Fat-soluble vitamins (D, E, K and A) have in recent years been put on the forefront of asthma and allergy research, primarily by studies on immunomodulatory properties of vitamin D and its association with child wheeze and eczema( Reference Litonjua 1 ). Maternal vitamin E intake has likewise been examined in observational studies and found to protect against child wheeze and asthma up to age 5 years( Reference Devereux, Turner and Craig 2 – Reference Miyake, Sasaki and Tanaka 4 ), though results from a recent randomised clinical trial were less convincing( Reference Greenough, Shaheen and Shennan 5 ). The latter null results could be explained by the fact that women were supplemented during the second trimester. It has been suggested that vitamin E influences airway development, and therefore the effect of supplementing vitamin E might be more pronounced in the first trimester( Reference Gonzalez-Reyes, Martinez and Martinez-Calonge 6 , Reference Islam, Narra and Cote 7 ).
Vitamin A and associated retinoids are important for growth, homeostasis and development( Reference Allende, Corell and Madrono 8 ). Vitamin A has also been shown to play a prominent role in immune functions. Animal and in vitro studies have demonstrated how retinoids enhance T-cell proliferation( Reference Friedman, Halevy and Schrift 9 ) and function in B-lymphocyte growth and development( Reference Blomhoff, Smeland and Erikstein 10 ). However, few human studies have examined the risk of child asthma in relation to prenatal levels of vitamin A. Vitamin A supplementation in pregnancy has been shown to increase a type 1 immune response( Reference Cox, Arthur and Kirkwood 11 ), suggesting that a skewed in utero milieu may reduce the risk of asthma in the child( Reference Holgate 12 ). A randomised clinical trial in Nepal conducted in a vitamin A-deficient population found no relationship with child asthma at 9–13 years of life( Reference Checkley, West and Wise 13 ), but found that supplementation improved lung function( Reference Checkley, West and Wise 14 ), while in a trial in Indonesia with β-carotene, children of supplemented mothers had lower levels of interferon-γ( Reference Wieringa, Dijkhuizen and Muhilal 15 ).
Little evidence exists on the role of vitamin K in asthma development, though new evidence suggests that vitamin K may have important functions beyond its role in the coagulation cascade( Reference Shearer and Newman 16 ). These include anti-inflammatory properties and free radical-scavenging activity, which may be important in immune system function and development.
Here we aim to replicate current findings on vitamin E and extend the present analyses to maternal intake of vitamins A and K from foods and supplements in relation to the risk of child asthma and allergy-related outcomes.
Methods
Study population
The Danish National Birth Cohort enrolled >100 000 pregnancies between 1996 and 2003 during their first antenatal visit as part of a study to examine pregnancy exposure on maternal and child health during pregnancy and postpartum. Women participated in two interviews during pregnancy (at gestational weeks 12 and 30) and two interviews after birth (at 6 and 18 months). They also filled out a FFQ in gestational week 25. The participants and their children were followed up through registry linkage using the unique identity number possessed by every Danish citizen and through a self-administered questionnaire when the children turned 7 years.
Of the 103 119 cohort pregnancies, we excluded 4190 multiple births and 303 stillborn singletons, and limited the present data to the first Danish National Birth Cohort pregnancies (n 84 020) in order to avoid dependencies among correlated measures. We had dietary information on 61 211 pregnant women and information on supplements from 44 772 women. The final dataset was limited to pregnant women with total (diet plus supplement) vitamin A, E and K intake (n 44 594). Sample size varied depending on missing data for the individual outcomes ( − 26 to 36 %).
The pregnant women provided written informed consent on behalf of their children. The Regional Scientific Ethics Committee for the municipalities of Copenhagen and Frederiksberg approved all study protocols, and all procedures were in accordance with the Declaration of Helsinki.
