persistent positive symptoms such as delusions. About 20% of patients with persistent symptoms do very well in treatment and another 40% show important improvements (e.g. Reference Kuipers, Garety and FowlerKuipers et al, 1997). Reference Tarrier, Yusupoff and KinneyTarrier et al(1998) report that, in a comparison with routine care alone, CBT resulted in almost eight times greater odds of a reduction in psychotic symptoms of 50% or more. In acute psychosis, there is evidence that CBT can speed time to recovery (Reference Drury, Birchwood and CochraneDrury et al, 1996; Reference Lewis, Tarrier and HaddockLewis et al, 2002). Furthermore, there is a small amount of evidence that some forms of CBT may reduce relapse rates (Reference Gumley, O'Grady and McNayGumley et al, 2003). The intervention is certainly popular with patients. However, not all respond to this approach. It is recommended for people with distressing delusions, since it enables individuals to engage with the collaborative goal of reducing distress. It is much less likely to be of use for individuals who are not distressed by their paranoid experiences. Cognitive deficits are not a contraindication for treatment, nor is the absence of insight into having an illness.
It is important to note that at this stage of development CBT for delusions is not a brief treatment; typically, it needs to be provided weekly for at least 6 months. Although similar to CBT for other disorders, clinicians should be aware that modifications to the approach are needed for delusions. Therapists using CBT for psychosis are often working with people who have complex disorders and need a good understanding of the psychology of psychosis, cognitive therapy skills, and regular supervision and support. It is also important to be aware that CBT is provided as part of a multi-modal treatment that includes antipsychotic medication and, for example, assertive community treatment, rehabilitation, supported employment and family intervention.
Assessment and formulation: ‘making sense of psychosis’
The initial task is to develop an individualised formulation that accounts for the patient’s paranoid thoughts and the associated distress. This occurs through detailed descriptions of paranoid experiences and their development. The formulation is a personalised account of the development of paranoid thoughts based on the cognitive model and is not simply ‘education about illness’. The clinician should be thinking about the following sorts of questions:
-
• On what evidence is the person basing their thoughts?
-
• How do paranoid thoughts build on the patient’s ideas about the self and others and ordinary worries?
-
• How do the thoughts make sense given previous life events?
-
• Is the person reacting to puzzling and confusing experiences?
-
• How is the person reasoning about their experiences?
-
• What behaviours are keeping the thoughts going?
The answers to these questions are then fed back to the patient for their opinion (e.g. ‘I may have this wrong, but could it be that, given the things that have happened in the past, your first reaction now is to think that others will be bad to you?’ or ‘From what you’ve said, you seem to rely on your instinct to know that there is threat, rather than think of many different explanations for others’ behaviour and weigh up the evidence – do I have that right, do you think?’). Gradually the therapist will develop a formulation – a multifactorial account of the development of the paranoid thoughts. Sometimes all, sometimes parts, of the formulation are shared with the patient.
There are a number of benefits to good formulation: † a full description of the patient’s subjective experiences is made, which is empathic, normalising, makes the experiences understandable and does not treat the patient as if they were ‘mad’; it enables patients to revisit their decision-making processes with the benefit of time and new information; it can provide an alternative non-delusional account of experiences; and it identifies targets of therapy. One of the most important elements in the therapy is that the clinician slows down and ‘unpacks’ the decision-making processes that lead to paranoid thoughts. This enables patients to gain distance from their thoughts so that they are more likely to review (often implicit) interpretations at any or all of the different steps in the development of their paranoid accounts. It also allows the clinician and the patient to introduce fresh information and other ideas that enable a different sense to be made of experiences. Given this renewed attempt at making sense, patients can consider how they might proceed differently in thought or behaviour.
Cognitive therapies were developed in a tradition that interventions should be assessed for their efficacy, and therefore formal measures of symptoms are routinely taken by therapists in individual cases to monitor treatment effectiveness (using, for example, PSYRATS; Reference Haddock, McCarron and TarrierHaddock et al, 1999).
