Dural arteriovenous fistulas (dAVFs) represent 10%–15% of all intracranial vascular malformations. Reference Newton and Cronqvist1 Cranial dAVFs occur near the transverse, sigmoid, and cavernous sinuses, and patients usually present with symptoms of pulsatile tinnitus and/or headaches. Reference Gandhi, Chen, Pearl, Huang, Gemmete and Kathuria2 The Borden classification system is used to characterize dAVFs according to their venous drainage pattern. Reference Borden, Wu and Shucart3 Borden type II and III dAVFs are associated with intracerebral hemorrhage (ICH) presentations and higher annual risks of rebleeding and mortality. Reference Gross and Du4
Intraosseous dAVFs are a rare variant where arterial blood supply fistulizes with diploic veins and drains into the cerebral venous system. Reference Tokuyama, Kiyosue, Hori and Nagatomi5 Case reports of intraosseous dAVFs have shown presentations with ICHs Reference Yako, Masuo, Kubo, Nishimura and Nakao6 and marked cortical venous drainage. Reference Tokuyama, Kiyosue, Hori and Nagatomi5 To date, however, intraosseous dAVFs have not been reported in association with contralateral hemorrhagic events. Here, we report a case of a patient with a left-sided intraosseous dAVF who presented with a right frontal lobe ICH.
A 70-year-old female with a previous history of hemicolectomy for an adenocarcinoma, chronic renal failure, and hyperthyroidism was brought to the hospital after being found in her home with decreased level of consciousness. She had returned from a recent travel 2 days prior and had since been feeling generally unwell with complaints of a headache at the base of her skull. Her Glasgow Coma Scale (GCS) score at the scene varied between 3 and 8, and she was noted to have a seizure en route to the hospital. Lorazepam and a loading dose of phenytoin were administered immediately. On physical examination, her blood pressure was 144/80 mmHg and other vital signs were unremarkable. She had a GCS score of 8 (eye 2, verbal 2, motor 4) and her right side withdrew to deep stimuli. She was hemiparetic on the left side with a left facial droop, and she had an upgoing plantar reflex on the left side. She had right-sided gaze deviation that crossed the midline with oculocephalic reflex.
The initial CT scan revealed a right frontal lobe ICH with associated vasogenic edema and mass effect (Figure 1A). Evidence of a small-volume subarachnoid hemorrhage was also noted in the right orbital sulci (Figure 1B). A CT venogram was performed that ruled out cerebral venous sinus abnormalities, and jugular veins appeared patent bilaterally. Prominent cortical veins were present in the right frontal lobe, and in particular, serpiginous vessels were seen in the right orbitofrontal region (Figure 1C–D). No obvious vascular nidus was observed; however, a prominent diploic venous channel transiting through the left sphenoid and frontal bones on its way to the midline was apparent (Figure 1 E–F). A catheter angiogram was performed on suspicion of a dAVF. On the left external carotid artery angiogram, an early-filling vein was noted along the posterolateral aspect of the left orbit that was supplied by the left middle meningeal artery (MMA) (Figure 2A–B). The location of this draining vein correlated with the prominent venous channel seen within the skull on the CT venogram. This vein crossed the midline and subsequently drained into multiple abnormal veins in the right frontal lobe. No vascular abnormalities were detected in the internal carotid artery bilaterally or in the right external carotid artery.

Figure 1. Initial CT investigations. (A–B) Axial noncontrast CT showing right frontal intracerebral hemorrhage with right frontal subarachnoid hemorrhage. (C–D) Coronal CT venogram showing prominence of cortical vessels surround the hematoma. Intraosseous venous structure is highlighted in D (white arrow) (E–F) Axial CT venogram showing a diploic venous channel through the sphenoid and frontal bone on the left and approaching midline (white arrows).
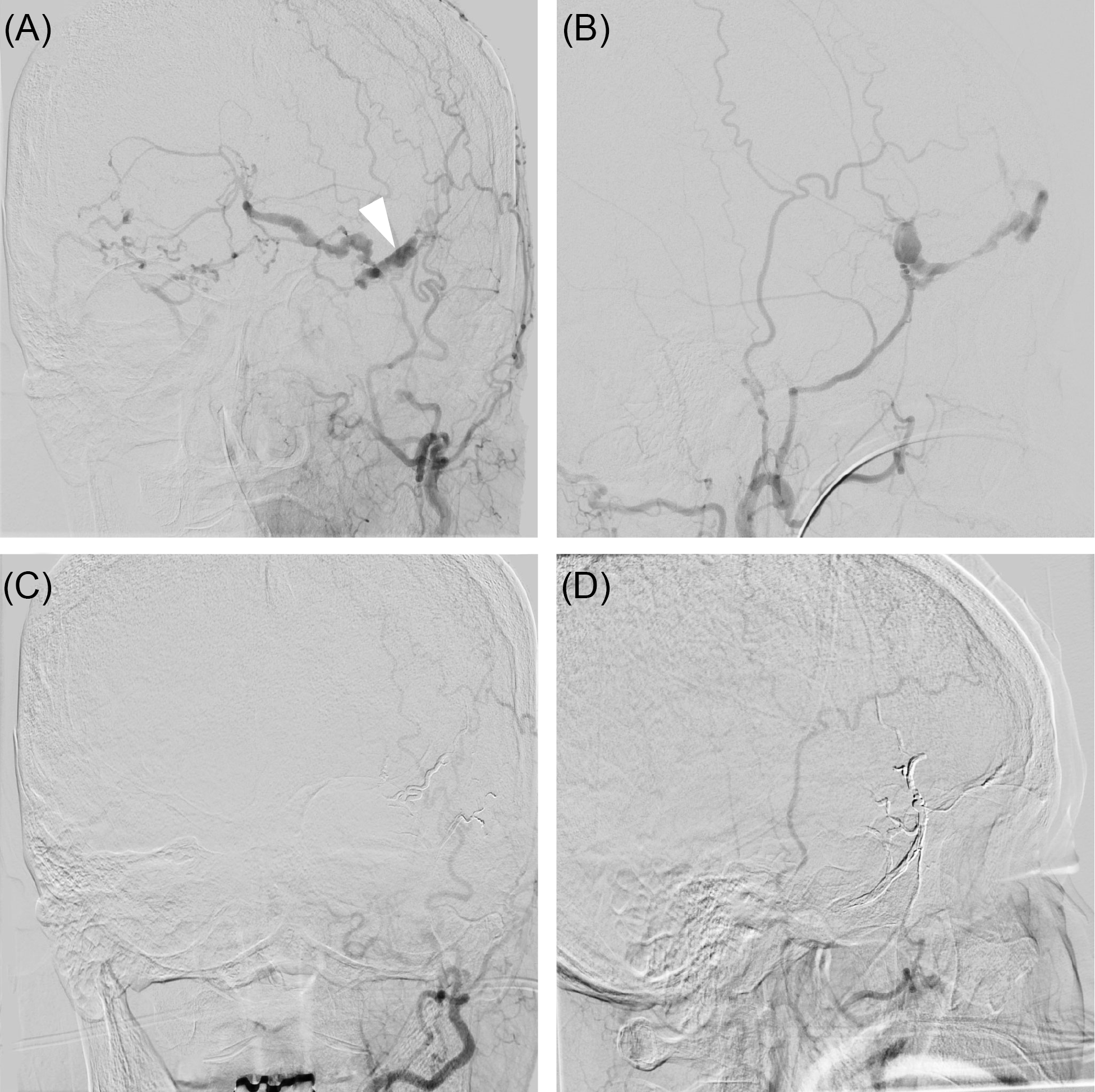