Dietary and supplement assessment
Dietary intake was assessed by using a validated( Reference Mikkelsen, Olsen and Rasmussen 17 , Reference Mikkelsen, Osler and Olsen 18 ) 360-item FFQ. The questionnaire was mailed to each participant at about week 25 of gestation, and assessed dietary habits and supplement use during the previous 4 weeks( Reference Olsen, Mikkelsen and Knudsen 19 ). In a validation study, estimated intake of retinol was found to correlate well with 7 d food records( Reference Mikkelsen, Osler and Olsen 18 ); vitamin E and K intakes were not validated. Daily dietary intakes of vitamins A, E and K were estimated by multiplying the reported frequencies of consumption with standard portion sizes and recipes and applying information on the content of micronutrients from the National Food Institute's Food Composition Databank (http://www.foodcomp.dk/v7/fcdb_search.asp). Dietary intakes were energy-adjusted using the residual method( Reference Willett 20 ), and women who reported intake that resulted in unrealistic energy intake estimates (arbitrarily set to < 2500 or >25 000 kJ/d) were excluded (0·5 %). Micronutrient intakes from supplements were calculated from the information that participants provided on the name of the product, the producer, the nutrient content per daily dose and the number of daily doses. We compiled a database of supplement use by combining the information from the Danish Veterinary and Food Administration with the frequency of intake reported by the participants and the daily recommended intake stated on the supplement.
Outcome assessment
We assessed child asthma status at two different time points using parental reports at 18 months and 7 years and population-based registry data. ‘Asthma at 18 months’ was defined from the phone interviews as a parental-reported doctor diagnosis. ‘Current asthma at 7 years’ was defined using standardised core questions from the International Study of Asthma and Allergies in Childhood (ISAAC)( Reference Asher, Keil and Anderson 21 ). To increase the specificity of the ‘current asthma at 7 years’ outcome, we combined the parental-reported doctor diagnosis and wheezing symptoms in the past 12 months( Reference Hederos, Hasselgren and Hedlin 22 ).
In addition to the questionnaire information, we used the data from two registries on hospital contacts and medication use to define asthma diagnoses in the first 7 years of life. These outcomes have been described in detail elsewhere( Reference Hansen, Strom and Maslova 23 ). Briefly, we defined ‘ever admitted asthma’ as children with a first asthma diagnosis in the Danish National Patient Register using the International Classification of Disease 10 codes. Furthermore, we obtained information on the use of anti-asthmatic medications from the Register of Medicinal Product Statistics. On the basis of the medication data, we used a validated algorithm to define ‘ever prescribed asthma’ as children with at least two prescriptions for inhaled β2-agonists or steroids or at least one prescription for any other anti-asthmatic drug( Reference Moth, Vedsted and Schiøtz 24 ).
Finally, allergic rhinitis cases were defined as a parental report of a doctor diagnosis of hay fever using an ISAAC question from the 7-year questionnaire.
Covariates
We collected and evaluated information on maternal sociodemographic and lifestyle covariates from the pregnancy interviews apart from breast-feeding which was based on the interview data from 6 and 18 months postpartum. These covariates included proficiency (by parental education level and occupation), maternal age at birth of child, parity, maternal pre-pregnancy BMI, maternal smoking during pregnancy, maternal exercise during pregnancy, breast-feeding duration, child sex, maternal and paternal history of asthma and allergies, and month of the last menstrual period. Dietary covariates that have previously shown associations with allergic disease were included: fruit and vegetable intake, and intake of long-chain n-3 fatty acids, vitamins D and C, Se and Zn from diet and supplements (all in quintiles; reviewed in Litonjua( Reference Litonjua 25 )). All covariates were self-reported except for maternal age and month of the last menstrual period which were extracted from the national registries. The missing indicator method was used to account for missing covariate data when the proportion of missing data was >1 % (socio-economic status, parity, pre-pregnancy BMI, parental history of asthma and allergies, maternal physical activity and breast-feeding); if ≤ 1 %, then the missing observations were deleted( Reference Greenland and Finkle 26 ).
Statistical analysis
First, we compared the distributions of maternal vitamin A, E and K intake across the categories of age-standardised covariates. We age-standardised the distribution because of significant differences in maternal vitamin intake across the age categories, with intake among women ≥ 30 years being higher compared with younger women.