Interventions after formulation
Making sense of persecutory experiences illuminates many potential therapeutic paths. Thus, if anomalous experiences are assessed as central to delusion formation – for instance, the paranoid thoughts are provoked by feelings of depersonalisation, a sense of reference, perceptual disturbances or hallucinations – therapy may aim to reduce the frequency of such experiences using a functional analysis (examining the triggers and reactions), to change the interpretation of the anomalous experiences, or simply to enhance coping strategies. Where anxiety and worry contribute to the persistence of paranoid ideas, other ways of dealing with thinking about fears can be introduced and worry-reduction strategies used (Reference WellsWells, 1997). In some cases it is possible to review with patients the evidence for and against different explanations for their experiences and to conduct behavioural experiments (i.e. to test out the persecutory thoughts). In other cases, the therapist and patient will be ‘working within’ persecutory delusions, and distress may be reduced by, for example, focusing on the interpretations associated with the most distressing aspects of the delusion (e.g. the degree to which the person is powerless, whether the threat is as widespread as thought), or Ed. by developing alternative ways of reacting to the threat. In our self-help book on overcoming paranoid and suspicious thoughts (Reference Freeman, Freeman and GaretyFreeman et al, 2006), intervention for paranoid thoughts is crystallised into six key steps (Box 2). These encourage the reader to:
Box 2 Six key self-help steps in overcoming paranoid thoughts
-
1 Become a detached observer of your fears. Readers are shown how to monitor and learn about their paranoid thoughts using diaries and writing exercises
-
2 Develop a detailed understanding of the causes of suspicious thoughts. Substantial information is provided on the causes of paranoid thoughts, and readers are shown in a structured way how to formulate their own experiences
-
3 Review paranoid interpretations rather than just accepting them. The rules of good decision-making are introduced and readers are shown how to review their paranoid thoughts and alternative explanations for their experiences
-
4 Test out suspicious thoughts. It is explained how to test out paranoid fears in behavioural experiments. Hierarchies of tests are constructed, predictions made and the results of tests considered
-
5 Let go of a suspicious thought when it comes. Readers are encouraged not to fight suspicious thoughts when they occur but instead to let them go and focus on what they are doing, not what they are thinking
-
6 Spend less time worrying about paranoid thoughts. Reduction in worry is attempted by showing how worrying makes things worse, introducing ‘worry periods’ and substituting problems
-
1 become a detached observer of their fears;
-
2 develop a detailed understanding of the causes of suspicious thoughts
-
3 review paranoid interpretations rather than just accepting them;
-
4 test out suspicious thoughts;
-
5 ‘let go’ of a suspicious thought if it comes;
-
6 reduce the time spent worrying about paranoid thoughts.
Frequently, clinicians also work with patients on improving low self-esteem (Reference Hall and TarrierHall & Tarrier, 2003), reducing depression, increasing activities and structuring time. Our theoretical model clearly indicates that reducing emotional difficulties should also lead to lessening of suspiciousness.
Finally, the therapist and patient may try to prevent relapse by identifying vulnerabilities and early warning signs and rehearsing compensatory strategies.
Conclusions
Cognitive–behavioural therapy for paranoid and suspicious thoughts draws on a range of techniques that are applied on the basis of an individualised formulation of the patient’s difficulties. However, importantly, what unites the techniques is the assumption that the patient’s subjective experiences should be taken seriously and that patients can be helped to make paranoid experiences less threatening, less interfering and more controllable. This parallels the psychological approaches taken to treat emotional disorders such as anxiety and depression and reflects a substantial advancement in the treatment of paranoid thoughts.
Declaration of interest
D.F. and P.G. are co-authors of a self-help book on overcoming paranoid and suspicious thoughts (Reference Freeman, Freeman and GaretyFreeman et al, 2006).
MCQs
-
1 1The approximate proportion of the general population (excluding those diagnosed) that regularly have paranoid thoughts is:
-
a 0–10%
-
b 10–20%
-
c 20–30%
-
d 30–40%
-
e Over 40%.
-
-
2 Persecutory thoughts are distinguished from anxious thoughts by:
-
a the fact that their content is incorrect
-
b the anticipation of danger
-
c the belief that harm is intended
-
d the level of distress
-
e the person acting on the thought.
-
-
3 In CBT the following is not considered as a potential cause of persecutory delusions:
-
a reasoning
-
b anomalous experiences
-
c anxiety
-
d diet
-
e ideas about self and others.
-
-
4 Persecutory ideas are considered as:
-
a fears partly caused by past experiences
-
b arising from random firing of neurons
-
c individuals’ attempts to make sense of events
-
d a product of thought disorder
-
e empty speech acts without meaning.
-
-
5 CBT for delusions is contraindicated if the patient:
-
a has poor insight
-
b has cognitive deficits
-
c is taking antipsychotic medication
-
d has persistent symptoms
-
e is not distressed by their paranoia.
-
MCQ answers
| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | F | a | F | a | F | a | T | a | F |
| b | T | b | F | b | F | b | F | b | F |
| c | F | c | T | c | F | c | T | c | F |
| d | F | d | F | d | T | d | F | d | F |
| e | F | e | F | e | F | e | F | e | T |







eLetters
No eLetters have been published for this article.