Figure 2. Catheter angiogram demonstrating dAVF before and after treatment. AP (A) and lateral (B) injections of the left external carotid artery in the arterial phase showing shunting through a prominent venous structure above the left orbit (white arrow), and crossing to the contralateral side. (C–D) Following treatment with Onyx liquid embolic agent, the dAVF was successfully obliterated.
A decision was made to proceed with endovascular embolization of the dAVF. The left MMA was accessed, and Onyx embolization agent (Medtronic, Irvine, CA) was injected via a Scepter XC balloon (Microvention, Aliso Viejo, CA). The vein, however, was not completely occluded with embolic material and a subsequent run demonstrated residual filling of the fistula via a branch of the accessory meningeal artery. This artery was then accessed, and Onyx embolization was repeated. Repeat runs of bilateral external and internal carotid arteries demonstrated no residual arteriovenous shunting.
Repeat head CT scans demonstrated appropriate evolution of the right frontal hematoma. A repeat diagnostic cerebral angiogram on post-procedure day 7 showed no evidence of a residual dAVF (Figure 2C–D). The patient was referred to a rehabilitation institute upon discharge after a 17-d course in the hospital. At 6 weeks, she had persistent weakness of her left upper and lower extremities. No other neurological or cognitive deficits were found. The patient was discharged home as she recovered functional independence.
The anatomical configuration of the present intraosseous dAVF can be characterized as Borden type III. The pathophysiology of the dAVFs is yet to be elucidated; however, two theories have attempted to explain this phenomenon: (1) elevated venous pressures result in the pathologic shunting of physiologic arteriovenous shunts between meningeal arteries and dural venous sinuses and (2) venous outflow obstruction with subsequent venous hypertension leading to decreased cerebral perfusion and increased angiogenesis. Reference Gandhi, Chen, Pearl, Huang, Gemmete and Kathuria2
Diploic veins traverse between the inner and outer table of the skull and communicate with the venous system via dural sinuses, pachymeningeal veins, and pericranial veins. Reference Garcia-Gonzalez, Cavalcanti and Agrawal7 Diploic veins in the frontal bone, which were involved in our case, are not known to cross the midline in normal anatomy. They maintain relatively consistent anatomical distributions with drainage into the superior sagittal sinus. Reference Garcia-Gonzalez, Cavalcanti and Agrawal7 In this case, the diploic channel exited the frontal bone at the midline and drained into contralateral cortical veins. Other diploic veins that have been described include the anterior temporal, posterior temporal, and occipital bone diploic veins. Reference Garcia-Gonzalez, Cavalcanti and Agrawal7 These veins form draining confluences near the pterion and asterion regions. Knowledge of the diploic venous anatomy is therefore not only important for understanding intraosseous dAVFs but it can also mitigate bleeding when performing craniotomies. Rivera-Lara et al. Reference Rivera-Lara, Gailloud and Nyquist8 have proposed classifying intraosseous dAVF based on their drainage pattern into either extracranial veins or dural sinuses; however, larger case series are required to identify the clinical relevance of such classification schemes.
The location of ICHs secondary to intraosseous dAVFs vary from subgaleal to subdural/epidural to intraparenchymal. Intraosseous dAVFs of ipsilateral and contralateral origin must therefore be considered in the differential diagnosis of ICH. Treatment strategies include transarterial or transvenous embolization, microsurgical disconnection, or a combination of both. These diverse treatment strategies reflect the complex and heterogenous nature of dAVFs and treatment options should be personalized as such.
Conflict of Interest
No conflicts of interest are declared by the authors.
Statement of Authorship
AA, JR, PD, and MC were involved in the clinical care of the patient described in this case report. AI and MK were responsible for collecting the relevant clinical data and writing the manuscript. All authors made significant contributions toward the discussion in the manuscript and provided final approval.