The main exposure was maternal total vitamin intake. In secondary analyses, we further separated out intake from diet and supplements in order to account for potentially different action of food v. tablet formulations. Secondary exposures included breaking up vitamin A intake into β-carotene and retinol. Maternal vitamin intake was modelled as both linear and by quintiles. To avoid undue influence of outliers in the linear analyses, we restricted the intake to 10 000 μg/d for vitamin A (n 44 removed), 1000 mg/d for vitamin E (n 3) and 700 μg/d for vitamin K (n 11) based on either the tolerable upper level or the empirical distribution when the former was missing. Quintiles of exposure were composed when possible and indicator values modelled, comparing each quintile to the lowest (reference) quintile. Furthermore, we examined non-linear relationships for exposures and covariates and OR of child asthma non-parametrically with restricted cubic splines( Reference Durrleman and Simon 27 ). Tests for non-linearity used the likelihood ratio test, comparing the model with only the linear term to that with both the linear and the cubic spline terms. As we have previously found a non-linear relationship between season of the last menstrual period and birth weight with child asthma (E Maslova, unpublished results), we entered these variables as cubic terms into the final model.
Log-binomial models were used to estimate relative risks and 95 % CI( Reference Wacholder 28 , Reference Skov, Deddens and Petersen 29 ). In a few instances, the models did not converge and log-Poisson models, which provide consistent, but not fully efficient, estimates of the relative risks and its CI, were used( Reference Zou 30 ). Median values for the exposure categories were entered separately into the models as a continuous variable to evaluate the P value for trend. Interactions by parental asthma and allergy history, breast-feeding and maternal vitamin D intake (vitamin A only) were examined using tertiles of maternal vitamin intake and evaluated using a robust score test( Reference Guo, Pan and Connett 31 ).
Covariates for the multivariable model were based on biological priors and risk factors for the outcomes identified in the literature. Variables suspected to be on causal pathways, such as gestational weight gain, birth weight, gestational age and child covariates (day-care attendance, antibiotics use in early life and exposure to pets), were initially excluded from the model to avoid overadjustment. Further adjustment for these covariates did not alter the results.
In sensitivity analyses, we dichotomised the exposures according to the US( 32 ) dietary recommendations. Due to the disagreement of an upper limit for pregnant women( Reference Rothman, Moore and Singer 33 ), we also examined the risk of asthma and allergic rhinitis for vitamin A intake categories of 1000, 2000 and 10 000 μg/d. To determine whether a high or low consumption of all the three vitamins influences the risk of the child outcomes, we composed a fat-soluble vitamin index, grouping women based on whether they were in (1) the lowest quintile of all the three vitamins, (2) the highest quintile of all the three vitamins and (3) any one of the other quintiles (reference). To isolate more clinically relevant asthma diagnoses from the registries rather than more benign wheeze in the first few years of life, we excluded asthma diagnoses that were made during the first 3 years of life( Reference Martinez, Wright and Taussig 34 ).
All tests were two-sided, and we used a threshold of P< 0·05 to denote statistical significance. The analyses were performed using the Statistical Analyses System software (release 9.3; SAS Institute).
Results
Study population
Among the pregnant women with information on fat-soluble vitamin intake, about one-half were between the ages 25 and 30 years (45 %), of high or medium proficiency (53 %) and nulliparous (not having given birth earlier) (56 %). Of the pregnant women, 9 and 32 % reported a history of asthma and allergies, respectively. The median intake of total vitamins A, E and K was 1359 (interquartile range 1083–1662) μg/d, 16 (interquartile range 14–18) mg/d and 122 (interquartile range 80–159) μg/d, respectively.
Table 1 shows the age-standardised covariate frequencies across the lowest and highest quintiles of maternal total vitamin A, E and K intake. High-frequency consumers of vitamin A tended to be older, to smoke daily, be multiparous and had marginally lower gestational weight gain. They had a slightly higher vegetable intake, and intake of total folate, n-3 fatty acids, Se, Zn and vitamins D, K and C, though the standard deviation tended to overlap across the quintiles of maternal vitamin A intake. Similar trends were found for high vitamin E and K consumers; however, pregnant women consuming vitamin E in the highest quintile were less likely to have a BMI ≥ 25 kg/m2, less likely to report daily smoking and more likely to be physically active. Consumers of vitamin K in the highest quintile were furthermore less likely to be unskilled and students, less likely to be daily smokers and were more physically active.
Table 1 Age-standardised predictors of total vitamin A, E and K intake among 44 594 women in the Danish National Birth Cohort* (Mean values and standard deviations or percentages)

* Values are standardised to the age distribution of the study population.
† Values are expressed in mg/d.
‡ Value is not age adjusted.
§ Fruit: citrus fruit+berries+banana+Danish fruit+other fruit.
∥ Vegetables: cabbage+onion+green leafy vegetables+root vegetables+tomato+other vegetables.
Comparing pregnant women with (n 33 415) and without (n 11 179) outcome data on asthma at 18 months, we found that those with outcome data were more likely to be nulliparous (55 v. 60 %) and more likely to have children born in the spring and summer (50 v. 44 %). Pregnant women with outcome data at the 7-year time point (n 28 678) v. no outcome data (n 15 916) were more likely to be ≤ 25 years (19 v. 23 %), of high to medium proficiency (55 v. 49 %), have a BMI in the 18·6–24·9 kg/m2 range (65 v. 60 %) and not smoking (77 v. 73 %).
Parental report of child asthma at 18 months and 7 years
The prevalence of child asthma at 18 months was 17 % (5632 out of 33 415) and 4 % (1122 out of 28 678) at 7 years. We did not find any association for maternal vitamin A, E and K intake and child asthma at 18 months, and for maternal vitamin A and E intake and current asthma at age 7 years (Tables 2–4 and Tables S1–S6). Maternal dietary vitamin A was related to current asthma at age 7 years (1·20, 95 % CI 1·03, 1·39 for a 1000 μg/d increase) (Table S1, available online). A higher intake of maternal total vitamin K was related to an increased risk of current asthma at age 7 years (Q5 v. Q1: 1·30, 95 % CI 0·99, 1·70), which was present already in Q2 (89 (sd 10) μg/d) (Table 4).
Table 2 Associations between maternal total vitamin A intake in mid-pregnancy and child asthma at 18 months and 7 years in the Danish National Birth Cohort (Relative risks (RR) and 95 % confidence intervals)
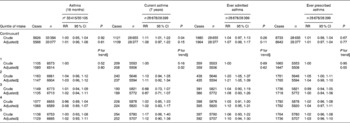
* Number of participants in the crude/adjusted analysis.
† Analysis excluded potential outliers as described in the main text. Unit of change was set to 1000 μg/d.
‡ Adjusted for maternal age, socio-economic status, parity, pre-pregnancy BMI, maternal physical activity, maternal smoking during pregnancy, breast-feeding duration, child sex, maternal history of asthma, maternal history of allergies, paternal history of asthma, paternal history of allergies, season of last menstrual period, and energy, fruit intake, vegetable intake, and intake of fish fatty acids (EPA+DPA+DHA), folic acid, vitamins D and C, Se and Zn (all in quintiles).
§ Median values for each quintile are entered as a continuous variable into the model.
Table 3 Associations between maternal total vitamin E intake in mid-pregnancy and child asthma at 18 months and 7 years in the Danish National Birth Cohort (Relative risks (RR) and 95 % confidence intervals)

* Number of participants in the crude/adjusted analysis.
† Analysis excluded potential outliers as described in the main text. Unit of change was set to 10 mg/d.
‡ Adjusted for maternal age, socio-economic status, parity, pre-pregnancy BMI, maternal physical activity, maternal smoking during pregnancy, breast-feeding duration, child sex, maternal history of asthma, maternal history of allergies, paternal history of asthma, paternal history of allergies, season of last menstrual period, and energy, fruit intake, vegetable intake, and intake of fish fatty acids (EPA+DPA+DHA), folic acid, vitamins D and C, Se and Zn (all in quintiles).
§ Median values for each quintile are entered as a continuous variable into the model.
Table 4 Associations between maternal total vitamin K intake in mid-pregnancy and child asthma at 18 months and 7 years in the Danish National Birth Cohort (Relative risks (RR) and 95 % confidence intervals)
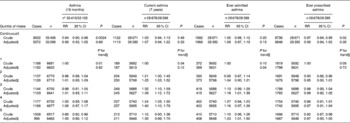
* Number of participants in the crude/adjusted analysis.
† Analysis excluded potential outliers as described in the main text. Unit of change was set to 100 μg/d.
‡ Adjusted for maternal age, socio-economic status, parity, pre-pregnancy BMI, smoking during pregnancy, partner's smoking during pregnancy, physical activity, child sex, maternal history of asthma, maternal history of allergies, paternal history of asthma and paternal history of allergies, and energy, fruit intake and vegetable intake, and intake of total EPA+DPA+DHA, vitamins C and D, folate, Zn and Se (all in quintiles).
§ Median values for each quintile are entered as a continuous variable into the model.
Registry-based ever asthma diagnosis at 7 years
Of the children, 7 % (1983 out of 28 678) and 30 % (8738 out of 28 678) were classified with asthma by the patient and medication registries, respectively. There was no association for maternal vitamin A and E intake with the registry-based asthma outcomes (Tables 2 and 3 and Tables S1, S2, S4 and S5), though maternal vitamin A intake from diet modestly increased the risk of an ever prescribed asthma diagnosis in children (Q5 v. Q1: 1·05, 95 % CI 0·99, 1·11; Table S1, available online). Maternal total vitamin K intake was directly associated with ever admitted asthma (Q5 v. Q1: 1·23, 95 % CI 1·01, 1·50) only; a similar association was present for maternal vitamin K intake from diet, but not supplements (Table 4; Tables S3 and S6, available online).
To exclude potential transient wheeze in early childhood that may have been captured and classified as asthma by the registries, we excluded the first 3 years of life from these analyses. The number of cases decreased from 1983 to 1014 for ever admitted asthma and from 8738 to 2118 for an ever prescribed asthma diagnosis. The associations were largely unaltered by restricting the analysis to diagnoses above age 3 years.
Parental report of ever child allergic rhinitis
A total of 5 % (1420 out of 28 536) of children were reported by their mother to have a hay fever diagnosis at the 7-year follow-up. Maternal intake of vitamins A, E and K were not related to ever child allergic rhinitis (Tables S7–S9) however, there was a suggestion towards an inverse association for maternal total vitamin A intake (Q5 v. Q1: 0·86, 95 % CI 0·70, 1·04, P= 0·12) and maternal total vitamin E intake (Q5 v. Q1: 0·84, 95 % CI 0·66, 1·06, P= 0·14) (Tables S7 and S8, available online).
Sensitivity analyses
When examining the relationship between maternal fat-soluble vitamin intake and child asthma and allergic rhinitis using the fat-soluble vitamin index, we found an inverse association for allergic rhinitis only. Consuming in the highest category of the fat-soluble vitamin index (n 948/13 516) decreased the risk of ever child allergic rhinitis at 7 years (all high v. middle group: 0·60, 95 % CI 0·37, 0·95).
For maternal vitamin K intake, meeting the recommended daily intake of 90 μg/d (n 30 191/44 594) was associated with an increased risk of current asthma at 7 years (1·31, 95 % CI 1·11, 1·51) and ever admitted asthma (1·15, 95 % CI 1·01, 1·30), but there were no associations with the other outcomes; we found no associations for maternal intake of vitamins A and E.
Since retinol and β-carotene may affect asthma by different aetiologies, we also examined these exposures separately. Maternal total retinol intake from supplements and diet was inversely associated with child allergic rhinitis only (Q5 (4188 (sd 81 879) μg/d) v. Q1 (632 (sd 146) μg/d): 0·79, 95 % CI 0·65, 0·96). Maternal dietary β-carotene intake was directly associated with current asthma at age 7 years (Q5 (6817 (sd 5319) μg/d) v. Q1 (889 (sd 226) μg/d): 1·38, 95 % CI 1·06, 1·80).
Examining intake at the high end of the distribution of maternal vitamin A intake (1000, 2000 and 10 000 μg/d) showed similar inverse associations for retinol, whereas extremely high intakes of β-carotene seemed to be inversely associated with child asthma.
We analysed the relationship of maternal vitamin A, E and K intake with any reported wheeze and >3 episodes v. ≤ 3 episodes/no wheeze in the first 18 months of the child's life. Maternal vitamin A intake from supplements, but not diet, showed a direct relationship with any wheeze symptoms (Q5 v. Q1: 1·17, 95 % CI 1·05, 1·30). A direct association was also observed between maternal dietary vitamin E intake and wheeze at 18 months (Q5 v. Q1: 1·06, 95 % CI 0·99, 1·13). For maternal vitamin K intake, no association was observed for wheeze at 18 months, but maternal total vitamin K intake was directly associated with recurrent wheeze found by comparing Q3 with Q1 (1·19, 95 % CI 1·04, 1·36), but not for other quintiles.
When testing interactions for maternal vitamin A intake and maternal and paternal asthma and allergies, breast-feeding and a vitamin A × vitamin D interaction, we found an increased risk of child asthma at 18 months related to maternal intake of total vitamin A among the children of mothers who reported a history of asthma (Q5 v. Q1: 1·21, 95 % CI 0·96, 1·54) and allergies (Q5 v. Q1: 1·18, 95 % CI 1·02, 1·37), and a decreased risk of ever prescribed asthma related to maternal vitamin E intake from supplements when mothers breast-fed ≥ 7 months (Q5 v. Q1: 0·87, 95 % CI 0·77, 0·99). We did not find any association in children of mothers who did not report a history of asthma and allergies and those who breast-fed < 7 months. No interactions were found for maternal vitamin K intake.
Discussion
We examined the relationship between maternal intake of vitamins A, E and K during pregnancy and child asthma and allergic rhinitis during the first 7 years of life in 44 594 mother–child pairs. We did not find any consistent patterns for maternal vitamin A and E intake in relation to child asthma and allergic rhinitis. Maternal vitamin K intake appeared to increase the risk of ever admitted asthma and current asthma at age 7 years, while maternal vitamin A and E intake modestly decreased the risk of child allergic rhinitis during the first 7 years of life. Differential associations with child allergic outcomes may be present for maternal retinol v. β-carotene intake. Consuming in the highest quintiles of all the three vitamins decreased the risk of child allergic rhinitis.
The present findings are in conflict with some of the previous studies of fat-soluble vitamins, but support a recent vitamin E supplementation trial( Reference Greenough, Shaheen and Shennan 5 ), which failed to show an effect of high-dose prenatal supplementation with vitamin C and E on respiratory outcomes at age 2 years. Other studies have found that maternal vitamin E intake during pregnancy reduced the risk of wheeze in children at the age of 2 years( Reference Litonjua, Rifas-Shiman and Ly 3 , Reference Miyake, Sasaki and Tanaka 4 , Reference Martindale, McNeill and Devereux 35 ), and noted that these results persisted for wheeze and asthma up to the age of 5 years( Reference Devereux, Turner and Craig 2 ). Other studies have reported both an increase in wheeze and no association( Reference West, Dunstan and McCarthy 36 , Reference Erkkola, Nwaru and Kaila 37 ). Comparison between studies should be done with care due to differences in study design and populations, and speculations regarding the potential threshold level of vitamin E intake for optimal immunity are difficult since some studies have not reported the levels of vitamin E intake in exposure groups( Reference Devereux, Turner and Craig 2 , Reference Martindale, McNeill and Devereux 35 ). We are aware of only one study that related maternal vitamin E intake during pregnancy to child allergic rhinitis and found no association( Reference Devereux, Turner and Craig 2 ). Studies on food sources of vitamin E in pregnancy and allergic rhinoconjunctivitis/rhinitis in children have found both inverse( Reference Ellwood, Asher and Bjorksten 38 ) and direct( Reference Farchi, Forastiere and Agabiti 39 ) associations. Maternal vitamin E supplementation has not demonstrated any benefit in improving the symptoms of seasonal or perennial allergic rhinitis in the offspring( Reference Montano Velazquez, Jauregui-Renaud and Banuelos Arias Adel 40 , Reference Shahar, Hassoun and Pollack 41 ).
Studies in infants have indicated that vitamin E may activate a type 1 immune response rather than an asthma-inducing type 2 response( Reference Baehner, Boxer and Allen 42 , Reference Chirico, Marconi and Colombo 43 ). Since early-life respiratory symptoms may include both transient wheeze due to respiratory infection and true asthma, it could explain previous findings of protective associations with wheeze at < 2 years of age and our own null finding for child asthma at 7 years of age. However, the present study suggests that high maternal vitamin E intake during pregnancy may modestly protect against child allergic rhinitis.
Few studies have examined maternal vitamin A supplementation in relation to allergic diseases. Consistent with our null finding, a trial in Nepal that supplemented women with 7000 μg retinol equivalents (RE) of provitamin A, 42 mg β-carotene or placebo during pregnancy has found no association with child asthma incidence, but showed improved lung function with supplementation( Reference Checkley, West and Wise 13 , Reference Checkley, West and Wise 14 ). A randomised trial among Indonesian women on β-carotene supplementation has noted lower interferon-γ production among their infants( Reference Wieringa, Dijkhuizen and Muhilal 15 ). In the present study, we found that a high intake of β-carotene decreased the risk of asthma, and these findings were strongest for maternal doses ≥ 10 000 μg/d. This suggests that both the quantity and quality of vitamin A may be important to consider or that the risk may vary by study population. Studies in infants have found that vitamin A-deficient infants have significantly lower interferon-γ production compared with infants with adequate vitamin A status( Reference Wieringa, Dijkhuizen and West 44 ). Animal studies have found opposite results, in which vitamin A deficiency has been reported to decrease the development of experimental asthma( Reference Cantorna, Nashold and Hayes 45 , Reference Schuster, Kenyon and Stephensen 46 ), suggesting that deficiency may skew towards a type 1 response and away from a more asthma-inducing type 2 response. An up-regulation of a type 1 response with vitamin A deficiency was also observed among children aged < 13 years examined cross-sectionally( Reference Jason, Archibald and Nwanyanwu 47 ). On the contrary, a study in pregnant women supplemented with retinol (v. placebo) has found increased IL-10 and interferon-γ production, skewing away from a type 2 response( Reference Cox, Arthur and Kirkwood 11 ). However, it is unclear whether these changes are sufficient to influence the development of the fetal immune system. The present results showed no increase in child asthma risk with a higher maternal intake of vitamin A, and only a weak increase for an ever prescribed asthma diagnosis. The differences in findings may include a difference in underlying vitamin A intake and biological levels where a change from a deficient or near-deficient state may have a positive impact on fetal respiratory and immune system development, while excess vitamin A from a sufficient state may have minor negative consequences. However, adverse effects cannot be excluded for other endpoints( Reference Rothman, Moore and Singer 33 ). Additionally, a family history of asthma and allergies may modify the risk of early asthma in the offspring.
We found that the risk of child allergic rhinitis was reduced with a higher maternal intake of vitamin A, specifically retinol. Studies in children have found a reduced risk of allergic rhinitis and associated symptoms with vitamin A sources such as vegetables( Reference Ellwood, Asher and Bjorksten 38 ) and milk( Reference Farchi, Forastiere and Agabiti 39 ), but not vitamin A itself( Reference Ellwood, Asher and Bjorksten 38 , Reference Huang and Pan 48 ). The inverse results found for maternal vitamin A and (indicative for) E intake in the present study may point to the importance of these nutrients in the prevention of sensitisation (e.g. T-helper cell switching, IgE production) rather than direct respiratory effects.
We initially hypothesised that proposed anti-inflammatory properties and free radical-scavenging activities of vitamin K16 may lead to a reduced risk of asthma and allergic rhinitis in children whose mothers ate at the higher end of the distribution. The results of the present study indicated the opposite, that maternal total vitamin K intake increases the risk of ever admitted asthma and current asthma in children at age 7 years. To our knowledge, this is the first study to examine maternal vitamin K intake during pregnancy in relation to these outcomes and hence give us no prior evidence on which to draw from. Despite the many beneficial effects of vitamin K on human health, since the 1980s, there have been several case reports of hypersensitivity and anaphylactic reactions to intravenous( Reference de la Rubia, Grau and Montserrat 49 – Reference Rich and Drage 54 ) and cutaneous( Reference Chung, Ramos-Caro and Beers 55 – Reference Lemlich, Green and Phelps 57 ) vitamin K injections. While rare and short-enduring, these and the present data may point to a greater and more complex involvement of vitamin K in sensitisation and related diseases.
There are some limitations to the present study. Dietary assessment using FFQ results in measurement error due to assumptions on portion sizes, quality of food tables and accuracy in self-reporting. Dietary measurement error is usually random and would therefore only underestimate the strength of any true underlying association to the null. In the present analysis, we were not able to adjust for exposure of child vitamin A, E and K intake during breast-feeding and in childhood due to the lack of this information; we can therefore not exclude the possibility that maternal diet served as a marker for diet during breast-feeding. However, both observational and supplementation studies have not been able to link either child intake of vegetables or supplements with asthma( Reference Checkley, West and Wise 13 , Reference Arvaniti, Priftis and Papadimitriou 58 – Reference Willers, Wijga and Brunekreef 61 ), indicating that any confounding by child diet is most probably minor or negligible. Observational studies with a long follow-up are prone to both confounding and selection bias. We cannot exclude the possibility of residual confounding by unmeasured or mismeasured covariates; nonetheless, by adjusting for numerous covariates, we limited the possibility of residual confounding. We also examined the distributions of sociodemographic and lifestyle covariates among participants and non-participants of the present study and found few differences, suggesting that any present selection bias would be limited.
The present study has several strengths. We were able to follow nearly 45 000 mother–child pairs prospectively and longitudinally. The FFQ used in the present study assessed diet in great detail, allowing us to capture maternal vitamin intake from both diet and supplements, as well as focus on both pre- and provitamin A in order to discern potential aetiological differences. The extensive dietary questionnaire would also more accurately assess energy intake and reduce measurement error when dietary intake is energy-adjusted.
Asthma and allergic disease have a time-dependent manifestation of symptoms( Reference Bel 62 – Reference Stein and Martinez 64 ). While wheeze and ‘asthma’ in the first few years of life may represent transient conditions due to viral infections, respiratory and sensitisation symptoms by age 7 years are more likely to represent clinical disease( Reference Henderson, Granell and Sterne 63 ). Following the children from conception to 7 years of age, we examined numerous outcomes stretching from early to later childhood, and thereby investigating possible associations with several phenotypes of asthma that may be governed by different aetiologies. In addition to self-reported measures of asthma that would be an overall measure of asthma and would not specifically distinguish between phenotypes of asthma, we were able to include two additional measures based on population-based register data. Admitted asthma represents a more severe phenotype or uncontrolled asthma that required treatment in a hospital setting, while prescribed asthma is more likely to be indicative of mild to moderate asthma requiring some form of medication. For both these registry-based outcomes, the majority of diagnoses were made < 3 years and may therefore not represent a permanent asthmatic phenotype, warranting, as in the present analysis, the examination of cases appearing only after the age of 3 years. For allergic rhinitis, we only had access to one ISAAC question at 7 years relating to an ever doctor diagnosis of hay fever. This question does not capture current or seasonal symptoms, but has been validated against skin prick tests, and self-reported hay fever has been shown to agree well with the symptoms of allergic rhinitis and atopy( Reference Braun-Fahrlander, Wuthrich and Gassner 65 , Reference Wuthrich, Schindler and Leuenberger 66 ).
In conclusion, in the present large prospective cohort of Danish mothers and children, we found no overall pattern of association between maternal intake of fat-soluble vitamins and child allergic disease; yet, maternal intake of vitamin K during pregnancy increased the risk of ever admitted asthma. Weak inverse associations were suggested for maternal total vitamin A and E intake with ever child allergic rhinitis. The results suggest differential associations for sources of intake as well as type of allergic outcome. These findings, especially for the less studied vitamin K, need to be replicated in different cohorts and mechanisms explored in animal studies.
Supplementary material
To view supplementary material for this article, please visit http://dx.doi.org/10./S0007114513003395
Acknowledgements
We thank Anne Ahrendt Bjerregaard for initial background research on maternal vitamin E intake and child asthma.
The present study was supported by the Danish Council for Strategic Research (09-067124); the Danish Council for Independent Research/Medical Sciences, Danish Agency for Science, Technology and Innovation (09-063410); the Lundbeck foundation (R13-A907); and the European Union Integrated Research Project EARNEST (FOOD-CT-2005-007036). The European Union project EARNEST (http://www.metabolic-programming.org) received financial support from the Commission of the European Communities under the FP 6 priority 5: food quality and safety. The Danish National Birth Cohort was financed by the March of Dimes Birth Defects Foundation, the Danish Heart Association, the Danish Medical Research Council, the Sygekassernes Helsefond, the Danish National Research Foundation, the Danish Pharmaceutical Association, the Ministry of Health, the National Board of Health and Statens Serum Institut. The supporting bodies for this project had no role in the design, analysis or writing of this article.
The authors' responsibilities were as follows: E. M. was involved in the study concept and design, prepared the data and performed the analyses; E. M., S. H. and M. S. conducted the main statistical analyses; E. M. and S. H. drafted the manuscript; E. M., S. H., M. S., T. I. H. and S. F. O. contributed to the critical advice and the revision of the manuscript; S. F. O. obtained funding; E. M. and S. F. O. had a role in the acquisition of the data and had responsibility for the entire content of the manuscript. All authors had full access to the study data.
None of the authors had a conflict of interest.






